Short-Term Effects of Exposure to Atmospheric Ozone on the Nasal and Respiratory Symptoms in Adolescents
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Exposure Assessment
2.3. Measures of Health Outcomes
2.4. Statistical Analysis
3. Results
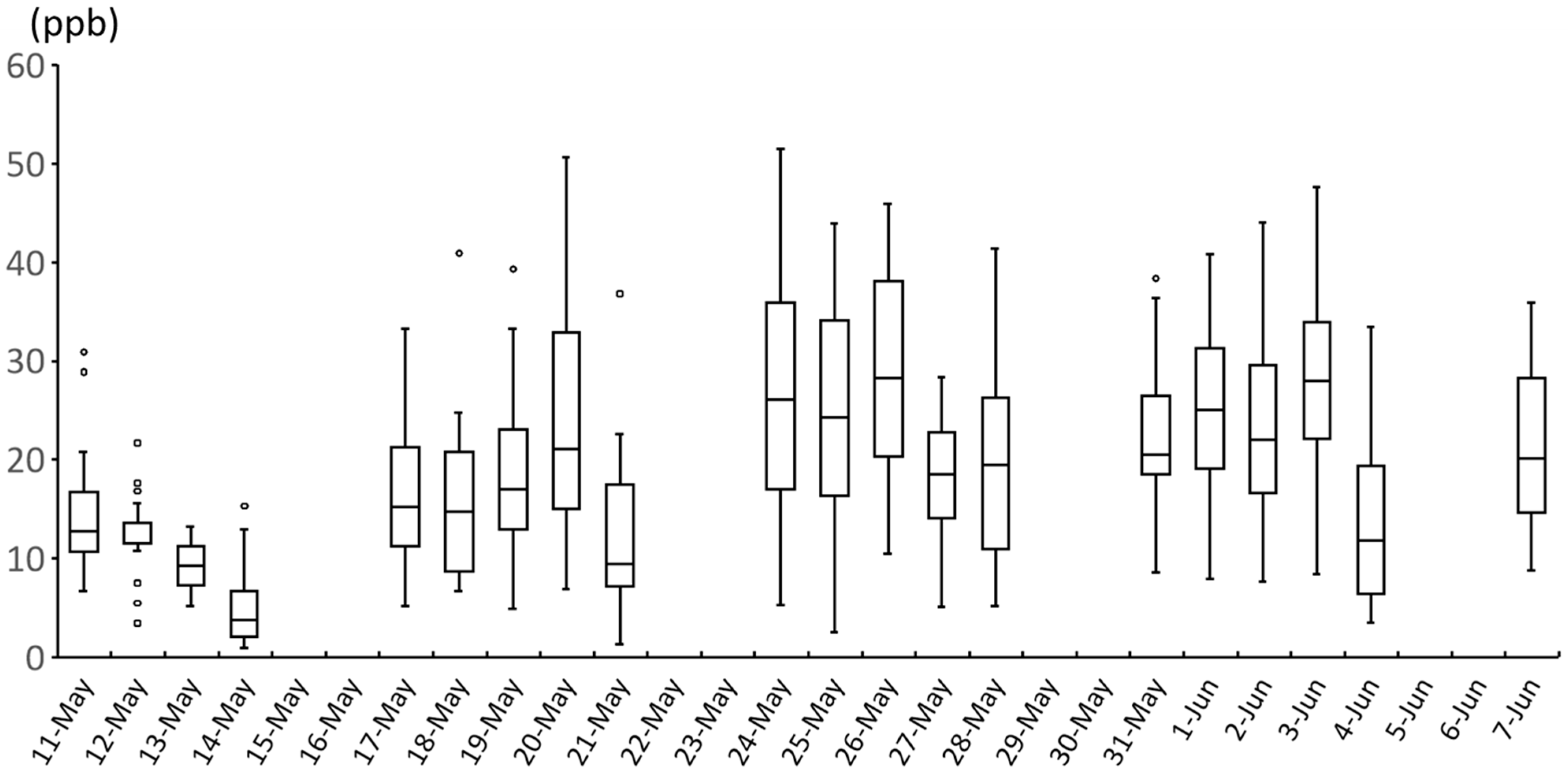
3.1. Descriptive Statistics
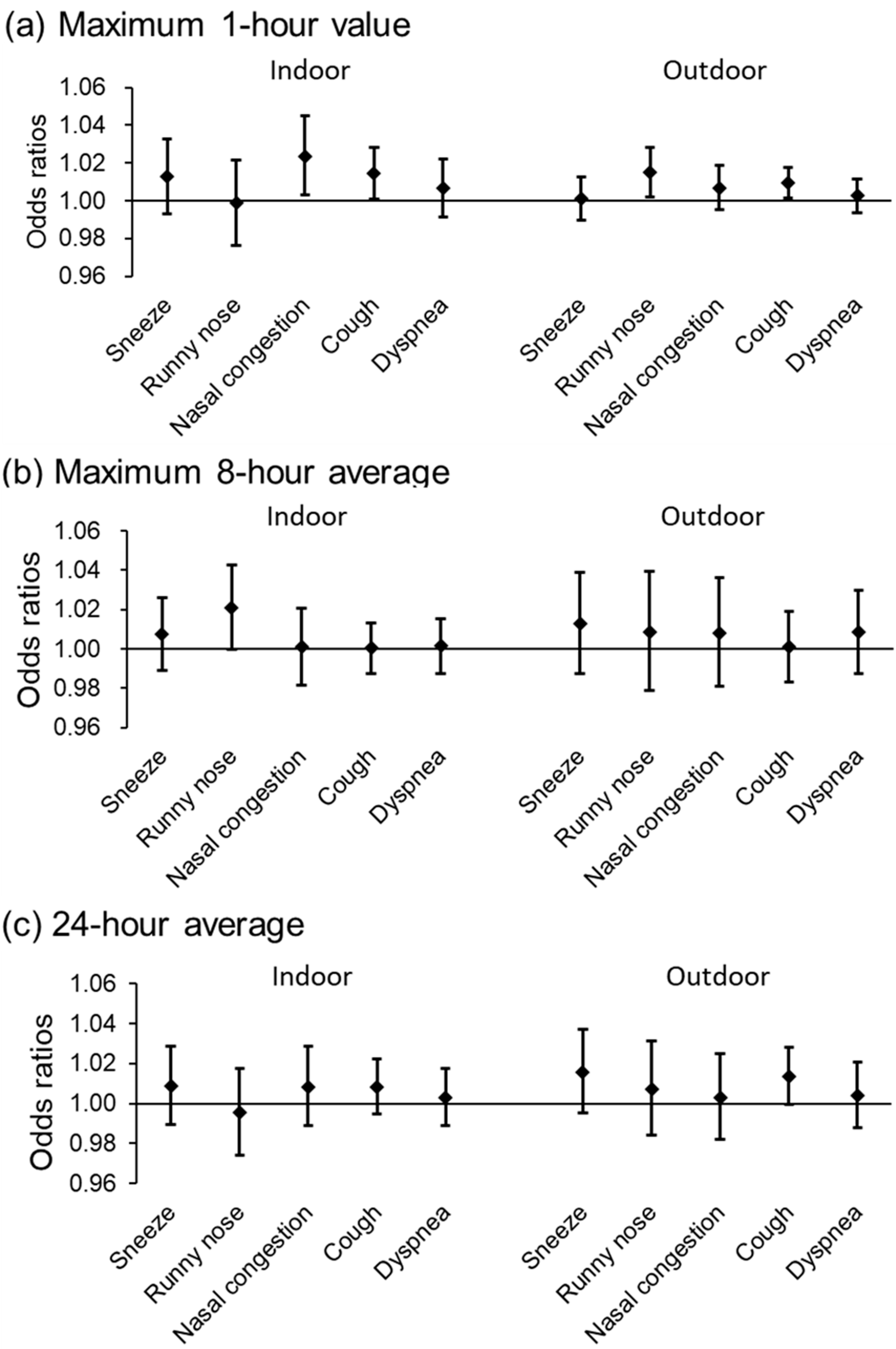
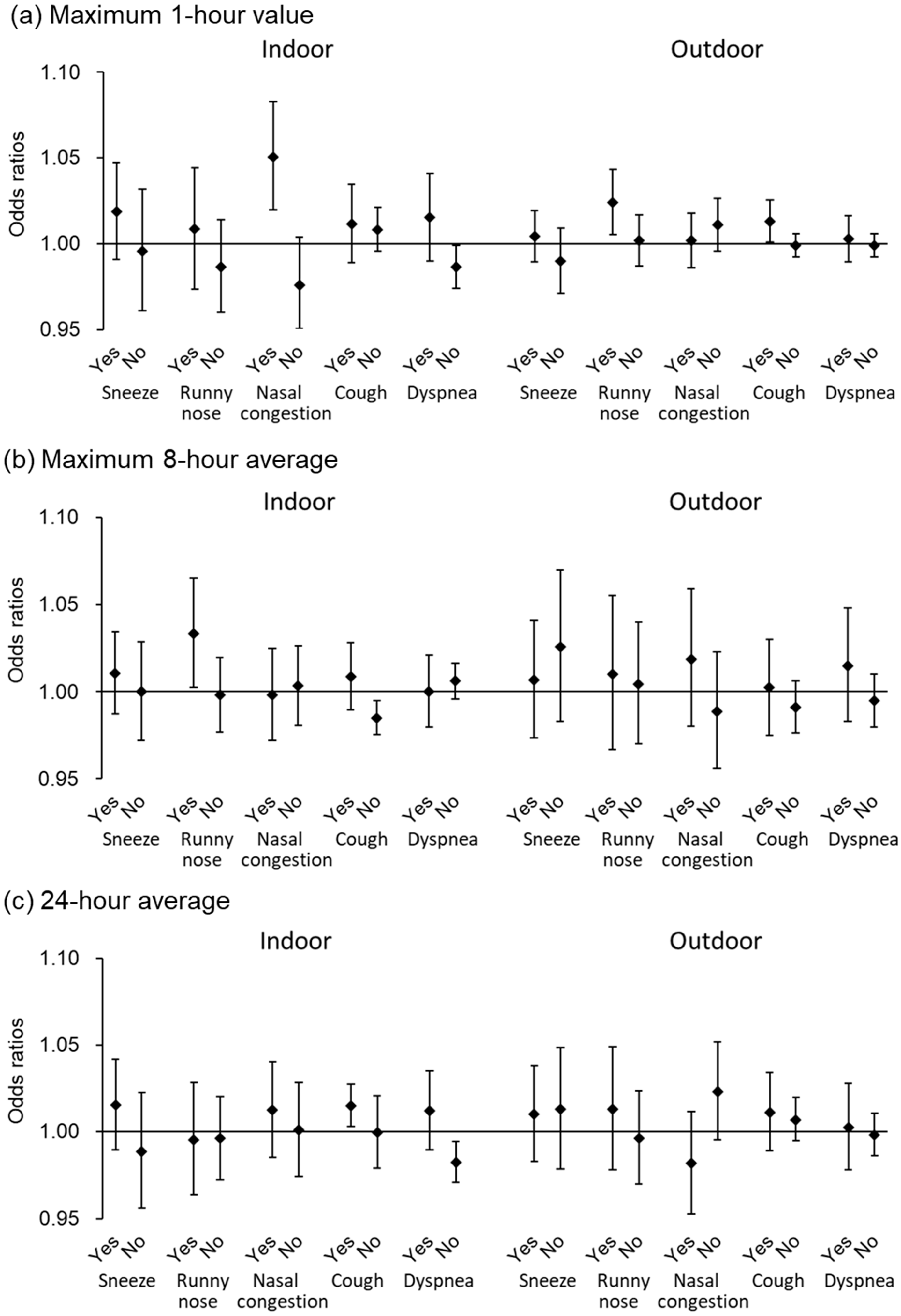
3.2. Relationship Between Indoor and Outdoor O3 Concentrations and Daily Symptoms
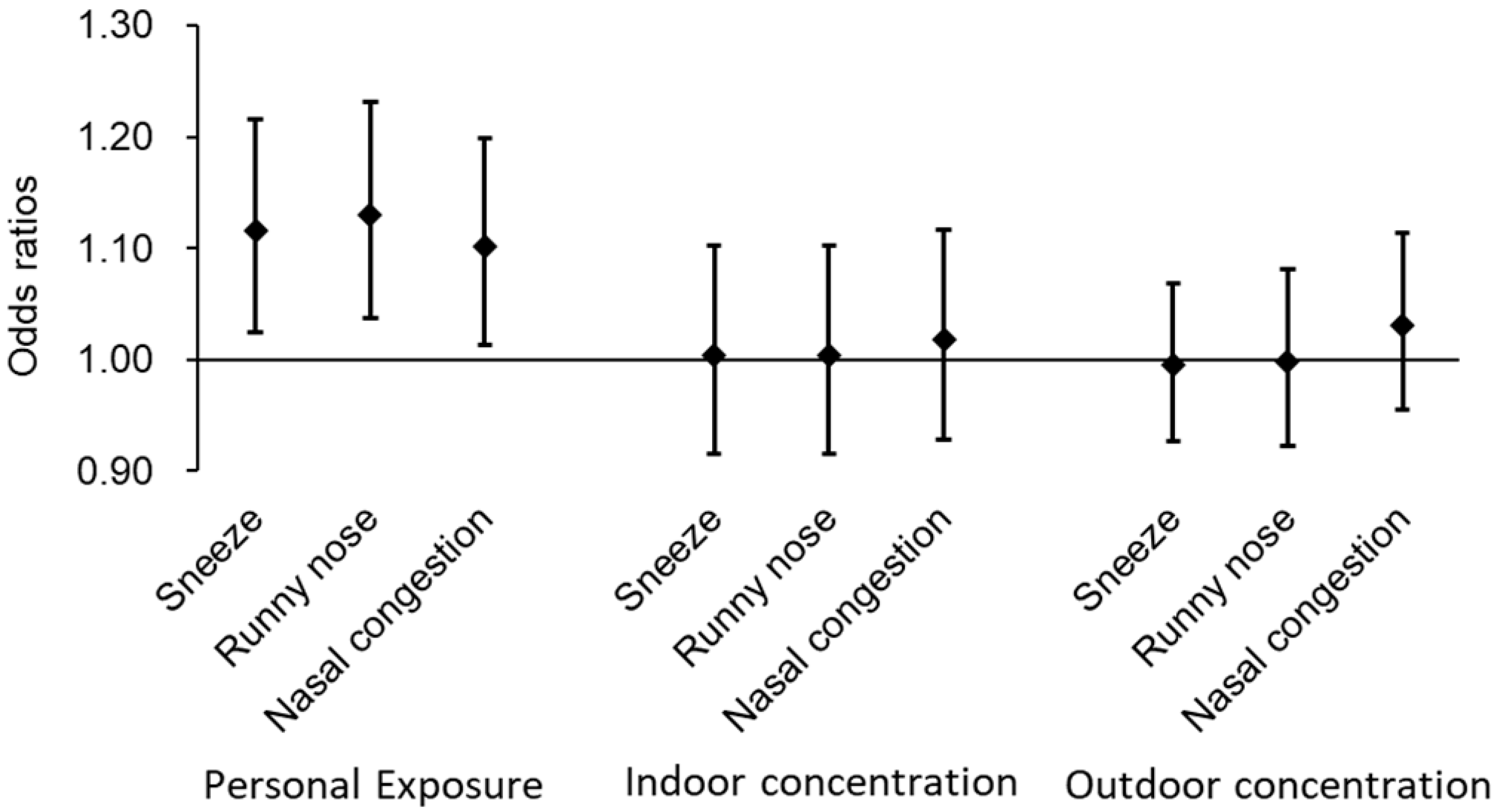
3.3. Relationship Between Personal O3 Exposure and Daily Symptoms
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Ox | photochemical oxidant |
| US EPA | United States Environmental Protection Agency |
| VOCs | volatile organic compounds |
| O3 | ozone |
| WHO | World Health Organization |
| IFN-γ | interferon-gamma |
| PM2.5 | particulate matter ≤ 2.5 μm in diameter |
| NO2 | nitrogen dioxide |
| OR | odds ratio |
| CI | confidence intervals |
| IQR | interquartile range |
| SD | standard deviation |
References
- United States Environmental Protection Agency. Integrated Science Assessment for Ozone and Related Photochemical Oxidants. EPA/600/R-20/012. 2020. Available online: https://www.epa.gov/isa/ (accessed on 10 February 2025).
- Ministry of the Environment, Government of Japan. Annual Report on the Environment, the Sound Material-Cycle Society and Biodiversity in Japan 2024; Ministry of the Environment, General Policy Division: Tokyo, Japan, 2024. Available online: https://www.env.go.jp/en/index_00003.html (accessed on 10 February 2025).
- Gad, S.C. Photochemical Oxidants. In Encyclopedia of Toxicology, 3rd ed.; Wexler, P., Ed.; Academic Press: Oxford, UK, 2014; pp. 926–927. [Google Scholar]
- GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar] [CrossRef]
- World Health Organization. WHO Global Air Quality Guidelines: Particulate Matter (PM2.5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide. 2021. Available online: https://apps.who.int/iris/handle/10665/345329 (accessed on 10 February 2025).
- Zhang, Y.; Ma, Y.; Feng, F.; Cheng, B.; Shen, J.; Wang, H.; Jiao, H.; Li, M. Respiratory mortality associated with ozone in China: A systematic review and meta-analysis. Environ. Pollut. 2021, 280, 116957. [Google Scholar] [CrossRef] [PubMed]
- Malley, C.S.; Henze, D.K.; Kuylenstierna, J.C.I.; Vallack, H.W.; Davila, Y.; Anenberg, S.C.; Turner, M.C.; Ashmore, M.R. Updated global estimates of respiratory mortality in adults ≥ 30 years of age attributable to long-term ozone exposure. Environ. Health Perspect. 2017, 125, 087021. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zu, Y.; Huang, L.; Zhang, H.; Wang, C.; Hu, J. Associations between daily outpatient visits for respiratory diseases and ambient fine particulate matter and ozone levels in Shanghai, China. Environ. Pollut. 2018, 240, 754–763. [Google Scholar] [CrossRef]
- Baloch, R.M.; Maesano, C.N.; Christoffersen, J.; Banerjee, S.; Gabriel, M.; Csobod, E.; de Oliveira Fernandes, E.; Annesi-Maesano, I.; SINPHONIE Study Group. Indoor air pollution, physical and comfort parameters related to schoolchildren’s health: Data from the European SINPHONIE study. Sci. Total Environ. 2020, 739, 139870. [Google Scholar] [CrossRef]
- Yoda, Y.; Otani, N.; Sakurai, S.; Shima, M. Acute effects of summer air pollution on pulmonary function and airway inflammation in healthy young women. J. Epidemiol. 2014, 24, 312–320. [Google Scholar] [CrossRef] [PubMed]
- Yoda, Y.; Takagi, H.; Wakamatsu, J.; Ito, T.; Nakatsubo, R.; Horie, Y.; Hiraki, T.; Shima, M. Acute effects of air pollutants on pulmonary function among students: A panel study in an isolated island. Environ. Health Prev. Med. 2017, 22, 33. [Google Scholar] [CrossRef]
- Berger, M.; Bastl, K.; Bastl, M.; Dirr, L.; Hutter, H.P.; Moshammer, H.; Gstöttner, W. Impact of air pollution on symptom severity during the birch, grass and ragweed pollen period in Vienna, Austria: Importance of O3 in 2010–2018. Environ. Pollut. 2020, 263 Pt A, 114526. [Google Scholar] [CrossRef]
- Gui, Z.H.; Guo, Z.Y.; Zhou, Y.; Dharmage, S.; Morawska, L.; Heinrich, J.; Cheng, Z.K.; Gan, H.; Lin, Z.W.; Zhang, D.Y.; et al. Long-term ambient ozone exposure and childhood asthma, rhinitis, eczema, and conjunctivitis: A multi-city study in China. J. Hazard. Mater. 2024, 478, 135577. [Google Scholar] [CrossRef]
- Weschler, C.J. Ozone’s impact on public health: Contributions from indoor exposures to ozone and products of ozone-initiated chemistry. Environ. Health Perspect. 2006, 114, 1489–1496. [Google Scholar] [CrossRef]
- Niu, Y.; Cai, J.; Xia, Y.; Yu, H.; Chen, R.; Lin, Z.; Liu, C.; Chen, C.; Wang, W.; Peng, L.; et al. Estimation of personal ozone exposure using ambient concentrations and influencing factors. Environ. Int. 2018, 117, 237–242. [Google Scholar] [CrossRef]
- Karakatsani, A.; Samoli, E.; Rodopoulou, S.; Dimakopoulou, K.; Papakosta, D.; Spyratos, D.; Grivas, G.; Tasi, S.; Angelis, N.; Thirios, A.; et al. Weekly personal ozone exposure and respiratory health in a panel of Greek schoolchildren. Environ. Health Perspect. 2017, 125, 077016. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Zhang, W.; Liu, S.; Wang, W.; Ji, X.; Zhao, Y.; Shima, M.; Yoda, Y.; Yang, D.; Huang, J.; et al. Cardiorespiratory effects of indoor ozone exposure during sleep and the influencing factors: A prospective study among adults in China. Sci. Total Environ. 2024, 924, 171561. [Google Scholar] [CrossRef] [PubMed]
- Stergiopoulou, A.; Katavoutas, G.; Samoli, E.; Dimakopoulou, K.; Papageorgiou, I.; Karagianni, P.; Flocas, H.; Katsouyanni, K. Assessing the associations of daily respiratory symptoms and lung function in schoolchildren using an Air Quality Index for ozone: Results from the RESPOZE panel study in Athens, Greece. Sci. Total Environ. 2018, 633, 492–499. [Google Scholar] [CrossRef] [PubMed]
- Sakellaris, I.; Saraga, D.; Mandin, C.; de Kluizenaar, Y.; Fossati, S.; Spinazze, A.; Cattaneo, A.; Mihucz, V.; Szigeti, T.; de Oliveira Fernandes, E.; et al. Association of subjective health symptoms with indoor air quality in European office buildings: The OFFICAIR project. Indoor Air 2021, 31, 426–439. [Google Scholar] [CrossRef]
- Samoli, E.; Dimakopoulou, K.; Evangelopoulos, D.; Rodopoulou, S.; Karakatsani, A.; Veneti, L.; Sionidou, M.; Tsolakoglou, I.; Krasanaki, I.; Grivas, G.; et al. Is daily exposure to ozone associated with respiratory morbidity and lung function in a representative sample of schoolchildren? Results from a panel study in Greece. J. Expo. Sci. Environ. Epidemiol. 2017, 27, 346–351. [Google Scholar] [CrossRef]
- Kim, C.S.; Alexis, N.E.; Rappold, A.G.; Kehrl, H.; Hazucha, M.J.; Lay, J.C.; Schmitt, M.T.; Case, M.; Devlin, R.B.; Peden, D.B.; et al. Lung function and inflammatory responses in healthy young adults exposed to 0.06 ppm ozone for 6.6 hours. Am. J. Respir. Crit. Care Med. 2011, 183, 1215–1221. [Google Scholar] [CrossRef]
- Ong, C.B.; Kumagai, K.; Brooks, P.T.; Brandenberger, C.; Lewandowski, R.P.; Jackson-Humbles, D.N.; Nault, R.; Zacharewski, T.R.; Wagner, J.G.; Harkema, J.R. Ozone-induced type 2 immunity in nasal airways. development and lymphoid cell dependence in mice. Am. J. Respir. Cell Mol. Biol. 2016, 54, 331–340. [Google Scholar] [CrossRef]
- Sun, N.; Niu, Y.; Zhang, R.; Huang, Y.; Wang, J.; Qiu, W.; Zhang, X.; Han, Z.; Bao, J.; Zhu, H.; et al. Ozone inhalation induces exacerbation of eosinophilic airway inflammation and Th2-skew immune response in a rat model of AR. Biomed. Pharmacother. 2021, 137, 111261. [Google Scholar] [CrossRef]
- Sun, N.; Huang, Y.; Zhang, X.; Niu, Y.; Duan, Y.; Kan, H.; Zhang, R. Involvements of Nrf2 and oxidative stress in the ozone-elicited exacerbation in an allergic rhinitis model. Ecotoxicol. Environ. Saf. 2023, 255, 114822. [Google Scholar] [CrossRef]
- Li, H.; Wu, S.; Pan, L.; Xu, J.; Shan, J.; Yang, X.; Dong, W.; Deng, F.; Chen, Y.; Shima, M.; et al. Short-term effects of various ozone metrics on cardiopulmonary function in chronic obstructive pulmonary disease patients: Results from a panel study in Beijing, China. Environ. Pollut. 2018, 232, 358–366. [Google Scholar] [CrossRef] [PubMed]
- Pan, Z.; Han, X.; Cao, M.; Guo, J.; Huang, D.; Sun, W.; Mi, J.; Liu, Y.; Xue, T.; Guan, T. Short-term exposure to ozone and ECG abnormalities in China: A nationwide longitudinal study. J. Hazard. Mater. 2023, 459, 132290. [Google Scholar] [CrossRef]
- Yang, C.; Yang, H.; Guo, S.; Wang, Z.; Xu, X.; Duan, X.; Kan, H. Alternative ozone metrics and daily mortality in Suzhou: The China Air Pollution and Health Effects Study (CAPES). Sci. Total Environ. 2012, 426, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Weschler, C.J. Ozone in indoor environments: Concentration and chemistry. Indoor Air 2000, 10, 269–288. [Google Scholar] [CrossRef]
- Ferris, B.G. Epidemiology Standardization Project (American Thoracic Society). Am. Rev. Respir. Dis. 1978, 118, 1–120. [Google Scholar]
- Molenberghs, G.; Verbeke, G. A review on linear mixed models for longitudinal data, possibly subject to dropout. Stat. Model. 2001, 1, 235–269. [Google Scholar] [CrossRef]
- Niu, Y.; Chen, R.; Xia, Y.; Cai, J.; Lin, Z.; Liu, C.; Chen, C.; Peng, L.; Zhao, Z.; Zhou, W.; et al. Personal ozone exposure and respiratory inflammatory response: The role of DNA methylation in the arginase-nitric oxide synthase pathway. Environ. Sci. Technol. 2018, 52, 8785–8791. [Google Scholar] [CrossRef]
- Yoda, Y.; Takagi, H.; Wakamatsu, J.; Ito, T.; Nakatsubo, R.; Horie, Y.; Hiraki, T.; Shima, M. Stronger association between particulate air pollution and pulmonary function among healthy students in fall than in spring. Sci. Total Environ. 2019, 675, 483–489. [Google Scholar] [CrossRef]
- Nassikas, N.J.; Luttmann-Gibson, H.; Rifas-Shiman, S.L.; Oken, E.; Gold, D.R.; Rice, M.B. Acute exposure to pollen and airway inflammation in adolescents. Pediatr. Pulmonol. 2024, 59, 1313–1320. [Google Scholar] [CrossRef]
- Okamoto, Y.; Horiguchi, S.; Yamamoto, H.; Yonekura, S.; Hanazawa, T. Present situation of cedar pollinosis in Japan and its immune responses. Allergol. Int. 2009, 58, 155–162. [Google Scholar] [CrossRef]
| Male (n = 24) | Female (n = 15) | Total (n = 39) | |
|---|---|---|---|
| Age (years), mean (SD) | 16.1 (0.3) | 16.1 (0.3) | 16.1 (0.3) |
| History of pollinosis and/or allergic rhinitis, n (%) | 17 (70.8) | 8 (53.3) | 25 (64.1) |
| Response to questionnaire on daily symptoms | n = 683 | n = 434 | n = 1117 |
| Sneeze (%) | 7.0 | 8.5 | 7.6 |
| Runny nose (%) | 11.6 | 11.1 | 11.4 |
| Nasal congestion (%) | 7.6 | 8.5 | 8.0 |
| Cough (%) | 2.5 | 2.8 | 2.6 |
| Dyspnea (%) | 2.6 | 0.7 | 1.9 |
| Mean | SD | Percentile | IQR | |||||
|---|---|---|---|---|---|---|---|---|
| Minimum | 25th | Median | 75th | Maximum | ||||
| Outdoor | ||||||||
| O3 1 h maximum, ppb | 141.5 | 57.2 | 49.4 | 107.4 | 141.6 | 177.8 | 290.4 | 70.4 |
| O3 Maximum 8 h average, ppb | 82.2 | 37.0 | 7.3 | 56.9 | 76.4 | 112.4 | 152.8 | 55.6 |
| O3 24 h average, ppb | 45.4 | 20.1 | 3.1 | 33.3 | 46.2 | 62.6 | 75.0 | 29.3 |
| Temperature, °C | 22.6 | 1.9 | 18.4 | 21.0 | 22.4 | 24.4 | 26.0 | 3.4 |
| Relative humidity, % | 57.6 | 10.0 | 44.2 | 50.4 | 54.1 | 62.5 | 80.2 | 12.1 |
| PM2.5 24 h average, μg/m3 | 9.1 | 3.5 | 3.2 | 7.0 | 8.7 | 10.8 | 18.9 | 3.8 |
| NO2 24 h average, ppb | 4.3 | 1.9 | 1.3 | 3.1 | 3.7 | 5.0 | 8.2 | 1.9 |
| Indoor | ||||||||
| O3 1 h maximum, ppb | 98.6 | 45.7 | 24.6 | 60.7 | 88.7 | 141.1 | 197.2 | 80.4 |
| O3 Maximum 8 h average, ppb | 66.8 | 30.1 | 12.4 | 42.2 | 73.5 | 84.4 | 128.4 | 42.2 |
| O3 24 h average, ppb | 44.4 | 20.4 | 9.5 | 27.5 | 44.0 | 56.8 | 89.7 | 29.3 |
| Temperature, °C | 26.3 | 2.3 | 23.0 | 24.1 | 26.1 | 28.1 | 30.1 | 4.0 |
| Relative humidity, % | 47.7 | 8.7 | 36.9 | 41.6 | 44.4 | 51.3 | 71.7 | 9.7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoda, Y.; Ito, T.; Wakamatsu, J.; Masuzaki, T.; Shima, M. Short-Term Effects of Exposure to Atmospheric Ozone on the Nasal and Respiratory Symptoms in Adolescents. Toxics 2025, 13, 196. https://doi.org/10.3390/toxics13030196
Yoda Y, Ito T, Wakamatsu J, Masuzaki T, Shima M. Short-Term Effects of Exposure to Atmospheric Ozone on the Nasal and Respiratory Symptoms in Adolescents. Toxics. 2025; 13(3):196. https://doi.org/10.3390/toxics13030196
Chicago/Turabian StyleYoda, Yoshiko, Takeshi Ito, Junko Wakamatsu, Tomonari Masuzaki, and Masayuki Shima. 2025. "Short-Term Effects of Exposure to Atmospheric Ozone on the Nasal and Respiratory Symptoms in Adolescents" Toxics 13, no. 3: 196. https://doi.org/10.3390/toxics13030196
APA StyleYoda, Y., Ito, T., Wakamatsu, J., Masuzaki, T., & Shima, M. (2025). Short-Term Effects of Exposure to Atmospheric Ozone on the Nasal and Respiratory Symptoms in Adolescents. Toxics, 13(3), 196. https://doi.org/10.3390/toxics13030196








