Exploration of Maternal and Fetal Toxicity Risks for Metronidazole-Related Teratogenicity and Hepatotoxicity through an Assessment in Albino Rats
Abstract
1. Introduction
2. Materials and Methods
2.1. Metronidazole Drug
2.2. Animal Care and Use
2.3. Determination of the Estrous Cycle
2.4. Mating and Pregnancy Snippets
2.5. Experimental Design
2.6. Narrative Toxicological Signs of Dams
3. Pregnancy Outcomes Evaluation
3.1. Dissection Procedure of Pregnant Rats
3.2. Macroscopical Evaluation
3.2.1. Fetus and Placenta
3.2.2. Blood and Serum Biochemistry
3.2.3. Histopathological Analysis
4. Statistical Analysis
5. Results
5.1. Maternal Toxicity
5.2. Preterm Birth and Abortion
5.3. Maternal Body Weight
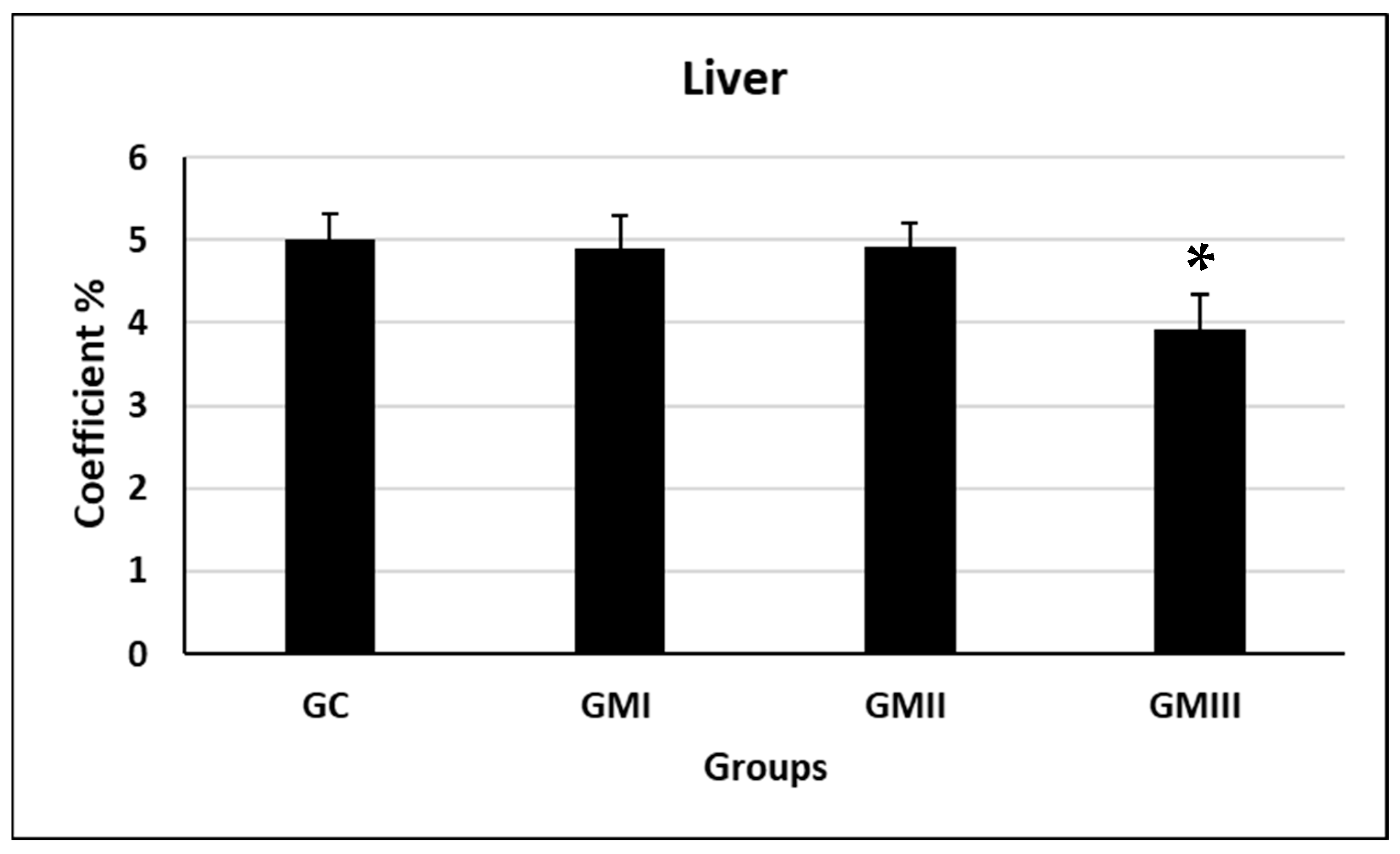
5.4. Liver Coefficients
6. Indices of Pregnancy Outcomes
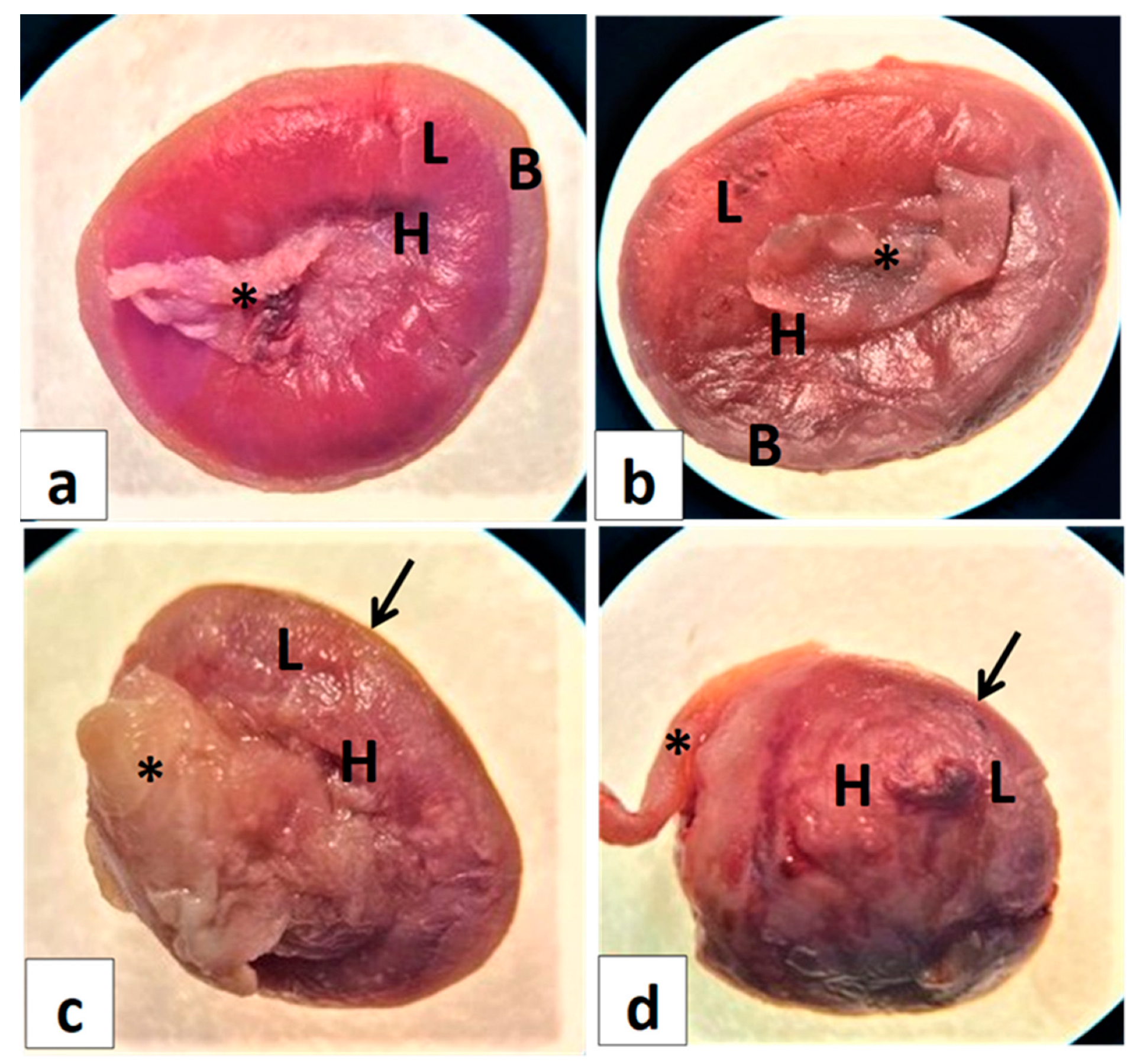
6.1. Gross Gravid Uterine Horns
6.2. Day 0–7 Experiment Findings
6.3. Day 7–14 Experiment Findings
6.4. Day 0–20 Experiment Findings
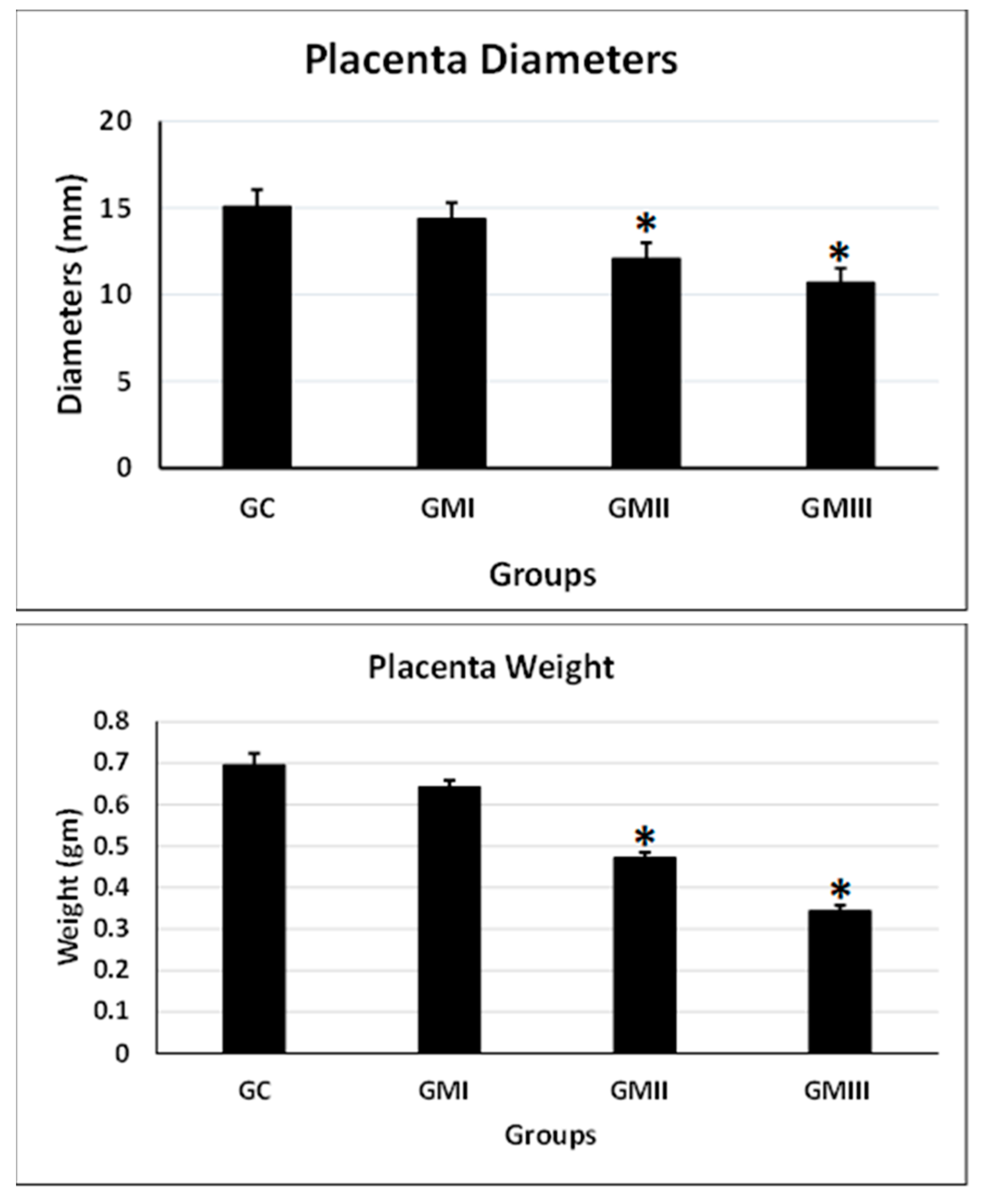
6.5. Placenta Weight and Diameter
6.6. Placental Morphology and Anatomy
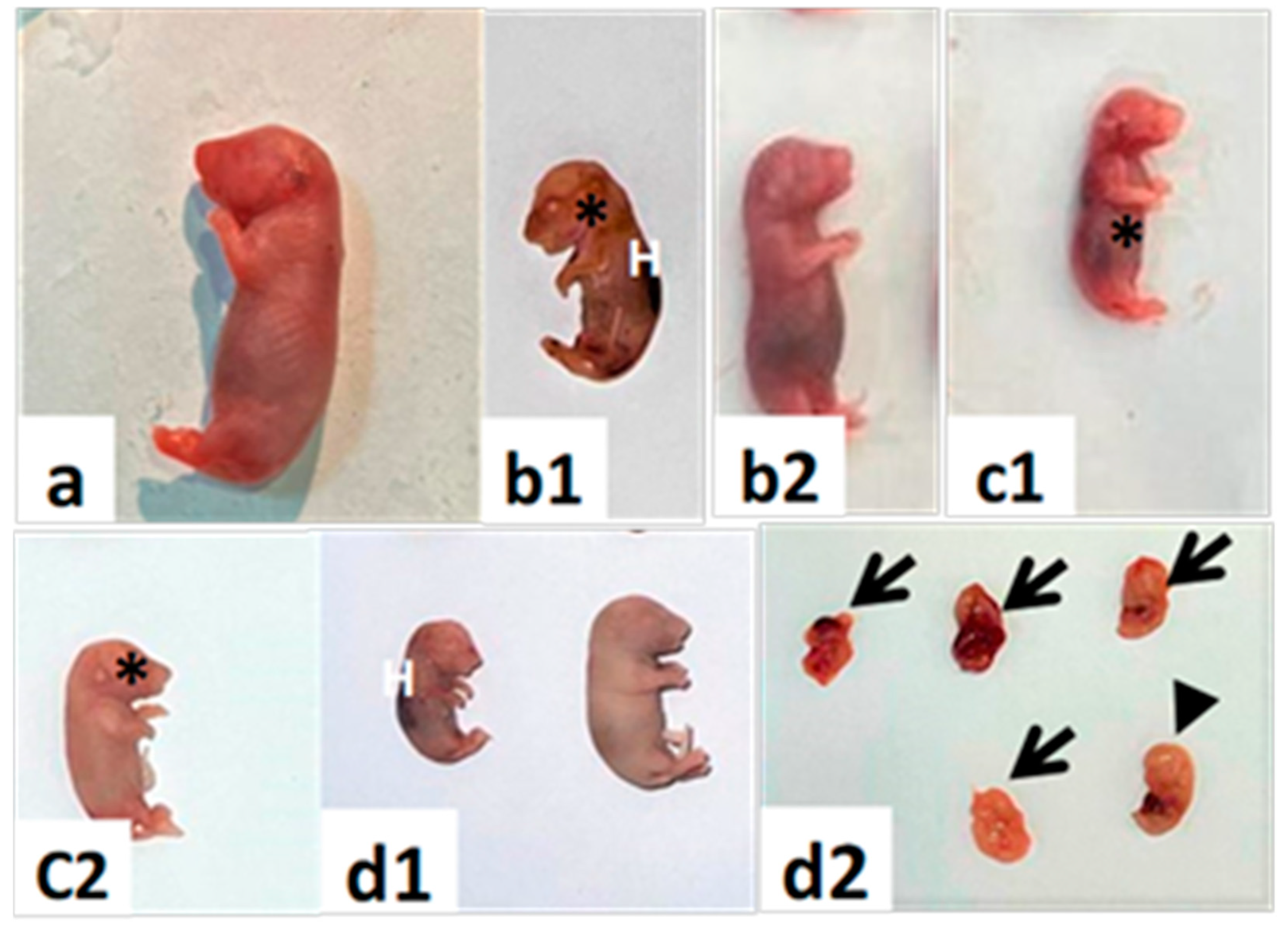
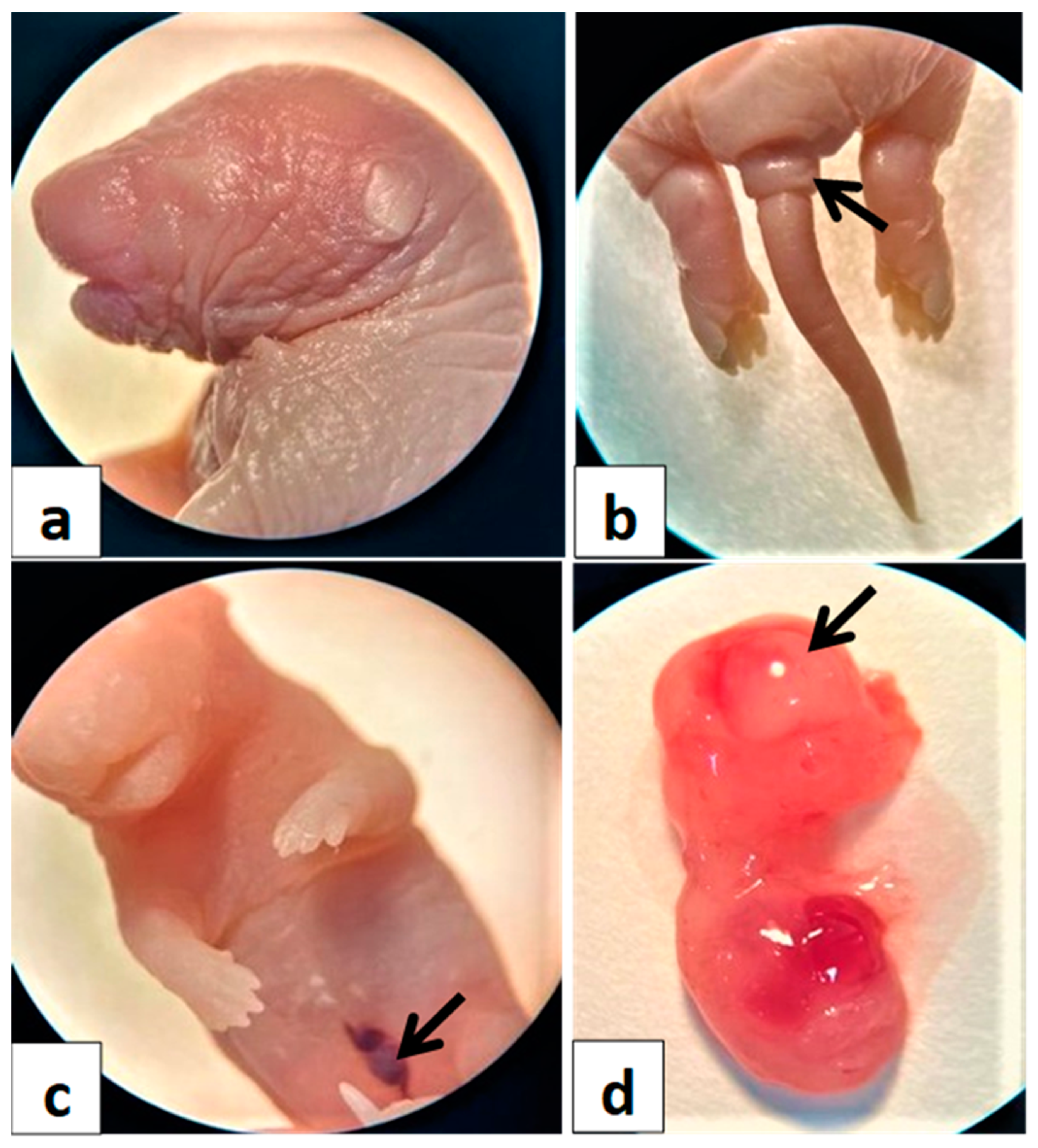
6.7. Gross Morphology of Fetal Abnormalities
6.7.1. Fetal Growth
6.7.2. Major Congenital Anomalies
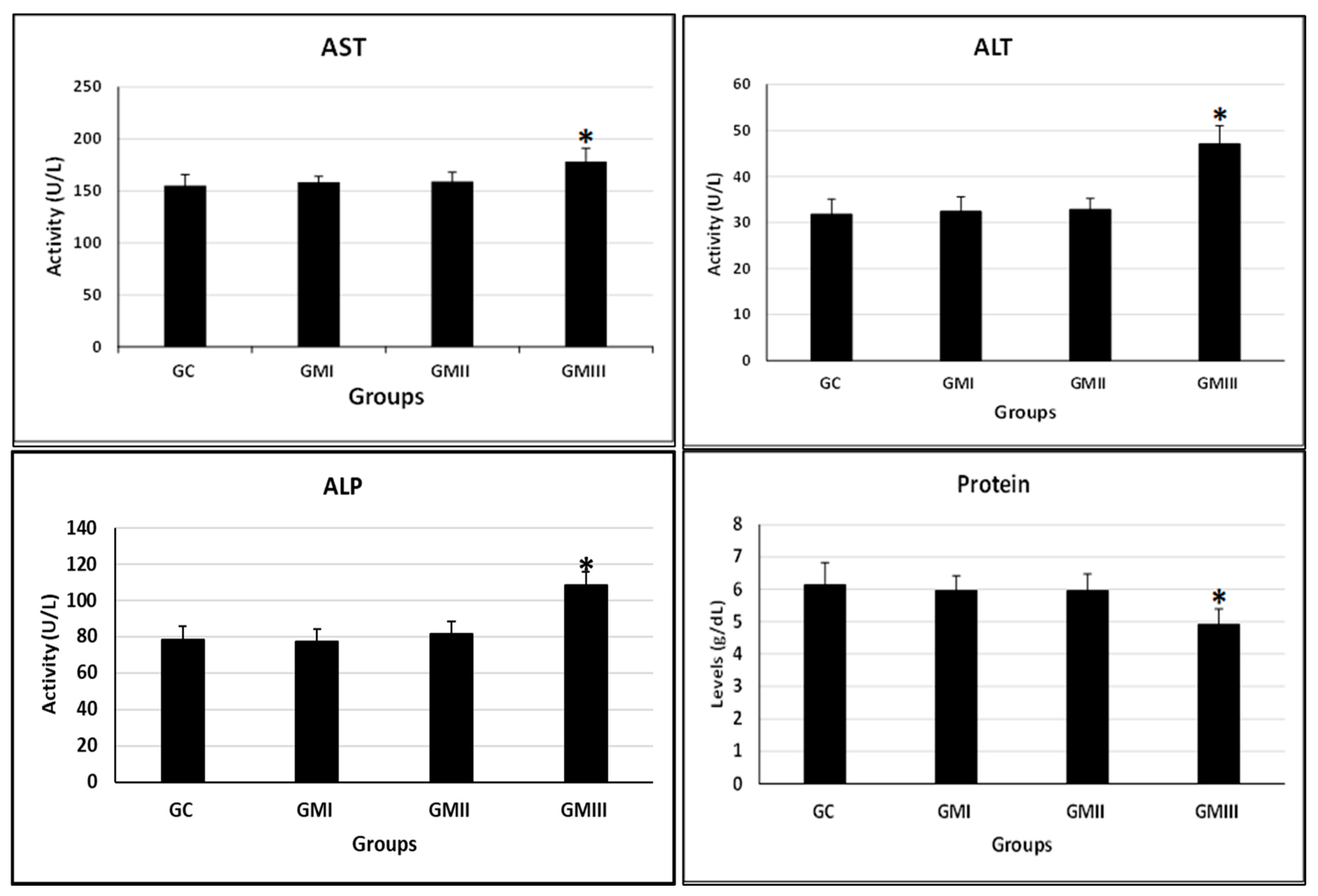
6.7.3. Blood Chemistry
6.8. Hepatic Histopathology
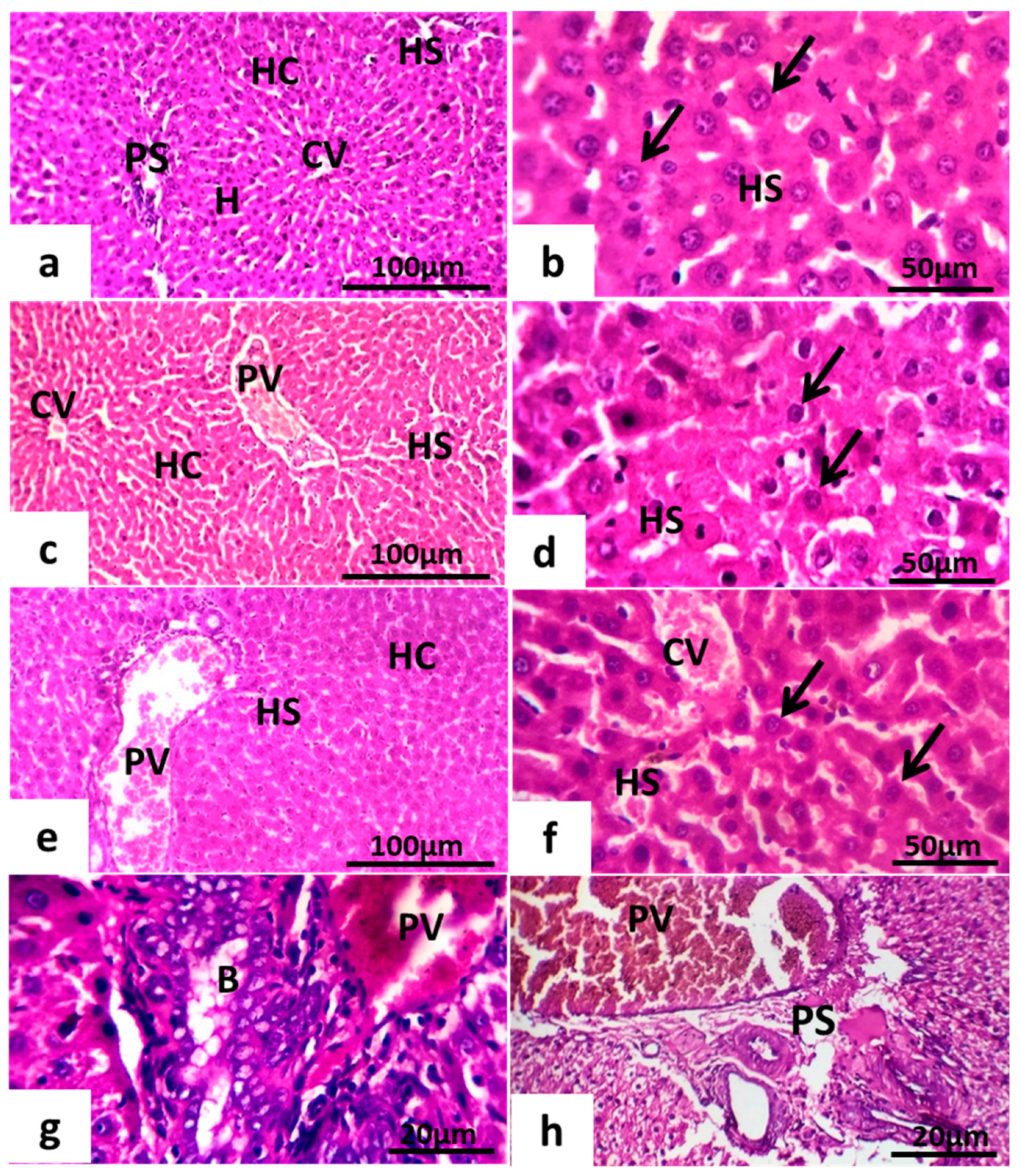
6.8.1. Maternal Hepatotoxicity
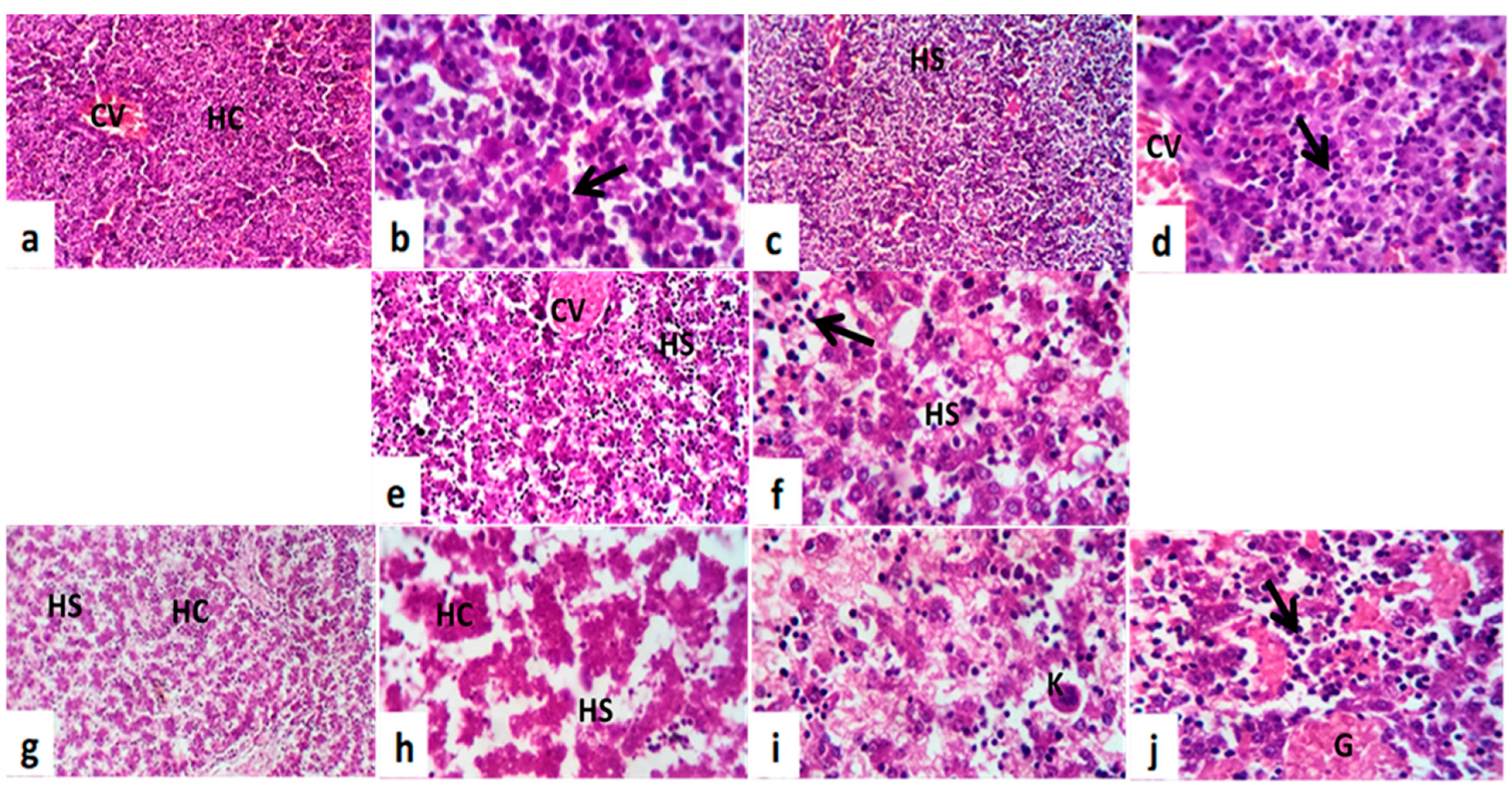
6.8.2. Fetal Hepatotoxicity
7. Discussion
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Telfer, S.M.; Lambin, X.N.; Birtles, R.N.; Beldomenico, P.; Burthe, S.; Paterson, S.F.; Begon, M. Species interactions in a parasite community drive infection risk in a wildlife population. Sci. J. 2010, 330, 243–246. [Google Scholar] [CrossRef]
- da Silva, W.E.; de Melo, I.M.F.; de Albuquerque, Y.M.L.; Mariano, A.F.; Wanderley-Teixeira, V.; Teixeira, Á.A. Effect of metronidazole on placental and fetal development in albino rats. Anim. Reprod. 2019, 16, 810–818. [Google Scholar] [CrossRef] [PubMed]
- Chisolm, M.S.; Payne, J.L. Management of psychotropic drugs during pregnancy. BMJ 2016, 352. [Google Scholar] [CrossRef] [PubMed]
- Abebe, M.; Asres, K.; Bekuretsion, Y.; Woldkidan, S.; Debebe, E.; Seyoum, G. Teratogenic Effect of High Dose of Syzygium guineense (Myrtaceae) Leaves on Wistar Albino Rat Embryos and Fetuses. Evid. Based Complement. Altern. Med. 2021, 2021, 6677395. [Google Scholar] [CrossRef]
- Gupta, R.K.; Gupta, R.C. Placental Toxicity. In Reproductive and Developmental Toxicology; Elsevier: Amsterdam, The Netherlands, 2022; pp. 1373–1397. [Google Scholar]
- Kupc, M.; Paunkov, A.; Strasser, D.; Soki, J.; Leitsch, D. Initial expression levels of nim A are decisive for protection against metronidazole in Bacteroides fragilis. Anaerobe 2022, 77, 102630. [Google Scholar] [CrossRef] [PubMed]
- Adil, M.; Iqbal, W.; Adnan, F.; Wazir, S.; Khan, I.; Khayam, M.U.; Khan, I.N. Association of metronidazole with cancer: A potential risk factor or inconsistent deductions? Curr. Drug Metab. 2018, 19, 902–909. [Google Scholar] [CrossRef]
- Muzny, C.A.; Van Gerwen, O.T.; Kissinger, P. Updates in trichomonas treatment including persistent infection and 5-nitroimidazole hypersensitivity. Curr. Opin. Infect. Dis. 2020, 33, 73–77. [Google Scholar] [CrossRef]
- Bagga, R.; Arora, P. Genital Micro-Organisms in Pregnancy. Front. Public Health 2020, 16, 225. [Google Scholar] [CrossRef]
- Bookstaver, P.B.; Bland, C.M.; Griffin, B.; Stover, K.R.; Eiland, L.S.; McLaughlin, M.A. Review of antibiotic use in pregnancy. Pharmacotherapy: J. Hum. Pharmacol. Drug Ther. 2015, 35, 1052–1062. [Google Scholar] [CrossRef]
- van Schalkwyk, J.; Yudin, M.H. Vulvovaginitis: Screening for and management of trichomoniasis, vulvovaginal candidiasis, and bacterial vaginosis. J. Obstet. Gynaecol. Can. 2015, 37, 266–274. [Google Scholar] [CrossRef]
- Waltmann, A.; McKinnish, T.R.; Duncan, J.A. Nonviral sexually transmitted infections in pregnancy: Current controversies and new challenges. Curr. Opin. Infect. Dis. 2021, 34, 40–49. [Google Scholar] [CrossRef] [PubMed]
- McCarter-Spaulding, D.E. Medications in pregnancy and lactation. MCN Am. J. Matern. Child Nurs. 2005, 30, 10–17. [Google Scholar] [CrossRef]
- Erdemli, M.; Turkoz, Y.; Altinoz, E.; Elibol, E.; Dogan, Z. Investigation of the effects of acrylamide applied during pregnancy on fetal brain development in rats and protective role of the vitamin E. Hum. Exp. Toxicol. 2016, 35, 1337–1344. [Google Scholar] [CrossRef]
- Erdemli, M.E.; Aladag, M.A.; Altinoz, E.; Demirtas, S.; Turkoz, Y.; Yigitcan, B.; Bag, H.G. Acrylamide applied during pregnancy causes the neurotoxic effect by lowering BDNF levels in the fetal brain. Neurotoxicol. Teratol. 2018, 67, 37–43. [Google Scholar] [CrossRef]
- Muanda, F.T.; Sheehy, O.; Bérard, A. Use of antibiotics during pregnancy and risk of spontaneous abortion. CMAJ 2017, 189, E625–E633. [Google Scholar] [CrossRef]
- Zemanova, N.; Lněničkova, K.; Vavrečkova, M.; Anzenbacherova, E.; Anzenbacher, P.; Zapletalova, I.; Hermanova, P.; Hudcovic, T.; Kozakova, H.; Jourova, L. Gut microbiome affects the metabolism of metronidazole in mice through regulation of hepatic cytochromes P450 expression. PLoS ONE 2021, 16, e0259643. [Google Scholar] [CrossRef] [PubMed]
- Chong, C.Y.L.; Orr, D.; Plank, L.D.; Vatanen, T.; O’Sullivan, J.M.; Murphy, R. Randomised Double-Blind Placebo-Controlled Trial of Inulin with Metronidazole in Non-Alcoholic Fatty Liver Disease (NAFLD). Nutrients 2020, 12, 937. [Google Scholar] [CrossRef] [PubMed]
- Eguchi, A.; Mizukami, S.; Nakamura, M.; Masuda, S.; Murayama, H.; Kawashima, M.; Inohana, M.; Nagahara, R.; Kobayashi, M.; Yamashita, R.; et al. Metronidazole enhances steatosis-related early-stage hepatocarcinogenesis in high fat diet-fed rats through DNA double-strand breaks and modulation of autophagy. Environ. Sci. Pollut. Res. Int. 2022, 29, 779–789. [Google Scholar] [CrossRef] [PubMed]
- Mudry, M.D.; Martínez-Flores, I.; Palermo, A.M.; Carballo, M.A.; Egozcue, J.; García Caldés, M. Embryolethality induced by metronidazole (MTZ) in Rattus norvegicus. Teratog. Carcinog. Mutagen. 2001, 21, 197–205. [Google Scholar] [CrossRef]
- Kazy, Z.; Puhó, E.; Czeizel, A.E. Teratogenic potential of vaginal metronidazole treatment during pregnancy. Eur. J. Obstet. Gynecol. Reprod. Biol. 2005, 123, 174–178. [Google Scholar] [CrossRef]
- Shennan, A.; Crawshaw, S.; Briley, A.; Hawken, J.; Seed, P.; Jones, G.; Poston, L.A. Randomised controlled Trial of metronidazole for the prevention of preterm birth in women positive for cervicovaginal fetal fibronectin: The PREMET Study. BJOG 2006, 113, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Burtin, P.; Taddio, A.; Ariburnu, O.; Einarson, T.R.; Koren, G. Safety of metronidazole in pregnancy: A meta-analysis. Am. J. Obstet. Gynecol. 1995, 172 Pt 1, 525–529. [Google Scholar] [CrossRef]
- Ajiji, P.; Uzunali, A.; Ripoche, E.; Vittaz, E.; Vial, T.; Maison, P. Investigating the efficacy and safety of metronidazole during pregnancy; A systematic review and meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. X 2021, 11, 100128. [Google Scholar] [CrossRef]
- Marcondes, F.K.; Bianchi, F.J.; Tanno, A.P. Determination of the oestrous cycle phases of rats: Some helpful considerations Braz. J. Biol. 2002, 62, 609–614. [Google Scholar]
- Cora, M.C.; Kooistra, L.; Travlos, G. Vaginal cytology of the laboratory rat and mouse: Review and criteria for the staging of the oestrous cycle using stained vaginal smears. Toxicol. Pathol. 2005, 43, 776–793. [Google Scholar] [CrossRef]
- Salewski, E. Farbemethode aum makroskopischen machweis von implantations-stellen arn uterus der ratte. Arch. Puthol. Exp. Pharmakol. 1964, 247, 367. [Google Scholar] [CrossRef]
- ElMazoudy, R.H.; Attia, A.A. Ginger causes subfertility and abortifacient in mice by targeting both oestrous cycle and blastocyst implantation without teratogenesis. Phytomedicine 2018, 50, 300–308. [Google Scholar] [CrossRef]
- Augustine-Rauch, K.; Zhang, C.X.; Panzica-Kelly, J.M. A developmental toxicology assay platform for screening teratogenic liability of pharmaceutical compounds. Birth Defects Res. Part B Dev. Reprod. Toxicol. 2016, 107, 4–20. [Google Scholar] [CrossRef] [PubMed]
- Koss, C.A.; Baras, D.C.; Lane, S.D.; Aubry, R.; Marcus, M.; Markowitz, L.E.; Koumans, E.H. Investigation of Metronidazole Use during Pregnancy and Adverse Birth Outcomes. Antimicrob. Agents Chemother. 2012, 56, 4800–4805. [Google Scholar] [CrossRef]
- Ceruelos, A.H.; Romero-Quezada, L.C.; Ledezma, R.J.C.; Contreras, L.L. Therapeutic uses of metronidazole and its side effects: An update. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 397–401. [Google Scholar]
- Zyro, D.; Radko, L.; Sliwinska, A.; Checinska, L.; Kusz, J.; Korona-Głowniak, I.; Przekora, A.; Wójcik, M.; Posyniak, A.; Ochocki, J. Multifunctional Silver(I) Complexes with Metronidazole Drug Reveal Antimicrobial Properties and Antitumor Activity against Human Hepatoma and Colorectal Adenocarcinoma Cells. Cancers 2022, 14, 900. [Google Scholar] [CrossRef] [PubMed]
- Buschini, A.; Ferrarini, L.; Franzoni, S.; Galati, S.; Lazzaretti, M.; Mussi, F.; de Albuquerque, C.N.; Zucchi, T.A.; Poli, P. Genotoxicity Revaluation of Three Commercial Nitroheterocyclic Drugs: Nifurtimox, Benznidazole, and Metronidazole. J. Parasitol. Res. 2009, 2009, 463575. [Google Scholar] [CrossRef] [PubMed]
- Talapatra, S.N.; Dasgupta, S.; Guha, G.; Auddy, M.; Muka Hopadhyay, A. Therapeutic efficacies of Coriandrum sativum aqueous extract against metronidazole induced genotoxicity in Channa punctatus peripheral erythrocytes. Food Chem. Toxicol. 2010, 48, 3458–3461. [Google Scholar] [CrossRef] [PubMed]
- Roy, L.D.; Giri, S.; Singh, S.; Giri, A. Effects of radiation and vitamin C treatment on metronidazole genotoxicity in mice. Mutat. Res. Genet. Toxicol. Environ. Mutagen. 2013, 753, 65–71. [Google Scholar] [CrossRef]
- Menendez, D.; Bendesky, A.; Rojas, E.; Salamanca, F.; Ostrosky- Wegman, P. Role of P53 functionality in the genotoxicity of metronidazole and its hydroxy metabolite. Mutat. Res. Genet. Toxicol. Environ. Mutagen. 2002, 501, 57–67. [Google Scholar] [CrossRef]
- El-Nahas, A.F.; El-Ashmawy, I.M. Reproductive and Cytogenetic Toxicity of Metronidazole in Male Mice. Basic Clin. Pharmacol. Toxicol. 2004, 94, 226–231. [Google Scholar] [CrossRef]
- Kovacic, P.; Somanathan, R. Nitroaromatic compounds: Environmental toxicity, carcinogenicity, mutagenicity, therapy, and mechanism. J. Appl. Toxicol. 2014, 34, 810–824. [Google Scholar] [CrossRef]
- Dingsdag, S.A.; Hunter, N. Metronidazole: An update on metabolism, structure-cytotoxicity and resistance mechanisms. J. Antimicrob. Chemother. 2017, 73, 265–279. [Google Scholar] [CrossRef]
- Goolsby, T.A.; Jakeman, B.; Gaynes, R.P. Clinical relevance of metronidazole and peripheral neuropathy: A systematic review of the literature. Int. J. Antimicrob. Agents 2018, 51, 319–325. [Google Scholar] [CrossRef]
- FDA. FDA-Approved Drug Products: Flagyl (Metronidazole) Capsules for Oral Administration. 2013. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/020334s008lbl.pdf (accessed on 12 August 2003.).
- Rosenfeld, C.S. Placental serotonin signaling, pregnancy outcomes, and regulation of fetal brain development. Biol. Reprod. 2020, 102, 532–538. [Google Scholar] [CrossRef]
- Barut, F.; Barut, A.; Gun, B.D.; Kandemir, N.O.; Harma, M.I.; Harma, M.; Ozdamar, S.O. Intrauterine growth restriction and placental angiogenesis. Diagn. Pathol. 2010, 5, 24. [Google Scholar] [CrossRef] [PubMed]
- Perez-Garcia, V.; Fineberg, E.; Wilson, R.; Murray, A.; Mazzeo, C.I.; Tudor, C.; Sienerth, A.; White, J.K.; Tuck, E.; Ryder, E.J.; et al. Placentation defects are highly prevalent in embryonic lethal mouse mutants. Nature 2018, 555, 463–468. [Google Scholar] [CrossRef]
- Rani, A.; Wadhwani, N.; Chavan-Gautam, P.; Joshi, S. Altered development and function of the placental regions in preeclampsia and its association with long-chain polyunsaturated fatty acids. Rev. Dev. Biol. 2016, 5, 582–597. [Google Scholar] [CrossRef] [PubMed]
- Woods, L.; Perez-Garcia, V.; Hemberger, M. Regulation of Placental Development, and Its Impact on Fetal Growth-New Insights from Mouse Models. Front. Endocrinol. 2018, 9, 570. [Google Scholar] [CrossRef] [PubMed]
- Erel, C.T.; Dane, B.; Calay, Z.; Kaleli, S.; Aydinli, K. Apoptosis in the placenta of pregnancies complicated with IUGR. Int. J. Gynecol. Obstet. 2001, 73, 229–235. [Google Scholar] [CrossRef]
- Furukawa, S.; Hayashi, S.; Usuda, K.; Abe, M.; Hagio, S.; Ogawa, I. Toxicological Pathology in the Rat Placenta. J. Toxicol. Pathol. 2011, 24, 95–111. [Google Scholar] [CrossRef] [PubMed]
- Onopiuk, B.; Onopiuk, P.; Dąbrowska, Z.; Dąbrowska, E.; Pietruska, M.; Car, H. Effect of Metronidazole on the Oxidoreductive Processes in the Submandibular and Parotid Glands in Experimental Research. Oxidative Med. Cell. Longev. 2018, 2018, 7083486. [Google Scholar] [CrossRef]
- Yang, J.; Wang, T.; Lin, G.; Li, M.; Zhu, R.; Yiannikouris, A.; Zhang, Y.; Mai, K. The Assessment of Diet Contaminated with Aflatoxin B(1) in Juvenile Turbot (Scophthalmus maximus) and the Evaluation of the Efficacy of Mitigation of a Yeast Cell Wall Extract. Toxins 2020, 12, 597. [Google Scholar] [CrossRef]
- Li, L.; Chen, T.; Yang, Z.; Chen, Y.; Liu, D.; Xiao, H.; Liu, M.; Liu, K.; Xu, J.; Liu, S.; et al. Nephrotoxicity Evaluation of Indium Phosphide Quantum Dots with Different Surface Modifications in BALB/c Mice. Int. J. Mol. Sci. 2020, 21, 7137. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Shen, W.; Hou, C.; Gao, X.; Wang, Q.; Wu, X.; Zhu, J. Low temperature-induced variation in plasma biochemical indices and aquaglyceroporin gene expression in the large yellow croaker Larimichthys crocea. Sci. Rep. 2019, 9, 2717. [Google Scholar] [CrossRef]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 140, e563–e595. [Google Scholar] [CrossRef]
- Rivadeneyra-Domínguez, E.; Pérez-Pérez, J.E.; Vázquez-Luna, A.; Díaz-Sobac, R.; Rodríguez-Landa, J.F. Effects of Cassava Juice (Manihot esculenta Crantz) on Renal and Hepatic Function and Motor Impairments in Male Rats. Toxins 2020, 12, 708. [Google Scholar] [CrossRef]
- Kraft, R.; Herndon, D.N.; Al-Mousawi, A.M.; Williams, F.N.; Finnerty, C.C.; Jeschke, M.G. Burn size and survival probability in paediatric patients in modern burn care: Prospective. observational cohort study. Lancet 2012, 379, 1013–1021. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; Deng, G.F.; Guo, X.Q.; Kuang, J.; Zhang, C.Y.; Cao, H.B.; Hu, G.L. Clinicopathology of Gout in Growing Layers Induced by Avian Nephrotrophic Strains of Infectious Bronchitis Virus. Pak. Vet. J. 2015, 35, 345–349. [Google Scholar]
- Thakur, R.; Sharma, A.; Lingaraju, M.C.; Begum, J.; Kumar, D.; Mathesh, K.; Kumar, P.; Singh, T.U.; Kumar, D. Ameliorative effect of ursolic acid on renal fibrosis in adenine-induced chronic kidney disease in rats. Biomed. Pharmacother. 2018, 101, 972–980. [Google Scholar] [CrossRef] [PubMed]
- Zhao, C.N.; Tang, G.Y.; Liu, Q.; Xu, X.Y.; Cao, S.Y.; Gan, R.Y.; Zhang, K.Y.; Meng, S.L.; Li, H.B. Five-Golden-Flowers Tea: Green Extraction and Hepatoprotective Effect against Oxidative Damage. Molecules 2018, 23, 2216. [Google Scholar] [CrossRef] [PubMed]

| Parameters | Experimental Groups | |||
|---|---|---|---|---|
| GC | GMI | GMII | GMIII | |
| Number of litters | 10 | 10 | 10 | 10 |
| Number of fetuses | 132.3 | 77.80 | 68.20 | 60.80 |
| Number of implantation sites/litter | 13.50 ± 1.25 | 8.75 ± 0.95 * | 8.69 ± 0.85 * | 7.28 ± 0.95 * |
| Number of resorption sites/litter | 0.27 ± 0.015 | 0.97 ± 0.013 * | 1.21 ± 0.002 * | 1.42 ± 0.002 * |
| Number of dead fetuses/litter | 0.00 | 0.00 | 0.66 ± 0.04 * | 0.78 ± 0.04 * |
| Number of live fetuses/litter | 13.23 ± 0.57 | 7.78 ± 1.30 * | 6.82 ± 1.30 * | 6.08 ± 1.30 * |
| Fetal body weight (g) | 5.02 ± 0.130 | 4.89 ± 0.300 | 3.52 ± 0.167 * | 2.99 ± 0.090 * |
| Crown-Rump Length (mm) | 40.01 ± 1.42 | 39.20 ± 2.21 | 26.32 ± 1.12 * | 21.50 ± 1.23 * |
| Lipid Index | Groups | |||
|---|---|---|---|---|
| GC | GMI | GMII | GMIII | |
| TC (mg/dL) | 81.51 ± 5.11 | 82.61 ± 6.12 | 85.43 ± 4.22 | 131.42 ± 7.12 * |
| TG (mg/dL) | 89.14 ± 6.31 | 88.33 ± 5.67 | 87.86 ± 5.17 | 166.8 ± 10.31 * |
| HDL (mg/dL) | 37.33 ± 3.22 | 40.21 ± 4.01 | 42.62 ± 3.15 | 35.04 ± 2.09 |
| LDL (mg/dL) | 16.24 ± 3.46 | 17.88 ± 1.96 | 18.21 ± 1.77 | 31.22 ± 2.41 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
AbdRabou, M.A.; Alrashdi, B.M.; Alruwaili, H.K.; Elmazoudy, R.H.; Alwaili, M.A.; Othman, S.I.; Alghamdi, F.A.; Fahmy, G.H. Exploration of Maternal and Fetal Toxicity Risks for Metronidazole-Related Teratogenicity and Hepatotoxicity through an Assessment in Albino Rats. Toxics 2023, 11, 303. https://doi.org/10.3390/toxics11040303
AbdRabou MA, Alrashdi BM, Alruwaili HK, Elmazoudy RH, Alwaili MA, Othman SI, Alghamdi FA, Fahmy GH. Exploration of Maternal and Fetal Toxicity Risks for Metronidazole-Related Teratogenicity and Hepatotoxicity through an Assessment in Albino Rats. Toxics. 2023; 11(4):303. https://doi.org/10.3390/toxics11040303
Chicago/Turabian StyleAbdRabou, Mervat A., Barakat M. Alrashdi, Hadeel K. Alruwaili, Reda H. Elmazoudy, Maha A. Alwaili, Sarah I. Othman, Fawzyah A. Alghamdi, and Gehan H. Fahmy. 2023. "Exploration of Maternal and Fetal Toxicity Risks for Metronidazole-Related Teratogenicity and Hepatotoxicity through an Assessment in Albino Rats" Toxics 11, no. 4: 303. https://doi.org/10.3390/toxics11040303
APA StyleAbdRabou, M. A., Alrashdi, B. M., Alruwaili, H. K., Elmazoudy, R. H., Alwaili, M. A., Othman, S. I., Alghamdi, F. A., & Fahmy, G. H. (2023). Exploration of Maternal and Fetal Toxicity Risks for Metronidazole-Related Teratogenicity and Hepatotoxicity through an Assessment in Albino Rats. Toxics, 11(4), 303. https://doi.org/10.3390/toxics11040303







