Use of Acupuncture in an Infant with Restlessness and Agitation
Abstract
1. Introduction
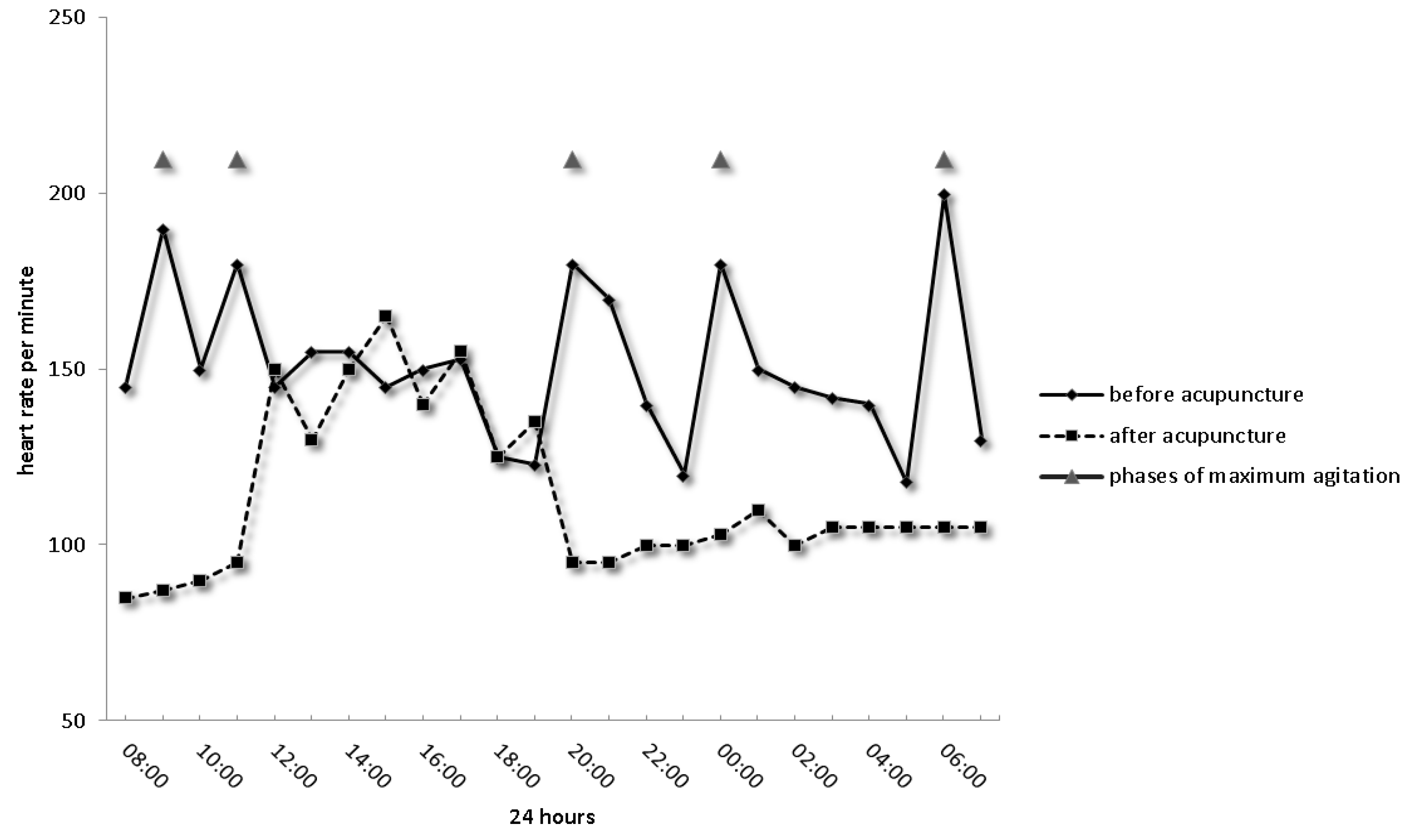
2. Case Report
Acupuncture Therapy
3. Methods
4. Discussion
5. Conclusions
Author Contributions
Funding
References
- Meyer, S.; Gortner, L.; Larsen, A.; Kutschke, G.; Gottschling, S.; Gräber, S.; Schroeder, N. Complementary and alternative medicine in paediatrics: A systematic overview/synthesis of Cochrane Collaboration reviews. Swiss Med. Wkly. 2013, 143, w13794. [Google Scholar] [CrossRef] [PubMed]
- Jindal, V.; Ge, A.; Mansky, P.J. Safety and Efficacy of Acupuncture in Children a Review of the Evidence. J. Pediatr. Hematol. Oncol. 2008, 30, 431–442. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.P.; Liu, P.H.; Lien, A.S.; Yang, S.L.; Chang, H.H.; Yen, H.R. Characteristics of traditional Chinese medicine use in children with asthma: A nationwide population-based study. Allergy 2013, 68, 1610–1613. [Google Scholar] [CrossRef] [PubMed]
- Thiel, M.; Stockert, K. Acupuncture in Neonates—Old Experience or New Evidence? J. Neonatal. Biol. 2013, 2. [Google Scholar] [CrossRef]
- Kemper, K.J.; Vohra, S.; Walls, R. The use of complementary and alternative medicine in pediatrics. Pediatrics 2008, 122, 1374–1386. [Google Scholar] [CrossRef] [PubMed]
- Rusy, L.M.; Weisman, S.J.; Heinsworth, K.R. Developing an in-patient acupuncture treatment in a pediatric hospital. J. Complement. Integr. Med. 2013, 10, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Golianu, B.; Yeh, A.M.; Brooks, M. Acupuncture for Pediatric Pain. Children 2014, 1, 134–148. [Google Scholar] [CrossRef] [PubMed]
- Gentry, K.R.; McGinn, K.L.; Kundu, A.; Lynn, M.A. Acupuncture therapy for infants: A preliminary report on reasons for consultation, feasibility, and tolerability. Paediatr. Aneasth. 2012, 22, 690–695. [Google Scholar] [CrossRef] [PubMed]
- Gottschling, S.; Reindl, T.K.; Meyer, S.; Berrang, J.; Henze, G.; Graeber, S.; Ong, M.F.; Graf, N. Acupuncture to alleviate chemotherapy-induced nausea and vomiting in pediatric oncology—A randomized multicenter crossover pilot trial. Klin. Paediatr. 2008, 220, 365–370. [Google Scholar] [CrossRef] [PubMed]
- Skjeie, H.; Skonnord, T.; Fetveit, A.; Brekke, M. Acupuncture for infantile colic: A blinding-validated, randomized controlled multicentre trial in general practice. Scand. J. Prim. Health Care 2013, 31, 190–196. [Google Scholar] [CrossRef] [PubMed]
- Landgren, K.; Kvorning, N.; Hallström, I. Acupuncture reduces crying in infants with infantile colic: A randomised, controlled, blind clinical study. Acupunct. Med. 2010, 28, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Reinthal, M.; Lund, I.; Ullman, D.; Lundeberg, T. Gastrointestinal symptoms of infantile colic and their change after light needling of acupuncture: A case series study of 913 infants. Chin. Med. 2011, 6, 28. [Google Scholar] [CrossRef] [PubMed]
- Landgren, K.; Kvorning, N.; Hallström, I. Feeding, stooling and sleeping patterns in infants with colic—A randomized controlled trial of minimal acupuncture. BMC Complement. Altern. Med. 2011, 11, 93. [Google Scholar] [CrossRef] [PubMed]
- Ecevit, A.; Ince, D.A.; Tarcan, A.; Cabioglu, M.T.; Kurt, A. Acupuncture in preterm babies during minor painful procedures. J. Tradit. Chin. Med. 2011, 31, 308–310. [Google Scholar] [CrossRef]
- Raith, W.; Urlesberger, B.; Schmölzer, G.M. Efficacy and safety of acupuncture in preterm and term infants. Evid.-Based. Complement. Alternat. Med. 2013, 2013, 739414. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.L.; Quah-Smith, I.; Schmölzer, G.M.; Niemtzow, R.; Oei, J.L. Acupuncture in the neonatal intensive care unit-using ancient medicine to help today’s babies: A review. J. Perinatol. 2017, 37, 749–756. [Google Scholar] [CrossRef] [PubMed]
- Ching, S.W.; Shu, L. A standard international acupuncture nomenclature: Memorandum from a WHO meeting. Bull. World Health Organ. 1990, 68, 165–169. [Google Scholar]
- MacPherson, H.; Altman, D.G.; Hammerschlag, R.; Lin, Y.; Wu, T.; White, A.; Moher, D.; STRICTA Revision Group. Revised standards for reporting interventions in clinical trials of acupuncture (STRICTA): Extending the CONSORT statement. Acupunct. Med. 2010, 28, 83–93. [Google Scholar] [CrossRef] [PubMed]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. BMC Med. 2010, 8, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.M.; Escalera, S.; Lin, E.C.; Maranets, I.; Kain, Z.N. Extra-1 acupressure for children undergoing anesthesia. Anesth. Analg. 2008, 107, 811–816. [Google Scholar] [CrossRef] [PubMed]
- Tugcu, A.U.; Cabioglu, T.; Abbasoglu, A.; Ecevit, A.; Ince, D.A.; Tarcan, A. Evaluation of peripheral perfusion in term newborns before and after Yintang (EX-HN 3) massage. J. Tradit. Chin. Med. 2015, 35, 642–645. [Google Scholar] [CrossRef]
- Kim, M.S.; Seo, K.M. Effects of Atipamezole and Naloxone on Electroencephalographic Spectral Edge Frequency 95 in Dogs Sedated by Acupuncture at GV20 and Yintang Point. J. Vet. Med. Sci. 2007, 69, 577–579. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.; Qu, S.; Zhang, J.; Chen, J.; Zhang, S.; Li, Z.; Chen, J.; Ouyang, H.; Huang, Y.; Tang, C. Correlation between the Effects of Acupuncture at Taichong (LR3) and Functional Brain Areas: A Resting-State Functional Magnetic Resonance Imaging Study Using True versus Sham Acupunture. Evid. Based Complement. Altern. Med. 2014, 2014, 729091. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Sapru, A.; Stewart, M.A.; Milet, M.J.; Hudes, M.; Livermore, L.F.; Flori, H.R. Using acupuncture for acute pain in hospitalized children. Pediatr. Crit. Care Med. 2009, 10, 291–296. [Google Scholar] [CrossRef] [PubMed]
- Usichenko, T.I.; Wolters, P.; Anders, E.F.; Splieth, C. Acupuncture Reduces Pain and Autonomic Distress during Injection of Local Anesthetic in Children: A Pragmatic Crossover Investigation. Clin. J. Pain 2016, 32, 82–86. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.C.; Tassone, R.F.; Jahng, S.; Rahbar, R.; Holzman, R.S.; Zurakowski, D.; Sethna, N.F. Acupuncture management of pain and emergence agitation in children after bilateral myringotomy and tympanostomy tube insertion. Paediatr. Anaesth. 2009, 19, 1096–1101. [Google Scholar] [CrossRef] [PubMed]
- Lu, G.W. Characteristics of afferent fiber innervation on acupuncture points zusanli. Am. J. Physiol. 1983, 245, R606–R612. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.S.; Ko, C.W.; Wu, C.Y.; Chen, G.H. Effect of Electrical Stimulation on Acupuncture Points in Diabetic Patients with Gastric Dysrhythmia: A Pilot Study. Digestion 2001, 64, 184–190. [Google Scholar] [CrossRef] [PubMed]
- Tsai, S.L.; Fox, L.M.; Murakami, M.; Tsung, J.W. Auricular Acupuncture in Emergency Department Treatment of Acute Pain. Ann. Emerg. Med. 2016, 68, 583–585. [Google Scholar] [CrossRef] [PubMed]
- Capone, F.; Assenza, G.; Di Pino, G.; Musumeci, G.; Ranieri, F.; Florio, L.; Barbato, C.; Di Lazzaro, V. The effect of transcutaneous vagus nerve stimulation on cortical excitability. J. Neural Transm. 2015, 122, 679–685. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Acupuncture: Review and Analysis of Reports on Controlled Clinical Trials; World Health Organisation: Geneva, Switzerland, 2002. [Google Scholar]
- Wong, V.; Cheuk, D.K.; Chu, V. Acupuncture for hypoxic ischemic encephalopathy in neonates. Cochrane Database Syst. Rev. 2013. [Google Scholar] [CrossRef] [PubMed]
- Carbajal, R.; Rousset, A.; Danan, C.; Coquery, S.; Nolent, P.; Ducrocq, S.; Saizou, C.; Lapillonne, A.; Granier, M.; Durand, P.; et al. Epidemiology and treatment of painful procedures in neonates in intensive care units. JAMA 2008, 300, 60–70. [Google Scholar] [CrossRef] [PubMed]
- Kundu, A.; Jimenez, N.; Lynn, A. Acupuncture therapy for prevention of emergence delirium in children undergoing general anesthesia. Med. Acupunct. 2008, 20, 151–154. [Google Scholar] [CrossRef]
- Hsiu, H.; Hsu, W.C.; Hsu, C.L.; Huang, S.M. Assessing the effects of acupuncture by comparing needling the hegu acupoint and needling nearby nonacupoints by spectral analysis of microcirculatory laser Doppler signals. Evid. Based Complement. Altern. Med. 2011, 2011, 435928. [Google Scholar] [CrossRef] [PubMed]
- Min, S.; Lee, H.; Kim, S.Y.; Park, J.Y.; Chae, Y.; Lee, H.; Park, H.J. Local Changes in Microcirculation and the Analgesic Effects of Acupuncture: A Laser Doppler Perfusion Imaging Study. J. Altern. Complement. Med. 2015, 21, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Yates, C.C.; Mitchell, A.J.; Lowe, L.M.; Lee, A.; Hall, R.W. Safety of Noninvasive Electrical Stimulation of Acupuncture Points during a Routine Neonatal Heel Stick. Med. Acupunct. 2013, 25, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.W.; Yan, V.C.; Zhang, H. Effect of acupuncture on heart rate variability: A systematic review. Evid.-Based Complement. Altern. Med. 2014, 2014, 819871. [Google Scholar] [CrossRef] [PubMed]
- He, W.; Rong, P.J.; Li, L.; Ben, H.; Zhu, B.; Litscher, G. Auricular acupuncture may suppress epileptic seizures via activating the parasympathetic nervous system: A hypothesis based on innovative methods. Evid.-Based Complement. Altern. Med. 2012, 2012, 615476. [Google Scholar] [CrossRef] [PubMed]
- Cotton, S.; Luberto, C.M.; Bogenschutz, L.H.; Pelly, T.H.; Dusek, J. Integrative Care Therapies and Pain in Hospitalized Children and Adolescents: A Retrospective Database Review. J. Altern. Complement. Med. 2014, 20, 98–102. [Google Scholar] [CrossRef] [PubMed]
- Raith, W.; Schmölzer, G.M.; Resch, B.; Reiterer, F.; Avian, A.; Koestenberger, M.; Urlesberger, B. Laser Acupuncture for Neonatal Abstinence Syndrome: A Randomized Controlled Trial. Pediatrics 2015, 136, 876–884. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, L.; Xiao, R.; Brown, E.R.; Sommers, E. Auricular acupressure augmentation of standard medical management of the neonatal Narcotic Abstinence Syndrome. Med. Acupunct. 2011, 23, 175–186. [Google Scholar] [CrossRef]
- Raith, W.; Litscher, G.; Müller, W.; Urlesberger, B. Laseracupuncture—A possible alternative treatment for agitation and pain in neonates? Paediatr. Anaesth. 2013, 23, 200–208. [Google Scholar] [CrossRef] [PubMed]
- Adams, D.; Cheng, F.; Jou, H.; Aung, S.; Yasui, Y.; Vohra, S. The safety of pediatric acupuncture: A systematic review. Pediatrics 2011, 128, 1575–1587. [Google Scholar] [CrossRef] [PubMed]

© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murg, K.; Raith, W.; Urlesberger, B. Use of Acupuncture in an Infant with Restlessness and Agitation. Medicines 2018, 5, 55. https://doi.org/10.3390/medicines5020055
Murg K, Raith W, Urlesberger B. Use of Acupuncture in an Infant with Restlessness and Agitation. Medicines. 2018; 5(2):55. https://doi.org/10.3390/medicines5020055
Chicago/Turabian StyleMurg, Katharina, Wolfgang Raith, and Berndt Urlesberger. 2018. "Use of Acupuncture in an Infant with Restlessness and Agitation" Medicines 5, no. 2: 55. https://doi.org/10.3390/medicines5020055
APA StyleMurg, K., Raith, W., & Urlesberger, B. (2018). Use of Acupuncture in an Infant with Restlessness and Agitation. Medicines, 5(2), 55. https://doi.org/10.3390/medicines5020055




