Selected Political Criminal Poisonings in the Years 1978–2020: Detection and Treatment
Abstract
:1. Introduction
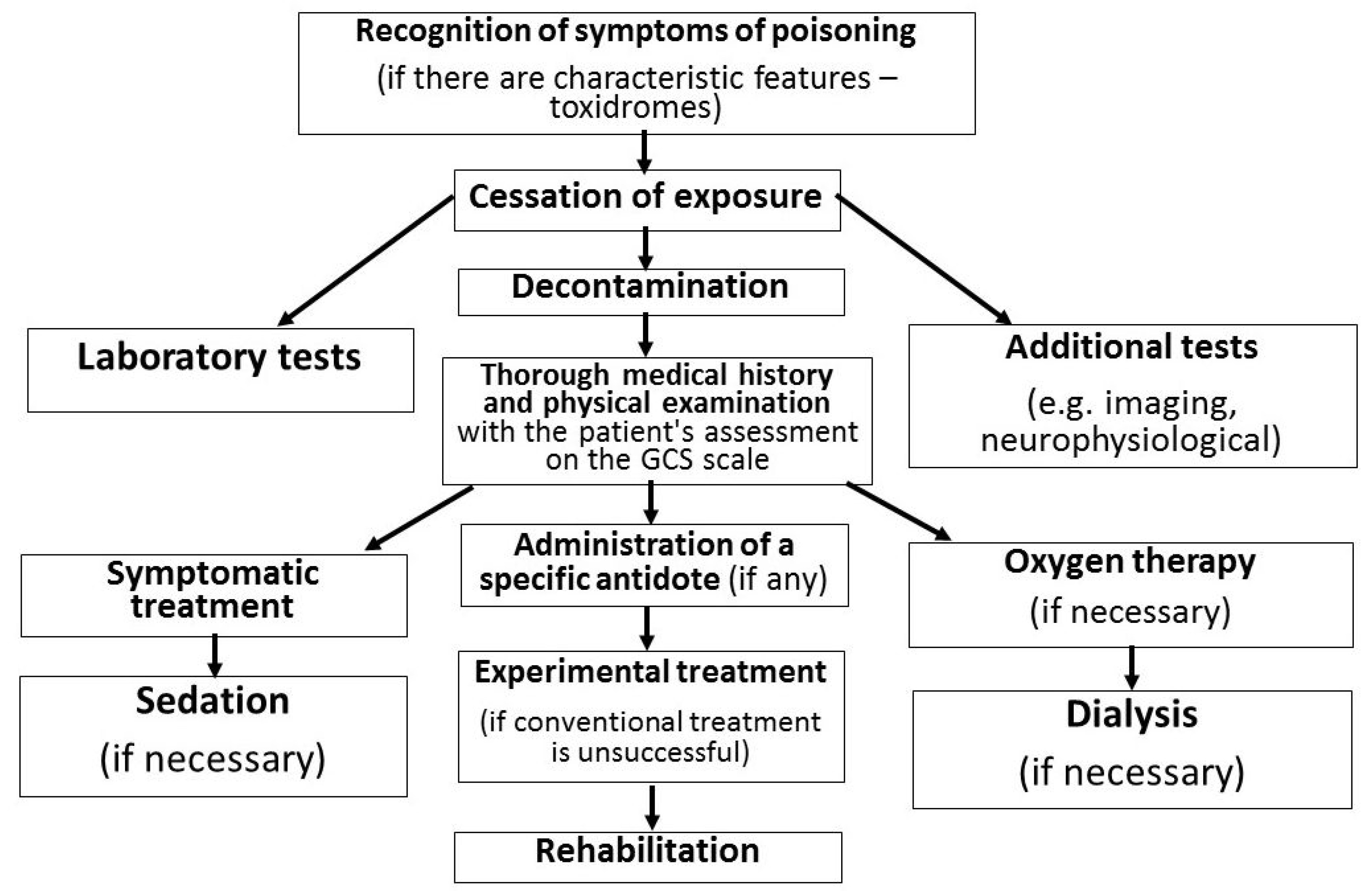
2. Criminal Poisoning Cases
3. Toxicological Properties, Treatment and Diagnostics
3.1. Ricin
3.1.1. Properties, Metabolic Pathway and Toxic Effects
3.1.2. First Aid and Treatment
3.1.3. Diagnostics
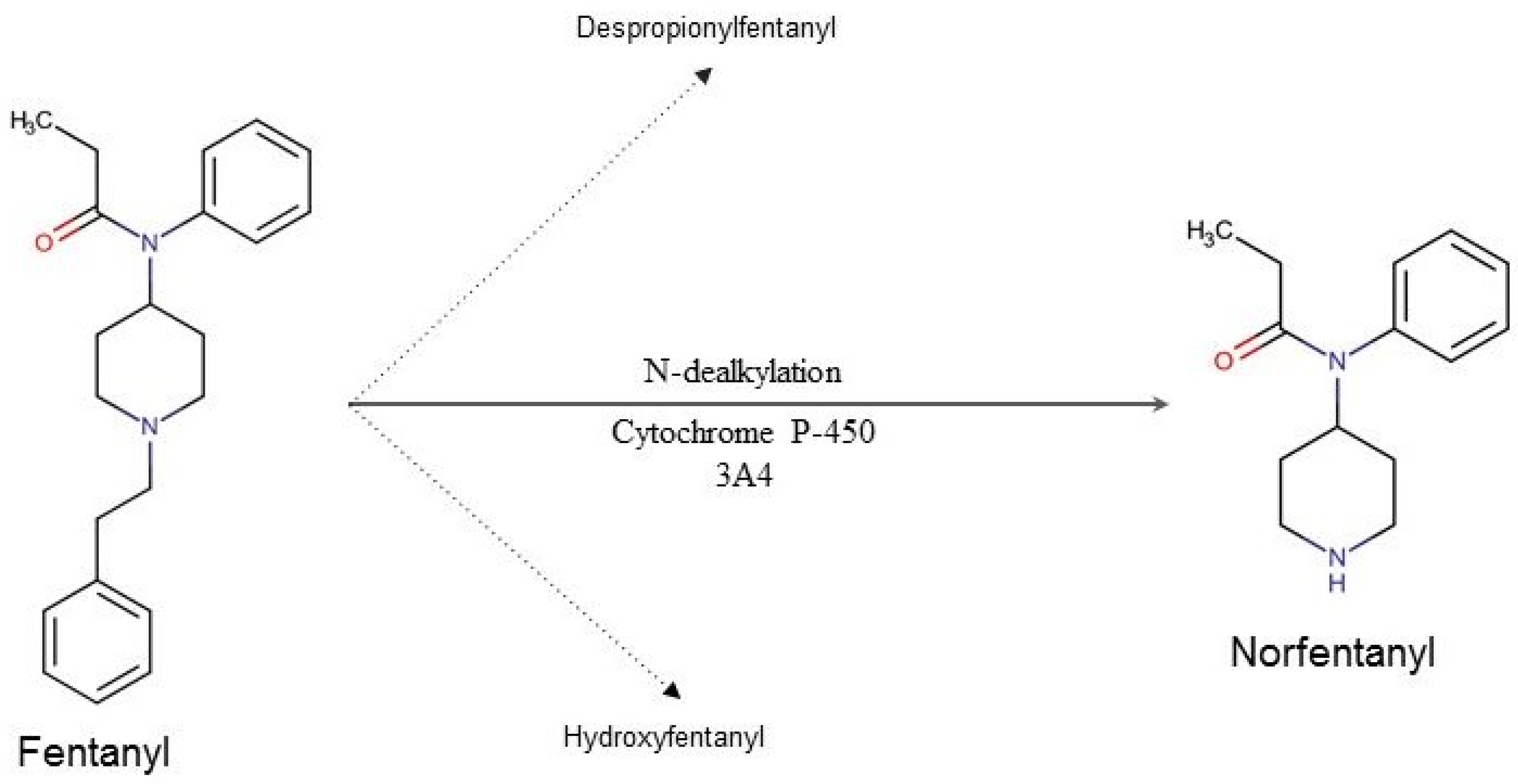
3.2. Fentanyl
3.2.1. Properties, Metabolic Pathway and Toxic Effects
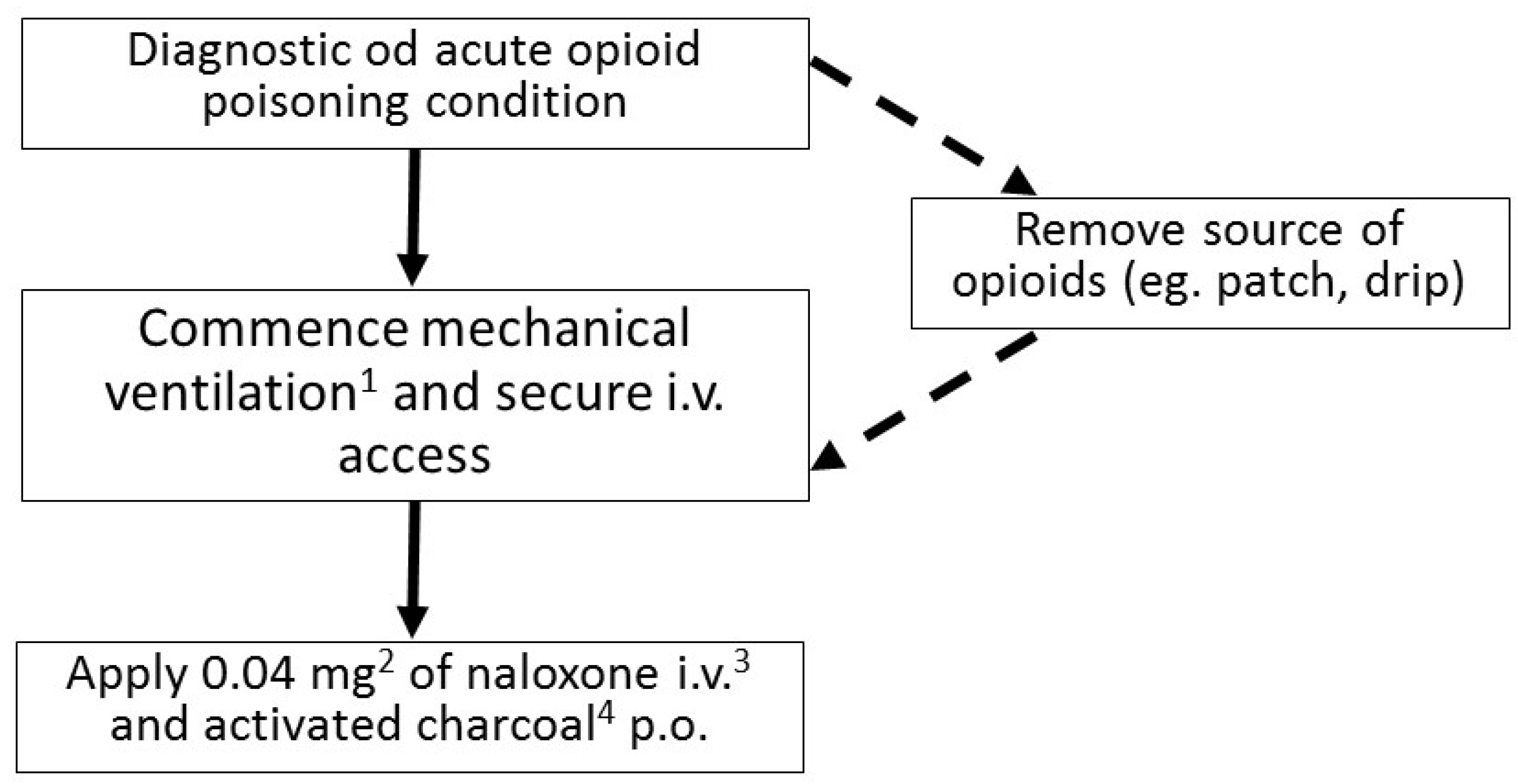
3.2.2. First Aid and Treatment
3.2.3. Diagnostics
3.3. TCDD
3.3.1. Properties, Metabolic Pathway and Toxic Effects
3.3.2. First aid and Treatment
3.3.3. Diagnostics
3.4. Isotope of Polonium 210Po
3.4.1. Properties, Metabolic Pathway and Toxic Effects
3.4.2. First aid and Treatment
3.4.3. Diagnostics
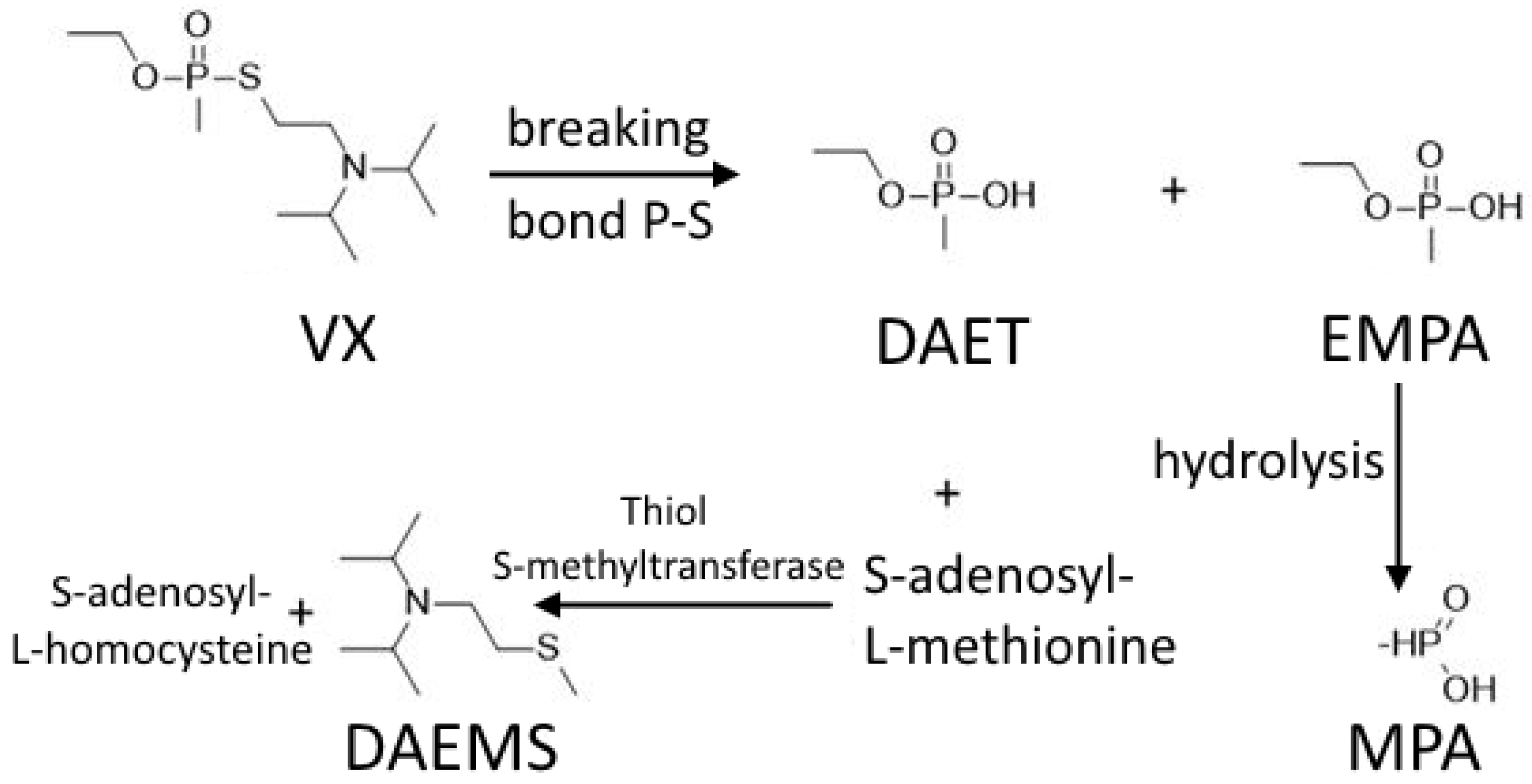
3.5. VX
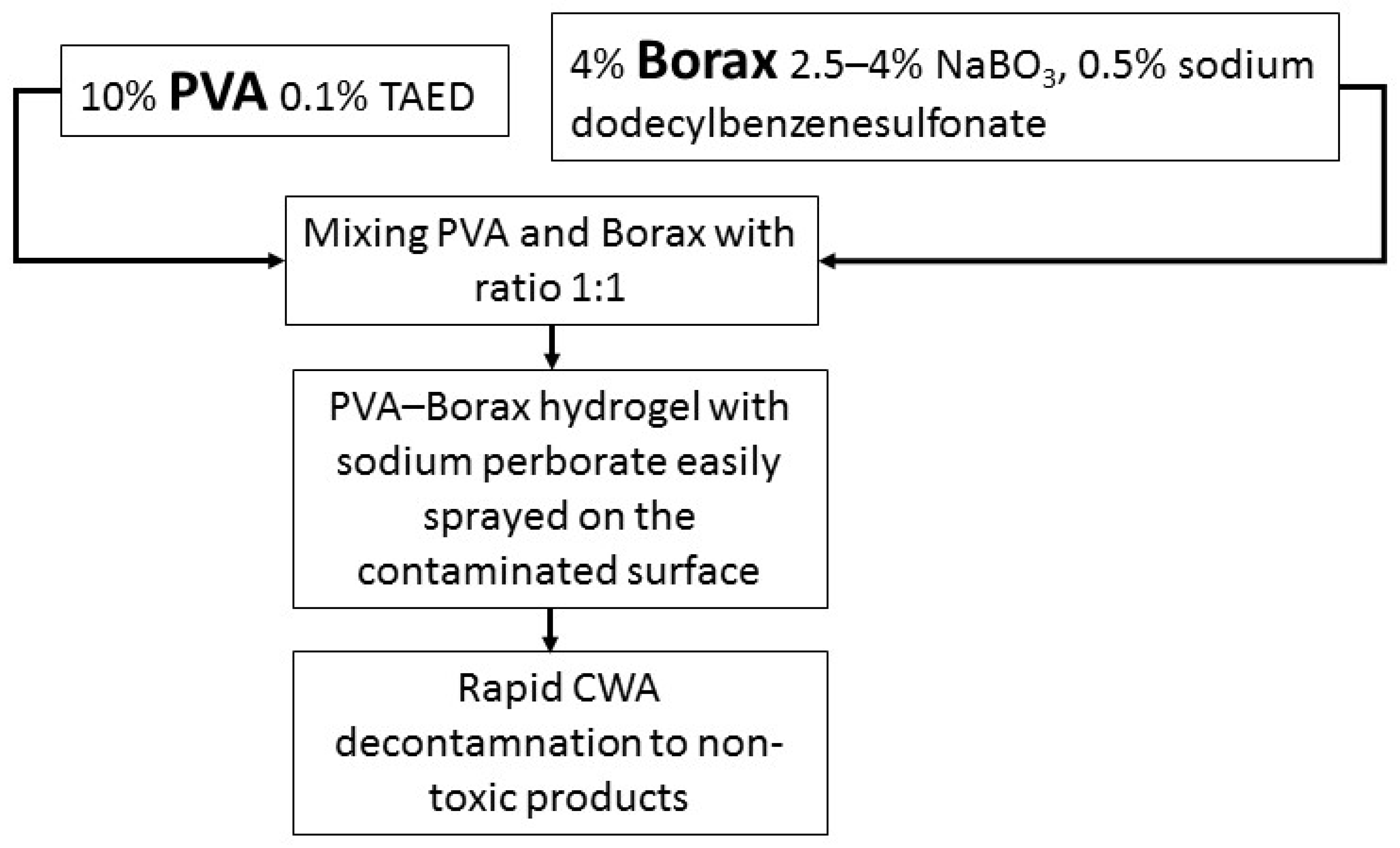
3.5.1. Properties, Metabolic Pathway and Toxic Effects
3.5.2. First Aid and Treatment
3.5.3. Diagnostics
3.6. Novichok
3.6.1. Properties, Metabolic Pathway and Toxic Effects
3.6.2. First Aid and Therapy
3.6.3. Diagnostics
4. Discussion
4.1. Ricin
4.2. Fentanyl
4.3. TCDD
4.4. Polonium Isotope 210Po
4.5. VX
4.6. Novichok
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Trestrail, J.H. Criminal Poisoning, Investigation Guide For Law Enforcement, Toxicologist, Forensic Scientists, and Attorneys; Humana Press: Totowa, NJ, USA, 2007. [Google Scholar]
- Nepovimova, E.; Kuca, K. The history of poisoning: From ancient times until modern ERA. Arch. Toxicol. 2019, 93, 11–24. [Google Scholar] [CrossRef] [PubMed]
- Gessen, M. We Now Know More About the Apparent Poisoning of the Pussy Riot Member Pyotr Verzilov. The New Yorker. 2018. Available online: https://www.newyorker.com/news/our-columnists/we-now-know-more-about-the-apparent-poisoning-of-the-pussy-riot-member-pyotr-verzilov (accessed on 20 July 2022).
- Monroe, J. Pussy Riot Member Seized by Police and Accused of Organizing Riots. Pitchfork. 2020. Available online: https://pitchfork.com/news/pussy-riot-member-seized-by-police-and-accused-of-organizing-riots/ (accessed on 30 June 2022).
- BBC News, Pussy Riot’s Pyotr Verzilov Blames Russia for ‘Poisoning’. 2018. Available online: https://www.bbc.com/news/world-europe-45658983 (accessed on 30 June 2022).
- Nehring, C. Umbrella or pen? The murder of Georgi Markov. New facts and old questions. J. Intell. Hist. 2017, 16, 47–58. [Google Scholar] [CrossRef]
- Warner, V.S. ‘Global Dissident’: Georgi Markov as a Cold War Playwright and Exile Rising to the Top: Markov’ s Literary Career in the Early 1960s. Studia Hist. Gedanensia 2014, 2014, 73–94. [Google Scholar]
- Ryall, J. Profile: Who Was Kim Jong-nam, the Exiled Half-Brother of North Korean Dictator Kim Jong-un? The Telegraph. 2017. Available online: https://www.telegraph.co.uk/news/2017/02/14/profile-kim-jong-nam-exiled-half-brother-north-korean-dictator/ (accessed on 30 June 2022).
- Otto, B.; Ngui, Y. How the Hit Team Came Together to Kill Kim Jong Nam. Wall Str. J. 2017. Available online: https://www.wsj.com/articles/emerging-details-point-to-north-korean-plot-in-scions-killing-1487787023 (accessed on 30 June 2022).
- Sang-Hun, C. Kim Jong-nam, the Hunted Heir to a Dictator Who Met Death in Exile-The New York Times. Wall Str. J. 2017. Available online: https://www.nytimes.com/2017/02/15/world/asia/kim-jong-nam-assassination-north-korea.html (accessed on 30 June 2022).
- Ng, E. Post-Mortem: VX Poison Killed Brother of North Korean Leader. AP NEWS. 2017. Available online: https://apnews.com/article/90e425dbaf1e44d1ba77e2eea890fc67 (accessed on 30 June 2022).
- Amend, N.; Niessen, K.V.; Seeger, T.; Wille, T.; Worek, F.; Thiermann, H. Diagnostics and treatment of nerve agent poisoning-current status and future developments. Ann. N. Y. Acad. Sci. 2020, 1479, 13–28. [Google Scholar] [CrossRef]
- The Chosun Ilbo (English Edition): Kim Jong-nam Says N. Korean Regime Won’t Last Long. 2012. Available online: http://english.chosun.com/site/data/html_dir/2012/01/17/2012011701790.html (accessed on 30 June 2022).
- Leong, T. Kim Jong Nam Had ‘Constricted, Pinpoint Pupils’ and Other Symptoms of VX Poisoning, Court Hears. SE Asia News & Top Stories-The Straits Times. The Straits Times. 2017. Available online: https://www.straitstimes.com/asia/se-asia/kim-jong-nam-had-no-pulse-when-he-arrived-at-klia-airport-clinic-doctor-tells-court (accessed on 30 June 2022).
- Nakagawa, T.; Tu, A.T. Murders with VX: Aum Shinrikyo in Japan and the assassination of Kim Jong-Nam in Malaysia. Forensic Toxicol. 2018, 36, 542–544. [Google Scholar] [CrossRef]
- ChemIDplus (National Library of Medicine). National Library of Medicine. 2022. Available online: https://chem.nlm.nih.gov/chemidplus/name (accessed on 30 June 2022).
- Moyer, R.A.; Sidell, F.R.; Salem, H. Encyclopedia of Toxicology; Elsevier Inc.: Amsterdam, The Netherlands, 2014. [Google Scholar] [CrossRef]
- Polito, L.; Bortolotti, M.; Battelli, M.; Calafato, G.; Bolognesi, A. Ricin: An ancient story for a timeless plant toxin. Toxins 2019, 11, 324. [Google Scholar] [CrossRef] [PubMed]
- Abbes, M.; Montana, M.; Curti, C.; Vanelle, P. Ricin poisoning: A review on contamination source, diagnosis, treatment, prevention and reporting of ricin poisoning. Toxicon 2021, 195, 86–92. [Google Scholar] [CrossRef]
- Audi, J.; Belson, M.; Patel, M.; Schier, J.; Osterloh, J. Ricin Poisoning. JAMA 2005, 294, 2342–2351. [Google Scholar] [CrossRef] [PubMed]
- Peng, P.W.; Sandler, A.N. A Review of the Use of Fentanyl Analgesia in the Management of Acute Pain in Adults. Anesthesiology 1999, 90, 576–599. [Google Scholar] [CrossRef]
- Pohjanvirta, J.; Tuomisto, R. Short-term toxicity of 2,3,7,8-tetrachlorodibenzo-p-dioxin in laboratory animals: Effects, mechanisms, and animal models. Pharmacol. Rev. 1994, 46, 483–549. [Google Scholar] [PubMed]
- Aylward, L.L.; Brunet, R.C.; Carrier, G.; Hays, S.M.; Cushing, C.A.; Needham, L.L.; Jr, D.G.P.; Gerthoux, P.M.; Brambilla, P.; Mocarelli, P. Concentration-dependent TCDD elimination kinetics in humans: Toxicokinetic modeling for moderately to highly exposed adults from Seveso, Italy, and Vienna, Austria, and impact on dose estimates for the NIOSH cohort. J. Expo. Sci. Environ. Epidemiol. 2005, 15, 51–65. [Google Scholar] [CrossRef]
- Le, M.H. Polonium 210, exposed. J. Med Toxicol. 2007, 3, 82–84. [Google Scholar] [CrossRef] [PubMed]
- Bide, D.J.; Risk, R.W. Inhalation Toxicity of Aerosolized Nerve Agents. 1. VX Revisited; Technical Report DRES-TR 2000-063; National Academies Press: Suffield, AB, Canada, 2000. [Google Scholar]
- Munro, N. Toxicity of the Organophosphate Chemical Warfare Agents GA, GB, and VX: Implications for Public Protection. Environ. Health Perspect. 1994, 102, 18–37. [Google Scholar] [CrossRef]
- Gratte, J.H.; Yang, L.I. Report of the Workshop on Chemical Agent Toxicity for Acute Effects, Institute for Defense Analyses, 11–12 May 1998; National Technical Reports Library: Alexandria, VA, USA, 2001.
- Ganie, S.Y.; Javaid, D.; Hajam, Y.A.; Reshi, M.S. Mechanisms and treatment strategies of organophosphate pesticide induced neurotoxicity in humans: A critical appraisal. Toxicology 2022, 472, 153181. [Google Scholar] [CrossRef]
- Moshiri, M.; Hamid, F.; Etemad, L. Ricin Toxicity: Clinical and Molecular Aspects. Rep. Biochem. Mol. Biol. 2016, 4, 60–65. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4986263/ (accessed on 30 June 2022). [PubMed]
- The Centers for Disease Control. HHS and USDA Select Agents and Toxins 7 CFR Part 331, 9 CFR Part 121, and 42 CFR Part 73. 2012; Volume 1, p. 2012. Available online: https://www.selectagents.gov/ (accessed on 30 June 2022).
- US Environmental Protection Agency. 40 C.F.R.: Appendix A to Part 355—The List of Extremely Hazardous Substances and Their Threshold Planning Quantities; U.S. Government Publishing Office: Washington, DC, USA, 2008; Volume 50, pp. 437–442.
- National Select Agent Registry. Permissible Toxin Amounts. 2017. Available online: https://www.selectagents.gov/sat/permissible.htm?CDC_AA_refVal=https%3A%2F%2Fwww.selectagents.gov%2FPermissibleToxinAmounts.html (accessed on 28 July 2022).
- Bozza, W.P.; Tolleson, W.H.; Rosado, L.A.R.; Zhang, B. Ricin detection: Tracking active toxin. Biotechnol. Adv. 2015, 33, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Coppock, R.W.; Dziwenka, M. Potential Agents That Can Cause Contamination of Animal Feedstuffs and Terror; Elsevier Inc.: Amsterdam, The Netherlands, 2015. [Google Scholar] [CrossRef]
- Falach, R.; Sapoznikov, A.; Evgy, Y.; Aftalion, M.; Makovitzki, A.; Agami, A.; Mimran, A.; Lerer, E.; Ben David, A.; Zichel, R.; et al. Post-Exposure Anti-Ricin Treatment Protects Swine against Lethal Systemic and Pulmonary Exposures. Toxins 2020, 12, 354. [Google Scholar] [CrossRef]
- Sisco, E.; Verkouteren, J.; Staymates, J.; Lawrence, J. Rapid detection of fentanyl, fentanyl analogues, and opioids for on-site or laboratory based drug seizure screening using thermal desorption DART-MS and ion mobility spectrometry. Forensic Chem. 2017, 4, 108–115. [Google Scholar] [CrossRef]
- International Narcotics Control Board (INCB). Narcotic Drug Report. United Nations, 2022. Available online: https://www.incb.org/incb/en/narcotic-drugs/Technical_Reports/2021/narcotic-drugs-technical-report-2021.html (accessed on 30 June 2022).
- Dziennik Urzędowy Ministra Zdrowia. Urzędowy Wykaz Produktów Leczniczych Dopuszczonych do Obrotu na Terytorium Rzeczypospolitej Polskiej. 2016. Available online: https://isap.sejm.gov.pl/isap.nsf/DocDetails.xsp?id=WDU20180001591 (accessed on 30 June 2022).
- National Institue on Drug Abuse. Overdose Death Rates. 2022. Available online: https://nida.nih.gov/research-topics/trends-statistics/overdose-death-rates (accessed on 29 July 2022).
- Drug Enforcement Agency (DEA). Fentanyl Flow to the United States (DEA-DCT-DIR-008-20). 2020; pp. 1–4. Available online: https://www.dea.gov/sites/default/files/2020-03/DEA_GOV_DIR-008-20 Fentanyl Flow in the United States_0.pdf (accessed on 30 June 2022).
- Boyer, E.W. Management of Opioid Analgesic Overdose. N. Engl. J. Med. 2012, 367, 146–155. [Google Scholar] [CrossRef]
- Greig, J.B. Veterans and Agent Orange: Health Effects of Herbicides Used in Vietnam. Occup. Environ. Med. 1995, 52, 144. [Google Scholar] [CrossRef]
- U.S. Environmental Protection Agency US EPA. EPA’s Reanalysis of Key Issues Related to Dioxin Toxicity and Response to NAS Comments. Support Summ. Inf. Integr. Risk Inf. Syst. 2012, 1. Available online: http://hero.epa.gov/index.cfm?action=reference.details&reference_id=543766%5Cnpapers2://publication/uuid/F27D8F6C-CE69-43C0-93C0-015427C58A6A (accessed on 30 June 2022).
- Saracci, R.; Kogevinas, M.; Winkelmann, R.; Bertazzi, P.; de Mesquita, B.B.; Coggon, D.; Green, L.; Kauppinen, T.; L’Abbé, K.; Littorin, M.; et al. Cancer mortality in workers exposed to chlorophenoxy herbicides and chlorophenols. Lancet 1991, 338, 1027–1032. [Google Scholar] [CrossRef]
- Pohjanvirta, R.; Viluksela, M. Novel Aspects of Toxicity Mechanisms of Dioxins and Related Compounds. Int. J. Mol. Sci. 2020, 21, 2342. [Google Scholar] [CrossRef]
- Mimura, J.; Fujii-Kuriyama, Y. Functional role of AhR in the expression of toxic effects by TCDD. Biochim. Biophys. Acta 2003, 1619, 263–268. [Google Scholar] [CrossRef]
- Geusau, A.; Schmaldienst, S.; Derfler, K.; Päpke, O.; Abraham, K. Severe 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) intoxication: Kinetics and trials to enhance elimination in two patients. Arch. Toxicol. 2002, 76, 316–325. [Google Scholar] [CrossRef]
- Geusau, A.; Tschachler, E.; Meixner, M.; Sandermann, S.; Päpke, O.; Wolf, C.; Valic, E.; Stingl, G.; McLachlan, M. Olestra increases faecal excretion of 2,3,7,8-tetrachlorodibenzo-p-dioxin. Lancet 1999, 354, 1266–1267. [Google Scholar] [CrossRef]
- Sorg, O.; Zennegg, M.; Schmid, P.; Fedosyuk, R.; Valikhnovskyi, R.; Gaide, O.; Kniazevych, V.; Saurat, J.-H. 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) poisoning in Victor Yushchenko: Identification and measurement of TCDD metabolites. Lancet 2009, 374, 1179–1185. [Google Scholar] [CrossRef]
- Harrison, J.; Fell, T.; Leggett, R.; Lloyd, D.; Puncher, M.; Youngman, M. The polonium-210 poisoning of Mr Alexander Litvinenko. J. Radiol. Prot. 2017, 37, 266–278. [Google Scholar] [CrossRef] [PubMed]
- Jefferson, R.D.; Goans, R.E.; Blain, P.G.; Thomas, S.H. Diagnosis and treatment of polonium poisoning. Clin. Toxicol. 2009, 47, 379–392. [Google Scholar] [CrossRef]
- Carvalho, F.P. Pesticides, environment, and food safety. Food Energy Secur. 2017, 6, 48–60. [Google Scholar] [CrossRef]
- Bastian, R.; Bachmaier, J.; Schmidt, D.; Salomon, S.; Jones, A.; Chiu, W.; Setlow, L.; Wolbarst, A.; Yu, C.; Goodman, J.; et al. Radioactive Materials in Biosolids: National Survey, Dose Modeling & POTW Guidance. Proc. Water Environ. Fed. 2004, 2004, 777–803. [Google Scholar] [CrossRef]
- The U.S. Nuclear Regulatory Commission (NRC). Polonium-210. June 2019. Available online: https://www.nrc.gov/reading-rm/doc-collections/fact-sheets/polonium.html (accessed on 29 July 2022).
- Bagnall, K.W. The Chemistry of Polonium. Adv. Inorg. Chem. Radiochem. 1962, 4, 197–226. [Google Scholar]
- Vardell, E. Chemical Hazards Emergency Medical Management (CHEMM). Med Ref. Serv. Q. 2012, 31, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.C. Handbook of Toxicology of Chemical Warfare Agents, 2nd ed.; Academic Press: Cambridge, MA, USA, 2015. [Google Scholar] [CrossRef]
- Organisation for the Prohibition of Chemical Weapons (OPCW). Convention on the Prohibition of the Development, Production, Stockpiling and Use of Chemical Weapons and on their Destruction. Chem. Eng. News 2001, 79, 23. Available online: https://www.opcw.org/chemical-weapons-convention/download-convention (accessed on 30 June 2022).
- Tsuchihashi, H.; Katagi, M.; Nishikawa, M.; Tatsuno, M. Identification of metabolites of nerve agent VX in serum collected from a victim. J. Anal. Toxicol. 1998, 22, 383–388. [Google Scholar] [CrossRef]
- Dachir, S.; Cohen, M.; Buch, H.; Kadar, T. Skin decontamination efficacy of sulfur mustard and VX in the pig model: A comparison between Fuller’s earth and RSDL. Chem. Interact. 2021, 336, 109393. [Google Scholar] [CrossRef]
- Katos, A.M.; Conti, M.L.; Moran, T.S.; Gordon, R.K.; Doctor, B.P.; Sciuto, A.M.; Nambiar, M.P. Abdominal bloating and irritable bowel syndrome like symptoms following microinstillation inhalation exposure to chemical warfare nerve agent VX in guinea pigs. Toxicol. Ind. Health 2007, 23, 231–240. [Google Scholar] [CrossRef]
- Keisar, O.R.; Nahum, V.; Yehezkel, L.; Marcovitch, I.; Columbus, I.; Fridkin, G.; Chen, R. Active and Strippable PVA/Borax/NaBO3 Hydrogel for Effective Containment and Decontamination of Chemical Warfare Agents. ACS Omega 2021, 6, 5359–5367. [Google Scholar] [CrossRef]
- Thors, L.; Wästerby, P.; Wigenstam, E.; Larsson, A.; Öberg, L.; Bucht, A. Do cold weather temperatures affect the efficacy of skin decontamination? . J. Appl. Toxicol. 2022, 42, 961–969. [Google Scholar] [CrossRef]
- CDC. Facts About VX. Centers for Disease Control and Prevention. Available online: https://emergency.cdc.gov/agent/vx/basics/facts.asp (accessed on 21 January 2021).
- Dong, J.; Sun, X.; Zhen, N.; Li, Z.; Liu, D.; Zou, B.; Dai, Q.; Chi, Y.; Chen, S.-L.; Poblet, J.M.; et al. Oxidative detoxification of nerve agent VX simulant by polyoxoniobate: Experimental and theoretical insights. J. Catal. 2021, 394, 83–93. [Google Scholar] [CrossRef]
- Kentrop, J.; Savransky, V.; Klaassen, S.D.; van Groningen, T.; Bohnert, S.; Cornelissen, A.S.; Cochrane, L.; Barry, J.; Joosen, M.J. Pharmacokinetics and efficacy of atropine sulfate/obidoxime chloride co-formulation against VX in a guinea pig model. Regul. Toxicol. Pharmacol. 2020, 119, 104823. [Google Scholar] [CrossRef]
- Newmark, J. Therapy for acute nerve agent poisoning. Neurol. Clin. Pract. 2019, 9, 337–342. [Google Scholar] [CrossRef] [PubMed]
- Chemical Hazards Emergency Medical Management (CHEMM), The U.S. Department of Health and Human Services. Fourth Generation Agents Hospital-Medical Management Guidelines. January 2019. Available online: https://chemm.hhs.gov/nerveagents/FGAMMGHospital.htm (accessed on 30 June 2022).
- Lee, J.Y.; Kim, C.; Lee, Y.H. Simultaneous Time-concentration Analysis of Soman and VX Adducts to Butyrylcholinesterase and Albumin by LC–MS-MS. J. Anal. Toxicol. 2018, 42, 293–299. [Google Scholar] [CrossRef]
- Takahashi, F.; Kazui, Y.; Miyaguchi, H.; Ohmori, T.; Tanaka, R.; Jin, J. Simple colorimetric screening of the nerve agent VX using gold nanoparticles and a hand-powered extraction device. Sens. Actuators B Chem. 2020, 327, 128902. [Google Scholar] [CrossRef]
- Stefanidou, M.; Athanaselis, S.; Spiliopoulou, H. Butyrylcholinesterase: Biomarker for exposure to organophosphorus insecticides. Intern. Med. J. 2009, 39, 57–60. [Google Scholar] [CrossRef] [PubMed]
- Katagi, M.; Tsuchihashi, H. VX and its decomposition products. In Drugs and Poisons in Humans; Springer: Berlin/Heidelberg, Germany, 2005; Volume 8, pp. 619–627. [Google Scholar] [CrossRef]
- ChemSee. Detectors for Pesticides and Warefare Chemicals. Available online: https://www.chemsee.com/commercial/toxic-gas/available-products/warefare-chemicals/ (accessed on 30 June 2022).
- Securetec Detektions-Systeme, A.G. Rapid Test Cholinesterase ChE Check Mobile. Available online: https://www.securetec.net/en/products/rapid-test-determination-cholinesterase-che-check-mobile (accessed on 31 January 2021).
- Franca, T.C.C.; Kitagawa, D.A.S.; Cavalcante, S.F.D.A.; da Silva, J.A.V.; Nepovimova, E.; Kuca, K. Novichoks: The Dangerous Fourth Generation of Chemical Weapons. Int. J. Mol. Sci. 2019, 20, 1222. [Google Scholar] [CrossRef] [PubMed]
- Castelvecchi, D. Novichok Nerve Agents Banned by Chemical-Weapons Treaty. Nature 2019. Available online: https://www.nature.com/articles/d41586-019-03686-y (accessed on 29 July 2022).
- Kloske, M.; Urbanowicza, U.W. Novichok Agents and A Substances. Chem. News 2018, 72, 9–10. [Google Scholar]
- Chai, P.R.; Hayes, B.D.; Erickson, T.B.; Boyer, E.W. Novichok agents: A historical, current, and toxicological perspective. Toxicol. Commun. 2018, 2, 45–48. [Google Scholar] [CrossRef]
- Nepovimova, E.; Kuca, K. Chemical warfare agent NOVICHOK-mini-review of available data. Food Chem. Toxicol. 2018, 121, 343–350. [Google Scholar] [CrossRef]
- Steindl, D.; Boehmerle, W.; Körner, R.; Praeger, D.; Haug, M.; Nee, J.; Schreiber, A.; Scheibe, F.; Demin, K.; Jacoby, P.; et al. Novichok nerve agent poisoning. Lancet 2020, 397, 249–252. [Google Scholar] [CrossRef]
- John, H.; Thiermann, H. Poisoning by organophosphorus nerve agents and pesticides: An overview of the principle strategies and current progress of mass spectrometry-based procedures for verification. J. Mass Spectrom. Adv. Clin. Lab 2021, 19, 20–31. [Google Scholar] [CrossRef]
- Tu, A.T. The use of VX as a terrorist agent: Action by Aum Shinrikyo of Japan and the death of Kim Jong-Nam in Malaysia: Four case studies. Glob. Secur. Health Sci. Policy 2020, 5, 48–56. [Google Scholar] [CrossRef]
- Wille, T.; Djordjević, S.; Worek, F.; Thiermann, H.; Vučinić, S. Early diagnosis of nerve agent exposure with a mobile test kit and implications for medical countermeasures: A trigger to react. BMJ Mil. Health 2020, 166, 99–102. [Google Scholar] [CrossRef] [PubMed]



| Substance Properties | Estimated Likelihood of Use in | Effect | |
|---|---|---|---|
| Acute Poisonings | Chronic Poisonings | ||
| Tasteless and colorless | high | high | Possibility of an unnoticed administration. |
| Well soluble in water | high | high | Easy administration, quick absorption and distribution. |
| Well soluble in fats | high | very high | Possible accumulation in the fatty tissue, as well as slow release from it. |
| Delayed effect onset | high | very high | Impedes detection of the perpetrator and assessment of true time and place of intoxication. |
| Unusual and difficult to detect | very high | very high | Impedes crime detection. |
| Low lethal dose | very high | very high | Facilitates poisoning by making a low dose necessary to cause death. |
| Easy access to the substance | low | high | Facilitates crime. |
| Chemically stable | high | very high | Facilitates storage and transport of the poison. |
| Quickly degradable after death | high | high | Impedes identification of the poison and the cause of death. |
| Occurring naturally within the body | high | high | Does not arouse suspicion in case of detection. |
| Occurring naturally in the burial place | low | low | Presence within the corpse does not arouse suspicion of poisoning. |
| Poison, Victim of Poisoning (Time, Place and Died/Survived after Poisoning) | Case Description | Symptoms of Poisoning, Treatment Undertaken, Results of Autopsy |
|---|---|---|
| Ricin, Georgi Ivanov Markov (11 September 1978, London, UK, died) [2,6,7] | A month before his death, while visiting a friend in Germany, Markov remembered an anonymous phone call (three months ago) that had threatened him with death if he continued to write broadcasts for Radio Free Europe. The last script Markov prepared for this radio was a text from July 1978—“The Mind Under House Arrest”, in which he accused Bulgarian radio commentators of cowardice and inability to express their own opinions. On 7 September 1978 (the 67th birthday of Bulgarian leader Todor Zhivkov), at circa 1.30 PM, Markov was waiting at the bus stop at the southern end of the Waterloo Bridge. Suddenly he felt pain in the back of his right thigh. As he turned, he saw a man bending down to get a dropped umbrella. The stranger, with a foreign accent, apologized to him for his clumsiness, then took a cab away. At first, Markov didn’t notice the whole thing until someone in the office told him about the red stain on the back of his pants. When Markov looked at the leg, he saw a red dot on his thigh. He assumed that the change would soon disappear and paid no attention to it. | Markov felt weakness 5 h after the incident. Then there was: fever and vomiting. The next day, the patient was admitted to St. James in Balhama. He had a high fever at the time and complained of abdominal pain, vomiting and diarrhea. After the examination, he was found to have enlarged, painful lymph nodes in his right groin, and a swelling of about 6 cm in diameter was observed on the posterior surface of the right thigh. The next day, the patient’s condition deteriorated—heart rate increased to 160 bpm, blood pressure dropped and increased sweating appeared. Symptoms indicated the development of septic shock. In morphology, an increase in leukocytosis was observed. Further symptoms were diuresis stopped and blood appeared in the vomit. The ECG (performed on 11 September 1978) revealed a complete atrioventricular block with numerous ventricular beats. On the same day, the patient had a cardiac arrest. During the autopsy performed on 12 September 1978, only a small mark on the back of the thigh was found. During internal examination, pulmonary edema resulting from heart failure, mild fatty liver, hemorrhagic necrosis of the small intestine and hemorrhagic lymph nodes in the right groin were found. Necrosis has also been observed in the testes, pancreas, and inguinal lymph nodes. Microscopic examination revealed small hemorrhagic foci in the myocardium. During the autopsy, a small metal ball with a diameter of about 1.5 mm was found, which fell out of the fragment of the thigh collected for examination. Two holes were drilled in the ball—one was open and the other was blind. It was found that the holes would be able to hold about 500 mg of a substance that could have contributed to Markov’s death. Already during the autopsy, it was suspected that the cause of death was not septic shock but poisoning with the toxin placed in the ball. |
| Fentanyl, Khaled Meshal (25 September 1997, Amman, Jordan, survived) | Khaled Mashal was a leader of the Palestinian political-military organization Hamas, which had been battling Israel for many years (especially in the area of Gaza Strip). Numerous suicide bombings conducted by the Hamas fundamentalists had led to the order of killing the Palestinian politician given by the authorities of Israel. On 25 September 1997 Meshal was attacked by two men from an Israeli intelligence—Mossad. The attack was carried out by spraying a toxic substance into the victims’ ear. | One of the first symptoms experienced by the victim was tinnitus and a sensation of an electrical current going through his body. After approximately 2 h he started feeling nauseous, short of breath and started vomiting soon after. He was admitted to a hospital where, due to acute respiratory failure, he needed a mechanical ventilation. Meshal’s condition improved only after administering the antidote (naloxone) provided by the Israeli authorities. |
| TCDD (2,3,7,8-tetrachlorodibenzo-p-dioxin), Viktor Andriyovych Yushchenko (5 August 2004, Kyiv, Ukraine, survived) [2] | Viktor Yushchenko, a political activist in opposition to pro-Russian political groups, and a candidate for president of Ukraine in the presidential election. On the day of the incident after dinner with Igor Smeshko (head of the Security Service), Yushchenko felt bad. Viktor Yushchenko’s wife said that on the evening of poisoning she felt a strange taste of “medicine” when kissing her husband. Viktor Yushchenko survived. Dose of absorbed poison estimated at approx. 1.5–2.5 mg TCDD. | Within hours of the exposure, Yushchenko developed nausea, vomiting and abdominal pain. On 6 August 2004, the patient was diagnosed with food poisoning. Due to the lack of improvement after treatment, the patient was transferred to the Rudolfinerhaus clinic in Vienna. In the clinic, Yushchenko was diagnosed with acute edema pancreatitis, toxic liver damage and gastrointestinal ulceration. After a week of treatment, the patient returned to Ukraine. Unfortunately, after two weeks, due to back pain and “half palsy of the face”, the patient had to be returned to the Viennese clinic. Approximately 3 weeks after the poisoning, the patient developed a characteristic chloracne on his face. Only this symptom led doctors to suspect dioxin poisoning. This suspicion was finally confirmed on 12 December 2004. The concentration of TCDD in the blood of Viktor Yushchenko was 50,000 times higher than the general population’s acceptable level of the above-mentioned substance in blood. During the treatment, attempts were made to accelerate the elimination of the xenobiotic by using orally olestra—an unabsorbed fat substitute. As a result of the measures taken, the half-life of TCDD in the patient’s body was reduced from approx. 7–8 years to approx. 15.4 months. The skin changes resolved within 3–5 years. |
| Isotope of polonium 210Po, Jasir Arafat (11 November 2004, Percy, France, died) [2] | Yassir Arafat was the president of the Palestinian Authority and leader of the liberation movement. Before his death, he was in solitary confinement at the Palestinian Authority headquarters in Ramallah for about 3 years. On 12 October 2004, about 4 h after a meal, he developed severe nausea, vomiting, abdominal pain and then watery diarrhea. On 29 October 2004, the patient was transferred to the French Percy Military Hospital in Clamart, where he was diagnosed with enteritis. Urine tests were negative for gamma-emitting radionuclides. On 11 November 2004, Arafat died of a cerebral hemorrhage. An autopsy was not performed. It was only after the murder of Litvinenko (2006) that it was suggested that the cause of Yassir Arafat’s death could have been polonium-210. As the biological samples collected during the patient’s hospitalization were destroyed in 2008, an exhumation was performed on 27 November 2012, on the basis of which it was found that the hypothesis of Arafat polonium-210 poisoning cannot be fully rejected. | About 4 h after the meal, the patient complained of nausea, vomiting, abdominal pain and watery diarrhea. The studies revealed: presence of megakaryocytes and an increased number of macrophages, enteritis, severe disseminated intravascular coagulation (DIC) with marked thrombocytopenia, cholestatic jaundice and renal failure. Arafat’s death was due to intussusception following a cerebral hemorrhage. |
| Isotope of polonium 210Po, Aleksander Litwinienko (1 November 2006, London, UK, died) [2] | Alexander Litvinenko (pseudonym Edwin Carter) was a former KGB lieutenant colonel. In 2000, he obtained asylum in Great Britain and began working as a consultant in the British intelligence services. On 1 November 2006, Litvinenko met with a former KGB agent. He felt bad after eating sushi. He developed stomachache, vomiting and diarrhea. On 3 November 2006, he presented himself to the Emergency Department of Barnet General Hospital under the pseudonym Edwin Carter. On 10 November 2006, the presence of the toxin Clostridium difficile was identified. In the course of presenting the diagnosis, the patient revealed his true identity and suggested that he may have been poisoned. On 17 November 2006, the results of the screening showed a slightly elevated thallium concentration, but below the toxic dose. Despite this, the patient was treated. Alexander Litvinenko died on 23 November 2006 as a result of cardiac arrest. Shortly after his death, urine samples collected from him on 22 November 2006 were analyzed, and poisoning with polonium-210 was found. | Day: 1–3—stomachache, vomiting, diarrhea, upper abdominal tenderness, slightly elevated urea levels. Day 11—the appearance of a fever. Day 13—alopecia, mucositis, progressive cytopenia. Day 18—jaundice with normal levels of alanine transaminase, bloody vomiting. Day 19—arrhythmias, fever, elevated markers of inflammation. Day 20–22—rapid deterioration in kidney function. Day 22—rash, progressive metabolic acidosis, oliguria, hypothermia, cardiogenic shock, impaired consciousness, cardiac arrest twice. Day 23—cardiac arrest, death. Autopsy results: blood-stained fibrous pericarditis, pleural effusion associated with bilateral pneumonia, ascites, generalized tissue autolysis in most organs, brain unchanged. Estimation of the concentration of polonium-210—4400 MBq. |
| organophosphorus compound VX, Kim Jong-nam (13 February 2017, Kuala Lumpur, Malaysia, died) [2] | Kim Jong-nam, as the eldest son of Kim Jong-Il, was originally being prepared for his successor [8]. As a result of a diplomatic scandal, his half-brother Kim Jong-Un seized power in North Korea and ordered his relative killed [9,10]. Jong-nam was poisoned at Kuala Lumpur Airport. The killing was carried out by two women. Within 7 s, each applied a poisoned handkerchief to his face [11,12,13]. | After the attack, Kim reported to an airport medical facility. There he observed: trembling hands, hyperhidrosis and weakness [11]. During a physical exam, Jong-nam showed symptoms of cholinergic syndrome [14]. He then received 1 mg of atropine and adrenaline. Due to respiratory failure, he was intubated and connected to a ventilator. The death occurred 20 min after the attack. The autopsy report is probably not available to the public [15]. |
| Novichok-type organophosphorus compound, Sergei Skripal (4 March 2018, London, UK, survived) [2] | Sergei Skripal became famous as a Russian military intelligence officer who in the 1990s decided to become a double agent for the British intelligence services. He obtained secret information while working at increasingly senior levels of the GRU and later also in government institutions. In December 2004, he was arrested and convicted of treason by a Moscow military court. In 2010, as part of a spy exchange between the Russian Federation and the United Kingdom, Skripal was transported to England, and he settled in Salisbury. Despite being exposed, he continued to cooperate with Western intelligence agencies. On 4 March 2018 Sergei Skripal and his daughter Yulia were found unconscious on a park bench in Salisbury. An investigation by British services found that they were poisoned by two GRU officers, Anatoly Chepiga and Alexander Mishkin, who sprayed the Novichok agent on the doorknob and front door of Skripal’s home. Traces of Novichok were also found in the pub where the Skripals spent the afternoon. The perfume bottle used by the agents as a container for the poison was then dumped in a container for donations to the needy. It was found by a random British man, Charlie Rowley, and given to his partner Dawn Sturgess. The woman died shortly after spraying her wrists with the substance contained therein. Despite wearing a full protective suit, a police officer searching Skripal’s home was admitted to hospital in serious condition. Investigators later determined that the bottle used in the incident contained enough Novichok to kill thousands of people. Specialists identified the agent used as most likely A-234. | According to the testimony of witnesses present at the scene, Sergei and Yulia Skripal were unconscious. Foam was coming out of Yulia’s mouth. On admission to hospital, the condition of both was described as critical. Due to the characteristic symptoms, treatment with atropine was immediately started, and anticonvulsants were included. The patients’ condition improved gradually. Yulia Skripal left the hospital on 9 April 2018, and her father on 18 May 2018. After the inspection, access to the interior of Skripal’s house was secured. Scaffolding was erected around the building, on which special protections were placed. It took about 4 months to strip the roof, clean the house and rebuild it. All vehicles involved in the incident, including ambulances and police cars, were disposed of and buried in the Cheltenham landfill. It has long been questioned how Skripals managed to survive the attack despite being exposed to such a high dose of A-234. Both one of the Novichok developers and other scientists agreed that weather played a significant role in the case. On the day of the Skripals’ poisoning in Salisbury, it was humid and foggy, and humidity reduces the harmfulness of this type of poison. It is worth noting that the weather conditions only hindered the poison’s absorption, not its toxicity per se. Skripals were also inadvertently helped by the agents who tried to liquidate them. To help Novichok stick to various surfaces, including skin, it was mixed with a gel-like substance. This agent slowed down the absorption of the poison into the body which made it possible to apply effective treatment. |
| Novichok-type organophosphorus compound, Alexei Navalny (20 August 2020, Tomsk, Russia, survived) | Alexei Navalny, leader of the Russian opposition, chairman of the Russia of the Future party and founder of the Foundation for the Fight against Corruption, has for many years strongly criticized the policies pursued by Vladimir Putin and his United Russia party. On 20 August 2020, Navalny boarded a flight from Tomsk to Moscow. During the flight his well-being suddenly deteriorated. Therefore, the pilots decided to make an emergency landing in Omsk and transport the patient to a local hospital. Navalny was successfully transported to the Charité hospital in Berlin on 22 August 2020. Navalny’s subsequent investigation revealed that Novichok had been sewn by FSB agents into the seams in his underwear left in his hotel room. | The first symptoms noticed in Navalny were pallor, intense sweating, drooling, vomiting and loss of consciousness. Doctors at the Omsk hospital quickly suspected poisoning with an agent from the acetylcholinesterase inhibitor group. Navalny was put into a coma, intubated, mechanically ventilated. The patient was also administered atropine. On admission to Charite Hospital, the patient was additionally observed to have hypothermia, bradycardia, impaired trunk reflexes, exaggerated tendon reflexes and pyramidal symptoms. Initial investigations confirmed that the patient had been poisoned with a paralytic agent from the cholinesterase inhibitor group. Laboratory evidence confirmed reduced butyrylcholinesterase levels in the patient’s blood. Based on samples sent to a specialized unit, Novichok was confirmed in blood, urine and on Navalny’s skin. The treatment included atropine and obidoxime. The patient left the hospital on his own after 33 days, including 24 days of respiratory therapy. |
| Toxic Substance (CAS) | Physicochemical Properties | Toxicological Properties | Refs. | |
|---|---|---|---|---|
| Lethal/Incapacitating Dose [mg⋅min−1⋅m−3] | Time of Death [h] | |||
| Ricin (9009-86-3) | White powder. It can be prepared in liquid/crystalline form. | Lethal dose:
| Several dozen hours (with p.o. possible delay in absorption up to 5 days) | [16,18,19,20] |
| Fentanyl (437-38-7) | Crystal-like solid, moderately water-soluble | Lethal dose:
| [16,21] | |
| TCDD (108-88-3) | Crystalline, colorless solid, soluble in organic solvents, hydrophobic | Lethal dose LD50:
| From several days to several weeks | [16,22,23] |
| Isotope of polonium 210Po | Radioactive metal, soluble in water, forming simple salts in dilute acids | Lethal dose LD50:
| From 2–3 weeks after the onset of symptoms | [16,24] |
| organophosphorus compound VX (50782-69-9) | Amber to transparent oily liquid, slightly soluble in water | Lethal dose (predicted):
| A few to several minutes—bronchospasm | [16,25,26,27] |
| organophosphorus compound Novichok (no clear identification of the compound) | Liquid, fine powder, no details available | For A-230 (estimated for human): LCt50—1.9–3 mg-min/m3 LD50—7.5 × 10−4 − 0.002 g/70 kg body weight Dla A-232 (estimated for human): LCt50—7 mg-min/m3 LD50—0.035 g/70 kg body weight Dla A-234 (estimated for human): LCt50—7 mg-min/m3 LD50—0.035 g/70 kg body weight | [16,28] | |
| No. | Stages during Treatment of 210Po Intoxication by the Oral Route |
|---|---|
| 1 | Gastric lavage—effective up to an hour after ingestion; reduces the risk of absorption. |
| 2 | Antiemetics, intravenous fluids, analgesics. |
| 3 | Treatment of bone marrow failure—application of colony simulations; in severe thrombocytopenia and anemia:
|
| 4 | Chelation therapy—reduces the retention of radiation in the blood and organs but increases retention in the kidneys (sometimes also in the liver and brain).
|
| 5 | Palliative care—In case of high irradiation—relieving symptoms and stress |
| Hospital Treatment of Poisoning with Paralytic and Convulsive Factors in Adults | |||
|---|---|---|---|
| Recommendations | POLISH—As a Procedure in the Case of Cholinergic Syndrome | AMERICAN—Specific for Poisoning with a Substance from the Paralytic and Convulsive Group | |
| Division into age groups | no | yes | |
| Initial activities and their sequence |
| ABCDDS:
| |
| Degree of poisoning | No separation | Mild/medium | Heavy |
| Basic treatment |
|
|
|
| Symptomatic treatment | In convulsions or overstimulation: diazepam 10 mg i.v., repeat as needed | In convulsions, additional doses of benzodiazepines or barbiturates may be used. In bronchospasm, if the desired effect has not been obtained with atropine, inhalation/nebulization with ipratropium and one of the following beta-agonists can be used: SABA—albuterol 2.5 mg/3 mL; terbutaline 1 mg/mL LABA—formoterol 0.02 mg/2 mL, salmeterol (only inhaled) 0.05 mg. If the above treatments are unsuccessful, you can give systemically 1–2 mg/kg methylprednisolone Siarczan magnezu 2 g i.v. | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brunka, Z.; Ryl, J.; Brushtulli, P.; Gromala, D.; Walczak, G.; Zięba, S.; Pieśniak, D.; Sein Anand, J.; Wiergowski, M. Selected Political Criminal Poisonings in the Years 1978–2020: Detection and Treatment. Toxics 2022, 10, 468. https://doi.org/10.3390/toxics10080468
Brunka Z, Ryl J, Brushtulli P, Gromala D, Walczak G, Zięba S, Pieśniak D, Sein Anand J, Wiergowski M. Selected Political Criminal Poisonings in the Years 1978–2020: Detection and Treatment. Toxics. 2022; 10(8):468. https://doi.org/10.3390/toxics10080468
Chicago/Turabian StyleBrunka, Zuzanna, Jan Ryl, Piotr Brushtulli, Daria Gromala, Grzegorz Walczak, Sonia Zięba, Dorota Pieśniak, Jacek Sein Anand, and Marek Wiergowski. 2022. "Selected Political Criminal Poisonings in the Years 1978–2020: Detection and Treatment" Toxics 10, no. 8: 468. https://doi.org/10.3390/toxics10080468
APA StyleBrunka, Z., Ryl, J., Brushtulli, P., Gromala, D., Walczak, G., Zięba, S., Pieśniak, D., Sein Anand, J., & Wiergowski, M. (2022). Selected Political Criminal Poisonings in the Years 1978–2020: Detection and Treatment. Toxics, 10(8), 468. https://doi.org/10.3390/toxics10080468






