Interaction Effect of Food Insecurity and Stroke on the Risk of All-Cause Mortality: NHANES 2015–2018
Abstract
1. Introduction
2. Methods
2.1. Study Participants and Procedures
2.2. Measures
2.2.1. Outcome Variable
2.2.2. Predictor Variables
2.2.3. Key Health-Related and Demographic Variables
2.3. Statistical Analysis
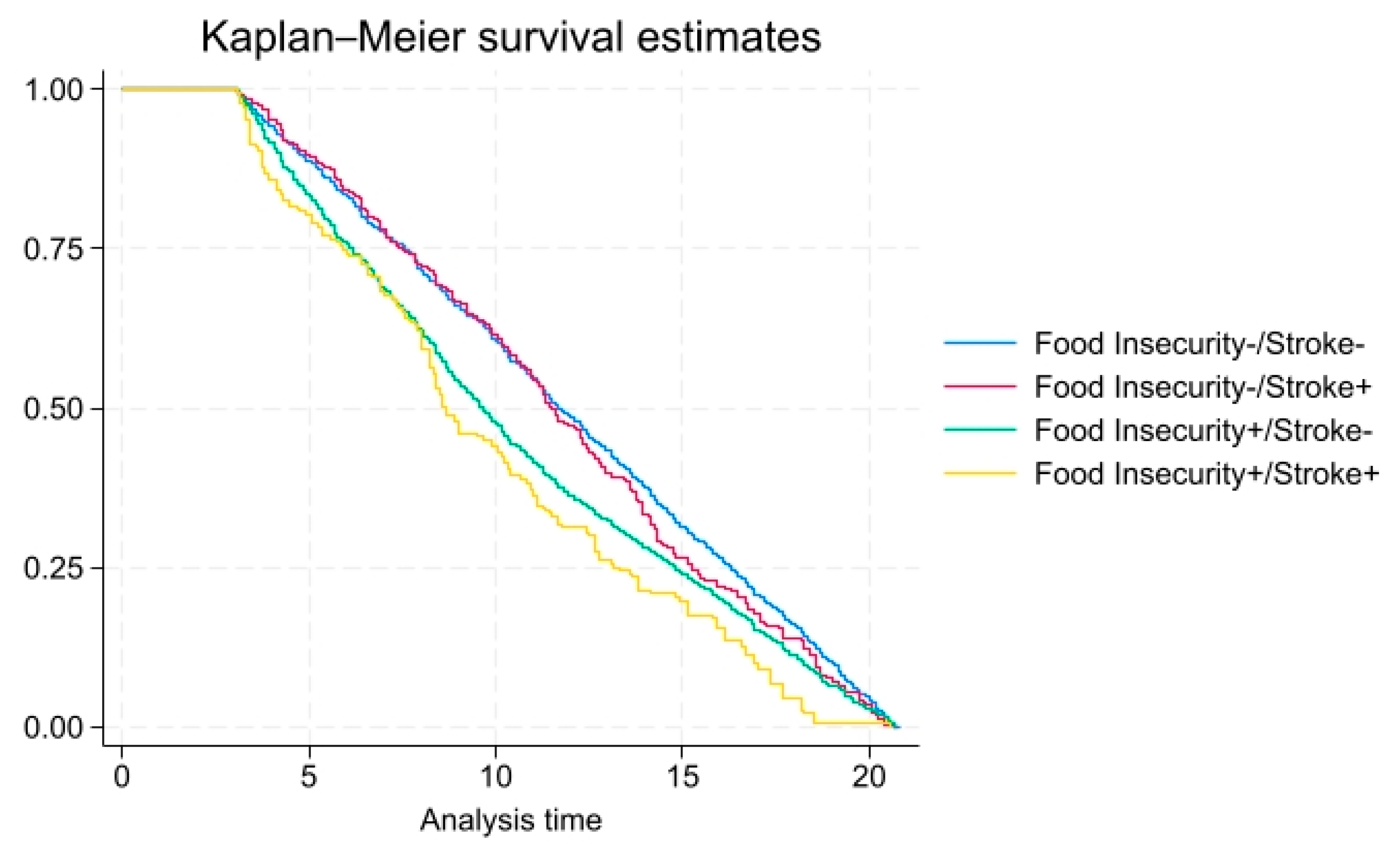
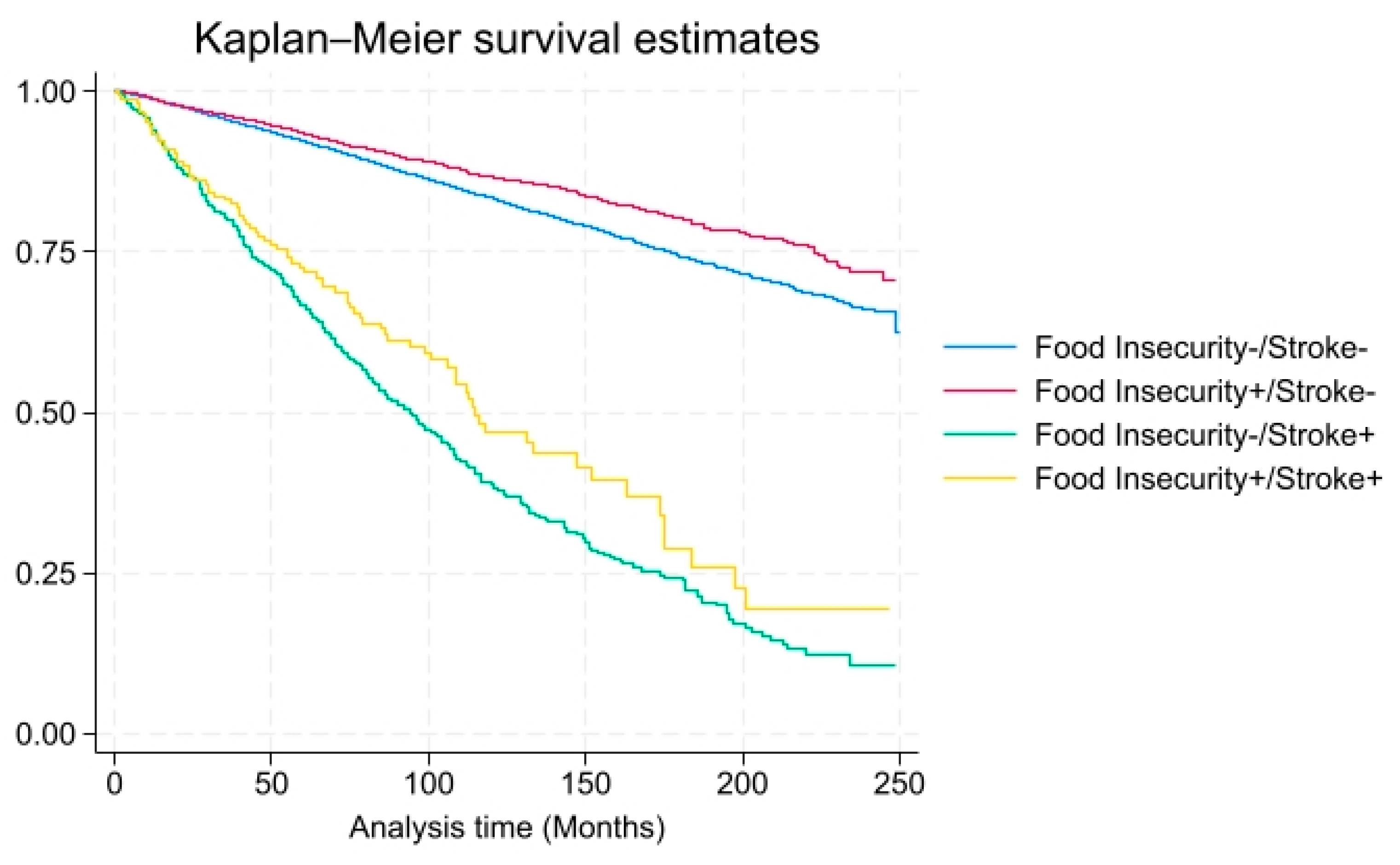
3. Results
4. Discussion
4.1. Limitations
4.2. Recommendations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- FAO. The State of Food Insecurity in the World 2001; FAO: Rome, Italy, 2002; Available online: http://www.fao.org/3/y1500e/y1500e00.htm (accessed on 13 November 2020).
- FAO. Hunger and Food Insecurity. Available online: https://www.fao.org/hunger/en (accessed on 13 November 2020).
- Khubchandani, J.; Banerjee, S.; Kopera-Frye, K.; Gonzales-Lagos, R.; Onukogu, C. Food insecurity and mortality risk among adults with Chronic Kidney Disease: A longitudinal cohort study of NHANES. Nutrire 2024, 49, 52. [Google Scholar] [CrossRef]
- Gundersen, C.; Ziliak, J.P. Food Insecurity and Health Outcomes. Health Aff. 2015, 34, 1830–1839. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, S.; Radak, T.; Khubchandani, J.; Gonzales-Lagos, R.; Dunn, P. Food insecurity and the risk of mortality among Hispanics with hypertension. Nutr. Metab. Cardiovasc. Dis. 2024, 34, 2555–2561. [Google Scholar] [CrossRef]
- Odoms-Young, A.; Brown, A.G.; Agurs-Collins, T.; Glanz, K. Food insecurity, neighborhood food environment, and health disparities: State of the science, research gaps and opportunities. Am. J. Clin. Nutr. 2024, 119, 850–861. [Google Scholar] [CrossRef]
- United States Department of Agriculture. Household Food Security in the United States, 2024; United States Department of Agriculture: Washington, DC, USA, 2024. Available online: https://www.ers.usda.gov/publications/ (accessed on 5 June 2025).
- National Center for Health Statistics (NCHS). Health Disparities in the United States: Food Insecurity and Chronic Disease Risk. 2020. Available online: https://www.cdc.gov/nchs/index.html (accessed on 5 June 2025).
- Centers for Disease Control and Prevention (CDC). Stroke Facts and Statistics; National Center for Health Statistics: Hyattsville, MD, USA, 2020. Available online: https://www.cdc.gov/stroke/facts.htm (accessed on 5 June 2025).
- Dennard, E.; Kristjansson, E.; Tchangalova, N.; Totton, S.; Winham, D.; O’Connor, A. Food insecurity among African Americans in the United States: A scoping review. PLoS ONE 2022, 17, e0274434. [Google Scholar] [CrossRef] [PubMed]
- Ing, C.T.; Clemens, B.; Ahn, H.J.; Kaholokula, J.K.A.; Hovmand, P.S.; Seto, T.B.; Novotny, R. Food insecurity and blood pressure in a multiethnic population. Int. J. Environ. Res. Public Health 2023, 20, 6242. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Schwedhelm, C.; Hoffmann, G.; Lampousi, A.M.; Knüppel, S.; Iqbal, K.; Bechthold, A.; Schlesinger, S.; Boeing, H. Food groups and risk of all-cause mortality: A systematic review and meta-analysis of prospective studies. Am. J. Clin. Nutr. 2017, 105, 1462–1473. [Google Scholar] [CrossRef]
- Banerjee, S.; Radak, T. Food insecurity and its impact on health: Examining risk factors and long-term outcomes. J. Nutr. Health 2019, 72, 212–225. [Google Scholar]
- Banerjee, S.; Radak, T.; Khubchandani, J.; Dunn, P. Food insecurity and mortality in American adults: Results from the NHANES-linked mortality study. Health Promot. Pract. 2021, 22, 204–214. [Google Scholar] [CrossRef]
- Walker, R.J.; Chawla, A.; Garacci, E.; Williams, J.S.; Mendez, C.; Ozieh, M.N.; Egede, L.E. Assessing the relationship between food insecurity and mortality among US adults. Ann. Epidemiol. 2019, 32, 43–48. [Google Scholar] [CrossRef]
- Kim-Tenser, M.A.; Ovbiagele, B.; Markovic, D.; Towfighi, A. Prevalence and predictors of food insecurity among stroke survivors in the United States. Stroke 2022, 53, 3369–3374. [Google Scholar] [CrossRef]
- Kirolos, A.; Goyheneix, M.; Eliasz, M.K.; Chisala, M.; Lissauer, S.; Gladstone, M.; Kerac, M. Neurodevelopmental, cognitive, behavioural and mental health impairments following childhood malnutrition: A systematic review. BMJ Glob. Health 2022, 7, e009330. [Google Scholar] [CrossRef] [PubMed]
- McMichael, A.J.; McGuinness, B.; Lee, J.; Minh, H.V.; Woodside, J.V.; McEvoy, C.T. Food insecurity and brain health in adults: A systematic review. Crit. Rev. Food Sci. Nutr. 2022, 62, 8728–8743. [Google Scholar] [CrossRef] [PubMed]
- Khubchandani, J.; Banerjee, S.; Gonzales-Lagos, R.; Kopera-Frye, K. Food Insecurity is Associated with a higher risk of mortality among Colorectal Cancer survivors. Gastrointest. Disord. 2024, 6, 461–467. [Google Scholar] [CrossRef]
- Banerjee, S.; Radak, T. Association between food insecurity, cardiorenal syndrome and all-cause mortality among low-income adults. Nutr. Health 2019, 25, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Chang, R.; Javed, Z.; Taha, M.; Yahya, T.; Valero-Elizondo, J.; Brandt, E.J.; Cainzos-Achirica, M.; Mahajan, S.; Ali, H.J.; Nasir, K. Food insecurity and cardiovascular disease: Current trends and future directions. Am. J. Prev. Cardiol. 2022, 9, 100303. [Google Scholar] [CrossRef]
- Brandt, E.J.; Mozaffarian, D.; Leung, C.W.; Berkowitz, S.A.; Murthy, V.L. Diet and food and nutrition insecurity and cardiometabolic disease. Circ. Res. 2023, 132, 1692–1706. [Google Scholar] [CrossRef]
- Brandt, E.J.; Tobb, K.; Cambron, J.C.; Ferdinand, K.; Douglass, P.; Nguyen, P.K.; Vijayaraghavan, K.; Islam, S.; Thamman, R.; Watson, K.; et al. Assessing and addressing social determinants of cardiovascular health: JACC state-of-the-art review. J. Am. Coll. Cardiol. 2023, 81, 1368–1385. [Google Scholar] [CrossRef]
- Te Vazquez, J.; Feng, S.N.; Orr, C.J.; Berkowitz, S.A. Food insecurity and cardiometabolic conditions: A review of recent research. Curr. Nutr. Rep. 2021, 10, 243–254. [Google Scholar] [CrossRef]
- Zoellner, E.R.; Patterson, M.A.; Sharrief, A.Z.; Savitz, S.I.; Tucker, W.J.; Miketinas, D.C. Dietary intake and quality among stroke survivors: NHANES 1999–2018. J. Nutr. 2023, 153, 3032–3040. [Google Scholar] [CrossRef]
- Parekh, T.; Xue, H.; Cheskin, L.J.; Cuellar, A.E. Food insecurity and housing instability as determinants of cardiovascular health outcomes: A systematic review. Nutr. Metab. Cardiovasc. Dis. 2022, 32, 1590–1608. [Google Scholar] [CrossRef]
- Springer, M.V.; Skolarus, L.E.; Patel, M. Food insecurity and perceived financial stress are associated with cost-related medication non-adherence in stroke. J. Health Care Poor Underserved 2023, 34, 625–639. [Google Scholar] [CrossRef]
- Mendy, V.L.; Vargas, R.; Cannon-Smith, G.; Payton, M.; Enkhmaa, B.; Zhang, L. Food insecurity and cardiovascular disease risk factors among Mississippi adults. Int. J. Environ. Res. Public Health 2018, 15, 2016. [Google Scholar] [CrossRef] [PubMed]
- Brandt, E.J.; Chang, T.; Leung, C.; Ayanian, J.Z.; Nallamothu, B.K. Food insecurity among individuals with cardiovascular disease and cardiometabolic risk factors across race and ethnicity in 1999–2018. JAMA Cardiol. 2022, 7, 1218–1226. [Google Scholar] [CrossRef] [PubMed]
- Dong, T.; Harris, K.; Freedman, D.; Janus, S.; Griggs, S.; Iyer, Y.; Nasir, K.; Neeland, I.J.; Rajagopalan, S.; Al-Kindi, S.G. Food insecurity and atherosclerotic cardiovascular disease risk in adults with diabetes. Nutrition 2023, 106, 111865. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Aspry, K.E.; Garfield, K.; Kris-Etherton, P.; Seligman, H.; Velarde, G.P.; Williams, K.; Yang, E.; ACC Prevention of Cardiovascular Disease Section Nutrition and Lifestyle Working Group and Disparities of Care Working Group. “Food is medicine” strategies for nutrition security and cardiometabolic health equity: JACC state-of-the-art review. J. Am. Coll. Cardiol. 2024, 83, 843–864. [Google Scholar] [CrossRef] [PubMed]
- De Marchis, E.H.; Torres, J.M.; Benesch, T.; Fichtenberg, C.; Allen, I.E.; Whitaker, E.M.; Gottlieb, L.M. Interventions addressing food insecurity in health care settings: A systematic review. Ann. Fam. Med. 2019, 17, 436–447. [Google Scholar] [CrossRef]
- Ostrer, I.R.; Seligman, H.K. Food Insecurity, Health, and Health Care in the US. JAMA 2025, 333, 1352–1353. [Google Scholar] [CrossRef]
- Frost, K.; Stafos, A.; Metcalf, A.L.; DeBourge, W.; Friesen, M.; Bryant, R.; Lawver, L.; Bullock, J.; Williams, K. Knowledge and barriers related to food insecurity screening in healthcare settings. Public Health Nurs. 2022, 39, 770–777. [Google Scholar] [CrossRef]
- Price, J.H.; Khubchandani, J.; Webb, F.J. Poverty and health disparities: What can public health professionals do? Health Promot. Pract. 2018, 19, 170–174. [Google Scholar] [CrossRef]
- Fraze, T.K.; Brewster, A.L.; Lewis, V.A.; Beidler, L.B.; Murray, G.F.; Colla, C.H. Prevalence of screening for food insecurity, housing instability, utility needs, transportation needs, and interpersonal violence by US physician practices and hospitals. JAMA Netw. Open 2019, 2, e1911514. [Google Scholar] [CrossRef] [PubMed]
- Sharma, V.; Sharma, R. Food is medicine initiative for mitigating food insecurity in the United States. J. Prev. Med. Public Health 2024, 57, 96. [Google Scholar] [CrossRef] [PubMed]
- US Preventive Services Task Force; Nicholson, W.K.; Silverstein, M.; Wong, J.B.; Chelmow, D.; Coker, T.R.; Fernandez, A.; Gibson, E.; Jaén, C.R.; Krousel-Wood, M.; et al. Screening for Food Insecurity: US Preventive Services Task Force Recommendation Statement. JAMA 2025, 333, 1333–1339. [Google Scholar] [PubMed]
- Oronce, C.I.A.; Miake-Lye, I.M.; Begashaw, M.M.; Booth, M.; Shrank, W.H.; Shekelle, P.G. Interventions to address food insecurity among adults in Canada and the US: A systematic review and meta-analysis. JAMA Health Forum 2021, 2, e212001. [Google Scholar] [CrossRef]

| Characteristics | Total Population (n = 16,308) | Stroke (+) (n = 647) | Stroke (−) (n = 15,661) |
|---|---|---|---|
| Food Insecurity * | 16.3 (14.5–18.0) | 23.9 (16.2–31.6) | 16.0 (14.3–17.7) |
| Smoking Status ** | |||
| Never Smoked | 56.9 (55.3–58.4) | 40.6 (35.6–45.6) | 57.4 (55.8–58.9) |
| Formerly Smoked | 24.5 (23.4–25.7) | 35.6 (30.0–41.2) | 24.2 (23.1–25.3) |
| Current Smoker | 18.6 (17.3–19.8) | 23.8 (18.7–28.9) | 18.4 (17.2–19.7) |
| Chronic Kidney Disease (CKD) ** | 14.1 (13.3–14.9) | 39.6 (35.6–43.5) | 13.3 (12.5–14.1) |
| BMI | |||
| Normal Weight BMI < 25 | 26.2 (24.2–28.1) | 19.5 (13.9–25.0) | 26.4 (24.4–28.4) |
| Overweight BMI = 25–29.9 | 32.0 (30.6–33.4) | 28.9 (22.1–35.7) | 32.1 (30.7–33.5) |
| Obese BMI = 30–39.9 | 33.4 (31.5–35.3) | 40.2 (33.5–47.0) | 33.2 (31.3–35.1) |
| Morbidly obese BMI ≥ 40 | 8.5 (7.5–9.6) | 11.4 (6.4–16.5) | 8.4 (7.3–9.5) |
| Hypertension ** | 33.3 (31.7–34.8) | 74.3 (70.1–78.6) | 32.0 (350.5–33.5) |
| Age ** | 47.9 (0.29) | 64.9 (0.71) | 47.4 (0.29) |
| Gender Females | 51.9 (51.1–52.7) | 55.8 (50.6–61.0) | 51.8 (50.9–52.7) |
| Family Poverty–Income Ratio (PIR < 1) ** | 14.3 (12.7–15.9) | 20.5 (14.9–26.10) | 14.1 (12.5–15.7) |
| Ethnicity ** | |||
| Non-Hispanic White | 63.9 (60.1–67.8) | 67.2 (61.0–73.4) | 63.8 (60.0–67.7) |
| Non-Hispanic Black | 11.4 (9.3–13.5) | 15.2 (11.7–18.7) | 11.3 (9.2–13.40 |
| Hispanic | 15.2 (12.5–18.0) | 8.3 (6.4–10.6) | 15.5 (12.7–18.2) |
| Other | 9.4 (8.1–10.8) | 9.3 (6.6–13.5) | 9.4 (8.1–10.8) |
| Education Level ** | |||
| Some High School | 15.1 (12.6–17.7) | 22.2 (17.2–27.2) | 14.9 (12.4–17.5) |
| High School Graduate | 20.8 (18.8–22.8) | 26.8 (20.3–33.4) | 20.6 (18.5–22.8) |
| Some College or Above | 64.1 (60.5–67.6) | 51.0 (44.4–57.5) | 64.4 (60.8–68.1) |
| Marital Status ** | |||
| Married | 54.3 (52.3–56.3) | 50.4 (42.2–56.6) | 54.4 (52.4–56.5) |
| Widowed | 5.9 (5.4–5.4) | 19.0 (14.8–23.2) | 5.5 (5.0–6.0) |
| Divorced | 10.2 (9.5–10.9) | 15.1 (11.0–19.2) | 10.0 (9.3–10.8) |
| Separated | 2.5 (2.2–2.9) | 2.3 (1.3–3.9) | 2.5 (2.2–2.9) |
| Never Married | 18.5 (17.3–19.8) | 8.7 (6.7–11.1) | 18.8 (17.5–20.1) |
| Living With Partner | 8.6 (7.8–9.5) | 4.6 (3.0–7.0) | 8.7 (7.9–9.7) |
| All Deaths (N, %) ** | 821 (3.8%) | 118 (17.0%) | 703 (3.4%) |
| Total Population HR (95%CI) | Food Insecurity Only HR (95%CI) | Stroke Only HR (95%CI) | Stroke and Food Insecurity HR (95%CI) | |
|---|---|---|---|---|
| Stroke/Food Insecurity | 1.35 (0.79–2.32) | 1.13 (0.63–2.03) | 0.87 (0.39–1.94) | 3.66 (1.64–8.14) ** |
| Smoking Status | ||||
| Never Smoked (Ref.) | Ref | Ref | Ref | Ref |
| Formerly Smoked | 1.62 (1.11–2.36) ** | 1.74 (1.12–2.70) * | 1.47 (0.67–3.25) | 0.95 (0.36–2.54) |
| Current Smoker | 1.87 (1.17–3.00) | 1.98 (1.12–3.50) | 1.73 (0.94–3.17) | 1.32 (0.39–4.46) |
| Chronic Kidney Disease (CKD) | 2.39 (1.64–3.50) ** | 2.43 (1.68–3.52) ** | 2.47(1.62–3.78) ** | 2.77 (1.12–6.85) * |
| Hypertension | 1.45 (1.01–2.07) * | 1.52 (1.03–2.25) * | 1.35 (0.82–2.22) | 0.79 (0.40–1.57) |
| Age | 1.07 (1.05–1.10) ** | 1.07 (1.05–1.10) ** | 1.09 (1.06–1.11) ** | 1.07 (1.03–1.12) * |
| Gender (Ref. Female) | 1.70 (1.21–2.40) ** | 1.69 (1.17–2.44) ** | 2.20 (1.38–3.52) ** | 1.25 (0.37–4.21) * |
| Family Poverty–Income Ratio (Ref: PIR > 1) | 2.54 (1.56–4.13) ** | 2.70 (1.43–5.08) ** | 2.72 (1.55–4.78) ** | 0.85 (0.25–2.90) |
| Ethnicity | ||||
| Non-Hispanic White | Ref | Ref | Ref | Ref |
| Non-Hispanic Black | 0.66 (0.43–1.00) | 0.69 (0.44–1.08) | 0.64 (0.33–1.24) | 0.31 (0.07–1.40) |
| Hispanic | 0.71 (0.48–1.05) | 0.71 (0.52–0.98)* | 1.13 (0.68–1.90) | 0.89 (0.20–4.05) |
| Other | 1.28 (0.77–2.13) | 1.36 (0.72–2.57) | 1.35 (0.68–2.65) | 0.49 (0.09–2.63) |
| Education Level | ||||
| Some College or Above | Ref | Ref | Ref | Ref |
| Some High School | 0.91 (0.55–1.51) | 0.98 (0.66–1.47) | 0.74 (0.24–1.55) | 0.46 (0.03–6.93) |
| High School Graduate | 1.03 (0.67–1.60) | 0.93 (0.61–1.43) | 1.01 (0.56–1.84) | 1.60 (0.53–4.85) |
| Marital Status | 1.51 (0.99–2.31) | 1.49 (0.97–2.28) * | 1.69 (0.99–2.86) | 2.67 (1.19–5.97) * |
| Total Population HR (95%CI) | Food Insecurity Only HR (95%CI) | Stroke Only HR (95%CI) | Stroke and Food Insecurity HR (95%CI) | |
|---|---|---|---|---|
| Stroke/Food Insecurity | 0.97 (0.56–1.68) | 0.74 (0.40–1.36) | 0.74 (0.30–1.85) | 7.20 (0.73–70.78) |
| Smoking Status | ||||
| Never Smoked (Ref.) | Ref | Ref | Ref | Ref |
| Formerly Smoked | 1.48 (0.73–0.71) | 1.56 (0.74–3.30) | 1.30 (0.55–3.06) | 0.34 (0.02–7.11) |
| Current Smoker | 1.4 (0.53–4.19) | 1.67 (0.50–5.61) | 1.80 (0.69–4.71) | 0.55 (0.01–33.01) |
| Chronic Kidney Disease (CKD) | 2.36 (1.49–3.73) ** | 2.25 (1.51–3.35) | 2.49 (1.52–4.26) ** | 2.92 (0.19–45.18) |
| Hypertension | 1.25 (0.66–2.36) | 1.31 (0.67–2.55) | 1.29 (0.53–3.12) | 0.73 (0.18 = 2.95) |
| BMI | 1.00 (0.95–1.05) | 1.00 (0.96–1.05) | 1.02 (0.98–1.06) | 0.85 (0.70–1.03) |
| Age | 1.07 (1.04–1.10) ** | 1.07 (1.04–1.10) ** | 1.09 (1.06–1.11) | 1.05 (1.00–1.11) * |
| Family Poverty–Income Ratio (Ref: PIR > 1) | 2.94(1.82–5.35) ** | 3.33 (1.54–7.18) ** | 2.63 (115–6.05) * | 0.58 (0.07–5.12) |
| Ethnicity | ||||
| Non-Hispanic White | Ref | Ref | Ref | Ref |
| Non-Hispanic Black | 1.10 (0.55–2.22) | 1.19 (0.60–2.39) | 1.13 (0.57–2.23) | 0.28 (0.05–1.59) |
| Hispanic | 0.84 (0.47–1.53) | 0.92 (0.52–1.61) | 1.12 (0.56–2.25) | 0.14 (0.01–3.11) |
| Other | 0.95 (0.38–2.36) | 0.92 (0.31–2.72) | 1.07 (0.39–2.96) | 0.41 (0.01–50.4) |
| Education Level | ||||
| Some College or Above | Ref | Ref | Ref | Ref |
| Some High School | 0.72 (0.43–1.22) | 0.66 (0.44–1.00) | 0.89 (0.49–1.62) | 1.21 (0.06–23.52) |
| High School Graduate | 1.17 (0.46–2.96) | 0.97 (0.33–2.89) | 1.11 (0.31–4.00) | 4.63 (0.60–35.91) |
| Marital Status | 1.51 (0.77–2.95) | 1.53 (0.70–3.36) | 1.40 (0.65–3.02) | 2.59 (0.23–28.94) |
| Total Population HR (95%CI) | Food Insecurity Only HR (95%CI) | Stroke Only HR (95%CI) | Stroke and Food Insecurity HR (95%CI) | |
|---|---|---|---|---|
| Stroke/Food Insecurity | 2.33 (1.09–4.99) | 2.03 (0.87–4.71) | 1.36 (0.45–4.12) | 8.76 (1.36–56.49) * |
| Smoking Status | ||||
| Never Smoked (Ref.) | Ref | Ref | Ref | Ref |
| Formerly Smoked | 1.39 (0.61–3.16) | 1.54 (0.57–4.11) | 1.51 (0.45–5.05) | 3.60 (0.09–145.76) |
| Current Smoker | 2.35 (1.19–4.68) * | 2.47 (1.13–5.41) | 0.68 (0.12–3.78) | 5.98 (0.02–1500.34) |
| Chronic Kidney Disease (CKD) | 2.31 (1.12–4.75) | 2.49 (1.28–4.84) | 2.28 (1.18–4.42) * | 7.04 (0.31–158.36) |
| Hypertension | 1.29 (0.70–2.36) | 1.18 (059–2.35) | 1.03 (0.49–2.18) | 7.61 (0.19–297.79) |
| BMI | 1.03 (0.98–1.08) | 1.03 (0.99–1.08) | 1.00 (0.94–1.06) | 0.91 (0.77–1.07) |
| Age | 1.09 (1.06–1.11) ** | 1.09 (1.06–1.11) | 1.09 (1.05–1.13) | 1.07 (0.95–1.21) |
| Family Poverty–Income Ratio (Ref: PIR > 1) | 1.61 (0.84–3.07) | 1.53 (0.68–3.48) | 1.94 (0.99–3.77) | 0.14 (0.00–8.64) |
| Ethnicity | ||||
| Non-Hispanic White | Ref | Ref | Ref | Ref |
| Non-Hispanic Black | 0.29 (0.18–0.47) | 0.34 (020–0.56) | 0.18 (0.03–1.21) | --- |
| Hispanic | 0.55 (0.26–1.18) | 0.52 (0.23–1.21) | 1.29 (0.45–3.68) | --- |
| Other | 1.59 (0.78–3/23) | 1.85 (0.75–4.53) | 1.70 (0.47–6.01) | --- |
| Education Level | ||||
| Some College or Above | Ref | Ref | Ref | Ref |
| Some High School | 1.40 (0.62–3.18) | 1.87 (0.84–4.18) | 0.79 (0.33–1.91) | 0.04 (0.01–0.97) * |
| High School Graduate | 1.14 (0.58–2.32) | 1.13 (0.52–2.44) | 1.19 (0.55–2.55) | 5.72 (0.78–41.78) |
| Marital Status | 1.57 (0.43–5.69) | 1.45 (0.37–5.64) | 2.56 (0.54–12.09) | 21.62 (0.25–1864.94) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Banerjee, S.; Davis, W.S.; Khubchandani, J.; Dunn, P. Interaction Effect of Food Insecurity and Stroke on the Risk of All-Cause Mortality: NHANES 2015–2018. Foods 2025, 14, 2281. https://doi.org/10.3390/foods14132281
Banerjee S, Davis WS, Khubchandani J, Dunn P. Interaction Effect of Food Insecurity and Stroke on the Risk of All-Cause Mortality: NHANES 2015–2018. Foods. 2025; 14(13):2281. https://doi.org/10.3390/foods14132281
Chicago/Turabian StyleBanerjee, Sri, W. Sumner Davis, Jagdish Khubchandani, and Patrick Dunn. 2025. "Interaction Effect of Food Insecurity and Stroke on the Risk of All-Cause Mortality: NHANES 2015–2018" Foods 14, no. 13: 2281. https://doi.org/10.3390/foods14132281
APA StyleBanerjee, S., Davis, W. S., Khubchandani, J., & Dunn, P. (2025). Interaction Effect of Food Insecurity and Stroke on the Risk of All-Cause Mortality: NHANES 2015–2018. Foods, 14(13), 2281. https://doi.org/10.3390/foods14132281








