Assessing the Acute Toxicological Effects of Annona muricata Leaf Ethanol Extract on Rats: Biochemical, Histopathological, and Metabolomics Analyses
Abstract
1. Introduction
2. Materials and Methods
2.1. Drugs and Chemicals
2.2. Plant Extract Preparation
2.3. Phytochemical Analysis
2.3.1. Flavonoids Test
2.3.2. Alkaloids Test
2.3.3. Saponins Test
2.3.4. Tannins Test
2.3.5. Steroids Test
2.3.6. Carbohydrate Test
2.4. Animal Experimental Analysis
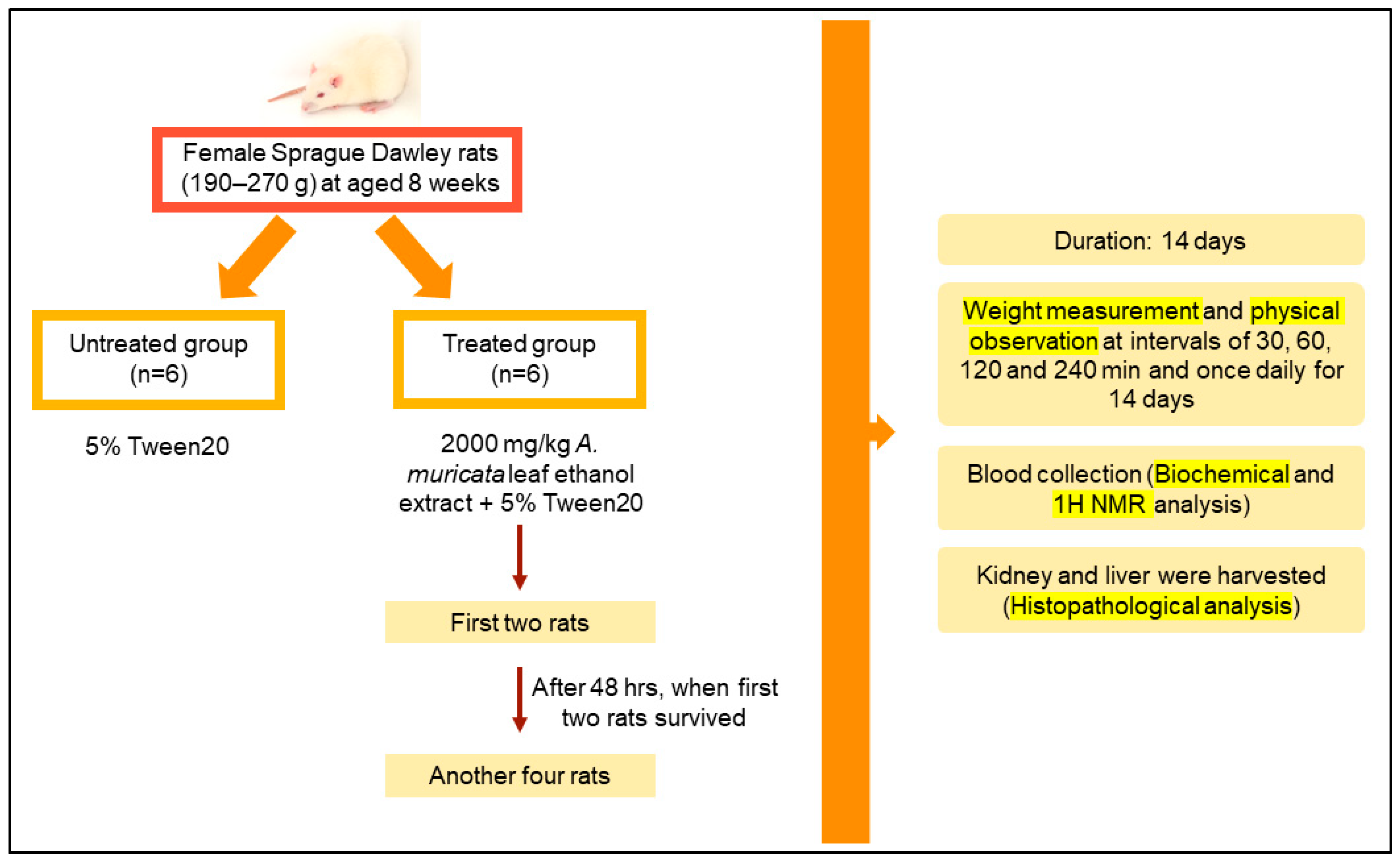
2.5. Acute Oral Toxicity Study
2.6. Biochemical Analysis
2.7. Histopathological Analysis
2.8. Serum and Urine Sample Preparation and 1H NMR Acquisition and Processing
2.9. Statistical Analysis
3. Results
3.1. Phytochemical Analysis
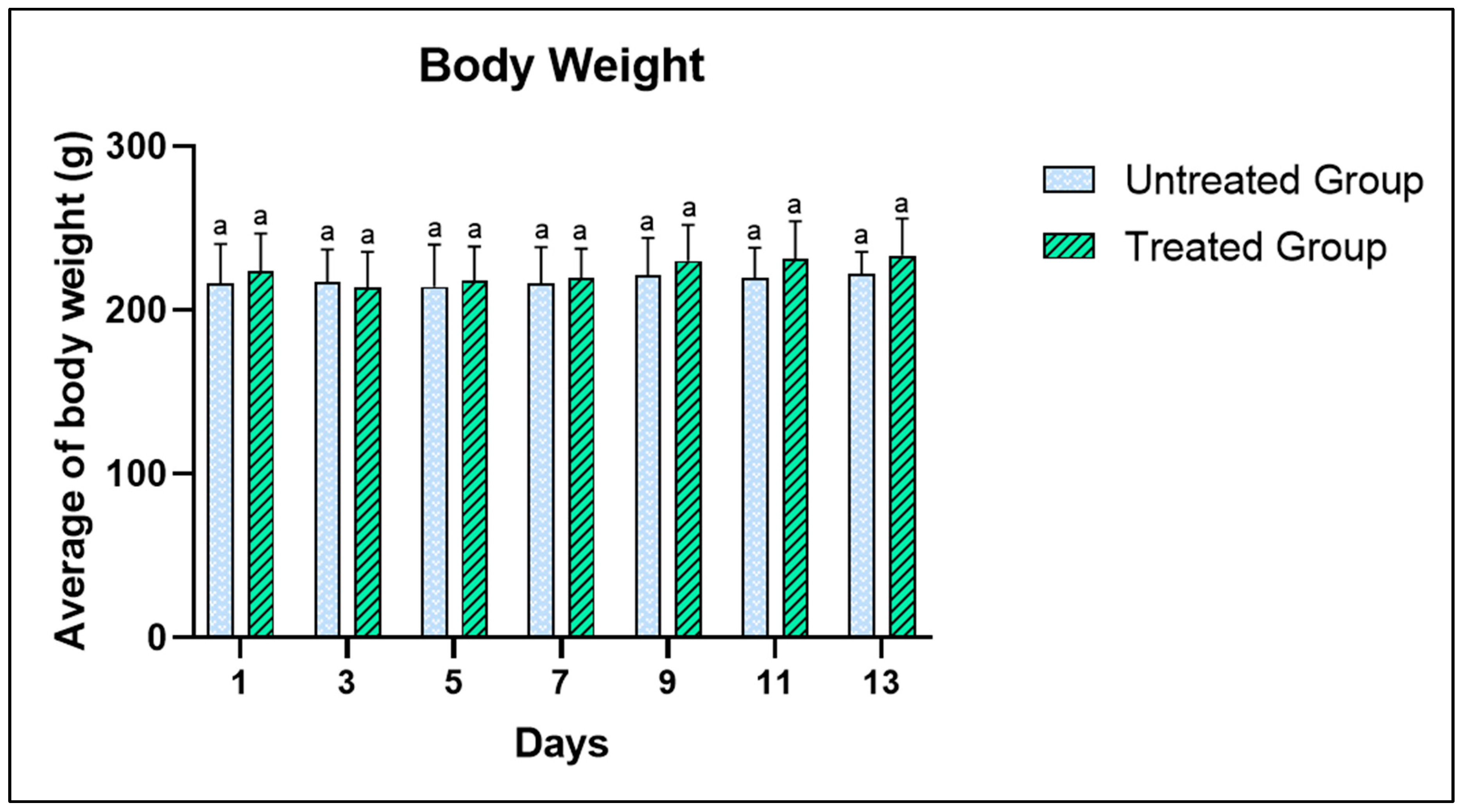
3.2. Acute Toxicity Test-Related Physical and Behavioral Changes
3.3. Biochemical Analysis
3.4. Histopathological Analysis
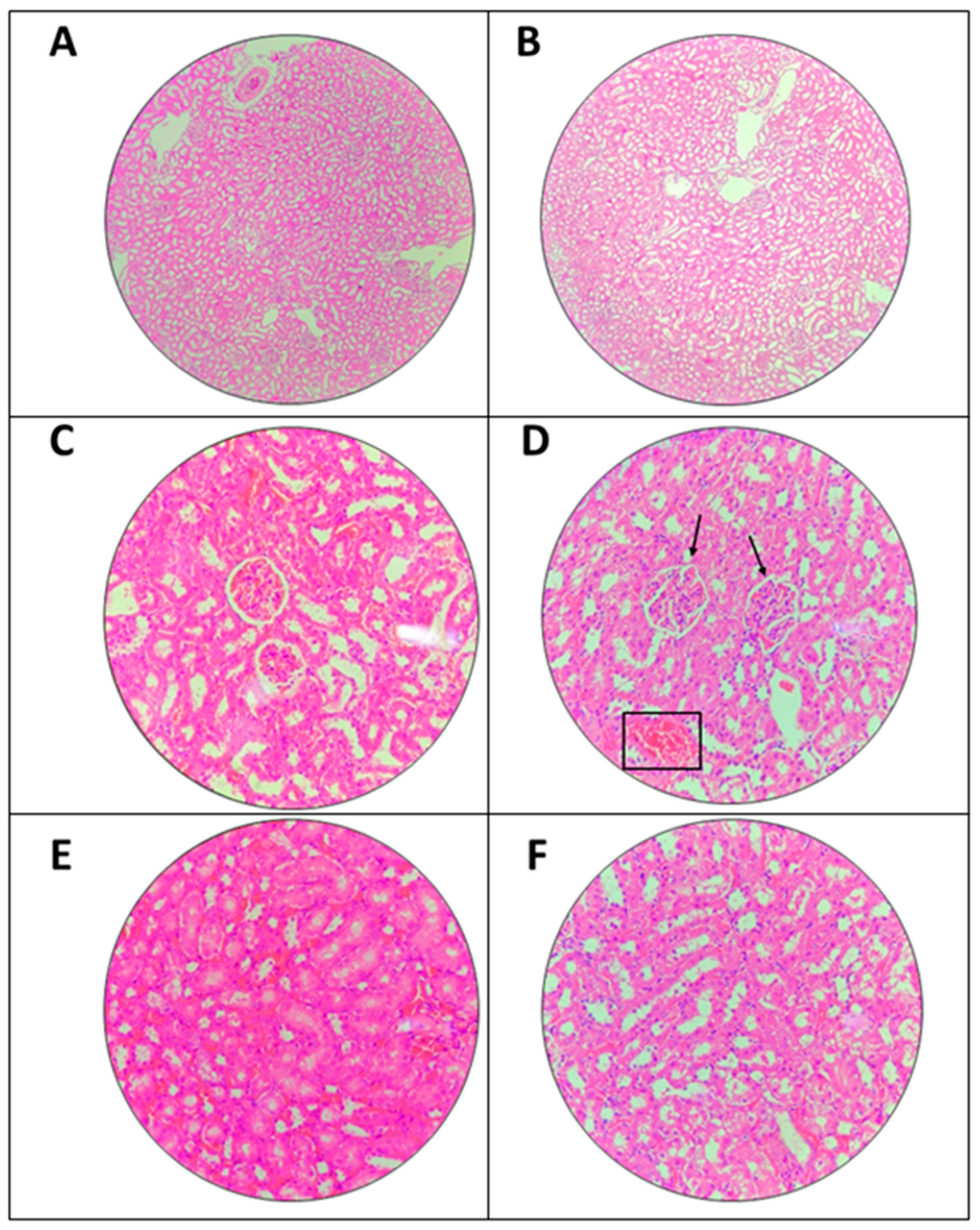
3.4.1. Effects of The Extract on Kidney
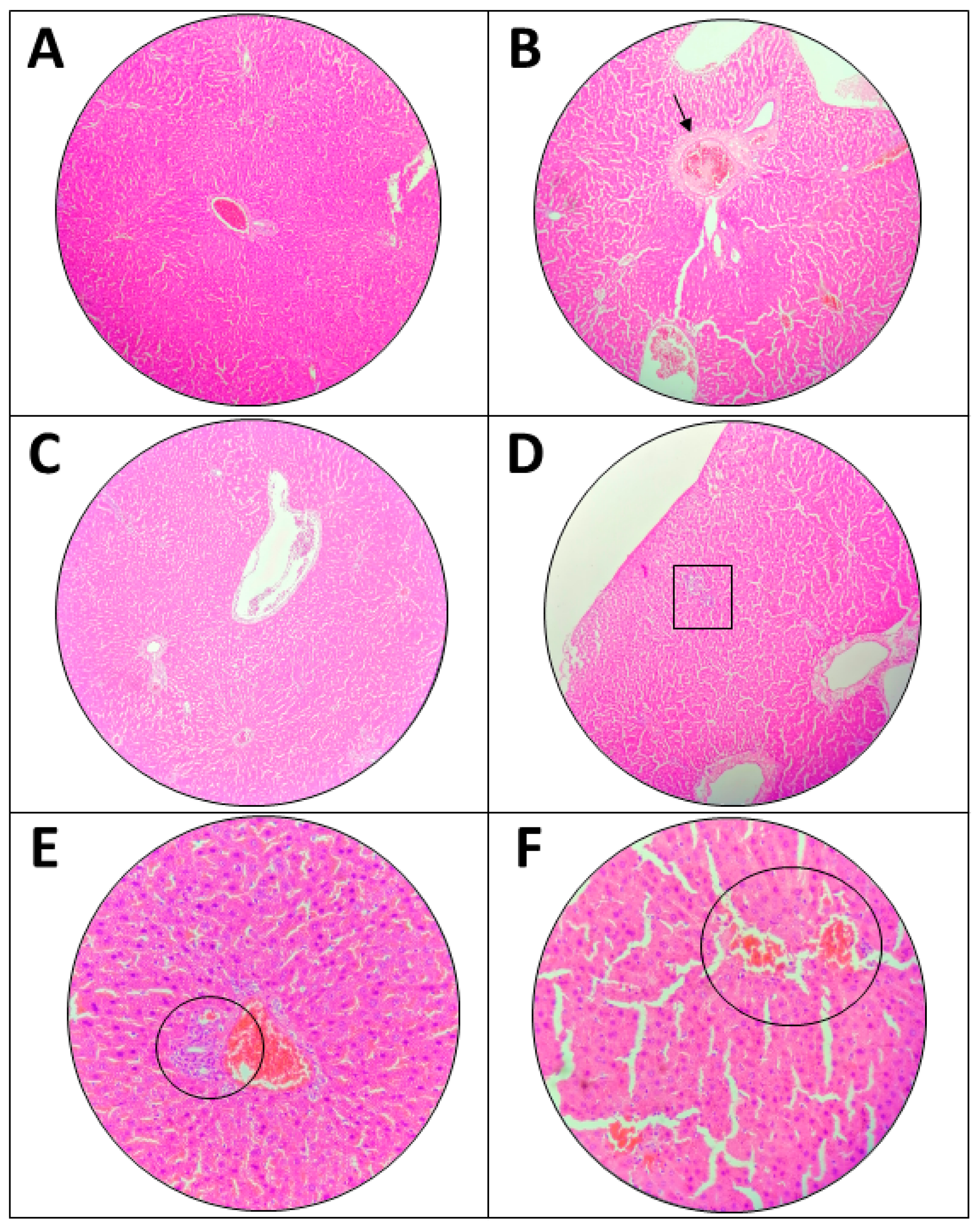
3.4.2. Effects of the Extract on Liver
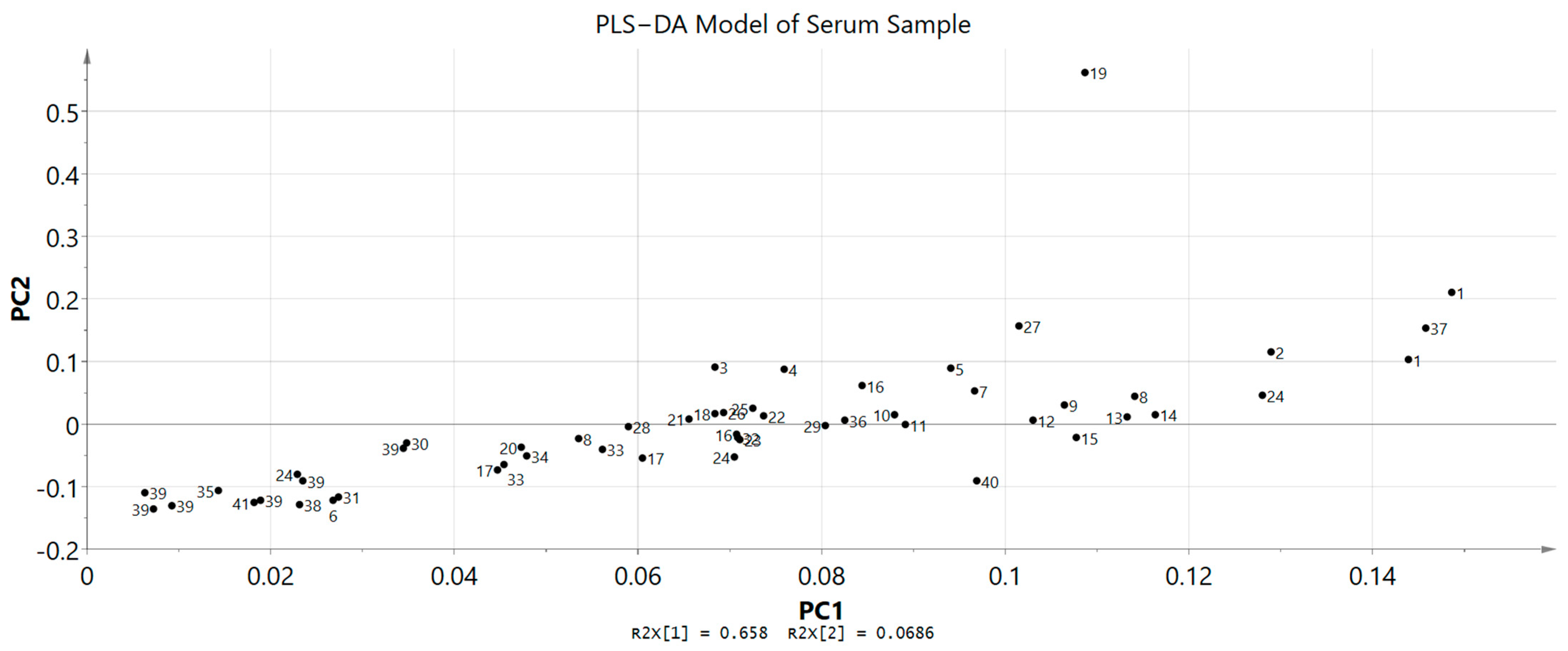
3.4.3. H NMR Serum Metabolomics Evaluation
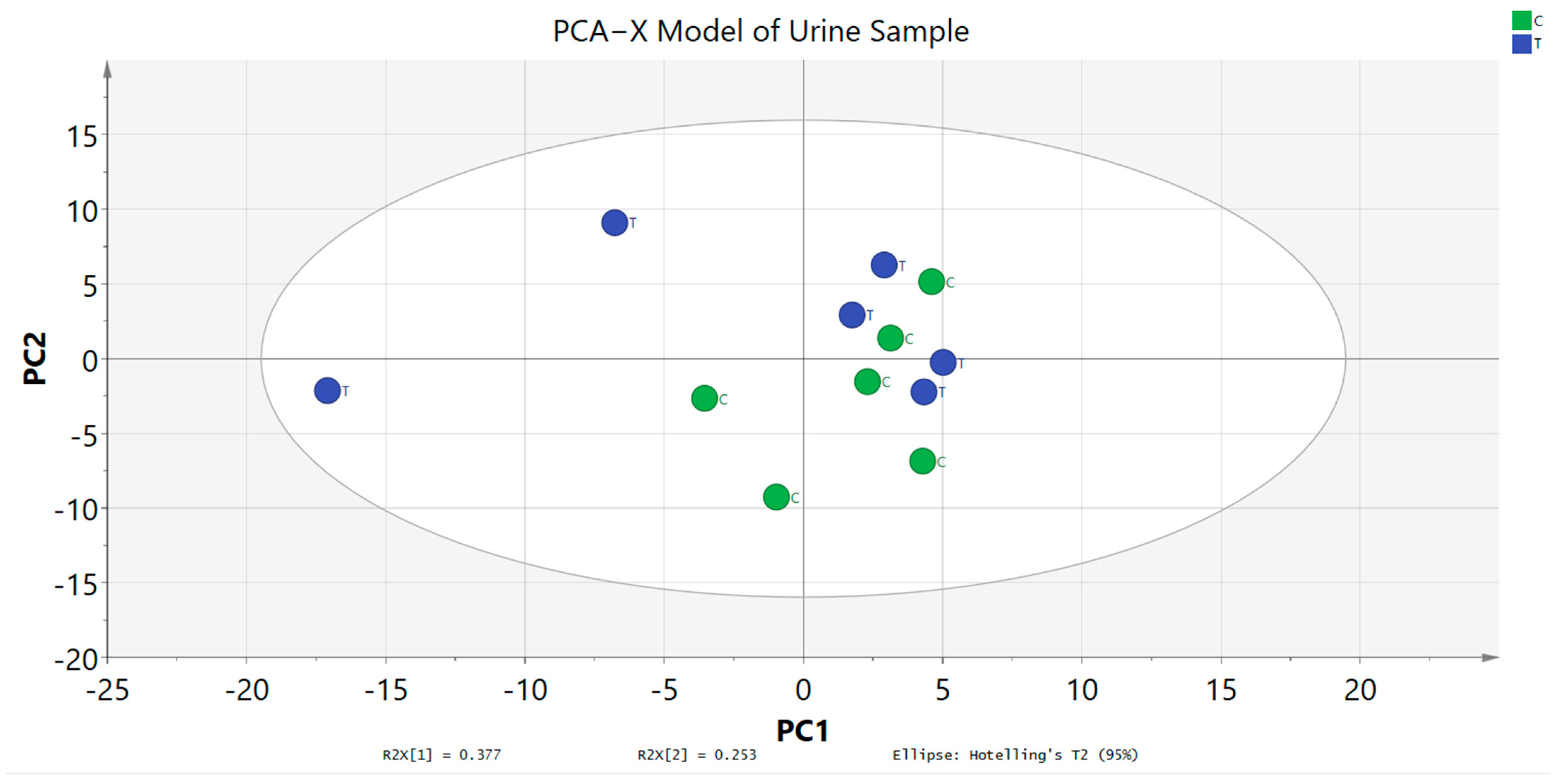
3.5. 1H NMR Urinary Metabolomics Evaluation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arthur, F.; Larbie, C.; Woode, E. Evaluation of Acute and Subchronic Toxicity of Annona muricata (Linn.) Aqueous Extract in Animals. Artic. Eur. J. Exp. Biol. Eur. J. Exp. Biol. 2011, 1, 115–124. [Google Scholar]
- Ekor, M. The Growing Use of Herbal Medicines: Issues Relating to Adverse Reactions and Challenges in Monitoring Safety. Front. Neurol. 2014, 4, 177. [Google Scholar] [CrossRef]
- Zubaidi, S.N.; Nani, H.M.; Saleh, M.; Kamal, A.; Qayyum, T.A.; Maarof, S.; Afzan, A.; Misnan, N.M.; Hamezah, H.S. Annona muricata: Comprehensive Review on the Ethnomedicinal, Phytochemistry, and Pharmacological Aspects Focusing on Antidiabetic Properties. Life 2023, 13, 353. [Google Scholar] [CrossRef] [PubMed]
- Coria-Téllez, A.V.; Montalvo-Gónzalez, E.; Yahia, E.M.; Obledo-Vázquez, E.N. Annona muricata: A Comprehensive Review on Its Traditional Medicinal Uses, Phytochemicals, Pharmacological Activities, Mechanisms of Action and Toxicity. Arab. J. Chem. 2018, 11, 662–691. [Google Scholar] [CrossRef]
- Wahab, S.M.A.; Jantan, I.; Haque, M.A.; Arshad, L. Exploring the Leaves of Annona muricata L. as a Source of Potential Anti-Inflammatory and Anticancer Agents. Front. Pharmacol. 2018, 9, 661. [Google Scholar] [CrossRef] [PubMed]
- Gyesi, J.N.; Opoku, R.; Borquaye, L.S. Chemical Composition, Total Phenolic Content, and Antioxidant Activities of the Essential Oils of the Leaves and Fruit Pulp of Annona muricata L. (Soursop) from Ghana. Biochem. Res. Int. 2019, 2019, 4164576. [Google Scholar] [CrossRef]
- Kasole, R.; Martin, H.D.; Kimiywe, J. Traditional medicine and its role in the management of diabetes mellitus:“patients’ and herbalists’ perspectives”. Evid. Based Complement. Altern. Med. 2019, 2019, 2835691. [Google Scholar] [CrossRef]
- Ferreira, G.G.; Quaresma, A.C.S.; Brandão, D.L.D.N.; Marinho, A.M.D.R.; Siqueira, J.E.D.S.; Correa, K.L.; Silva-Júnior, J.O.C.; Percario, S.; Dolabela, M.F. Evaluation of Genotoxicity and Toxicity of Annona muricata L. Seeds and In Silico Studies. Molecules 2023, 28, 231. [Google Scholar] [CrossRef]
- OECD. Test No. 425: Acute Oral Toxicity: Up-and-Down Procedure. In Oecd Guidelines for the Testing of Chemicals; OECD Publishing: Paris, France, 2004; pp. 1–15. [Google Scholar] [CrossRef]
- Chen, D.Q.; Chen, H.; Chen, L.; Tang, D.D.; Miao, H.; Zhao, Y.Y. Metabolomic Application in Toxicity Evaluation and Toxicological Biomarker Identification of Natural Product. Chem. Biol. Interact. 2016, 252, 114–130. [Google Scholar] [CrossRef]
- Arpornchayanon, W.; Subhawa, S.; Jaijoy, K.; Lertprasertsuk, N.; Soonthornchareonnon, N.; Sireeratawong, S. Safety of the Oral Triphala Recipe from Acute and Chronic Toxicity Tests in Sprague-Dawley Rats. Toxics 2022, 10, 514. [Google Scholar] [CrossRef]
- Haslauer, K.E.; Hemmler, D.; Schmitt-Kopplin, P.; Heinzmann, S.S. Guidelines for the Use of Deuterium Oxide (D2O) in 1H NMR Metabolomics. Anal. Chem. 2019, 91, 11063–11069. [Google Scholar] [CrossRef]
- Dolan, J.W. When Should an Internal Standard Be Used? Available online: https://www.chromatographyonline.com/view/when-should-internal-standard-be-used-0 (accessed on 20 May 2023).
- Mediani, A.; Abas, F.; Maulidiani, M.; Khatib, A.; Tan, C.P.; Ismail, I.S.; Shaari, K.; Ismail, A.; Lajis, N.H. Metabolic and Biochemical Changes in Streptozotocin Induced Obese-Diabetic Rats Treated with Phyllanthus niruri Extract. J. Pharm. Biomed. Anal. 2016, 128, 302–312. [Google Scholar] [CrossRef]
- Trease, G.E.; Evans, W.C. Trease and Evan’s Textbook of Pharmacognosy; Saunders Publishers: London, UK, 1989; ISBN 9780702029332. [Google Scholar]
- Sherif, H.B.; Baba, G.; Abdullahi, S.M. Acute and Sub- Chronic Toxicity Profile of Annona muricata (Sour Sop) on Wister Albino Rats. Bayero J. Pure Appl. Sci. 2018, 10, 57. [Google Scholar] [CrossRef][Green Version]
- Lipnick, R.L.; Cotruvo, J.A.; Hill, R.N.; Bruce, R.D.; Stitzel, K.A.; Walker, A.P.; Chu, I.; Goddard, M.; Segal, L.; Springer, J.A.; et al. Comparison of the Up-and-down, Conventional LD50, and Fixed-Dose Acute Toxicity Procedures. Food Chem. Toxicol. 1995, 33, 223–231. [Google Scholar] [CrossRef] [PubMed]
- Khoo, L.W.; Kow, A.S.F.; Maulidiani, M.; Lee, M.T.; Tan, C.P.; Shaari, K.; Tham, C.L.; Abas, F. Hematological, Biochemical, Histopathological And 1H-NMR Metabolomics Application in Acute Toxicity Evaluation of Clinacanthus nutans Water Leaf Extract. Molecules 2018, 23, 2172. [Google Scholar] [CrossRef] [PubMed]
- OECD. OECD Test No. 423: Acute Oral Toxicity—Acute Toxic Class Method. In OECD Guidelines for the Testing of Chemicals; OECD Publishing: Paris, France, 2002; Section 4; pp. 1–14. [Google Scholar] [CrossRef]
- Chan, W.J.J.; McLachlan, A.J.; Hanrahan, J.R.; Harnett, J.E. The Safety and Tolerability of Annona muricata Leaf Extract: A Systematic Review. J. Pharm. Pharmacol. 2020, 72, 13182. [Google Scholar] [CrossRef] [PubMed]
- Florence, N.T.; Benoit, M.Z.; Jonas, K.; Alexandra, T.; Désiré, D.D.P.; Pierre, K.; Théophile, D. Antidiabetic and Antioxidant Effects of Annona muricata (Annonaceae), Aqueous Extract on Streptozotocin-Induced Diabetic Rats. J. Ethnopharmacol. 2014, 151, 784–790. [Google Scholar] [CrossRef]
- Oliveira Souza, D.; dos Santos Sales, V.; Kelly de Souza Rodrigues, C.; Rolim de Oliveira, L.; Cristina Santiago Lemos, I.; de Araújo Delmondes, G.; Brito Monteiro, Á.; Petícia do Nascimento, E.; Rodolpho Sobreira Dantas Nóbrega de Figuêiredo, F.; Galberto Martins da Costa, J.; et al. Phytochemical Analysis and Central Effects of Annona muricata Linnaeus: Possible Involvement of the Gabaergic and Monoaminergic Systems. Iran. J. Pharm. Res. 2018, 17, 1306–1317. [Google Scholar]
- Adewole, S.O.; Ojewole, J.A.O. Protective Effects of Annona muricata Linn. (Annonaceae) Leaf Aqueous Extract on Serum Lipid Profiles and Oxidative Stress in Hepatocytes of Streptozotocin-Treated Diabetic Rats. African J. Tradit. Complement. Altern. Med. 2009, 6, 30–41. [Google Scholar] [CrossRef]
- Vilaanueva, A.B.; Ferrer, D.A.; Civeira, M.E.; Gutierrez, C.I.; Laguna, C.M.; Cerrada, L.E. Methanol Poisoning. Med. Intensiva 2002, 26, 264–266. [Google Scholar]
- Gema, M.-O.; Marlon, R.-L.; Joel, D.-R.; Fátima, R.-C.F.D.; Silvia, L.-S. Effect of Ethanol and Methanol on the Total Phenolic Content and Antioxidant Capacity of Chia Seeds (Salvia Hispanica L.). Sains Malaysiana 2020, 49, 1283–1292. [Google Scholar] [CrossRef]
- Gavamukulya, Y.; Abou-Elella, F.; Wamunyokoli, F.; AEl-Shemy, H. Phytochemical Screening, Anti-Oxidant Activity and in Vitro Anticancer Potential of Ethanolic and Water Leaves Extracts of Annona muricata (Graviola). Asian Pac. J. Trop. Med. 2014, 7, S355–S363. [Google Scholar] [CrossRef] [PubMed]
- Acésio, N.O.; Carrijo, G.S.; Batista, T.H.; Damasceno, J.L.; Côrrea, M.B.; Tozatti, M.G.; Cunha, W.R.; Tavares, D.C. Assessment of the Antioxidant, Cytotoxic, and Genotoxic Potential of the Annona muricata Leaves and Their Influence on Genomic Stability. J. Toxicol. Environ. Health Part A Curr. Issues 2017, 80, 1290–1300. [Google Scholar] [CrossRef]
- Bantel, H.; Lügering, A.; Heidemann, J.; Volkmann, X.; Poremba, C.; Strassburg, C.P.; Manns, M.P.; Schulze-Osthoff, K. Detection of Apoptotic Caspase Activation in Sera from Patients with Chronic HCV Infection Is Associated with Fibrotic Liver Injury. Hepatology 2004, 40, 1078–1087. [Google Scholar] [CrossRef]
- Matsushige, A.; Kotake, Y.; Matsunami, K.; Otsuka, H.; Ohta, S.; Takeda, Y. Annonamine, a New Aporphine Alkaloid from the Leaves of Annona muricata. Chem. Pharm. Bull. 2012, 60, 257–259. [Google Scholar] [CrossRef]
- Fofana, S.; Keita, A.; Balde, S.; Ziyaev, R.; Aripova, S.F. Alkaloids from Leaves of Annona muricata. Chem. Nat. Compd. 2012, 48, 714. [Google Scholar] [CrossRef]
- Kamarul Zaman, M.A.; Mohamad Azzeme, A. Plant Toxins: Alkaloids and Their Toxicities. GSC Biol. Pharm. Sci. 2018, 6, 021–029. [Google Scholar] [CrossRef]
- Opara, P.O.; Enemor, V.H.A.; Eneh, F.U.; Emengaha, F.C. Blood Glucose—Lowering Potentials of Annona muricata Leaf Extract in Alloxan—Induced Diabetic Rats. Eur. J. Biol. Biotechnol. 2021, 2, 106–113. [Google Scholar] [CrossRef]
- Eggadi, V.; Gundamedi, S.; Sheshagiri, S.B.B.; Revoori, S.K.; Jupally, V.R.; Kulandaivelu, U. Evaluation of Anticancer Activity of Annona muricata in 1, 2-Dimethyl Hydrazine Induced Colon Cancer. World Appl. Sci. J. 2014, 32, 444–450. [Google Scholar] [CrossRef]
- Hoekstra, L.T.; De Graaf, W.; Nibourg, G.A.A.; Heger, M.; Bennink, R.J.; Stieger, B.; Van Gulik, T.M. Physiological and Biochemical Basis of Clinical Liver Function Tests: A Review. Ann. Surg. 2013, 257, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Okafor, A.C.; Nonso, E.E.; Obinna, O.K.; Mark, A.D.; Luke, N.M.; Pearl, O.A.; O’Brien, C.J.; Uchenna, A.F.; Ikenna, A.J.; Richard, N.N.; et al. Effect of Methanolic Extract of Carica papaya Seed on Renal Function and Antioxidant Activities Following Ibuprofen-Induced Toxicity on Male Wistar Rats. Free. Radic. Antioxid. 2022, 12, 36–40. [Google Scholar] [CrossRef]
- Gowda, S.; Desai, P.B.; Kulkarni, S.S.; Hull, V.V.; Math, A.A.K.; Vernekar, S.N. Markers of Renal Function Tests. N. Am. J. Med. Sci. 2010, 2, 170–173. [Google Scholar]
- Moghadamtousi, S.Z.; Rouhollahi, E.; Karimian, H.; Fadaeinasab, M.; Abdulla, M.A.; Kadir, H.A. Gastroprotective Activity of Annona muricata Leaves against Ethanol-Induced Gastric Injury in Rats via Hsp70/Bax Involvement. Drug Des. Devel. Ther. 2014, 8, 2099–2111. [Google Scholar] [CrossRef]
- Radi, Z.A. Kidney Pathophysiology, Toxicology, and Drug-Induced Injury in Drug Development. Int. J. Toxicol. 2019, 38, 215–227. [Google Scholar] [CrossRef] [PubMed]
- Alarifi, S.; Al-Doaiss, A.; Alkahtani, S.; Al-Farraj, S.A.; Al-Eissa, M.S.; Al-Dahmash, B.; Al-Yahya, H.; Mubarak, M. Blood Chemical Changes and Renal Histological Alterations Induced by Gentamicin in Rats. Saudi J. Biol. Sci. 2012, 19, 103–110. [Google Scholar] [CrossRef]
- Almansour, M.; Jarrar, Q.; Battah, A.; Obeidat, F.; Battah, K.; Jarrar, B. Renal Histopathological Alterations Induced by Nanosilver Toxicity: The Size Effect. Micro Nano Lett. 2016, 11, 862–865. [Google Scholar] [CrossRef]
- Wang, X.; Rezeng, C.; Wang, Y.; Li, J.; Zhang, L.; Chen, J.; Li, Z. Toxicological Risks of Renqingchangjue in Rats Evaluated by 1H NMR-Based Serum and Urine Metabolomics Analysis. ACS Omega 2020, 5, 2169–2179. [Google Scholar] [CrossRef] [PubMed]
- Olayode, O.A.; Daniyan, M.O.; Olayiwola, G. Biochemical, Hematological and Histopathological Evaluation of the Toxicity Potential of the Leaf Extract of Stachytarpheta cayennensis in Rats. J. Tradit. Complement. Med. 2020, 10, 544–554. [Google Scholar] [CrossRef] [PubMed]
- Amadi, C.N.; Orisakwe, O.E. Herb-Induced Liver Injuries in Developing Nations: An Update. Toxics 2018, 6, 24. [Google Scholar] [CrossRef]
- Zheng, E.X.; Navarro, V.J. Liver Injury from Herbal, Dietary, and Weight Loss Supplements: A Review. J. Clin. Transl. Hepatol. 2015, 3, 93–98. [Google Scholar] [CrossRef]
- Al-Medhtiy, M.H.; Jabbar, A.A.; Shareef, S.H.; Ibrahim, I.A.A.; Alzahrani, A.R.; Abdulla, M.A. Histopathological Evaluation of Annona muricata in TAA-Induced Liver Injury in Rats. Processes 2022, 10, 1613. [Google Scholar] [CrossRef]
- Bollard, M.E.; Stanley, E.G.; Lindon, J.C.; Nicholson, J.K.; Holmes, E. NMR-Based Metabonomic Approaches for Evaluating Physiological Influences on Biofluid Composition. NMR Biomed. 2005, 18, 143–162. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.M.; Chung, R.T.; Study, A.L.F. Development of an Accurate Index for Predicting outcomes of Patients with Acute Liver Failure. Gastroenterology 2013, 143, 1237–1243. [Google Scholar] [CrossRef]
- Gasmi, B.; Kleiner, D.E. Liver Histology Diagnostic and Prognostic Features. Clin. Liver Dis. 2020, 24, 61–74. [Google Scholar] [CrossRef] [PubMed]
- Baba, G.; Abdullahi, S.M. Sub-Chronic Toxicity Profile Of Annona muricata (Sour Sop) On Wister Albino Rats. Bayero J. Pure Appl. Sci. 2017, 10, 57–63. [Google Scholar]
- Agu, K.; Okolie, N.; Eze, I.; Anionye, J.; Falodun, A. Phytochemical Analysis, Toxicity Profile, and Hemomodulatory Properties of Annona muricata (Soursop). Egypt. J. Haematol. 2017, 42, 36. [Google Scholar] [CrossRef]



| Phytochemicals in A. muricata | Presences |
|---|---|
| Flavonoids | +++ |
| Alkaloids | +++ |
| Saponin | − |
| Tannins | + |
| Steroids | + |
| Triterpenes | + |
| Carbohydrate | +++ |
| Liver Function Test | |||
|---|---|---|---|
| Parameter | Unit | Treatment | |
| Untreated Group | Treated Group | ||
| ALT | U/L | 38.33 ± 8.08 a | 40.00 ± 1.00 a |
| AST | U/L | 130.67 ± 25.15 a | 134.00 ± 9.54 a |
| ALP | U/L | 99.33 ± 12.58 a | 101.00 ± 8.19 a |
| Renal Function Test | |||
|---|---|---|---|
| Parameter | Unit | Treatment | |
| Untreated Group | Treated Group | ||
| Creatinine | µmol/L | 22.50 ± 2.08 a | 25.75 ± 1.50 a |
| Urea | mmol/L | 6.55 ± 0.78 a | 6.39 ± 0.90 a |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zubaidi, S.N.; Qadi, W.S.M.; Maarof, S.; Mohmad Misnan, N.; Mohammad Noor, H.S.; Hamezah, H.S.; Baharum, S.N.; Rosli, N.; Jam, F.A.; Al-Olayan, E.; et al. Assessing the Acute Toxicological Effects of Annona muricata Leaf Ethanol Extract on Rats: Biochemical, Histopathological, and Metabolomics Analyses. Toxics 2023, 11, 688. https://doi.org/10.3390/toxics11080688
Zubaidi SN, Qadi WSM, Maarof S, Mohmad Misnan N, Mohammad Noor HS, Hamezah HS, Baharum SN, Rosli N, Jam FA, Al-Olayan E, et al. Assessing the Acute Toxicological Effects of Annona muricata Leaf Ethanol Extract on Rats: Biochemical, Histopathological, and Metabolomics Analyses. Toxics. 2023; 11(8):688. https://doi.org/10.3390/toxics11080688
Chicago/Turabian StyleZubaidi, Siti Norliyana, Wasim S. M. Qadi, Syahida Maarof, Norazlan Mohmad Misnan, Halimatul Saadiah Mohammad Noor, Hamizah Shahirah Hamezah, Syarul Nataqain Baharum, Nurwahyuna Rosli, Faidruz Azura Jam, Ebtesam Al-Olayan, and et al. 2023. "Assessing the Acute Toxicological Effects of Annona muricata Leaf Ethanol Extract on Rats: Biochemical, Histopathological, and Metabolomics Analyses" Toxics 11, no. 8: 688. https://doi.org/10.3390/toxics11080688
APA StyleZubaidi, S. N., Qadi, W. S. M., Maarof, S., Mohmad Misnan, N., Mohammad Noor, H. S., Hamezah, H. S., Baharum, S. N., Rosli, N., Jam, F. A., Al-Olayan, E., Wang, C., Hellal, K., Buzgaia, N., & Mediani, A. (2023). Assessing the Acute Toxicological Effects of Annona muricata Leaf Ethanol Extract on Rats: Biochemical, Histopathological, and Metabolomics Analyses. Toxics, 11(8), 688. https://doi.org/10.3390/toxics11080688







