Food Preservatives and the Rising Tide of Early-Onset Colorectal Cancer: Mechanisms, Controversies, and Emerging Innovations
Abstract
1. Introduction
2. Historical Background of Food Preservatives
2.1. Development of Preservatives in the Food Industry
2.2. Types of Synthetic and Natural Preservatives
2.3. Regulatory Oversight and Classification Systems (e.g., EFSA, FDA)
2.4. The Rise of Natural Preservatives as Alternatives
2.5. Consumption Patterns of Preservatives
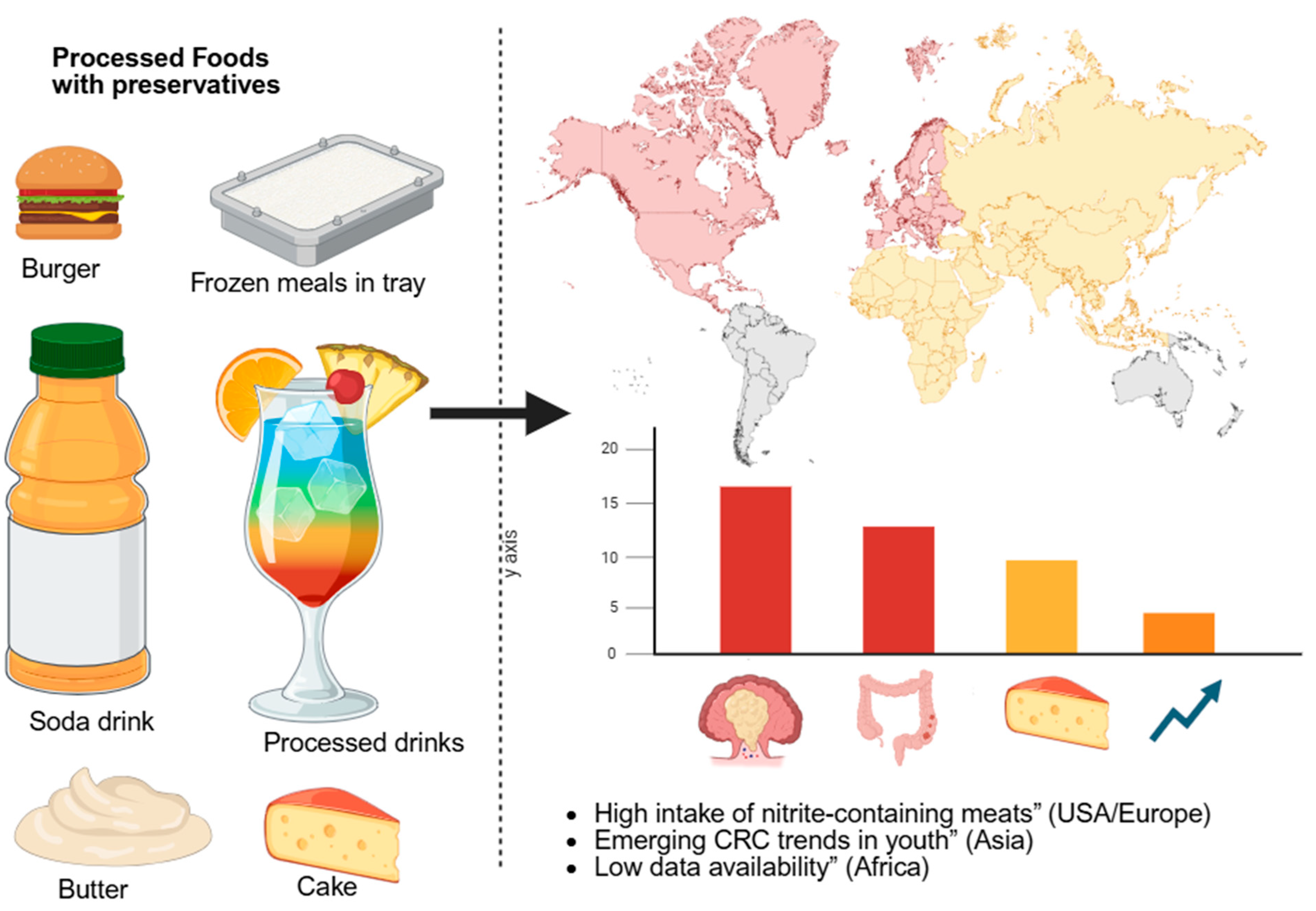
3. Epidemiological Link Between Food Preservatives and EOCRC
3.1. Review of Population-Based Studies (USA, Europe, Asia, Africa)
3.2. Case Studies and Global Statistics on EOCRC Trends
3.3. Regional Diets High in Processed Foods vs. Cancer Prevalence
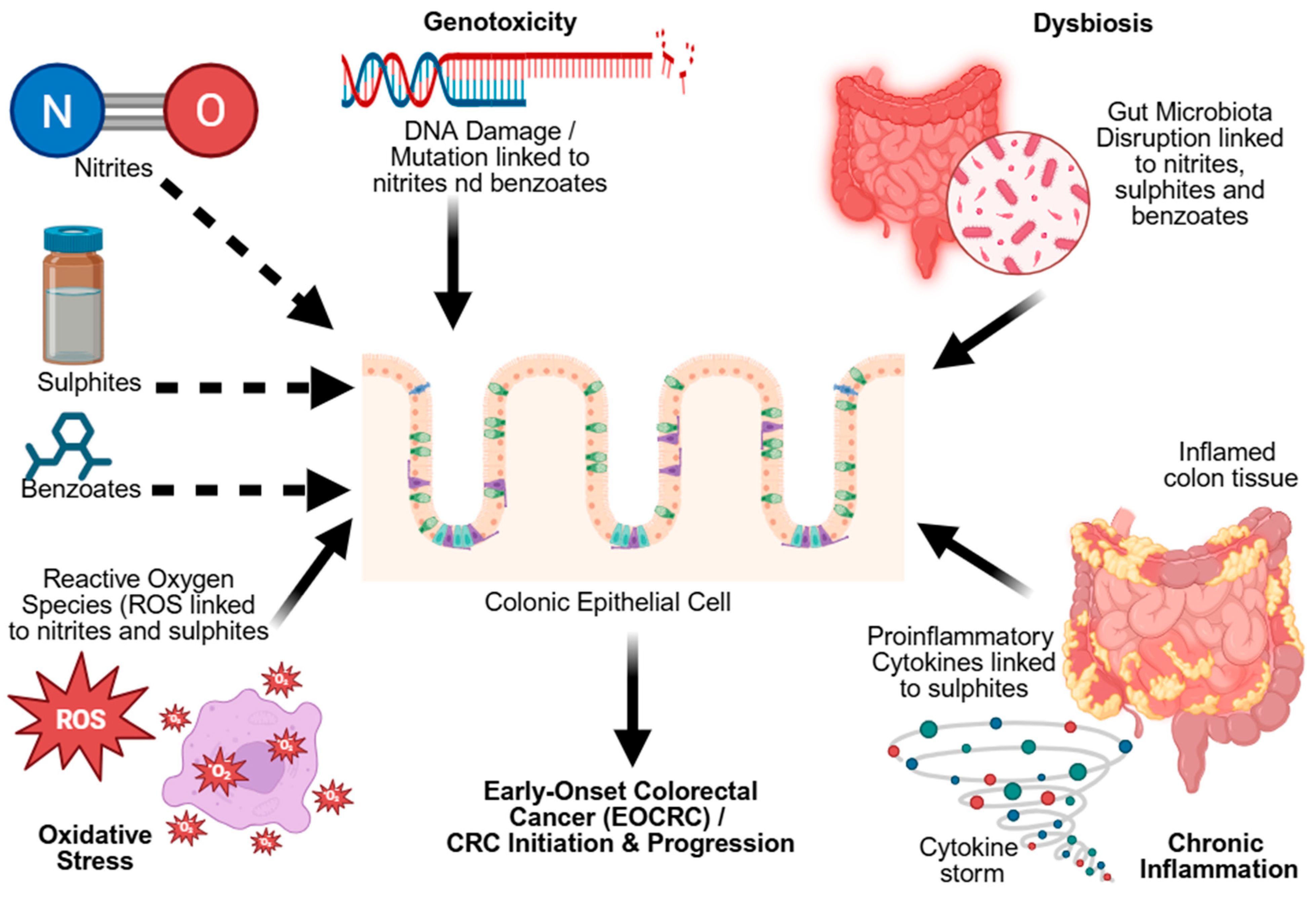
4. Molecular Mechanisms Linking Preservatives to EOCRC
4.1. Genotoxic and Carcinogenic Effects
4.2. Microbiota Dysbiosis and Metabolic Disruption
4.3. Oxidative Stress and Inflammation
4.4. Immune Modulation and Chronic Inflammation
5. Critical Evaluation of Current Studies and Findings
5.1. Conflicting Findings and Ongoing Scientific Debates
5.2. Strengths and Weaknesses in Research Methodologies
5.3. Gaps and Inconsistencies in the Scientific Literature
5.4. In Vitro Evidence
5.5. Animal Studies
5.6. Human Studies
6. Case Studies
6.1. Evidence from Specific Populations and Experimental Models Linking Diet to EOCRC
6.2. Traditional vs. Preserved Food Patterns in Young Adults Diagnosed with CRC
7. Innovations in Preservative Alternatives
Limitations of Natural Preservatives
8. Challenges and Limitations
9. Future Directions
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gandini, A.; Taieb, J.; Blons, H.; Netter, J.; Laurent-Puig, P.; Gallois, C. Early-Onset colorectal Cancer: From the laboratory to the clinic. Cancer Treat. Rev. 2024, 130, 102821. [Google Scholar] [CrossRef]
- Dharwadkar, P.; Zaki, T.A.; Murphy, C.C. Colorectal Cancer in Younger Adults. Hematol. Oncol. Clin. N. Am. 2022, 36, 449–470. [Google Scholar] [CrossRef]
- Fanzo, J.; Bellows, A.L.; Spiker, M.L.; Thorne-Lyman, A.L.; Bloem, M.W. The importance of food systems and the environment for nutrition. Am. J. Clin. Nutr. 2021, 113, 7–16. [Google Scholar] [CrossRef]
- Onyeaka, H.; Ghosh, S.; Obileke, K.; Miri, T.; Odeyemi, O.A.; Nwaiwu, O.; Tamasiga, P. Preventing chemical contaminants in food: Challenges and prospects for safe and sustainable food production. Food Control 2024, 155, 110040. [Google Scholar] [CrossRef]
- Dey, S.; Nagababu, B.H. Applications of food color and bio-preservatives in the food and its effect on the human health. Food Chem. Adv. 2022, 1, 100019. [Google Scholar] [CrossRef]
- Mafe, A.N.; Edo, G.I.; Makia, R.S.; Joshua, O.A.; Akpoghelie, P.O.; Gaaz, T.S.; Jikah, A.N.; Yousif, E.; Isoje, E.F.; Igbuku, U.A.; et al. A review on food spoilage mechanisms, food borne diseases and commercial aspects of food preservation and processing. Food Chem. Adv. 2024, 5, 100852. [Google Scholar] [CrossRef]
- Julizan, N.; Ishmayana, S.; Zainuddin, A.; Van Hung, P.; Kurnia, D. Potential of Syzygnium polyanthum as Natural Food Preservative: A Review. Foods 2023, 12, 2275. [Google Scholar] [CrossRef]
- Farid, N.; Waheed, A.; Motwani, S. Synthetic and natural antimicrobials as a control against food borne pathogens: A review. Heliyon 2023, 9, e17021. [Google Scholar] [CrossRef] [PubMed]
- Teshome, E.; Forsido, S.F.; Rupasinghe, H.P.V.; Olika Keyata, E. Potentials of Natural Preservatives to Enhance Food Safety and Shelf Life: A Review. Sci. World J. 2022, 2022, 9901018. [Google Scholar] [CrossRef]
- Singh, G.; Chaudhry, Z.; Boyadzhyan, A.; Sasaninia, K.; Rai, V. Dysbiosis and colorectal cancer: Conducive factors, biological and molecular role, and therapeutic prospectives. Explor. Target. Anti-Tumor Ther. 2025, 6, 1002329. [Google Scholar] [CrossRef]
- Vitaloni, M.; Maguet, K.; Carlan, A.; Stack, P.; de Jong, V.; Williams, R.; Maravic, Z. Clinical challenges and patient experiences in early-onset colorectal cancer: Insights from seven European countries. BMC Gastroenterol. 2025, 25, 378. [Google Scholar] [CrossRef] [PubMed]
- Anastasiou, I.A.; Kounatidis, D.; Vallianou, N.G.; Skourtis, A.; Dimitriou, K.; Tzivaki, I.; Tsioulos, G.; Rigatou, A.; Karampela, I.; Dalamaga, M. Beneath the Surface: The Emerging Role of Ultra-Processed Foods in Obesity-Related Cancer. Curr. Oncol. Rep. 2025, 27, 390–414. [Google Scholar] [CrossRef] [PubMed]
- Cave, R.; Cole, J.; Mkrtchyan, H.V. Surveillance and prevalence of antimicrobial resistant bacteria from public settings within urban built environments: Challenges and opportunities for hygiene and infection control. Environ. Int. 2021, 157, 106836. [Google Scholar] [CrossRef] [PubMed]
- Sridhar, A.; Ponnuchamy, M.; Kumar, P.S.; Kapoor, A. Food preservation techniques and nanotechnology for increased shelf life of fruits, vegetables, beverages and spices: A review. Environ. Chem. Lett. 2021, 19, 1715–1735. [Google Scholar] [CrossRef] [PubMed]
- Hassoun, A.; Jagtap, S.; Trollman, H.; Garcia-Garcia, G.; Abdullah, N.A.; Goksen, G.; Bader, F.; Ozogul, F.; Barba, F.J.; Cropotova, J.; et al. Food processing 4.0: Current and future developments spurred by the fourth industrial revolution. Food Control 2023, 145, 109507. [Google Scholar] [CrossRef]
- Musyoka, J.N.; Abong’, G.O.; Mbogo, D.M.; Fuchs, R.; Low, J.; Heck, S.; Muzhingi, T. Effects of Acidification and Preservatives on Microbial Growth during Storage of Orange Fleshed Sweet Potato Puree. Int. J. Food Sci. 2018, 2018, 8410747. [Google Scholar] [CrossRef]
- Habib, M.; Singh, S.; Jan, S.; Jan, K.; Bashir, K. The future of the future foods: Understandings from the past towards SDG-2. npj Sci. Food 2025, 9, 138. [Google Scholar] [CrossRef]
- Abideen, A.Z.; Sundram, V.P.K.; Pyeman, J.; Othman, A.K.; Sorooshian, S. Food Supply Chain Transformation through Technology and Future Research Directions—A Systematic Review. Logistics 2021, 5, 83. [Google Scholar] [CrossRef]
- Lempart-Rapacewicz, A.; Kudlek, E.; Brukało, K.; Rapacewicz, R.; Lempart, Ł.; Dudziak, M. The Threat of Food Additive Occurrence in the Environment—A Case Study on the Example of Swimming Pools. Foods 2023, 12, 1188. [Google Scholar] [CrossRef]
- Rathee, P.; Sehrawat, R.; Rathee, P.; Khatkar, A.; Akkol, E.K.; Khatkar, S.; Redhu, N.; Türkcanoğlu, G.; Sobarzo-Sánchez, E. Polyphenols: Natural Preservatives with Promising Applications in Food, Cosmetics and Pharma Industries; Problems and Toxicity Associated with Synthetic Preservatives; Impact of Misleading Advertisements; Recent Trends in Preservation and Legislation. Materials 2023, 16, 4793. [Google Scholar] [CrossRef]
- Zhou, X.; Qiao, K.; Wu, H.; Zhang, Y. The Impact of Food Additives on the Abundance and Composition of Gut Microbiota. Molecules 2023, 28, 631. [Google Scholar] [CrossRef]
- Arokiyaraj, S.; Dinakarkumar, Y.; Shin, H. A comprehensive overview on the preservation techniques and packaging of processed meat products: Emphasis on natural derivatives. J. King Saud Univ. Sci. 2024, 36, 103032. [Google Scholar] [CrossRef]
- Yen, S.H.Y.; Barrett, E.; Coyle, D.H.; Wu, J.H.Y.; Louie, J.C.Y. The distribution and co-occurrence of food additives in pre-packaged foods in Hong Kong. Food Control 2024, 158, 110210. [Google Scholar] [CrossRef]
- Alamri, M.S.; Qasem, A.A.A.; Mohamed, A.A.; Hussain, S.; Ibraheem, M.A.; Shamlan, G.; Alqah, H.A.; Qasha, A.S. Food packaging’s materials: A food safety perspective. Saudi J. Biol. Sci. 2021, 28, 4490–4499. [Google Scholar] [CrossRef]
- HAMPL, R.; STÁRKA, L. Endocrine Disruptors and Gut Microbiome Interactions. Physiol. Res. 2020, 69, S211–S223. [Google Scholar] [CrossRef] [PubMed]
- Sokal-Dembowska, A.; Jarmakiewicz-Czaja, S.; Tabarkiewicz, J.; Filip, R. Nitrate and Nitrite in the Diet: Protective and Harmful Effects in Health and Disease. Curr. Nutr. Rep. 2025, 14, 89. [Google Scholar] [CrossRef]
- Ritota, M.; Manzi, P. Natural Preservatives from Plant in Cheese Making. Animals 2020, 10, 749. [Google Scholar] [CrossRef]
- Al-Habsi, N.; Al-Khalili, M.; Haque, S.A.; Al Akhzami, N.; Gonzalez-Gonzalez, C.R.; Al Harthi, S.; Al Jufaili, S.M. Herbs and spices as functional food ingredients: A comprehensive review of their therapeutic properties, antioxidant and antimicrobial activities, and applications in food preservation. J. Funct. Foods 2025, 129, 106882. [Google Scholar] [CrossRef]
- Yu, H.H.; Chin, Y.-W.; Paik, H.-D. Application of Natural Preservatives for Meat and Meat Products against Food-Borne Pathogens and Spoilage Bacteria: A Review. Foods 2021, 10, 2418. [Google Scholar] [CrossRef]
- Queiroz, L.P.; Nogueira, I.B.R.; Ribeiro, A.M. Flavor Engineering: A comprehensive review of biological foundations, AI integration, industrial development, and socio-cultural dynamics. Food Res. Int. 2024, 196, 115100. [Google Scholar] [CrossRef] [PubMed]
- Tachie, C.; Nwachukwu, I.D.; Aryee, A.N.A. Trends and innovations in the formulation of plant-based foods. Food Prod. Process. Nutr. 2023, 5, 16. [Google Scholar] [CrossRef]
- Rot, T.; Kovačević, D.; Habschied, K.; Mastanjević, K. N-Nitrosamines in Meat Products: Formation, Detection and Regulatory Challenges. Processes 2025, 13, 1555. [Google Scholar] [CrossRef]
- Shakil, M.H.; Trisha, A.T.; Rahman, M.; Talukdar, S.; Kobun, R.; Huda, N.; Zzaman, W. Nitrites in Cured Meats, Health Risk Issues, Alternatives to Nitrites: A Review. Foods 2022, 11, 3355. [Google Scholar] [CrossRef]
- Irwin, S.V.; Fisher, P.; Graham, E.; Malek, A.; Robidoux, A. Sulfites inhibit the growth of four species of beneficial gut bacteria at concentrations regarded as safe for food. PLoS ONE 2017, 12, e0186629. [Google Scholar] [CrossRef]
- Gulcin, İ. Antioxidants: A comprehensive review. Arch. Toxicol. 2025, 99, 1893–1997. [Google Scholar] [CrossRef]
- Xiao, N.; Ruan, S.; Mo, Q.; Zhao, M.; Feng, F. The Effect of Sodium Benzoate on Host Health: Insight into Physiological Indexes and Gut Microbiota. Foods 2023, 12, 4081. [Google Scholar] [CrossRef]
- Awaad, S.S.; Sherief, M.A.; Mousa, S.M.; Orabi, A.; Abdel-Salam, A.B. A comparative study on the antifungal effect of potassium sorbate, chitosan, and nano-chitosan against Rhodotorula mucilaginosa and Candida albicans in skim milk acid-coagulated (Karish) cheese. Vet. World 2023, 16, 1991–2001. [Google Scholar] [CrossRef]
- Ku, H.-H.; Yang, S.-C.; Hsiao, H.-A.; Chen, J.-S.; Ling, M.-P. Assessing Dietary Exposure Risk to Food Preservatives Among the Eating-Out Population in Taiwan Using the Total Diet Study Method. Foods 2025, 14, 365. [Google Scholar] [CrossRef]
- Zhang, F.; Nan, X.; Wang, H.; Guo, Y.; Xiong, B. Research on the Applications of Calcium Propionate in Dairy Cows: A Review. Animals 2020, 10, 1336. [Google Scholar] [CrossRef]
- Liñán-Atero, R.; Aghababaei, F.; García, S.R.; Hasiri, Z.; Ziogkas, D.; Moreno, A.; Hadidi, M. Clove Essential Oil: Chemical Profile, Biological Activities, Encapsulation Strategies, and Food Applications. Antioxidants 2024, 13, 488. [Google Scholar] [CrossRef]
- Mao, Q.-Q.; Xu, X.-Y.; Cao, S.-Y.; Gan, R.-Y.; Corke, H.; Beta, T.; Li, H.-B. Bioactive Compounds and Bioactivities of Ginger (Zingiber officinale Roscoe). Foods 2019, 8, 185. [Google Scholar] [CrossRef]
- Lahiri, D.; Nag, M.; Dutta, B.; Sarkar, T.; Pati, S.; Basu, D.; Abdul Kari, Z.; Wei, L.S.; Smaoui, S.; Wen Goh, K.; et al. Bacteriocin: A natural approach for food safety and food security. Front. Bioeng. Biotechnol. 2022, 10, 1005918. [Google Scholar] [CrossRef] [PubMed]
- Nieto, G.; Ros, G.; Castillo, J. Antioxidant and Antimicrobial Properties of Rosemary (Rosmarinus officinalis, L.): A Review. Medicines 2018, 5, 98. [Google Scholar] [CrossRef]
- Parveen, B.; Rajinikanth, V.; Narayanan, M. Natural plant antioxidants for food preservation and emerging trends in nutraceutical applications. Discov. Appl. Sci. 2025, 7, 845. [Google Scholar] [CrossRef]
- Karwowska, M.; Kononiuk, A. Nitrates/Nitrites in Food—Risk for Nitrosative Stress and Benefits. Antioxidants 2020, 9, 241. [Google Scholar] [CrossRef]
- Walczak-Nowicka, Ł.J.; Herbet, M. Sodium Benzoate—Harmfulness and Potential Use in Therapies for Disorders Related to the Nervous System: A Review. Nutrients 2022, 14, 1497. [Google Scholar] [CrossRef]
- Nasrollahzadeh, A.; Mokhtari, S.; Khomeiri, M.; Saris, P.E.J. Antifungal Preservation of Food by Lactic Acid Bacteria. Foods 2022, 11, 395. [Google Scholar] [CrossRef]
- Aghababaei, F.; Hadidi, M. Recent Advances in Potential Health Benefits of Quercetin. Pharmaceuticals 2023, 16, 1020. [Google Scholar] [CrossRef]
- Fabbrini, M.; D’Amico, F.; Barone, M.; Conti, G.; Mengoli, M.; Brigidi, P.; Turroni, S. Polyphenol and Tannin Nutraceuticals and Their Metabolites: How the Human Gut Microbiota Influences Their Properties. Biomolecules 2022, 12, 875. [Google Scholar] [CrossRef] [PubMed]
- Sun, W.; Shahrajabian, M.H. Therapeutic Potential of Phenolic Compounds in Medicinal Plants—Natural Health Products for Human Health. Molecules 2023, 28, 1845. [Google Scholar] [CrossRef] [PubMed]
- Masyita, A.; Mustika Sari, R.; Dwi Astuti, A.; Yasir, B.; Rahma Rumata, N.; Emran, T.B.; Nainu, F.; Simal-Gandara, J. Terpenes and terpenoids as main bioactive compounds of essential oils, their roles in human health and potential application as natural food preservatives. Food Chem. X 2022, 13, 100217. [Google Scholar] [CrossRef] [PubMed]
- Barciela, P.; Perez-Vazquez, A.; Prieto, M.A. Azo dyes in the food industry: Features, classification, toxicity, alternatives, and regulation. Food Chem. Toxicol. 2023, 178, 113935. [Google Scholar] [CrossRef]
- Soni, S.; W., A.J.; Kurian, C.; Chakraborty, P.; Paari, K.A. Food additives and contaminants in infant foods: A critical review of their health risk, trends and recent developments. Food Prod. Process. Nutr. 2024, 6, 63. [Google Scholar] [CrossRef]
- Faour-Klingbeil, D.; Todd, E. A Review on the Rising Prevalence of International Standards: Threats or Opportunities for the Agri-Food Produce Sector in Developing Countries, with a Focus on Examples from the MENA Region. Foods 2018, 7, 33. [Google Scholar] [CrossRef]
- Gültekin, F. Food Additives And Microbiota. North Clin. Istanb. 2020, 7, 192–200. [Google Scholar] [CrossRef]
- Campolina, G.A.; Cardoso, M.d.G.; Caetano, A.R.S.; Nelson, D.L.; Ramos, E.M. Essential Oil and Plant Extracts as Preservatives and Natural Antioxidants Applied to Meat and Meat Products: A Review. Food Technol. Biotechnol. 2023, 61, 212–225. [Google Scholar] [CrossRef]
- Venkatesan, U.; Muniyan, R. Review on the extension of shelf life for fruits and vegetables using natural preservatives. Food Sci. Biotechnol. 2024, 33, 2477–2496. [Google Scholar] [CrossRef]
- Chauhan, K.; Rao, A. Clean-label alternatives for food preservation: An emerging trend. Heliyon 2024, 10, e35815. [Google Scholar] [CrossRef] [PubMed]
- Dong, H.; Xu, Y.; Zhang, Q.; Li, H.; Chen, L. Activity and safety evaluation of natural preservatives. Food Res. Int. 2024, 190, 114548. [Google Scholar] [CrossRef]
- Wu, J.; Zang, M.; Wang, S.; Zhao, B.; Bai, J.; Xu, C.; Shi, Y.; Qiao, X. Nisin: From a structural and meat preservation perspective. Food Microbiol. 2023, 111, 104207. [Google Scholar] [CrossRef] [PubMed]
- Meena, M.; Prajapati, P.; Ravichandran, C.; Sehrawat, R. Natamycin: A natural preservative for food applications—A review. Food Sci. Biotechnol. 2021, 30, 1481–1496. [Google Scholar] [CrossRef]
- Salih, H.M.; Amachawadi, R.G.; Kang, Q.; Li, Y.; Nagaraja, T.G. In-Vitro Antimicrobial Activities of Grape Seed, Green Tea, and Rosemary Phenolic Extracts Against Liver Abscess Causing Bacterial Pathogens in Cattle. Microorganisms 2024, 12, 2291. [Google Scholar] [CrossRef]
- Terrazas-Pineda, K.A.; Alamilla-Beltrán, L.; Acero-Ortega, C.A.; Damas-Espinoza, J.A.; Calderón-Domínguez, G.; Mora-Escobedo, R.; Vega-Sánchez, V.; Gómez-de Anda, F.R. Antimicrobial Activity of Cinnamon, Tea Tree, and Thyme Essential Oils Against Pathogenic Bacteria Isolated from Tilapia (Oreochromis spp.) in Aquaculture Farms. Molecules 2025, 30, 2799. [Google Scholar] [CrossRef]
- Sorrenti, V.; Burò, I.; Consoli, V.; Vanella, L. Recent Advances in Health Benefits of Bioactive Compounds from Food Wastes and By-Products: Biochemical Aspects. Int. J. Mol. Sci. 2023, 24, 2019. [Google Scholar] [CrossRef]
- Gomes, B.A.F.; Alexandre, A.C.S.; de Andrade, G.A.V.; Zanzini, A.P.; de Barros, H.E.A.; Ferraz e Silva, L.M.d.S.; Costa, P.A.; Boas, E.V. de B.V. Recent advances in processing and preservation of minimally processed fruits and vegetables: A review—Part 2: Physical methods and global market outlook. Food Chem. Adv. 2023, 2, 100304. [Google Scholar] [CrossRef]
- Martínez, S.; Carballo, J. Physicochemical, Sensory and Nutritional Properties of Foods Affected by Processing and Storage. Foods 2021, 10, 2970. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Shen, X.; Jiang, W.; Xi, Y.; Li, S. Comprehensive review of emerging contaminants: Detection technologies, environmental impact, and management strategies. Ecotoxicol. Environ. Saf. 2024, 278, 116420. [Google Scholar] [CrossRef] [PubMed]
- Bennett, G.; Bardon, L.A.; Gibney, E.R. A Comparison of Dietary Patterns and Factors Influencing Food Choice among Ethnic Groups Living in One Locality: A Systematic Review. Nutrients 2022, 14, 941. [Google Scholar] [CrossRef] [PubMed]
- Nnaji, N.D.; Onyeaka, H.; Ughamba, K.T.; Ononugbo, C.M.; Olovo, C.V.; Mazi, I.M. Chemical Toxicants Used for Food Preservation in Africa. Is it a Case of Ignorance or Food Fraud? A Review. Health Sci. Rep. 2025, 8, e70333. [Google Scholar] [CrossRef]
- Tristan Asensi, M.; Napoletano, A.; Sofi, F.; Dinu, M. Low-Grade Inflammation and Ultra-Processed Foods Consumption: A Review. Nutrients 2023, 15, 1546. [Google Scholar] [CrossRef]
- Clemente-Suárez, V.J.; Beltrán-Velasco, A.I.; Redondo-Flórez, L.; Martín-Rodríguez, A.; Tornero-Aguilera, J.F. Global Impacts of Western Diet and Its Effects on Metabolism and Health: A Narrative Review. Nutrients 2023, 15, 2749. [Google Scholar] [CrossRef] [PubMed]
- Hino, H.; Sparks, L. Clean food consumerism: Scale development and validation. Food Qual. Prefer. 2025, 132, 105554. [Google Scholar] [CrossRef]
- Maleš, I.; Pedisić, S.; Zorić, Z.; Elez-Garofulić, I.; Repajić, M.; You, L.; Vladimir-Knežević, S.; Butorac, D.; Dragović-Uzelac, V. The medicinal and aromatic plants as ingredients in functional beverage production. J. Funct. Foods 2022, 96, 105210. [Google Scholar] [CrossRef]
- Munekata, P.E.S.; Pateiro, M.; Domínguez, R.; Nieto, G.; Kumar, M.; Dhama, K.; Lorenzo, J.M. Bioactive Compounds from Fruits as Preservatives. Foods 2023, 12, 343. [Google Scholar] [CrossRef]
- Kruk, M.E.; Gage, A.D.; Arsenault, C.; Jordan, K.; Leslie, H.H.; Roder-DeWan, S.; Adeyi, O.; Barker, P.; Daelmans, B.; Doubova, S.V.; et al. High-quality health systems in the Sustainable Development Goals era: Time for a revolution. Lancet Glob. Health 2018, 6, e1196–e1252. [Google Scholar] [CrossRef]
- Fanzo, J.; McLaren, R.; Bellows, A.; Carducci, B. Challenges and opportunities for increasing the effectiveness of food reformulation and fortification to improve dietary and nutrition outcomes. Food Policy 2023, 119, 102515. [Google Scholar] [CrossRef]
- Wu, C.W.-K.; Lui, R.N. Early-onset colorectal cancer: Current insights and future directions. World J. Gastrointest. Oncol. 2022, 14, 230–241. [Google Scholar] [CrossRef]
- Hang, D.; Wang, L.; Fang, Z.; Du, M.; Wang, K.; He, X.; Khandpur, N.; Rossato, S.L.; Wu, K.; Hu, Z.; et al. Ultra-processed food consumption and risk of colorectal cancer precursors: Results from 3 prospective cohorts. JNCI J. Natl. Cancer Inst. 2023, 115, 155–164. [Google Scholar] [CrossRef]
- Lian, Y.; Wang, G.-P.; Chen, G.-Q.; Chen, H.-N.; Zhang, G.-Y. Association between ultra-processed foods and risk of cancer: A systematic review and meta-analysis. Front. Nutr. 2023, 10, 1175994. [Google Scholar] [CrossRef] [PubMed]
- Ashari, L.S.; Abd Rashid, A.A.; Mohd Razif, S.; Yeong Yeh, L.; Jan Mohamed, H.J. Diet is Linked to Colorectal Cancer Risk among Asian Adults: A Scoping Review. Malays. J. Med. Sci. 2023, 30, 8–31. [Google Scholar] [CrossRef] [PubMed]
- Reardon, T.; Tschirley, D.; Liverpool-Tasie, L.S.O.; Awokuse, T.; Fanzo, J.; Minten, B.; Vos, R.; Dolislager, M.; Sauer, C.; Dhar, R.; et al. The processed food revolution in African food systems and the double burden of malnutrition. Glob. Food Sec. 2021, 28, 100466. [Google Scholar] [CrossRef]
- Kraemer, M.V.d.S.; Fernandes, A.C.; Chaddad, M.C.C.; Uggioni, P.L.; Rodrigues, V.M.; Bernardo, G.L.; Proença, R.P. da C. Aditivos alimentares na infância: Uma revisão sobre consumo e consequências à saúde. Rev. Saude Publica 2022, 56, 32. [Google Scholar] [CrossRef]
- Hosseini, F.; Majdi, M.; Naghshi, S.; Sheikhhossein, F.; Djafarian, K.; Shab-Bidar, S. Nitrate-nitrite exposure through drinking water and diet and risk of colorectal cancer: A systematic review and meta-analysis of observational studies. Clin. Nutr. 2021, 40, 3073–3081. [Google Scholar] [CrossRef]
- Wang, Y.; Nguyen, L.H.; Mehta, R.S.; Song, M.; Huttenhower, C.; Chan, A.T. Association Between the Sulfur Microbial Diet and Risk of Colorectal Cancer. JAMA Netw. Open 2021, 4, e2134308. [Google Scholar] [CrossRef] [PubMed]
- Qian, F.; Riddle, M.C.; Wylie-Rosett, J.; Hu, F.B. Red and Processed Meats and Health Risks: How Strong Is the Evidence? Diabetes Care 2020, 43, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Crowe, W.; Pan, X.; Mackle, J.; Harris, A.; Hardiman, G.; Elliott, C.T.; Green, B.D. Dietary inclusion of nitrite-containing frankfurter exacerbates colorectal cancer pathology and alters metabolism in APCmin mice. npj Sci. Food 2022, 6, 60. [Google Scholar] [CrossRef] [PubMed]
- Chazelas, E.; Pierre, F.; Druesne-Pecollo, N.; Esseddik, Y.; Szabo de Edelenyi, F.; Agaesse, C.; De Sa, A.; Lutchia, R.; Gigandet, S.; Srour, B.; et al. Nitrites and nitrates from food additives and natural sources and cancer risk: Results from the NutriNet-Santé cohort. Int. J. Epidemiol. 2022, 51, 1106–1119. [Google Scholar] [CrossRef]
- Aykan, N.F. Red meat and colorectal cancer. Oncol. Rev. 2015, 9, 288. [Google Scholar] [CrossRef]
- Chang, V.C.; Cotterchio, M.; De, P.; Tinmouth, J. Risk factors for early-onset colorectal cancer: A population-based case–control study in Ontario, Canada. Cancer Causes Control 2021, 32, 1063–1083. [Google Scholar] [CrossRef]
- Yiu, C.H.; Ianni, B.D.; Fujita, K.; Tan, E.C.K.; Hilmer, S.N.; Lu, C.Y. Utilization and associated factors of <scp> TPMT </scp> testing among Australian adults receiving thiopurines: A national retrospective data-linkage study. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2025, 45, 12–19. [Google Scholar] [CrossRef]
- Shu, L.; Huang, Y.; Si, C.; Zhu, Q.; Zheng, P.; Zhang, X. Association between ultra-processed food intake and risk of colorectal cancer: A systematic review and meta-analysis. Front. Nutr. 2023, 10, 1170992. [Google Scholar] [CrossRef]
- Sifaki-Pistolla, D.; Poimenaki, V.; Fotopoulou, I.; Saloustros, E.; Mavroudis, D.; Vamvakas, L.; Lionis, C. Significant Rise of Colorectal Cancer Incidence in Younger Adults and Strong Determinants: 30 Years Longitudinal Differences between under and over 50s. Cancers 2022, 14, 4799. [Google Scholar] [CrossRef]
- Ullah, F.; Pillai, A.B.; Omar, N.; Dima, D.; Harichand, S. Early-Onset Colorectal Cancer: Current Insights. Cancers 2023, 15, 3202. [Google Scholar] [CrossRef]
- Pan, H.; Tang, Y.; Zhu, H.; Sun, Y.; Chi, P.; Huang, Y. Global burden, trends, and risk factors of early-onset and late-onset colorectal cancer from 1990 to 2021, with projections to 2040: A population-based study. BMC Gastroenterol. 2025, 25, 486. [Google Scholar] [CrossRef]
- Babalola, O.O.; Akinnusi, E.; Ottu, P.O.; Bridget, K.; Oyubu, G.; Ajiboye, S.A.; Waheed, S.A.; Collette, A.C.; Adebimpe, H.O.; Nwokafor, C.V.; et al. The impact of ultra-processed foods on cardiovascular diseases and cancer: Epidemiological and mechanistic insights. Asp. Mol. Med. 2025, 5, 100072. [Google Scholar] [CrossRef]
- Chu, A.H.; Lin, K.; Croker, H.; Kefyalew, S.; Becerra-Tomás, N.; Dossus, L.; González-Gil, E.M.; Ahmadi, N.; Park, Y.; Krebs, J.; et al. Dietary patterns and colorectal cancer risk: Global Cancer Update Programme (CUP Global) systematic literature review. Am. J. Clin. Nutr. 2025, 121, 999–1016. [Google Scholar] [CrossRef]
- Mohammad, N.M.A.B.; Shahril, M.R.; Shahar, S.; Fenech, M.; Sharif, R. Association between Diet-related Behaviour and Risk of Colorectal Cancer: A Scoping Review. J. Cancer Prev. 2022, 27, 208–220. [Google Scholar] [CrossRef]
- Tabung, F.K.; Brown, L.S.; Fung, T.T. Dietary Patterns and Colorectal Cancer Risk: A Review of 17 Years of Evidence (2000–2016). Curr. Colorectal Cancer Rep. 2017, 13, 440–454. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.; Chen, C.; Zhao, D.; Li, C. Impact of ultra-processed meat products on human health: Review and outlook. J. Food Sci. 2025, 90, e70040. [Google Scholar] [CrossRef]
- LeBlanc, K.E.; Baer-Sinnott, S.; Lancaster, K.J.; Campos, H.; Lau, K.H.K.; Tucker, K.L.; Kushi, L.H.; Willett, W.C. Perspective: Beyond the Mediterranean Diet—Exploring Latin American, Asian, and African Heritage Diets as Cultural Models of Healthy Eating. Adv. Nutr. 2024, 15, 100221. [Google Scholar] [CrossRef]
- Atchade, A.M.; Williams, J.L.; Mermelstein, L.; Nemesure, B. Unraveling the complexities of early-onset colorectal cancer: A perspective on dietary and microbial influences. Front. Public Health 2024, 12, 1370108. [Google Scholar] [CrossRef]
- Hofseth, L.J.; Hebert, J.R.; Chanda, A.; Chen, H.; Love, B.L.; Pena, M.M.; Murphy, E.A.; Sajish, M.; Sheth, A.; Buckhaults, P.J.; et al. Early-onset colorectal cancer: Initial clues and current views. Nat. Rev. Gastroenterol. Hepatol. 2020, 17, 352–364. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, H.A.; Sulaiman, G.M.; Al-Saffar, A.Z.; Abomughaid, M.M.; Hussein, N.N.; Salih, Z.T.; Hadi, N.A.; Mohsin, M.H.; Al-kuraishy, H.M.; Khan, R.A.; et al. Roles of foods and related components: An overview on cancer causatives, and plausible preventions. Appl. Food Res. 2025, 5, 101132. [Google Scholar] [CrossRef]
- Mafe, A.N.; Büsselberg, D. The Effect of Microbiome-Derived Metabolites in Inflammation-Related Cancer Prevention and Treatment. Biomolecules 2025, 15, 688. [Google Scholar] [CrossRef]
- de Oliveira, I.; Santos-Buelga, C.; Aquino, Y.; Barros, L.; Heleno, S.A. New frontiers in the exploration of phenolic compounds and other bioactives as natural preservatives. Food Biosci. 2025, 68, 106571. [Google Scholar] [CrossRef]
- Modeel, S.; Siwach, S.; Dolkar, P.; Chaurasia, M.; Yadav, P.; Atri, A.; Yadav, A.; Negi, T.; Negi, R.K. Emerging Risk Factors and the Role of Gut Microbiota in Immunomodulation and Therapeutic Implications in Colorectal Cancer. Cancer Pathog. Ther. 2025, 8. [Google Scholar] [CrossRef]
- Yarmolinsky, L.; Nakonechny, F.; Haddis, T.; Khalfin, B.; Dahan, A.; Ben-Shabat, S. Natural Antimicrobial Compounds as Promising Preservatives: A Look at an Old Problem from New Perspectives. Molecules 2024, 29, 5830. [Google Scholar] [CrossRef]
- Stead, E.R.; Bjedov, I. Balancing DNA repair to prevent ageing and cancer. Exp. Cell Res. 2021, 405, 112679. [Google Scholar] [CrossRef]
- Rudrapal, M.; Khairnar, S.J.; Khan, J.; Dukhyil, A.B.; Ansari, M.A.; Alomary, M.N.; Alshabrmi, F.M.; Palai, S.; Deb, P.K.; Devi, R. Dietary Polyphenols and Their Role in Oxidative Stress-Induced Human Diseases: Insights Into Protective Effects, Antioxidant Potentials and Mechanism(s) of Action. Front. Pharmacol. 2022, 13, 806470. [Google Scholar] [CrossRef]
- Ma, Z.F.; Lee, Y.Y. The Role of the Gut Microbiota in Health, Diet, and Disease with a Focus on Obesity. Foods 2025, 14, 492. [Google Scholar] [CrossRef]
- Liu, C.; Zhan, S.; Tian, Z.; Li, N.; Li, T.; Wu, D.; Zeng, Z.; Zhuang, X. Food Additives Associated with Gut Microbiota Alterations in Inflammatory Bowel Disease: Friends or Enemies? Nutrients 2022, 14, 3049. [Google Scholar] [CrossRef]
- Sankarganesh, P.; Bhunia, A.; Ganesh Kumar, A.; Babu, A.S.; Gopukumar, S.T.; Lokesh, E. Short-chain fatty acids (SCFAs) in gut health: Implications for drug metabolism and therapeutics. Med. Microecol. 2025, 25, 100139. [Google Scholar] [CrossRef]
- Garvey, M. Intestinal Dysbiosis: Microbial Imbalance Impacts on Colorectal Cancer Initiation, Progression and Disease Mitigation. Biomedicines 2024, 12, 740. [Google Scholar] [CrossRef]
- Fitsum, S.; Gebreyohannes, G.; Sbhatu, D.B. Bioactive compounds in fermented foods: Health benefits, safety, and future perspectives. Appl. Food Res. 2025, 5, 101097. [Google Scholar] [CrossRef]
- Schell, L.D.; Chadaideh, K.S.; Allen-Blevins, C.R.; Venable, E.M.; Carmody, R.N. Dietary preservatives alter the gut microbiota in vitro and in vivo with sex-specific consequences for host metabolic development in a mouse model. Am. J. Clin. Nutr. 2025, 122, 221–234. [Google Scholar] [CrossRef] [PubMed]
- Diakité, M.T.; Diakité, B.; Koné, A.; Balam, S.; Fofana, D.; Diallo, D.; Kassogué, Y.; Traoré, C.B.; Kamaté, B.; Ba, D.; et al. Relationships between gut microbiota, red meat consumption and colorectal cancer. J. Carcinog. Mutagen. 2022, 13, 1000385. [Google Scholar] [PubMed]
- Mirzaei, R.; Bouzari, B.; Hosseini-Fard, S.R.; Mazaheri, M.; Ahmadyousefi, Y.; Abdi, M.; Jalalifar, S.; Karimitabar, Z.; Teimoori, A.; Keyvani, H.; et al. Role of microbiota-derived short-chain fatty acids in nervous system disorders. Biomed. Pharmacother. 2021, 139, 111661. [Google Scholar] [CrossRef]
- Hrncir, T. Gut Microbiota Dysbiosis: Triggers, Consequences, Diagnostic and Therapeutic Options. Microorganisms 2022, 10, 578. [Google Scholar] [CrossRef]
- Benameur, T.; Porro, C.; Twfieg, M.-E.; Benameur, N.; Panaro, M.A.; Filannino, F.M.; Hasan, A. Emerging Paradigms in Inflammatory Disease Management: Exploring Bioactive Compounds and the Gut Microbiota. Brain Sci. 2023, 13, 1226. [Google Scholar] [CrossRef]
- Mráz, P.; Kopecký, M.; Hasoňová, L.; Hoštičková, I.; Vaníčková, A.; Perná, K.; Žabka, M.; Hýbl, M. Antibacterial Activity and Chemical Composition of Popular Plant Essential Oils and Their Positive Interactions in Combination. Molecules 2025, 30, 1864. [Google Scholar] [CrossRef]
- de Melo, L.F.M.; Aquino-Martins, V.G.d.Q.; da Silva, A.P.; Oliveira Rocha, H.A.; Scortecci, K.C. Biological and pharmacological aspects of tannins and potential biotechnological applications. Food Chem. 2023, 414, 135645. [Google Scholar] [CrossRef]
- Jarmakiewicz-Czaja, S.; Piątek, D.; Filip, R. The impact of selected food additives on the gastrointestinal tract in the example of nonspecific inflammatory bowel diseases. Arch. Med. Sci. 2022, 18, 1286–1296. [Google Scholar] [CrossRef]
- Mao, H.; Zhao, X.; Sun, S. NF-κB in inflammation and cancer. Cell. Mol. Immunol. 2025, 22, 811–839. [Google Scholar] [CrossRef]
- Seto, T.; Grondin, J.A.; Khan, W.I. Food Additives: Emerging Detrimental Roles on Gut Health. FASEB J. 2025, 39, e70810. [Google Scholar] [CrossRef]
- Li, C.; Xue, Y.; Ba, X.; Wang, R. The Role of 8-oxoG Repair Systems in Tumorigenesis and Cancer Therapy. Cells 2022, 11, 3798. [Google Scholar] [CrossRef]
- Dong, R.; Wang, J.; Guan, R.; Sun, J.; Jin, P.; Shen, J. Role of Oxidative Stress in the Occurrence, Development, and Treatment of Breast Cancer. Antioxidants 2025, 14, 104. [Google Scholar] [CrossRef]
- Singh, N.; Yadav, S.S. A review on health benefits of phenolics derived from dietary spices. Curr. Res. Food Sci. 2022, 5, 1508–1523. [Google Scholar] [CrossRef]
- Coventry, B.J.; Henneberg, M. The Immune System and Responses to Cancer: Coordinated Evolution. F1000Research 2021, 4, 552. [Google Scholar] [CrossRef] [PubMed]
- Franko, N.; Markovič, T.; Žižek, P.; Kodila, A.; Mlinarič Raščan, I.; Sollner Dolenc, M. Unravelling immunomodulatory effects of bisphenol A substitutes on human macrophages, T and B lymphocytes using in vitro models. Ecotoxicol. Environ. Saf. 2025, 300, 118406. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Li, C.; Zhang, W.; Wang, Y.; Qian, P.; Huang, H. Inflammation and aging: Signaling pathways and intervention therapies. Signal Transduct. Target. Ther. 2023, 8, 239. [Google Scholar] [CrossRef] [PubMed]
- Borowczak, J.; Szczerbowski, K.; Maniewski, M.; Kowalewski, A.; Janiczek-Polewska, M.; Szylberg, A.; Marszałek, A.; Szylberg, Ł. The Role of Inflammatory Cytokines in the Pathogenesis of Colorectal Carcinoma—Recent Findings and Review. Biomedicines 2022, 10, 1670. [Google Scholar] [CrossRef]
- Sun, Y.; Keat, O.B.; Rajabi, S. The role of physical activity and epigenetic changes in colorectal cancer prevention. Cancer Cell Int. 2025, 25, 227. [Google Scholar] [CrossRef]
- Allegra, A.; Mirabile, G.; Ettari, R.; Pioggia, G.; Gangemi, S. The Impact of Curcumin on Immune Response: An Immunomodulatory Strategy to Treat Sepsis. Int. J. Mol. Sci. 2022, 23, 14710. [Google Scholar] [CrossRef]
- Puzzono, M.; Mannucci, A.; Grannò, S.; Zuppardo, R.A.; Galli, A.; Danese, S.; Cavestro, G.M. The Role of Diet and Lifestyle in Early-Onset Colorectal Cancer: A Systematic Review. Cancers 2021, 13, 5933. [Google Scholar] [CrossRef]
- Crowe, W.; Elliott, C.T.; Green, B.D. A Review of the In Vivo Evidence Investigating the Role of Nitrite Exposure from Processed Meat Consumption in the Development of Colorectal Cancer. Nutrients 2019, 11, 2673. [Google Scholar] [CrossRef]
- Kliemann, N.; Rauber, F.; Bertazzi Levy, R.; Viallon, V.; Vamos, E.P.; Cordova, R.; Freisling, H.; Casagrande, C.; Nicolas, G.; Aune, D.; et al. Food processing and cancer risk in Europe: Results from the prospective EPIC cohort study. Lancet Planet. Health 2023, 7, e219–e232. [Google Scholar] [CrossRef]
- Kim, J.H.; Jun, S.; Kim, J. Dietary intake and cancer incidence in Korean adults: A systematic review and meta-analysis of observational studies. Epidemiol. Health 2023, 45, e2023102. [Google Scholar] [CrossRef]
- Uzokwe, C.A.; Nkwoala, C.C.; Ebenso, B.E.; Beer, S.; Williams, G.; Iheme, G.O.; Opara, C.G.; Sanusi, R.A.; Ene-Obong, H.N.; Cade, J.E. Development and Pilot Study of myfood24 West Africa—An Online Tool for Dietary Assessment in Nigeria. Nutrients 2024, 16, 3497. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Wang, P.P.; Zhao, J.; Green, R.; Sun, Z.; Roebothan, B.; Squires, J.; Buehler, S.; Dicks, E.; Zhao, J.; et al. Dietary N-nitroso compounds and risk of colorectal cancer: A case–control study in Newfoundland and Labrador and Ontario, Canada. Br. J. Nutr. 2014, 111, 1109–1117. [Google Scholar] [CrossRef] [PubMed]
- Kunst, C.; Schmid, S.; Michalski, M.; Tümen, D.; Buttenschön, J.; Müller, M.; Gülow, K. The Influence of Gut Microbiota on Oxidative Stress and the Immune System. Biomedicines 2023, 11, 1388. [Google Scholar] [CrossRef] [PubMed]
- Nohmi, T. Thresholds of Genotoxic and Non-Genotoxic Carcinogens. Toxicol. Res. 2018, 34, 281–290. [Google Scholar] [CrossRef]
- Lis, K.; Bartuzi, Z. Plant Food Dyes with Antioxidant Properties and Allergies—Friend or Enemy? Antioxidants 2023, 12, 1357. [Google Scholar] [CrossRef] [PubMed]
- Petimar, J.; Smith-Warner, S.A.; Fung, T.T.; Rosner, B.; Chan, A.T.; Hu, F.B.; Giovannucci, E.L.; Tabung, F.K. Recommendation-based dietary indexes and risk of colorectal cancer in the Nurses’ Health Study and Health Professionals Follow-up Study. Am. J. Clin. Nutr. 2018, 108, 1092–1103. [Google Scholar] [CrossRef]
- Tahiri, M.; Johnsrud, C.; Steffensen, I.-L. Evidence and hypotheses on adverse effects of the food additives carrageenan (E 407)/processed Eucheuma seaweed (E 407a) and carboxymethylcellulose (E 466) on the intestines: A scoping review. Crit. Rev. Toxicol. 2023, 53, 521–571. [Google Scholar] [CrossRef]
- Popoola, A.A.; Frediani, J.K.; Hartman, T.J.; Paynabar, K. Mitigating underreported error in food frequency questionnaire data using a supervised machine learning method and error adjustment algorithm. BMC Med. Inform. Decis. Mak. 2023, 23, 178. [Google Scholar] [CrossRef]
- Pettigrew, S.; Jongenelis, M.I.; Jones, A.; Hercberg, S.; Julia, C. An 18-country analysis of the effectiveness of five front-of-pack nutrition labels. Food Qual. Prefer. 2023, 104, 104691. [Google Scholar] [CrossRef]
- AlQurashi, A.A.; Marar, S.D.; Ayyash, M.; AlRawi, H.Z.; Abu-Shaheen, A. Comparing the influence of front-of-pack nutrition labels on Saudi consumers’ understanding and food selection. Front. Public Health 2025, 13, 1527531. [Google Scholar] [CrossRef]
- Deschasaux-Tanguy, M.; Druesne-Pecollo, N.; Esseddik, Y.; de Edelenyi, F.S.; Allès, B.; Andreeva, V.A.; Baudry, J.; Charreire, H.; Deschamps, V.; Egnell, M.; et al. Diet and physical activity during the coronavirus disease 2019 (COVID-19) lockdown (March–May 2020): Results from the French NutriNet-Santé cohort study. Am. J. Clin. Nutr. 2021, 113, 924–938. [Google Scholar] [CrossRef]
- Patangia, D.V.; Anthony Ryan, C.; Dempsey, E.; Paul Ross, R.; Stanton, C. Impact of antibiotics on the human microbiome and consequences for host health. Microbiologyopen 2022, 11, e1260. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, D.E.; Ruan, Y.; Farah, E.; Hutchinson, J.M.; Hilsden, R.J.; Brenner, D.R. Risk factors for early-onset colorectal cancer: A Canadian prospective cohort study. Cancer Epidemiol. 2024, 91, 102578. [Google Scholar] [CrossRef] [PubMed]
- Akimoto, N.; Ugai, T.; Zhong, R.; Hamada, T.; Fujiyoshi, K.; Giannakis, M.; Wu, K.; Cao, Y.; Ng, K.; Ogino, S. Rising incidence of early-onset colorectal cancer—A call to action. Nat. Rev. Clin. Oncol. 2021, 18, 230–243. [Google Scholar] [CrossRef] [PubMed]
- Domínguez-Oliva, A.; Hernández-Ávalos, I.; Martínez-Burnes, J.; Olmos-Hernández, A.; Verduzco-Mendoza, A.; Mota-Rojas, D. The Importance of Animal Models in Biomedical Research: Current Insights and Applications. Animals 2023, 13, 1223. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Hecht, S.S. Metabolic Activation and DNA Interactions of Carcinogenic N-Nitrosamines to Which Humans Are Commonly Exposed. Int. J. Mol. Sci. 2022, 23, 4559. [Google Scholar] [CrossRef]
- Gizaw, Z. Public health risks related to food safety issues in the food market: A systematic literature review. Environ. Health Prev. Med. 2019, 24, 68. [Google Scholar] [CrossRef]
- Koios, D.; Machado, P.; Lacy-Nichols, J. Representations of Ultra-Processed Foods: A Global Analysis of How Dietary Guidelines Refer to Levels of Food Processing. Int. J. Health Policy Manag. 2022, 11, 2588–2599. [Google Scholar] [CrossRef]
- Olvera-Rosales, L.-B.; Cruz-Guerrero, A.-E.; Ramírez-Moreno, E.; Quintero-Lira, A.; Contreras-López, E.; Jaimez-Ordaz, J.; Castañeda-Ovando, A.; Añorve-Morga, J.; Calderón-Ramos, Z.-G.; Arias-Rico, J.; et al. Impact of the Gut Microbiota Balance on the Health–Disease Relationship: The Importance of Consuming Probiotics and Prebiotics. Foods 2021, 10, 1261. [Google Scholar] [CrossRef]
- Gharib, E. Closing Editorial: Colorectal Cancer—A Molecular Genetics Perspective. Int. J. Mol. Sci. 2024, 25, 12604. [Google Scholar] [CrossRef]
- Song, M.; Garrett, W.S.; Chan, A.T. Nutrients, Foods, and Colorectal Cancer Prevention. Gastroenterology 2015, 148, 1244–1260.e16. [Google Scholar] [CrossRef]
- Vikram, H.P.R.; Kumar, T.P.; Kumar, G.; Beeraka, N.M.; Deka, R.; Suhail, S.M.; Jat, S.; Bannimath, N.; Padmanabhan, G.; Chandan, R.S.; et al. Nitrosamines crisis in pharmaceuticals—Insights on toxicological implications, root causes and risk assessment: A systematic review. J. Pharm. Anal. 2024, 14, 100919. [Google Scholar] [CrossRef]
- Wairimu, N.W.; Wairagu, P.; Chepukosi, K.W.; Obiero, G.F.; Okanya, P.W.; Isaac, A.O.; Nyariki, J.N. Sodium Metabisulfite-Induced Hematotoxicity, Oxidative Stress, and Organ Damage Ameliorated by Standardized Ginkgo biloba in Mice. J. Toxicol. 2023, 2023, 7058016. [Google Scholar] [CrossRef] [PubMed]
- Alexander, D.D.; Weed, D.L.; Miller, P.E.; Mohamed, M.A. Red Meat and Colorectal Cancer: A Quantitative Update on the State of the Epidemiologic Science. J. Am. Coll. Nutr. 2015, 34, 521–543. [Google Scholar] [CrossRef]
- Rostampoor, Z.; Afrashteh, S.; Mohammadianpanah, M.; Ghaem, H.; Zeegers, M.P.; Fararouei, M. Lifestyle, dietary pattern and colorectal cancer: A case-control study. BMC Nutr. 2024, 10, 138. [Google Scholar] [CrossRef]
- Irwin, S.V.; Deardorff, L.M.; Deng, Y.; Fisher, P.; Gould, M.; June, J.; Kent, R.S.; Qin, Y.; Yadao, F. Sulfite preservatives effects on the mouth microbiome: Changes in viability, diversity and composition of microbiota. PLoS ONE 2022, 17, e0265249. [Google Scholar] [CrossRef]
- Zhang, Q.; Chumanevich, A.A.; Nguyen, I.; Chumanevich, A.A.; Sartawi, N.; Hogan, J.; Khazan, M.; Harris, Q.; Massey, B.; Chatzistamou, I.; et al. The synthetic food dye, Red 40, causes DNA damage, causes colonic inflammation, and impacts the microbiome in mice. Toxicol. Reports 2023, 11, 221–232. [Google Scholar] [CrossRef]
- Wu, H.; Ma, W.; Wang, Y.; Wang, Y.; Sun, X.; Zheng, Q. Gut microbiome-metabolites axis: A friend or foe to colorectal cancer progression. Biomed. Pharmacother. 2024, 173, 116410. [Google Scholar] [CrossRef] [PubMed]
- Caceres-Matos, R.; Castro-Méndez, A.; Domínguez, M.; Pabón-Carrasco, D.; Pabón-Carrasco, M. The Influence of Ultra-Processed Food on Colorectal Cancer: A Systematic Review. Gastrointest. Disord. 2024, 6, 164–179. [Google Scholar] [CrossRef]
- Khan, I.S.; Dar, K.B.; Ganie, S.A.; Ali, M.N. Toxicological impact of sodium benzoate on inflammatory cytokines, oxidative stress and biochemical markers in male Wistar rats. Drug Chem. Toxicol. 2022, 45, 1345–1354. [Google Scholar] [CrossRef] [PubMed]
- Adigun, A.O.; Adebile, T.M.; Okoye, C.; Ogundipe, T.I.; Ajekigbe, O.R.; Mbaezue, R.N.; Okobi, O.E. Causes and Prevention of Early-Onset Colorectal Cancer. Cureus 2023, 15, e45095. [Google Scholar] [CrossRef]
- Cediel, G.; Reyes, M.; Corvalán, C.; Levy, R.B.; Uauy, R.; Monteiro, C.A. Ultra-processed foods drive to unhealthy diets: Evidence from Chile. Public Health Nutr. 2021, 24, 1698–1707. [Google Scholar] [CrossRef]
- Kuczmarski, M.F.; Cotugna, N.; Evans, M.K.; Zonderman, A.B. Food Choices and Diet-Related Disparities Among Socioeconomically Diverse White and African American Urban Women. Dietetics 2025, 4, 10. [Google Scholar] [CrossRef]
- Holowatyj, A.N.; Maude, A.S.; Musa, H.S.; Adamu, A.; Ibrahim, S.; Abdullahi, A.; Manko, M.; Aminu, S.M.; Mohammed, A.; Idoko, J.; et al. Patterns of Early-Onset Colorectal Cancer Among Nigerians and African Americans. JCO Glob. Oncol. 2020, 6, 1647–1655. [Google Scholar] [CrossRef]
- Nithya, A.; Misra, S.; Panigrahi, C.; Dalbhagat, C.G.; Mishra, H.N. Probiotic potential of fermented foods and their role in non-communicable diseases management: An understanding through recent clinical evidences. Food Chem. Adv. 2023, 3, 100381. [Google Scholar] [CrossRef]
- Kumar, G.S.; Kulkarni, M.; Rathi, N. Evolving Food Choices Among the Urban Indian Middle-Class: A Qualitative Study. Front. Nutr. 2022, 9, 844413. [Google Scholar] [CrossRef] [PubMed]
- Mafe, A.N.; Büsselberg, D. Could a Mediterranean Diet Modulate Alzheimer’s Disease Progression? The Role of Gut Microbiota and Metabolite Signatures in Neurodegeneration. Foods 2025, 14, 1559. [Google Scholar] [CrossRef]
- Carroll, K.L.; Frugé, A.D.; Heslin, M.J.; Lipke, E.A.; Greene, M.W. Diet as a Risk Factor for Early-Onset Colorectal Adenoma and Carcinoma: A Systematic Review. Front. Nutr. 2022, 9, 896330. [Google Scholar] [CrossRef]
- Ofosu, F.K.; Daliri, E.B.-M.; Elahi, F.; Chelliah, R.; Lee, B.-H.; Oh, D.-H. New Insights on the Use of Polyphenols as Natural Preservatives and Their Emerging Safety Concerns. Front. Sustain. Food Syst. 2020, 4, 525810. [Google Scholar] [CrossRef]
- El-Saadony, M.T.; Saad, A.M.; Korma, S.A.; Salem, H.M.; Abd El-Mageed, T.A.; Alkafaas, S.S.; Elsalahaty, M.I.; Elkafas, S.S.; Mosa, W.F.A.; Ahmed, A.E.; et al. Garlic bioactive substances and their therapeutic applications for improving human health: A comprehensive review. Front. Immunol. 2024, 15, 1277074. [Google Scholar] [CrossRef]
- Prasad, J.; Kumar, N.; Pratibha; Jaiswal, R.; Yadav, A.; Sharma, S.P.; Fawole, O.A.; Kaushik, N. Biopolymer based composite packaging: A sustainable approach for fruits and vegetables preservation. Appl. Food Res. 2025, 5, 101211. [Google Scholar] [CrossRef]
- Mafe, A.N.; Nkene, I.H.; Ali, A.B.M.; Edo, G.I.; Akpoghelie, P.O.; Yousif, E.; Isoje, E.F.; Igbuku, U.A.; Ismael, S.A.; Essaghah, A.E.A.; et al. Smart Probiotic Solutions for Mycotoxin Mitigation: Innovations in Food Safety and Sustainable Agriculture. Probiotics Antimicrob. Proteins 2025. [Google Scholar] [CrossRef]
- Chandrasekaran, P.; Weiskirchen, S.; Weiskirchen, R. Effects of Probiotics on Gut Microbiota: An Overview. Int. J. Mol. Sci. 2024, 25, 6022. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Xue, R. Nanostructured materials for smart food packaging: Integrating preservation and antimicrobial properties. Alex. Eng. J. 2025, 124, 446–461. [Google Scholar] [CrossRef]
- Lourenço, S.C.; Moldão-Martins, M.; Alves, V.D. Antioxidants of Natural Plant Origins: From Sources to Food Industry Applications. Molecules 2019, 24, 4132. [Google Scholar] [CrossRef]
- Kennedy, D.O. Polyphenols and the Human Brain: Plant “Secondary Metabolite” Ecologic Roles and Endogenous Signaling Functions Drive Benefits. Adv. Nutr. 2014, 5, 515–533. [Google Scholar] [CrossRef] [PubMed]
- Günal-Köroğlu, D.; Karabulut, G.; Ozkan, G.; Yılmaz, H.; Gültekin-Subaşı, B.; Capanoglu, E. Allergenicity of Alternative Proteins: Reduction Mechanisms and Processing Strategies. J. Agric. Food Chem. 2025, 73, 7522–7546. [Google Scholar] [CrossRef] [PubMed]
- Ciobanu, M.-M.; Flocea, E.-I.; Boișteanu, P.-C. The Impact of Artificial and Natural Additives in Meat Products on Neurocognitive Food Perception: A Narrative Review. Foods 2024, 13, 3908. [Google Scholar] [CrossRef] [PubMed]
- Barba-Ostria, C.; Carrera-Pacheco, S.E.; Gonzalez-Pastor, R.; Heredia-Moya, J.; Mayorga-Ramos, A.; Rodríguez-Pólit, C.; Zúñiga-Miranda, J.; Arias-Almeida, B.; Guamán, L.P. Evaluation of Biological Activity of Natural Compounds: Current Trends and Methods. Molecules 2022, 27, 4490. [Google Scholar] [CrossRef]
- Wang, H.; Chen, Y.; Wang, L.; Liu, Q.; Yang, S.; Wang, C. Advancing herbal medicine: Enhancing product quality and safety through robust quality control practices. Front. Pharmacol. 2023, 14, 1265178. [Google Scholar] [CrossRef]
- Kim, H.; Melio, A.; Simianu, V.; Mankaney, G. Challenges and Opportunities for Colorectal Cancer Prevention in Young Patients. Cancers 2025, 17, 2043. [Google Scholar] [CrossRef]
- Sadler, C.R.; Grassby, T.; Hart, K.; Raats, M.; Sokolović, M.; Timotijevic, L. Processed food classification: Conceptualisation and challenges. Trends Food Sci. Technol. 2021, 112, 149–162. [Google Scholar] [CrossRef]
- Li, S.; Liu, J.; Zhang, X.; Gu, Q.; Wu, Y.; Tao, X.; Tian, T.; Pan, G.; Chu, M. The Potential Impact of Antibiotic Exposure on the Microbiome and Human Health. Microorganisms 2025, 13, 602. [Google Scholar] [CrossRef]
- Van Norman, G.A. Limitations of Animal Studies for Predicting Toxicity in Clinical Trials. JACC Basic Transl. Sci. 2020, 5, 387–397. [Google Scholar] [CrossRef]
- Bever, A.M.; Song, M. Early-life exposures and adulthood cancer risk: A life course perspective. JNCI J. Natl. Cancer Inst. 2023, 115, 4–7. [Google Scholar] [CrossRef] [PubMed]
- Beya, M.M.; Netzel, M.E.; Sultanbawa, Y.; Smyth, H.; Hoffman, L.C. Plant-Based Phenolic Molecules as Natural Preservatives in Comminuted Meats: A Review. Antioxidants 2021, 10, 263. [Google Scholar] [CrossRef]
- Baneshi, M.; Aryee, A.N.A.; English, M.; Mkandawire, M. Designing Plant-Based Smart Food Packaging Solutions for Prolonging Consumable Life of Perishable Foods. Food Chem. Adv. 2024, 5, 100769. [Google Scholar] [CrossRef]
- Pramesh, C.S.; Badwe, R.A.; Bhoo-Pathy, N.; Booth, C.M.; Chinnaswamy, G.; Dare, A.J.; de Andrade, V.P.; Hunter, D.J.; Gopal, S.; Gospodarowicz, M.; et al. Priorities for cancer research in low- and middle-income countries: A global perspective. Nat. Med. 2022, 28, 649–657. [Google Scholar] [CrossRef]
- Popkin, B.M.; Laar, A. Nutrition transition’s latest stage: Are ultra-processed food increases in low- and middle-income countries dooming our preschoolers’ diets and future health? Pediatr. Obes. 2025, 20, e70002. [Google Scholar] [CrossRef] [PubMed]
- Novais, C.; Molina, A.K.; Abreu, R.M.V.; Santo-Buelga, C.; Ferreira, I.C.F.R.; Pereira, C.; Barros, L. Natural Food Colorants and Preservatives: A Review, a Demand, and a Challenge. J. Agric. Food Chem. 2022, 70, 2789–2805. [Google Scholar] [CrossRef]
- Giannakourou, M.C.; Taoukis, P.S. Effect of Alternative Preservation Steps and Storage on Vitamin C Stability in Fruit and Vegetable Products: Critical Review and Kinetic Modelling Approaches. Foods 2021, 10, 2630. [Google Scholar] [CrossRef]
- Mei, J.; Ma, X.; Xie, J. Review on Natural Preservatives for Extending Fish Shelf Life. Foods 2019, 8, 490. [Google Scholar] [CrossRef]
- Siddiqui, S.A.; Khan, S.; Mehdizadeh, M.; Bahmid, N.A.; Adli, D.N.; Walker, T.R.; Perestrelo, R.; Câmara, J.S. Phytochemicals and bioactive constituents in food packaging—A systematic review. Heliyon 2023, 9, e21196. [Google Scholar] [CrossRef]
- Sharman, R.; Harris, Z.; Ernst, B.; Mussallem, D.; Larsen, A.; Gowin, K. Lifestyle Factors and Cancer: A Narrative Review. Mayo Clin. Proc. Innov. Qual. Outcomes 2024, 8, 166–183. [Google Scholar] [CrossRef]
- Loke, Y.L.; Chew, M.T.; Ngeow, Y.F.; Lim, W.W.D.; Peh, S.C. Colon Carcinogenesis: The Interplay Between Diet and Gut Microbiota. Front. Cell. Infect. Microbiol. 2020, 10, 603086. [Google Scholar] [CrossRef]
- Safarchi, A.; Al-Qadami, G.; Tran, C.D.; Conlon, M. Understanding dysbiosis and resilience in the human gut microbiome: Biomarkers, interventions, and challenges. Front. Microbiol. 2025, 16, 1559521. [Google Scholar] [CrossRef] [PubMed]
- Crosbie, E.; Gomes, F.S.; Olvera, J.; Rincón-Gallardo Patiño, S.; Hoeper, S.; Carriedo, A. A policy study on front–of–pack nutrition labeling in the Americas: Emerging developments and outcomes. Lancet Reg. Health Am. 2023, 18, 100400. [Google Scholar] [CrossRef] [PubMed]
- Dutta, D.; Sit, N. Application of natural extracts as active ingredient in biopolymer based packaging systems. J. Food Sci. Technol. 2023, 60, 1888–1902. [Google Scholar] [CrossRef] [PubMed]
| Preservative Name | Type | Mode of Action | Common Applications | Known or Suspected Health Effects | Regulatory Status |
|---|---|---|---|---|---|
| Sodium nitrite | Synthetic | Antimicrobial, antioxidant | Cured meats (sausages, bacon), processed meats | Nitrosamine formation, genotoxicity | Regulated; limits set by FDA/EFSA [32] |
| Sodium nitrate | Synthetic | Antimicrobial precursor | Cured meats, preserved vegetables | Nitrosamine risk under acidic conditions | Regulated [33] |
| Sulfites (SO2, K/Na Bisulfite) | Synthetic | Antimicrobial, anti-browning | Dried fruits, wines, soft drinks | Microbiota disruption, potential asthma exacerbation | Allergen labeling required [34] |
| BHA/BHT | Synthetic | Lipid oxidation inhibitor | Snack foods, oils, baked goods | Oxidative stress, pro-oxidant effects in vivo | GRAS; debated globally [35] |
| Benzoates (sodium benzoate) | Synthetic | Antimicrobial (preserves acids) | Beverages, jams, acidic products | DNA damage, possible microbiota imbalance | E211 (EU); regulated [36] |
| Potassium sorbate | Synthetic | Antifungal | Cheese, bakery products | Generally safe; mild irritant in excess | GRAS (FDA), E202 (EU) [37] |
| Sorbic acid | Synthetic | Antifungal | Beverages, jams, dairy products | Minimal risk under ADI limits | EFSA acceptable daily intake [38] |
| Calcium propionate | Synthetic | Mold inhibitor | Bakery goods | Generally recognized as safe; some behavioral concerns | Extensively studied; GRAS [39] |
| Clove oil | Natural | Antimicrobial, antioxidant | Spices, sauces, preserved vegetables | Generally recognized as safe; limited long-term data | Natural additive; regional variation [40] |
| Ginger extract | Natural | Antimicrobial, pH modulation | Beverages, marinades, pickles | Minimal adverse effects; efficacy under study | Under review in some jurisdictions [41] |
| Nisin | Natural (peptide) | Bacteriocin targeting Gram-positives | Cheese, meat products | Safe, scalable use under investigation | Approved by FDA, EFSA [42] |
| Rosemary extract | Natural | Antioxidant, antimicrobial | Oils, dressings, processed meats | Low toxicity; antioxidant-rich | Emerging approval paths [43] |
| Green tea polyphenols | Natural | Antioxidant | Beverage preservation, meat systems | Promising safety; efficacy still being studied | Under research for food-grade use [44] |
| Category | Examples | Primary Composition | Functional Role in Foods | Associated Health Effects |
|---|---|---|---|---|
| Synthetic preservatives | Nitrites/nitrates | Inorganic salts (NO2−, NO3−) | Color stabilization in meats; antimicrobial action | May form carcinogenic nitrosamines; linked to gut microbiota disruption [45] |
| Benzoates (e.g., sodium benzoate) | Aromatic carboxylic acid derivative | Inhibits yeast, mold, and bacteria | Potential allergic reactions; microbiome alteration [46] | |
| Sorbates (e.g., potassium sorbate) | Unsaturated fatty acid salt | Antifungal activity extends shelf life | Generally regarded as safe, but may cause mild irritation at high doses [47] | |
| Natural preservatives | Flavonoids (e.g., quercetin, catechins) | Polyphenolic compounds | Antioxidant; antimicrobial; color stabilization | Protective against oxidative stress; gut microbiota modulation [48] |
| Tannins | Polyphenolic biomolecules | Astringent; antimicrobial; antioxidant | Potential anti-inflammatory effects; high doses may reduce nutrient absorption [49] | |
| Phenolic acids (e.g., gallic acid, ferulic acid) | Hydroxybenzoic and hydroxycinnamic acids | Antimicrobial; antioxidant | May support gut health; anti-inflammatory properties [50] | |
| Essential oils (e.g., thymol, carvacrol, eugenol) | Volatile terpenoids and phenylpropanoids | Broad-spectrum antimicrobial; flavor enhancement | Possible anti-inflammatory and immunomodulatory benefits; sensory changes at high concentrations [51] |
| Region | Sample Size/Cohort | Focus (Preservatives/Diet Type) | Key Findings | Limitations |
|---|---|---|---|---|
| France | ~106,000 | Nitrate, nitrite, N-nitroso compounds | Positive association with colorectal cancer (long-term exposure) | Limited to adult CRC, not EOCRC specifically [83] |
| USA | 214,797 participants; 3217 CRC cases | Sulfur microbial diet (processed meats, low veg) | HR 1.27 (distal CRC) in the highest quintile of sulfur diet | Not stratified for EOCRC [84] |
| Multiple | 26 studies across regions | Western diet, processed meat, sugary drinks | Processed foods are consistent modifiable risk factors in EOCRC | Heterogeneous designs, few preservative-specific data [85] |
| UK/global | Experimental/mechanistic | Sodium nitrite servings in the diet | Processed meats linked to CRC pathogenesis in model systems | Animal/mechanistic relevance only [86] |
| France | 79,284 women | Food additive nitrites/nitrates | HR ~1.22–1.26 for colorectal cancer (not statistically significant for CRC) | Underpowered for CRC subtype, observational [87] |
| Preservative/Group | Study Design & Region | Cohort Size | Risk Estimate (RR/HR/OR, CI) | Key Note |
|---|---|---|---|---|
| Nitrites/nitrates | Prospective cohort (Europe, EPIC) | ~520,000 | HR 1.17 (95% CI 1.02–1.34) | Processed meat intake linked to CRC risk [88]. |
| Sodium benzoate | Case–control (Asia) | ~2500 cases | OR 1.22 (95% CI 1.01–1.48) | Higher intake associated with EOCRC in younger adults [89]. |
| Sulphites | Retrospective cohort (Australia) | ~45,000 | RR 1.11 (95% CI 0.97–1.26) | No strong association; signals require more data [90]. |
| General processed foods (multiple additives) | Multi-country pooled analysis | >1 million | HR 1.25 (95% CI 1.10–1.40) | Preservative-rich UPFs linked to EOCRC onset [91]. |
| Preservative Type | Examples | Relative Risk | Key Concerns/Notes |
|---|---|---|---|
| High risk | Nitrites, nitrates | High | Formation of carcinogenic N-nitroso compounds; strongly linked to colorectal cancer in epidemiological and animal studies [139]. |
| Medium risk | Benzoates | Medium | Potential to disrupt gut microbiota and induce oxidative stress; limited but concerning evidence from in vitro and case–control studies [140]. |
| Low risk | Sorbates | Low | Minimal genotoxic or carcinogenic evidence; generally considered safe at regulatory levels [141]. |
| Natural preservatives | Fermentation-derived sulfites, plant extracts | Generally low | A safer profile, but risks include allergenicity (sulfites) and inconsistent potency of plant-derived compounds [142]. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mafe, A.N.; Büsselberg, D. Food Preservatives and the Rising Tide of Early-Onset Colorectal Cancer: Mechanisms, Controversies, and Emerging Innovations. Foods 2025, 14, 3079. https://doi.org/10.3390/foods14173079
Mafe AN, Büsselberg D. Food Preservatives and the Rising Tide of Early-Onset Colorectal Cancer: Mechanisms, Controversies, and Emerging Innovations. Foods. 2025; 14(17):3079. https://doi.org/10.3390/foods14173079
Chicago/Turabian StyleMafe, Alice N., and Dietrich Büsselberg. 2025. "Food Preservatives and the Rising Tide of Early-Onset Colorectal Cancer: Mechanisms, Controversies, and Emerging Innovations" Foods 14, no. 17: 3079. https://doi.org/10.3390/foods14173079
APA StyleMafe, A. N., & Büsselberg, D. (2025). Food Preservatives and the Rising Tide of Early-Onset Colorectal Cancer: Mechanisms, Controversies, and Emerging Innovations. Foods, 14(17), 3079. https://doi.org/10.3390/foods14173079







