On the Need for Human Studies of PM Exposure Activation of the NLRP3 Inflammasome
Abstract
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lane, K.J.; Scammell, M.K.; Levy, J.I.; Fuller, C.H.; Parambi, R.; Zamore, W.; Mwamburi, M.; Brugge, D. Positional error and time-activity patterns in near-highway proximity studies: An exposure misclassification analysis. Environ. Health 2013, 12, 75. [Google Scholar] [CrossRef] [PubMed]
- Walker, D.I.; Lane, K.J.; Liu, K.; Uppal, K.; Patton, A.P.; Durant, J.L.; Jones, D.P.; Brugge, D.; Pennell, K.D. Metabolomic assessment of exposure to near-highway ultrafine particles. J. Expo. Sci. Environ. Epidemiol. 2019, 29, 469–483. [Google Scholar] [CrossRef] [PubMed]
- Nephew, B.C.; Nemeth, A.; Hudda, N.; Beamer, G.; Mann, P.; Petitto, J.; Cali, R.; Febo, M.; Kulkarni, P.; Poirier, G.; et al. Traffic-related particulate matter affects behavior, inflammation, and neural integrity in a developmental rodent model. Environ. Res. 2020, 183, 109242. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Gu, X.; Deng, F.; Mu, L.; Baccarelli, A.A.; Guo, X.; Wu, S. Ambient particulate air pollution and circulating C-reactive protein level: A systematic review and meta-analysis. Int. J. Hyg. Environ. Health 2019, 222, 756–764. [Google Scholar] [CrossRef] [PubMed]
- Lane, K.J.; Levy, J.I.; Scammell, M.K.; Peters, J.L.; Patton, A.P.; Reisner, E.; Lowe, L.; Zamore, W.; Durant, J.L.; Brugge, D. Association of modeled long-term personal exposure to ultrafine particles with inflammatory and coagulation biomarkers. Environ. Int. 2016, 92, 173–182. [Google Scholar] [CrossRef]
- Lane, K.J.; Levy, J.I.; Patton, A.P.; Durant, J.L.; Zamore, W.; Brugge, D. Relationship between traffic-related air pollution and inflammation biomarkers using structural equation modelling. Sci. Total Environ. 2023, 870, 161874. [Google Scholar] [CrossRef]
- Brook, R.D.; Rajagopalan, S.; Pope III, C.A.; Brook, J.R.; Bhatnagar, A.; Diez-Roux, A.V.; Holguin, F.; Hong, Y.; Luepker, R.V.; Mittleman, M.A. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation 2010, 121, 2331–2378. [Google Scholar] [CrossRef]
- Cohen, A.J.; Brauer, M.; Burnett, R.; Anderson, H.R.; Frostad, J.; Estep, K.; Balakrishnan, K.; Brunekreef, B.; Dandona, L.; Dandona, R. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: An analysis of data from the Global Burden of Diseases Study 2015. Lancet 2017, 389, 1907–1918. [Google Scholar] [CrossRef]
- Duan, S.; Wang, N.; Huang, L.; Zhao, Y.; Shao, H.; Jin, Y.; Zhang, R.; Li, C.; Wu, W.; Wang, J. NLRP3 inflammasome activation is associated with PM2. 5-induced cardiac functional and pathological injury in mice. Environ. Toxicol. 2019, 34, 1246–1254. [Google Scholar] [CrossRef]
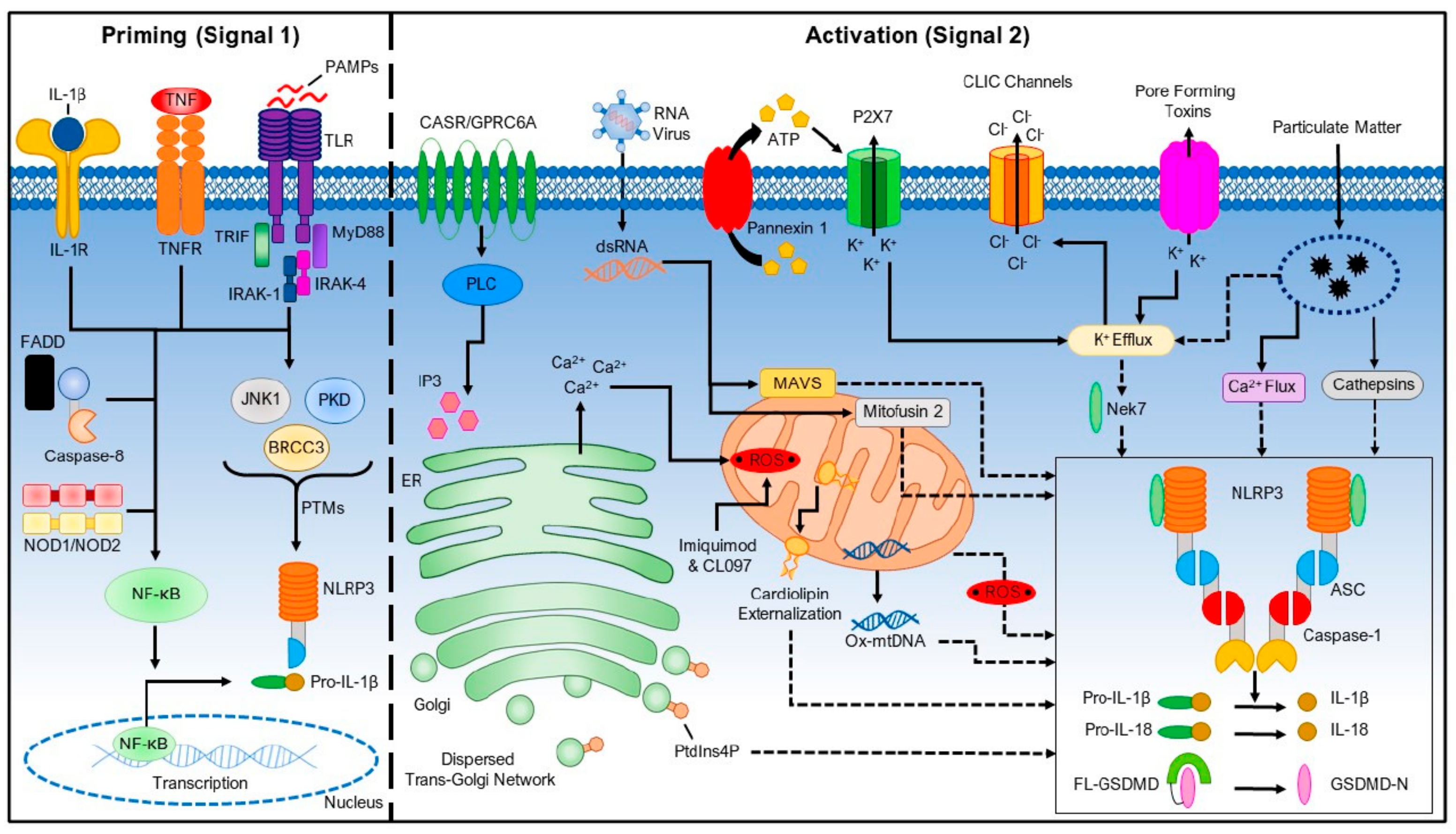
- Kelley, N.; Jeltema, D.; Duan, Y.; He, Y. The NLRP3 inflammasome: An overview of mechanisms of activation and regulation. Int. J. Mol. Sci. 2019, 20, 3328. [Google Scholar] [CrossRef]
- Swanson, K.V.; Deng, M.; Ting, J.P.-Y. The NLRP3 inflammasome: Molecular activation and regulation to therapeutics. Nat. Rev. Immunol. 2019, 19, 477–489. [Google Scholar] [CrossRef] [PubMed]
- Leso, V.; Fontana, L.; Iavicoli, I. Nanomaterial exposure and sterile inflammatory reactions. Toxicol. Appl. Pharmacol. 2018, 355, 80–92. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-K.; Choe, J.-Y.; Park, K.-Y. Anti-inflammatory effect of artemisinin on uric acid-induced NLRP3 inflammasome activation through blocking interaction between NLRP3 and NEK7. Biochem. Biophys. Res. Commun. 2019, 517, 338–345. [Google Scholar] [CrossRef] [PubMed]
- Gao, L.; Qin, J.X.; Shi, J.Q.; Jiang, T.; Wang, F.; Xie, C.; Gao, Q.; Zhi, N.; Dong, Q.; Guan, Y.T. Fine particulate matter exposure aggravates ischemic injury via NLRP3 inflammasome activation and pyroptosis. CNS Neurosci. Ther. 2022, 28, 1045–1058. [Google Scholar] [CrossRef] [PubMed]
- Niu, L.; Li, L.; Xing, C.; Luo, B.; Hu, C.; Song, M.; Niu, J.; Ruan, Y.; Sun, X.; Lei, Y. Airborne particulate matter (PM2. 5) triggers cornea inflammation and pyroptosis via NLRP3 activation. Ecotoxicol. Environ. Saf. 2021, 207, 111306. [Google Scholar] [CrossRef] [PubMed]
- Tien, C.-P.; Chen, C.-H.; Lin, W.-Y.; Liu, C.-S.; Liu, K.-J.; Hsiao, M.; Chang, Y.-C.; Hung, S.-C. Ambient particulate matter attenuates Sirtuin1 and augments SREBP1-PIR axis to induce human pulmonary fibroblast inflammation: Molecular mechanism of microenvironment associated with COPD. Aging 2019, 11, 4654. [Google Scholar] [CrossRef] [PubMed]
- Xu, F.; Qiu, X.; Hu, X.; Shang, Y.; Pardo, M.; Fang, Y.; Wang, J.; Rudich, Y.; Zhu, T. Effects on IL-1β signaling activation induced by water and organic extracts of fine particulate matter (PM2.5) in vitro. Environ. Pollut. 2018, 237, 592–600. [Google Scholar] [CrossRef]
- Zheng, R.; Tao, L.; Jian, H.; Chang, Y.; Cheng, Y.; Feng, Y.; Zhang, H. NLRP3 inflammasome activation and lung fibrosis caused by airborne fine particulate matter. Ecotoxicol. Environ. Saf. 2018, 163, 612–619. [Google Scholar] [CrossRef]
- Zheng, R.; Zhang, J.; Han, X.; Wu, Y.; Yan, J.; Song, P.; Wang, Y.; Wu, X.; Zhang, H. Particulate matter aggravates Alzheimer’s disease by activating the NLRP3 inflammasome to release ASC specks. Environ. Sci. Nano 2021, 8, 2177–2190. [Google Scholar] [CrossRef]
- Zhong, Y.; Wang, Y.; Zhang, C.; Hu, Y.; Sun, C.; Liao, J.; Wang, G. Identification of long non-coding RNA and circular RNA in mice after intra-tracheal instillation with fine particulate matter. Chemosphere 2019, 235, 519–526. [Google Scholar] [CrossRef]
- Chan, Y.L.; Wang, B.; Chen, H.; Ho, K.F.; Cao, J.; Hai, G.; Jalaludin, B.; Herbert, C.; Thomas, P.S.; Saad, S. Pulmonary inflammation induced by low-dose particulate matter exposure in mice. Am. J. Physiol. Lung Cell. Mol. Physiol. 2019, 317, L424–L430. [Google Scholar] [CrossRef] [PubMed]
- Du, X.; Jiang, S.; Zeng, X.; Zhang, J.; Pan, K.; Zhou, J.; Xie, Y.; Kan, H.; Song, W.; Sun, Q. Air pollution is associated with the development of atherosclerosis via the cooperation of CD36 and NLRP3 inflammasome in ApoE-/-mice. Toxicol. Lett. 2018, 290, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Du, X.; Jiang, S.; Zeng, X.; Zhang, J.; Pan, K.; Song, L.; Zhou, J.; Kan, H.; Sun, Q.; Zhao, J. Fine particulate matter-induced cardiovascular injury is associated with NLRP3 inflammasome activation in Apo E-/-mice. Ecotoxicol. Environ. Saf. 2019, 174, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Ding, S.; Zhang, G.; Dong, Y. Ambient particulate matter exposure plus a high-fat diet exacerbate renal injury by activating the NLRP3 inflammasome and TGF-β1/Smad2 signaling pathway in mice. Ecotoxicol. Environ. Saf. 2022, 238, 113571. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Zhang, G.; Yu, M.; Gu, J.; Zheng, Y.; Sun, J.; Ding, S. Quercetin improves the adipose inflammatory response and insulin signaling to reduce “real-world” particulate matter-induced insulin resistance. Environ. Sci. Pollut. Res. 2022, 29, 2146–2157. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Hua, Q.; Shao, Y.; Zeng, H.; Liu, Y.; Diao, Q.; Zhang, H.; Qiu, M.; Zhu, J.; Li, X. Circular RNA circBbs9 promotes PM2. 5-induced lung inflammation in mice via NLRP3 inflammasome activation. Environ. Int. 2020, 143, 105976. [Google Scholar] [CrossRef]
- Li, J.; Zhang, Y.; Zhang, L.; An, Z.; Song, J.; Wang, C.; Ma, Y.; Gu, Q.; Luo, Q.; Yang, W. Fine particulate matter exposure exacerbated nasal mucosal damage in allergic rhinitis mice via NLRP3 mediated pyroptosis. Ecotoxicol. Environ. Saf. 2021, 228, 112998. [Google Scholar] [CrossRef]
- Song, L.; Lei, L.; Jiang, S.; Pan, K.; Zeng, X.; Zhang, J.; Zhou, J.; Xie, Y.; Zhou, L.; Dong, C. NLRP3 inflammasome is involved in ambient PM2. 5-related metabolic disorders in diabetic model mice but not in wild-type mice. Inhal. Toxicol. 2021, 33, 260–267. [Google Scholar] [CrossRef]
- Ding, S.; Wang, H.; Wang, M.; Bai, L.; Yu, P.; Wu, W. Resveratrol alleviates chronic “real-world” ambient particulate matter-induced lung inflammation and fibrosis by inhibiting NLRP3 inflammasome activation in mice. Ecotoxicol. Environ. Saf. 2019, 182, 109425. [Google Scholar] [CrossRef]
- Lee, C.-W.; Chi, M.-C.; Hsu, L.-F.; Yang, C.-M.; Hsu, T.-H.; Chuang, C.-C.; Lin, W.-N.; Chu, P.-M.; Lee, I.-T. Carbon monoxide releasing molecule-2 protects against particulate matter-induced lung inflammation by inhibiting TLR2 and 4/ROS/NLRP3 inflammasome activation. Mol. Immunol. 2019, 112, 163–174. [Google Scholar] [CrossRef]
- Zhou, L.; Li, P.; Zhang, M.; Han, B.; Chu, C.; Su, X.; Li, B.; Kang, H.; Ning, J.; Zhang, B. Carbon black nanoparticles induce pulmonary fibrosis through NLRP3 inflammasome pathway modulated by miR-96 targeted FOXO3a. Chemosphere 2020, 241, 125075. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M.; MacFadyen, J.G.; Thuren, T.; Libby, P. Residual inflammatory risk associated with interleukin-18 and interleukin-6 after successful interleukin-1β inhibition with canakinumab: Further rationale for the development of targeted anti-cytokine therapies for the treatment of atherothrombosis. Eur. Heart J. 2020, 41, 2153–2163. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M.; MacFadyen, J.G.; Everett, B.M.; Libby, P.; Thuren, T.; Glynn, R.J.; Kastelein, J.; Koenig, W.; Genest, J.; Lorenzatti, A. Relationship of C-reactive protein reduction to cardiovascular event reduction following treatment with canakinumab: A secondary analysis from the CANTOS randomised controlled trial. Lancet 2018, 391, 319–328. [Google Scholar] [CrossRef]
- Özenver, N.; Efferth, T. Phytochemical inhibitors of the NLRP3 inflammasome for the treatment of inflammatory diseases. Pharmacol. Res. 2021, 170, 105710. [Google Scholar] [CrossRef]
- Wang, Q.; Su, C.-P.; Zhang, H.-M.; Ren, Y.-L.; Wang, W.; Guo, S.-Z. Anti-inflammatory mechanism of heat-clearing and detoxifying Chinese herbs. China J. Chin. Mater. Med. 2018, 43, 3787–3794. [Google Scholar] [CrossRef]
- Muluye, R.A.; Bian, Y.; Alemu, P.N. Anti-inflammatory and antimicrobial effects of heat-clearing Chinese herbs: A current review. J. Tradit. Complement. Med. 2014, 4, 93–98. [Google Scholar] [CrossRef]
- Pan, M.-H.; Chiou, Y.-S.; Tsai, M.-L.; Ho, C.-T. Anti-inflammatory activity of traditional Chinese medicinal herbs. J. Tradit. Complement. Med. 2011, 1, 8–24. [Google Scholar] [CrossRef]
- Ichikawa, H.; Wang, X.; Konishi, T. Role of component herbs in antioxidant activity of shengmai san—A traditional Chinese medicine formula preventing cerebral oxidative damage in rat. Am. J. Chin. Med. 2003, 31, 509–521. [Google Scholar] [CrossRef]
- Zijlstra, F.J.; Van den Berg-de Lange, I.; Huygen, F.J.; Klein, J. Anti-inflammatory actions of acupuncture. Mediat. Inflamm. 2003, 12, 59–69. [Google Scholar] [CrossRef]
- McDonald, J.L.; Cripps, A.W.; Smith, P.K.; Smith, C.A.; Xue, C.C.; Golianu, B. The anti-inflammatory effects of acupuncture and their relevance to allergic rhinitis: A narrative review and proposed model. Evid. Based Complement. Altern. Med. 2013, 2013, 591796. [Google Scholar] [CrossRef]
- Kavoussi, B.; Ross, B.E. The neuroimmune basis of anti-inflammatory acupuncture. Integr. Cancer Ther. 2007, 6, 251–257. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.K.; Bae, H. Acupuncture and immune modulation. Auton. Neurosci. 2010, 157, 38–41. [Google Scholar] [CrossRef] [PubMed]
- Corlin, L.; Woodin, M.; Thanikachalam, M.; Lowe, L.; Brugge, D. Evidence for the healthy immigrant effect in older Chinese immigrants: A cross-sectional study. BMC Public Health 2014, 14, 603. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brugge, D.; Li, J.; Zamore, W. On the Need for Human Studies of PM Exposure Activation of the NLRP3 Inflammasome. Toxics 2023, 11, 202. https://doi.org/10.3390/toxics11030202
Brugge D, Li J, Zamore W. On the Need for Human Studies of PM Exposure Activation of the NLRP3 Inflammasome. Toxics. 2023; 11(3):202. https://doi.org/10.3390/toxics11030202
Chicago/Turabian StyleBrugge, Doug, Jianghong Li, and Wig Zamore. 2023. "On the Need for Human Studies of PM Exposure Activation of the NLRP3 Inflammasome" Toxics 11, no. 3: 202. https://doi.org/10.3390/toxics11030202
APA StyleBrugge, D., Li, J., & Zamore, W. (2023). On the Need for Human Studies of PM Exposure Activation of the NLRP3 Inflammasome. Toxics, 11(3), 202. https://doi.org/10.3390/toxics11030202





