The Role of Tableware Size in Healthy Eating—Effects on Downstream Food Intake
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Testing Food Models
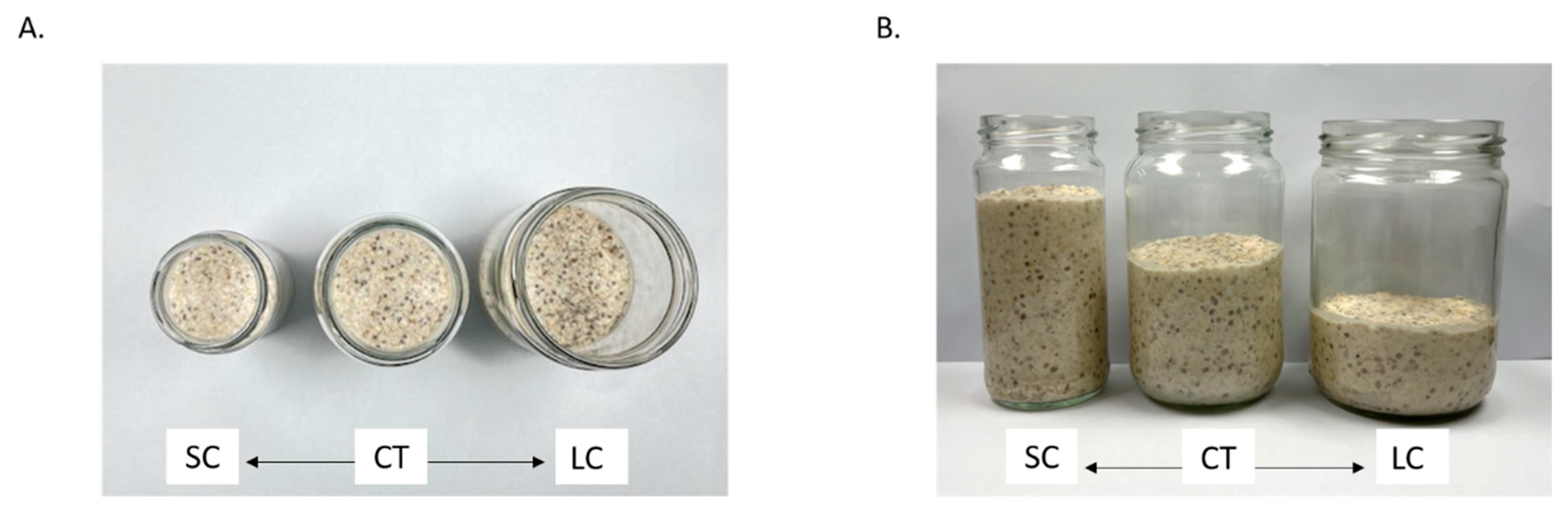
2.3. Serving Jars
2.4. Experimental Procedure
2.5. Data Analyses
2.5.1. Data Pre-Processing
2.5.2. Statistical Analyses
3. Results
3.1. Participant Characteristics
3.2. Effects of the Session Order
3.3. Comparisons of Within-Meal Measures across Three Jar Size Conditions
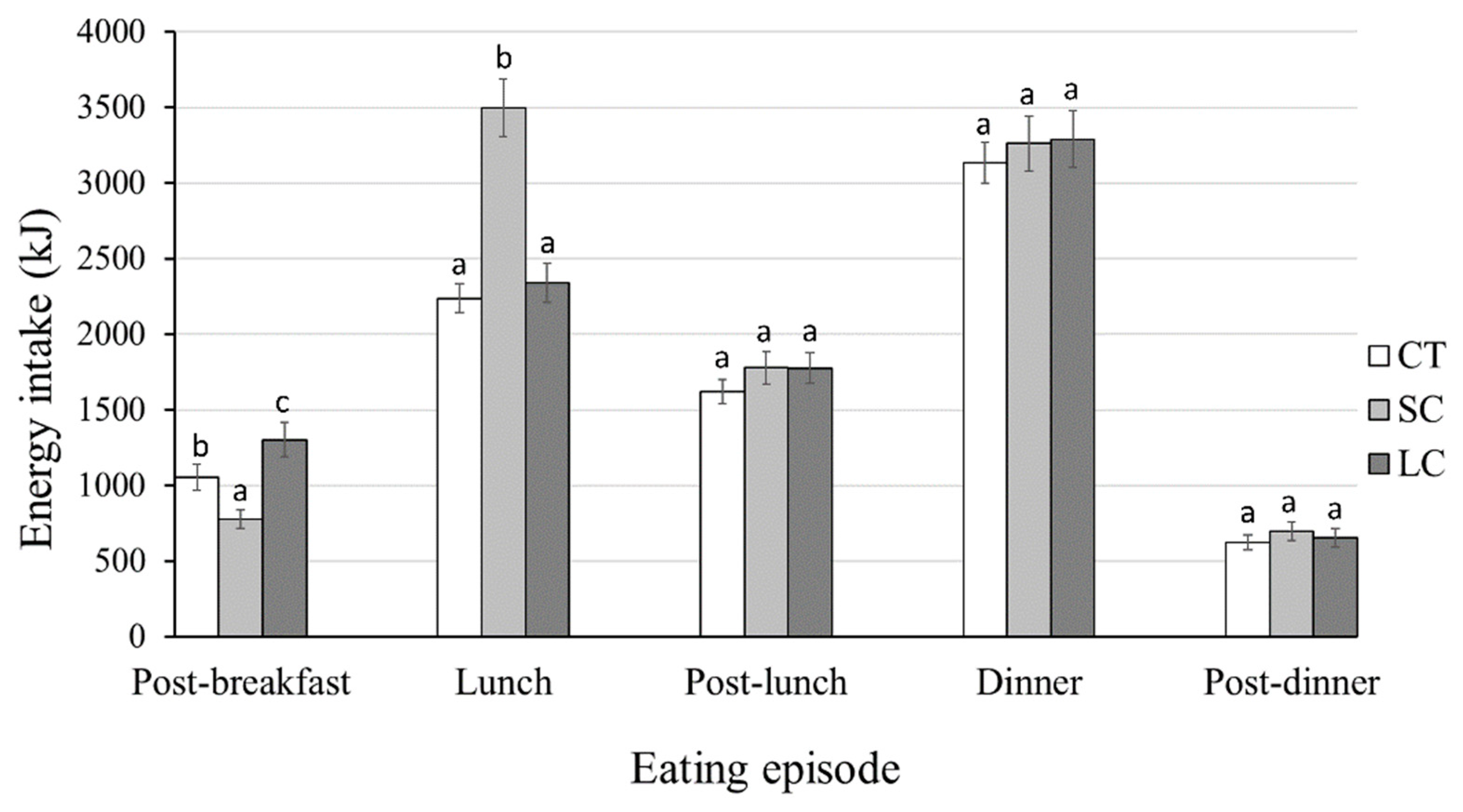
3.4. Effects of Jar Size on Subsequent Energy Intake
3.5. Debrief from the Participants
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chaput, J.P.; Klingenberg, L.; Astrup, A.; Sjödin, A.M. Modern sedentary activities promote overconsumption of food in our current obesogenic environment. Obes. Rev. 2011, 12, e12–e20. [Google Scholar] [CrossRef] [PubMed]
- Ferretti, F.; Mariani, M.; Sarti, E. Is the development of obesogenic food environments a self-reinforcing process? Evidence from soft drink consumption. Glob. Health 2021, 17, 91. [Google Scholar] [CrossRef]
- De Ridder, D.; De Vet, E.; Stok, M.; Adriaanse, M.; De Wit, J. Obesity, overconsumption and self-regulation failure: The unsung role of eating appropriateness standards. Health Psychol. Rev. 2013, 7, 146–165. [Google Scholar] [CrossRef]
- Cohen, D.A. Neurophysiological pathways to obesity: Below awareness and beyond individual control. Diabetes 2008, 57, 1768–1773. [Google Scholar] [CrossRef] [PubMed]
- Harnischfeger, F.; Dando, R. Obesity-induced taste dysfunction, and its implications for dietary intake. Int. J. Obes. 2021, 45, 1644–1655. [Google Scholar] [CrossRef] [PubMed]
- Wansink, B. Environmental factors that increase the food intake and consumption volume of unknowing consumers. Annu. Rev. Nutr. 2004, 24, 455–479. [Google Scholar] [CrossRef]
- Bschaden, A.; Dörsam, A.; Cvetko, K.; Kalamala, T.; Stroebele-Benschop, N. The impact of lighting and table linen as ambient factors on meal intake and taste perception. Food Qual. Prefer. 2020, 79, 103797. [Google Scholar] [CrossRef]
- Thomas, D.W.; Smith, M. The effect of music on caloric consumption among nursing home residents with dementia of the Alzheimer’s type. Act. Adapt. Aging 2009, 33, 1–16. [Google Scholar] [CrossRef]
- Wang, Q.J.; Spence, C.; Knoeferle, K. Timing is everything: Onset timing moderates the crossmodal influence of background sound on taste perception. J. Exp. Psychol. Hum. Percept. Perform. 2020, 46, 1118–1126. [Google Scholar] [CrossRef]
- Hollands, G.J.; Shemilt, I.; Marteau, T.M.; Jebb, S.A.; Lewis, H.B.; Wei, Y.; Higgins, J.P.; Ogilvie, D. Portion, package or tableware size for changing selection and consumption of food, alcohol and tobacco. Cochrane Database Syst. Rev. 2015, 2018, CD011045. [Google Scholar] [CrossRef]
- Pham, C.; Garg, N. More Than Meets the Eye: The Influence of Tableware Aesthetics on Food Consumption. ACR N. Am. Adv. 2018, 46, 80–85. [Google Scholar]
- Abeywickrema, S.; Oey, I.; Peng, M. Sensory specific satiety or appetite? Investigating effects of retronasally-introduced aroma and taste cues on subsequent real-life snack intake. Food Qual. Prefer. 2022, 100, 104612. [Google Scholar] [CrossRef]
- Wansink, B.; Van Ittersum, K. Portion size me: Plate-size induced consumption norms and win-win solutions for reducing food intake and waste. J. Exp. Psychol. Appl. 2013, 19, 320. [Google Scholar] [CrossRef] [PubMed]
- Van Ittersum, K.; Wansink, B. Plate size and color suggestibility: The Delboeuf illusion’s bias on serving and eating behavior. J. Consum. Res. 2012, 39, 215–228. [Google Scholar] [CrossRef]
- Smith, J.M.; Ditschun, T.L. Controlling satiety: How environmental factors influence food intake. Trends Food Sci. Technol. 2009, 20, 271–277. [Google Scholar] [CrossRef]
- Peng, M.; Adam, S.; Hautus, M.J.; Shin, M.; Duizer, L.M.; Yan, H. See food diet? Cultural differences in estimating fullness and intake as a function of plate size. Appetite 2017, 117, 197–202. [Google Scholar] [CrossRef]
- Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report; National Heart, Lung, and Blood Institute: Bethesda, MD, USA, 1998.
- Robinson, E.; Nolan, S.; Tudur-Smith, C.; Boyland, E.J.; Harrold, J.A.; Hardman, C.A.; Halford, J.C. Will smaller plates lead to smaller waists? A systematic review and meta-analysis of the effect that experimental manipulation of dishware size has on energy consumption. Obes. Rev. 2014, 15, 812–821. [Google Scholar] [CrossRef]
- Anderson, D.A.; Schaumberg, K.; Anderson, L.M.; Reilly, E.E. Is level of intuitive eating associated with plate size effects? Eat. Behav. 2015, 18, 125–130. [Google Scholar] [CrossRef]
- Rolls, B.J.; Roe, L.S.; Halverson, K.H.; Meengs, J.S. Using a smaller plate did not reduce energy intake at meals. Appetite 2007, 49, 652–660. [Google Scholar] [CrossRef]
- Shah, M.; Schroeder, R.; Winn, W.; Adams-Huet, B. A pilot study to investigate the effect of plate size on meal energy intake in normal weight and overweight/obese women. J. Hum. Nutr. Diet. 2011, 24, 612–615. [Google Scholar] [CrossRef]
- Yip, W.; Wiessing, K.R.; Budgett, S.; Poppitt, S.D. Using a smaller dining plate does not suppress food intake from a buffet lunch meal in overweight, unrestrained women. Appetite 2013, 69, 102–107. [Google Scholar] [CrossRef]
- Libotte, E.; Siegrist, M.; Bucher, T. The influence of plate size on meal composition. Literature review and experiment. Appetite 2014, 82, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Holden, S.S.; Zlatevska, N.; Dubelaar, C. Whether Smaller Plates Reduce Consumption Depends on Who’s Serving and Who’s Looking: A Meta-Analysis. J. Assoc. Consum. Res. 2016, 1, 134–146. [Google Scholar] [CrossRef]
- Shimpo, M.; Akamatsu, R. The effects of bowl size and portion size on food intake and fullness ratings in a sample of Japanese men. Public Health Nutr. 2018, 21, 3216–3222. [Google Scholar] [CrossRef] [PubMed]
- Dörsam, A.F.; Weiland, A.; Sauer, H.; Giel, K.E.; Stroebele-Benschop, N.; Zipfel, S.; Enck, P.; Mack, I. The Role of Dishware Size in the Perception of Portion Size in Children and Adolescents with Obesity. Nutrients 2021, 13, 2062. [Google Scholar] [CrossRef]
- Peng, M. How does plate size affect estimated satiation and intake for individuals in normal-weight and overweight groups? Obes. Sci. Pract. 2017, 3, 282–288. [Google Scholar] [CrossRef] [PubMed]
- Wang, E.; Cakmak, Y.O.; Peng, M. Eating with eyes—Comparing eye movements and food choices between overweight and lean individuals in a real-life buffet setting. Appetite 2018, 125, 152–159. [Google Scholar] [CrossRef]
- Zimmerman, A.R.; Mason, A.; Rogers, P.J.; Brunstrom, J.M. Obese and overweight individuals are less sensitive to information about meal times in portion-size judgements. Int. J. Obes. 2018, 42, 905–910. [Google Scholar] [CrossRef]
- Davis, C.; Curtis, C.; Tweed, S.; Patte, K. Psychological factors associated with ratings of portion size: Relevance to the risk profile for obesity. Eat. Behav. 2007, 8, 170–176. [Google Scholar] [CrossRef]
- Rizk, M.T.; Treat, T.A. Sensitivity to portion size of unhealthy foods. Food Qual. Prefer. 2015, 45, 121–131. [Google Scholar] [CrossRef]
- Peng, M.; Cahayadi, J.; Geng, X.; Eidels, A. Mixed messages: Assessing interactions between portion-size and energy-density perceptions in different weight and sex groups. Appetite 2020, 144, 104462. [Google Scholar] [CrossRef] [PubMed]
- Hardman, C.A.; Jones, A.; Burton, S.; Duckworth, J.J.; McGale, L.S.; Mead, B.R.; Roberts, C.A.; Field, M.; Werthmann, J. Food-related attentional bias and its associations with appetitive motivation and body weight: A systematic review and meta-analysis. Appetite 2021, 157, 104986. [Google Scholar] [CrossRef] [PubMed]
- DiSantis, K.I.; Birch, L.L.; Davey, A.; Serrano, E.L.; Zhang, J.; Bruton, Y.; Fisher, J.O. Plate size and children’s appetite: Effects of larger dishware on self-served portions and intake. Pediatrics 2013, 131, e1451–e1458. [Google Scholar] [CrossRef] [PubMed]
- Steenhuis, I.H.; Vermeer, W.M. Portion size: Review and framework for interventions. Int. J. Behav. Nutr. Phys. Act. 2009, 6, 58. [Google Scholar] [CrossRef]
- Haynes, A.; Hardman, C.A.; Makin, A.D.; Halford, J.C.; Jebb, S.A.; Robinson, E. Visual perceptions of portion size normality and intended food consumption: A norm range model. Food Qual Prefer 2019, 72, 77. [Google Scholar] [CrossRef]
- Robinson, E.; Oldham, M.; Cuckson, I.; Brunstrom, J.M.; Rogers, P.J.; Hardman, C.A. Visual exposure to large and small portion sizes and perceptions of portion size normality: Three experimental studies. Appetite 2016, 98, 28–34. [Google Scholar] [CrossRef]
- World Health Organization. Body Mass Index (BMI) Standards. 2021. Available online: https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/body-mass-index (accessed on 5 January 2023).
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Hodge, A.; Patterson, A.J.; Brown, W.J.; Ireland, P.; Giles, G. The Anti Cancer Council of Victoria FFQ: Relative validity of nutrient intakes compared with weighed food records in young to middle-aged women in a study of iron supplementation. Aust. N. Z. J. Public Health 2000, 24, 576–583. [Google Scholar] [CrossRef]
- Abeywickrema, S.; Ginieis, R.; Oey, I.; Perry, T.; Keast, R.S.; Peng, M. Taste but not smell sensitivities are linked to dietary macronutrient composition. Appetite 2023, 181, 106385. [Google Scholar] [CrossRef]
- Chepulis, L.; Hill, S.; Mearns, G. The nutritional quality of New Zealand breakfast cereals: An update. Public Health Nutr. 2017, 20, 3234–3237. [Google Scholar] [CrossRef]
- Williams, E.J. Experimental designs balanced for the estimation of residual effects of treatments. Aust. J. Chem. 1949, 2, 149–168. [Google Scholar] [CrossRef]
- Cardello, A.V.; Schutz, H.G.; Lesher, L.L.; Merrill, E. Development and testing of a labeled magnitude scale of perceived satiety. Appetite 2005, 44, 1–13. [Google Scholar] [CrossRef]
- Forde, C.G. Measuring satiation and satiety. In Methods in Consumer Research; Elsevier: Amsterdam, The Netherlands, 2018; Volume 2, pp. 151–182. [Google Scholar]
- Forde, C.G.; Almiron-Roig, E.; Brunstrom, J.M. Expected satiety: Application to weight management and understanding energy selection in humans. Curr. Obes. Rep. 2015, 4, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Baranowski, T. 24-hour recall and diet record methods. Nutr. Epidemiol. 2012, 40, 49–69. [Google Scholar]
- Van Strien, T.; Frijters, J.E.; Bergers, G.P.; Defares, P.B. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int. J. Eat. Disord. 1986, 5, 295–315. [Google Scholar] [CrossRef]
- Capra, S. Nutrient Reference Values for Australia and New Zealand: Including Recommended Dietary Intakes; Commonwealth of Australia: Canberra, Australia, 2006. [Google Scholar]
- Huang, T.T.K.; Roberts, S.B.; Howarth, N.C.; McCrory, M.A. Effect of screening out implausible energy intake reports on relationships between diet and BMI. Obes. Res. 2005, 13, 1205–1217. [Google Scholar] [CrossRef]
- Roza, A.M.; Shizgal, H.M. The Harris Benedict equation reevaluated: Resting energy requirements and the body cell mass. Am. J. Clin. Nutr. 1984, 40, 168–182. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, R.A. When to use the B onferroni correction. Ophthalmic Physiol. Opt. 2014, 34, 502–508. [Google Scholar] [CrossRef]
- Ministry of Health, New Zealand. Annual Data Explorer 2021/22: New Zealand Health Survey 2021; Ministry of Health of New Zealand: Auckland, New Zealand, 2022. [Google Scholar]
- Wilson, R.; Abbott, J.H. Age, period and cohort effects on body mass index in New Zealand, 1997–2038. Aust. N. Z. J. Public Health 2018, 42, 396–402. [Google Scholar] [CrossRef]
- Nunnally, J.C. Psychometric theory—25 years ago and now. Educ. Res. 1975, 4, 7–21. [Google Scholar]
- Mack, I.; Teufel, M.; Enck, P. What role does tableware size play in energy consumption of children and adults? Eat. Weight. Disord.-Stud. Anorex. Bulim. Obes. 2019, 24, 595–596. [Google Scholar] [CrossRef] [PubMed]
- Sakurai, S.; Narumi, T.; Ban, Y.; Tanikawa, T.; Hirose, M. Affecting our perception of satiety by changing the size of virtual dishes displayed with a tabletop display. In Proceedings of the International Conference on Virtual, Augmented and Mixed Reality, Las Vegas, NV, USA, 21–26 July 2013; pp. 90–99. [Google Scholar]
- Anderson, C.; Hildreth, J.A.D.; Howland, L. Is the desire for status a fundamental human motive? A review of the empirical literature. Psychol. Bull. 2015, 141, 574. [Google Scholar] [CrossRef] [PubMed]
- Caljouw, S.R.; van Wijck, R. Is the glass half full or half empty? How to reverse the effect of glass elongation on the volume poured. PloS ONE 2014, 9, e109374. [Google Scholar] [CrossRef] [PubMed]
- Krishna, A. Interaction of senses: The effect of vision versus touch on the elongation bias. J. Consum. Res. 2006, 32, 557–566. [Google Scholar] [CrossRef]
- Miller, T.M.; Abdel-Maksoud, M.F.; Crane, L.A.; Marcus, A.C.; Byers, T.E. Effects of social approval bias on self-reported fruit and vegetable consumption: A randomized controlled trial. Nutr. J. 2008, 7, 18. [Google Scholar] [CrossRef]
- Schoeller, D.A. How accurate is self-reported dietary energy intake? Nutr. Rev. 1990, 48, 373–379. [Google Scholar] [CrossRef]

| Participants Recruited into the Study (N = 61) | Participants Included in the Main Analyses (N = 40) | |
|---|---|---|
| Mean ± Standard Deviation (Range) | Mean ± Standard Deviation (Range) | |
| Age (years) | 28 ± 7 (20–40) | 27 ± 6 (21–39) |
| BMI (kg∙m−2) | 28.3 ± 6.3 (19.7–41.5) | 27.7 ± 5.9 (19.7–41.5) |
DEBQ eating score
| 2.2 ± 0.4 (0.9–3.5) 2.2 ± 0.8 (1.0–4.8) 3.4 ± 0.7 (1.4–4.5) | 2.0 ± 0.6 (1.0–3.3) 2.1 ± 0.8 (1.0–4.7) 3.2 ± 0.6 (1.9–4.3) |
| Self-selected portion size (g) | 259.8 ± 65.3 (159.0–388.0) | 226.0 ± 46.2 (159.0–310.4) |
Baseline SLIM ratings
| −58.3 ± −17.8 (−19.8 to −72.3) −60.5 ± −22.4 (−17.6 to −83.4) −64.5 ± −20.0 (−20.6 to −72.1) | −56.8 ± −19.5 (−23.1 to −70.2) −59.4 ± −21.6 (−19.4 to −83.4) −60.3 ± −17.9 (−25.8 to −65.4) |
Hedonic VAS ratings
| 31.5 ± 22.2 (4.1 to 57.0) 32.4 ± 25.4 (3.8 to 58.8) 31.7 ± 20.8 (4.3 to 58.1) | 30.6 ± 18.5 (5.3 to 52.2) 29.5 ± 21.0 (3.8 to 55.7) 31.2 ± 19.7 (5.1 to 57.0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abeywickrema, S.; Peng, M. The Role of Tableware Size in Healthy Eating—Effects on Downstream Food Intake. Foods 2023, 12, 1230. https://doi.org/10.3390/foods12061230
Abeywickrema S, Peng M. The Role of Tableware Size in Healthy Eating—Effects on Downstream Food Intake. Foods. 2023; 12(6):1230. https://doi.org/10.3390/foods12061230
Chicago/Turabian StyleAbeywickrema, Sashie, and Mei Peng. 2023. "The Role of Tableware Size in Healthy Eating—Effects on Downstream Food Intake" Foods 12, no. 6: 1230. https://doi.org/10.3390/foods12061230
APA StyleAbeywickrema, S., & Peng, M. (2023). The Role of Tableware Size in Healthy Eating—Effects on Downstream Food Intake. Foods, 12(6), 1230. https://doi.org/10.3390/foods12061230







