A Narrative Review on Dietary Strategies to Provide Nitric Oxide as a Non-Drug Cardiovascular Disease Therapy: Beetroot Formulations—A Smart Nutritional Intervention
Abstract
1. Introduction
2. Nitric Oxide
3. Dietary NO3− and Endothelial Dysfunction Therapy
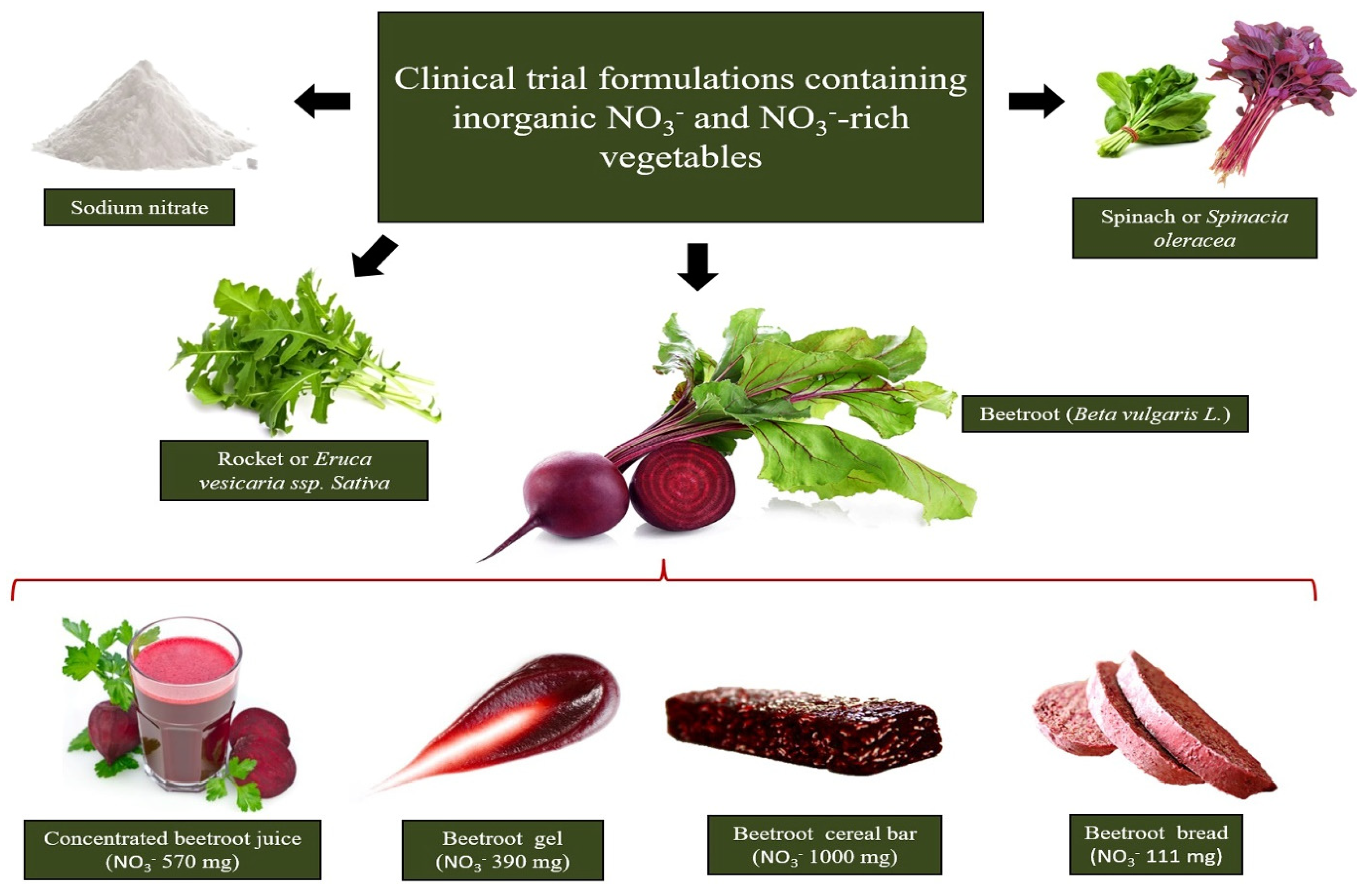
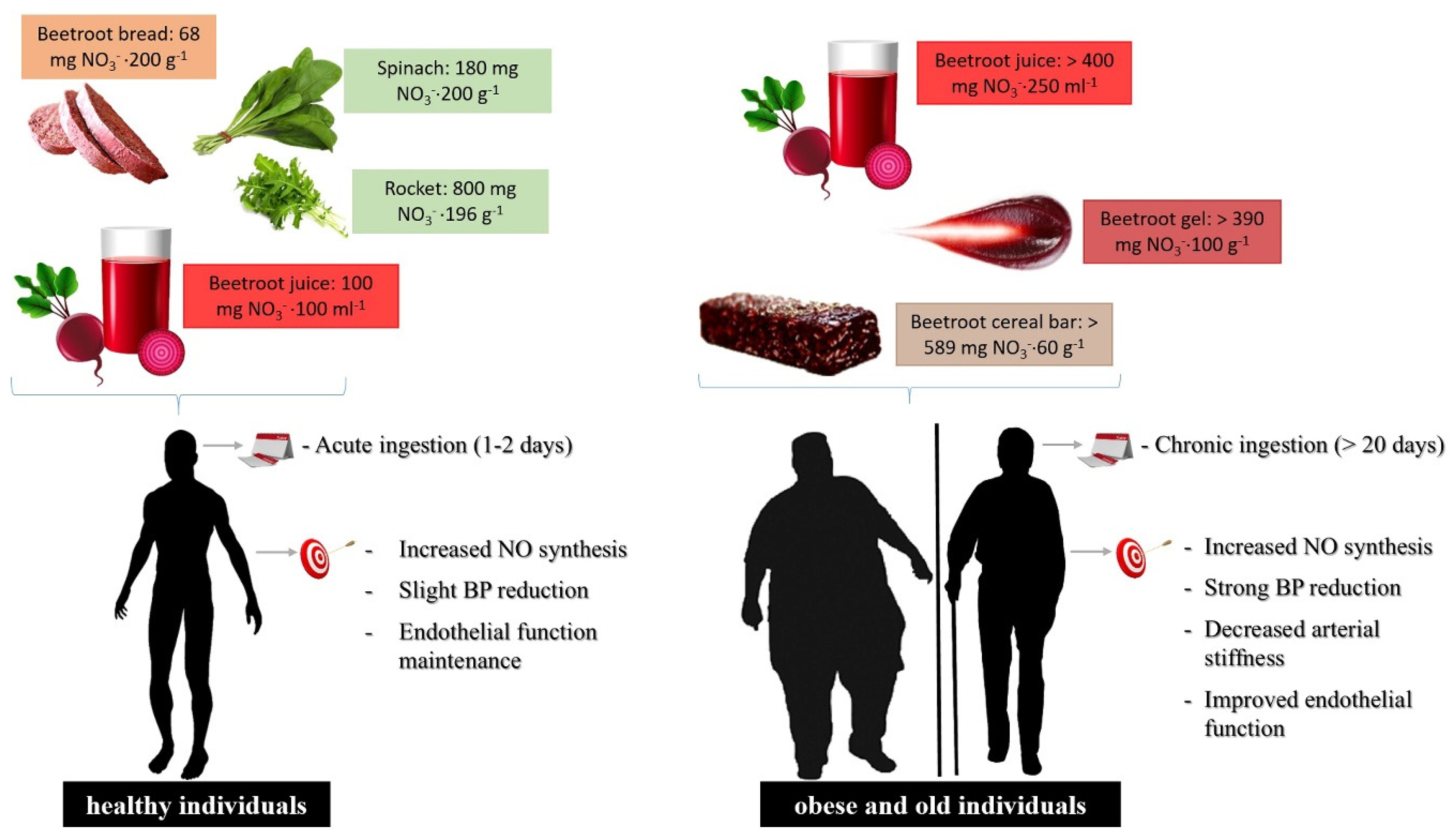
4. Dietary NO3− Vegetable Sources
5. Plasma NO3−/NO2− Increments on Cardiovascular Health and Impaired Cardiovascular Functions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Storch, A.S.; Mattos, J.D.; Alves, R.; Galdino, I.S.; Rocha, H.N.M. Methods of endothelial function assessment: Description and applications. Int. J. Cardiovasc. Sci. 2017, 30, 262–273. [Google Scholar] [CrossRef]
- Lai, W.K.C.; Kan, M.Y. Homocysteine-induced endothelial dysfunction. Ann. Nutr. Metab. 2015, 67, 1–12. [Google Scholar] [CrossRef]
- Krüger-Genge, A.; Blocki, A.; Franke, R.P.; Jung, F. Vascular endothelial cell biology: An update. Int. J. Mol. Sci. 2019, 20, 4411. [Google Scholar] [CrossRef] [PubMed]
- Carrillo, J.A.; Zafrilla, M.P.; Marhuenda, J. Cognitive Function and Consumption of Fruit and Vegetable Polyphenols in a Young Population: Is There a Relationship? Foods 2019, 8, 507. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, A.; Gao, L.; Thakur, A.; Siu, P.M.; Lai, C.W.K. Role of free fatty acids in endothelial dysfunction. J. Biomed. Sci. 2017, 24, 1–15. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Fruit and Vegetables for Health: Report of a Joint FAP/WHO Workshop; World Health Organization: Geneva, Switzerland, 2004; Available online: https://apps.who.int/iris/handle/10665/43143 (accessed on 15 February 2021).
- U.S. Department of Health and Human Services; U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans; U.S. Department of Health and Human Services/U.S. Department of Agriculture: Washington, DC, USA, 2015. Available online: https://health.gov/our-work/food-and-nutrition/2015-2020-dietary-guidelines/ (accessed on 17 February 2021).
- Lidder, S.; Webb, A. Vascular effects of dietary nitrate (as found in green leafy vegetables and beetroot) via the nitrate-nitrite-nitric oxide pathway. Br. J. Clin. Pharmacol. 2013, 75, 677–696. [Google Scholar] [CrossRef] [PubMed]
- Baião, D.S.; da Silva, D.V.T.; Del Aguila, E.M.; Paschoalin, V.M.F. Nutritional, bioactive and physicochemical characteristics of different beetroot formulations. Food Addit. 2017, 20–44. [Google Scholar] [CrossRef]
- Karwowska, M.; Kononiuk, A. Nitrates/nitrites in food—Risk for nitrosative stress and benefits. Antioxidants 2020, 9, 241. [Google Scholar] [CrossRef]
- Hobbs, A.J.; Moncada, S. Antiplatelet properties of a novel, non-NO-based soluble guanylate cyclase activator. Vasc. Pharmacol. 2003, 40, 149–154. [Google Scholar] [CrossRef]
- Stringham, J.M.; Stringham, N.T. Nitric Oxide and Lutein: Function, Performance, and Protection of Neural Tissue. Foods 2015, 4, 678–689. [Google Scholar] [CrossRef]
- Lundberg, J.O.; Gladwin, M.T.; Ahluwalia, A.; Benjamin, N.; Bryan, N.S.; Butler, A.; Cabrales, P.; Fago, A.; Feelisch, M.; Ford, P.C.; et al. Nitrate and nitrite in biology, nutrition and therapeutics. Nat. Chem. Biol. 2009, 5, 865–869. [Google Scholar] [CrossRef]
- Bryan, N.S. Cardioprotective actions of nitrite therapy and dietary considerations. Front. Biosci. 2009, 14, 4793–4808. [Google Scholar] [CrossRef]
- Donato, A.J.; Morgan, R.G.; Walker, A.E.; Lesniewski, L.A. Cellular and molecular biology of aging endothelial cells. J. Mol. Cell. Cardiol. 2015, 89, 122–135. [Google Scholar] [CrossRef] [PubMed]
- Virdis, A. Endothelial dysfunction in obesity: Role of inflammation. High Blood Press. Cardiovasc. Prev. 2016, 23, 83–85. [Google Scholar] [CrossRef] [PubMed]
- Daiber, A.; Steven, S.; Weber, A.; Shuvaev, V.V.; Muzykantov, V.R.; Laher, I.; Li, H.; Lamas, S.; Münzel, T. Targeting vascular (endothelial) dysfunction. Br. J. Pharmacol. 2017, 174, 1591–1619. [Google Scholar] [CrossRef] [PubMed]
- Hasler, C.M. The changing face of functional foods. J. Am. Coll. Nutr. 2000, 19, 499S–506S. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, S. Functional foods against metabolic syndrome (obesity, diabetes, hypertension and dyslipidemia) and cardiovascular disease. Trends Food Sci. Technol. 2014, 35, 114–128. [Google Scholar] [CrossRef]
- Vulić, J.J.; Ćebović, T.N.; Čanadanović-Brunet, J.M.; Ćetković, G.S.; Čanadanović, V.M.; Djilas, S.M.; Šaponjac, V.T.T. In vivo and in vitro antioxidant effects of beetroot pomace extracts. J. Funct. Foods 2014, 6, 168–175. [Google Scholar] [CrossRef]
- Thakur, N.; Raigond, P.; Singh, Y.; Mishra, T.; Singh, B.; Lal, M.K.; Dutt, S. Recent updates on bioaccessibility of phytonutrients. Trends Food Sci. Technol. 2020, 97, 366–380. [Google Scholar] [CrossRef]
- Borgi, L.; Muraki, I.; Satija, A.; Willett, W.C.; Rimm, E.B.; Forman, J.P. Fruit and vegetable consumption and the incidence of hypertension in three prospective cohort studies. Hypertension 2016, 67, 288–293. [Google Scholar] [CrossRef]
- Aune, D.; Giovannucci, E.; Boffetta, P.; Fadnes, L.T.; Keum, N.; Norat, T.; Greenwood, D.C.; Riboli, E.; Vatten, L.J.; Tonstad, S. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality: A systematic review and dose-response meta-analysis of prospective studies. Int. J. Epidemiol. 2017, 46, 1029–1056. [Google Scholar] [CrossRef] [PubMed]
- Van Breda, S.G.J.; de Kok, T.M.C.M. Smart combinations of bioactive compounds in fruits and vegetables may guide new strategies for personalized prevention of chronic diseases. Mol. Nutr. Food Res. 2018, 62, 1700597. [Google Scholar] [CrossRef] [PubMed]
- Sawicki, T.; Martinez-Villaluenga, C.; Frias, J.; Wiczkowski, W.; Peñas, E.; Bączek, N.; Zieliński, H. The effect of processing and in vitro digestion on the betalain profile and ACE inhibition activity of red beetroot products. J. Funct. Foods 2019, 55, 229–237. [Google Scholar] [CrossRef]
- Mirvish, S.S. Role of N-nitroso compounds (NOC) and N-nitrosation in etiology of gastric, esophageal, nasopharyngeal and bladder cancer and contribution to cancer of known exposures to NOC. Cancer Lett. 1995, 93, 17–48. [Google Scholar] [CrossRef]
- Katan, M.B. Nitrate in foods: Harmful or healthy? Am. J. Clin. Nutr. 2009, 90, 11–12. [Google Scholar] [CrossRef] [PubMed]
- Blekkenhorst, L.C.; Bondonno, N.P.; Liu, A.H.; Ward, N.C.; Prince, R.L.; Lewis, J.R.; Devine, A.; Croft, K.D.; Hodgson, J.M.; Bondonno, C.P. Nitrate, the oral microbiome, and cardiovascular health: A systematic literature review of human and animal studies. Am. J. Clin. Nutr. 2018, 107, 504–522. [Google Scholar] [CrossRef]
- Alidadi, M.; Jamialahmadi, T.; Cicero, A.F.G.; Bianconi, V.; Pirro, M.; Banach, M.; Sahebkar, A. The potential role of plant-derived natural products in improving arterial stiffness: A review of dietary intervention studies. Trends Food Sci. Technol. 2020, 99, 426–440. [Google Scholar] [CrossRef]
- Baião, D.S.; da Silva, D.V.T.; Paschoalin, V.M.F. Beetroot, a remarkable vegetable: Its nitrate and phytochemical contents can be adjusted in novel formulations to benefit health and support cardiovascular disease therapies. Antioxidants 2020, 9, 960. [Google Scholar] [CrossRef]
- Anjana, S.U.; Muhammad, I.; Abrol, Y.P. Are nitrate concentrations in leafy vegetables within safe limits? Curr. Sci. 2007, 92, 355–360. Available online: http://www.jstor.org/stable/24096732 (accessed on 5 March 2021).
- Blekkenhorst, L.C.; Sim, M.; Bondonno, C.P.; Bondonno, N.P.; Ward, N.C.; Prince, R.L.; Devine, A.; Lewis, J.R.; Hodgson, J.M. Cardiovascular health benefits of specific vegetable types: A narrative review. Nutrients 2018, 10, 595. [Google Scholar] [CrossRef]
- Hord, N.G.; Tang, Y.; Bryan, N.S. Food sources of nitrates and nitrites: The physiologic context for potential health benefits. Am. J. Clin. Nutr. 2009, 90, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Santamaria, P.; Elia, A.; Serio, F.; Todaro, E. A survey of nitrate and oxalate content in fresh vegetables. J. Sci. Food Agric. 1999, 79, 1882–1888. [Google Scholar] [CrossRef]
- European Food Safety Authority (EFSA). Opinion of the scientific panel on contaminants in the food chain on a request from the European Commission to perform a scientific risk assessment on nitrate in vegetables. EFSA J. 2008, 689, 1–79. [Google Scholar] [CrossRef]
- Tamme, T.; Reinik, M.; Roasto, M.; Meremäe, K.; Kiss, A. Nitrate in leafy vegetables, culinary herbs, and cucumber grown under cover in Estonia: Content and intake. Food Addit. Contam. Part B 2010, 3, 108–113. [Google Scholar] [CrossRef] [PubMed]
- van Velzen, A.G.; Sips, A.J.; Schothorst, R.C.; Lambers, A.C.; Meulenbelt, J. The oral bioavailability of nitrate from nitrate-rich vegetables in humans. Toxicol. Lett. 2008, 181, 177–181. [Google Scholar] [CrossRef] [PubMed]
- Hobbs, D.A.; Kaffa, N.; George, T.W.; Methven, L.; Lovegrove, J.A. Blood pressure-lowering effects of beetroot juice and novel beetroot-enriched bread products in normotensive male subjects. Br. J. Nutr. 2012, 108, 2066–2074. [Google Scholar] [CrossRef] [PubMed]
- Hobbs, D.A.; Goulding, M.G.; Nguyen, A.; Malaver, T.; Walker, C.F.; George, T.W.; Methven, L.; Lovegrove, J.A. Acute ingestion of beetroot bread increases Endothelium-Independent vasodilation and lowers diastolic blood pressure in healthy men: A randomized controlled trial. J. Nutr. 2013, 143, 1399–1405. [Google Scholar] [CrossRef] [PubMed]
- Jajja, A.; Sutyarjoko, A.; Lara, J.; Rennie, K.; Brandt, K.; Qadir, O.; Siervo, M. Beetroot supplementation lowers daily systolic blood pressure in older, overweight subjects. Nutr. Res. 2014, 34, 868–875. [Google Scholar] [CrossRef] [PubMed]
- Kapil, V.; Khambata, R.S.; Robertson, A.; Caulfield, M.J.; Ahluwalia, A. Dietary nitrate provides sustained blood pressure lowering in hypertensive patients: A randomized, phase 2, double-blind, placebo-controlled study. Hypertension 2015, 65, 320–327. [Google Scholar] [CrossRef]
- Baião, D.S.; Conte-Junior, C.A.; Paschoalin, V.M.F.; Alvares, T.S. Beetroot juice increase nitric oxide metabolites in both men and women regardless of body mass. Int. J. Food Sci. Nutr. 2016, 67, 40–46. [Google Scholar] [CrossRef]
- Bezerra, A.D.L.; Costa, E.C.; Pacheco, D.A.; Souza, D.C.; Farias-Junior, L.F.; Ritti-Dia, R.M.; Grigolo, G.B.; Júnior, P.I.H.B.; Krause, M.; Fayh, A.P.T. Effect of acute dietary nitrate supplementation on the post-exercise ambulatory blood pressure in obese males: A randomized, controlled, crossover trial. J. Sports Sci. Med. 2019, 18, 118–127. [Google Scholar]
- Silva, D.V.T.; Silva, F.O.; Perrone, D.; Pierucci, A.P.T.R.; Conte-Junior, C.A.; Alvares, T.S.; Del Aguila, E.M.; Paschoalin, V.M.F. Physicochemical, nutritional, and sensory analyses of a nitrate-enriched beetroot gel and its effects on plasmatic nitric oxide and blood pressure. Food Nutr. Res. 2016, 60, 29909. [Google Scholar] [CrossRef]
- Baião, D.S.; d’El-Rei, J.; Alves, G.; Neves, M.F.; Perrone, D.; Del Aguila, E.D.; Paschoalin, V.M.F. Chronic effects of nitrate supplementation with a newly designed beetroot formulation on biochemical and hemodynamic parameters of individuals presenting risk factors for cardiovascular diseases: A pilot study. J. Funct. Foods 2019, 58, 85–94. [Google Scholar] [CrossRef]
- Liu, A.H.; Bondonno, C.P.; Croft, K.D.; Puddey, I.B.; Woodman, R.J.; Rich, L.; Ward, N.C.; Vita, J.A.; Hodgson, J.M. Effects of a nitrate-rich meal on arterial stiffness and blood pressure in healthy volunteers. Nitric Oxide 2013, 35, 123–130. [Google Scholar] [CrossRef]
- Bondonno, C.P.; Yang, X.; Croft, K.D.; Considine, M.J.; Ward, N.C.; Rich, L.; Puddey, I.B.; Swinny, E.; Mubarak, A.; Hodgson, J.M. Flavonoid-rich apples and nitrate-rich spinach augment nitric oxide status and improve endothelial function in healthy men and women: A randomized controlled trial. Free Radic. Biol. Med. 2012, 52, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Jonvik, K.L.; Nyakayiru, J.; Pinckaers, P.J.; Senden, J.M.; van Loon, L.J.; Verdijk, L.B. Nitrate-rich vegetables increase plasma nitrate and nitrite concentrations and lower blood pressure in healthy adults. J. Nutr. 2016, 146, 986–993. [Google Scholar] [CrossRef]
- Haun, C.T.; Kephart, W.C.; Holland, A.M.; Mobley, C.B.; McCloskey, A.E.; Shake, J.J.; Pascoe, D.D.; Roberts, M.D.; Martin, J.S. Differential vascular reactivity responses acutely following ingestion of a nitrate rich red spinach extract. Eur. J. Appl. Physiol. 2016, 116, 2267–2279. [Google Scholar] [CrossRef]
- Ashor, A.W.; Jajja, A.; Sutyarjoko, A.; Brandt, K.; Qadir, O.; Lara, J.; Siervo, M. Effects of beetroot juice supplementation on microvascular blood flow in older overweight and obese subjects: A pilot randomised controlled study. J. Hum. Hypertens. 2015, 29, 511–513. [Google Scholar] [CrossRef]
- Baião, D.S.; Silva, F.O.; d’El-Rei, J.; Neves, M.F.; Perrone, D.; Del Aguila, E.M.; Paschoalin, V.M.F. A new functional beetroot formulation enhances adherence to nitrate supplementation and health outcomes in clinical practice. SDRP J. Food Sci. Technol. 2018, 3, 484–496. [Google Scholar] [CrossRef]
- Webb, A.J.; Patel, N.; Loukogeorgakis, S.; Okorie, M.; Aboud, Z.; Misra, S.; Rashid, R.; Miall, P.; Deanfield, J.; Benjamin, N.; et al. Acute blood pressure lowering, vasoprotective, and antiplatelet properties of dietary nitrate via bioconversion to nitrite. Hypertension 2008, 51, 784–790. [Google Scholar] [CrossRef]
- Ormesher, L.; Myers, J.E.; Chmiel, C.; Wareing, M.; Greenwood, S.L.; Tropea, T.; Lundberg, J.O.; Weitzberg, E.; Nihlen, C.; Sibley, C.P.; et al. Effects of dietary nitrate supplementation, from beetroot juice, on blood pressure in hypertensive pregnant women: A randomized, double-blind, placebo-controlled feasibility trial. Nitric Oxide 2018, 80, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Bondonno, C.P.; Liu, A.H.; Croft, K.D.; Ward, N.C.; Shinde, S.; Moodley, Y.; Lundberg, J.O.; Puddey, I.B.; Woodman, R.J.; Hodgson, J.M. Absence of an effect of high nitrate intake from beetroot juice on blood pressure in treated hypertensive individuals: A randomized controlled trial. Am. J. Clin. Nutr. 2015, 102, 368–375. [Google Scholar] [CrossRef]
- Lara, J.; Ashor, A.W.; Oggioni, C.; Ahluwalia, A.; Mathers, J.C.; Siervo, M. Effects of inorganic nitrate and beetroot supplementation on endothelial function: A systematic review and meta-analysis. Eur. J. Nutr. 2016, 55, 451–459. [Google Scholar] [CrossRef] [PubMed]
- Ambriz-Pérez, D.L.; Leyva-López, N.; Gutierrez-Grijalva, E.P.; Heredia, J.B. Phenolic compounds: Natural alternative in inflammation treatment. A Review. Cogent. Food Agric. 2016, 2, 1–14. [Google Scholar] [CrossRef]
- Appeldoorn, M.M.; Venema, D.P.; Peters, T.H.F.; Koenen, M.E.; Arts, I.C.W.; Vincken, J.P.; Gruppen, H.; Keijer, J.; Hollman, P.C.H. Some Phenolic Compounds Increase the Nitric Oxide Level in Endothelial Cells in Vitro. J. Agric. Food Chem. 2009, 57, 7693–7699. [Google Scholar] [CrossRef]
| Vegetable | NO3− Content/mg·kg−1 | |
|---|---|---|
| High NO3− content (>1000 mg·kg−1) | Rocket or arugula (Eruca vesicaria subsp. sativa) | 2848 [2597–3100] |
| Green spinach (Spinacia oleracea) | 2500 [2013–2797] | |
| Coriander (Coriandrum sativum) | 2445 | |
| Basil (Ocimum basilicum) | 2292 [507–4695] | |
| Celery (Apium graveolens) | 2200 [900–3500] | |
| Parsley (Petroselinum crispum) | 2134 [1700–2101] | |
| Radish (Raphanus raphanistrum subsp. sativus) | 2064 [1878–2250] | |
| Butter leaf lettuce (Lactuca sativa variety capitata) | 2000 | |
| Bok choy (Brassica rapa subsp. chinensis) | 1933 | |
| Lettuce (Lactuca sativa) | 1893 [970–2782] | |
| Beet greens (Beta vulgaris subsp. vulgaris) | 1852 [1060–2600] | |
| Kohlrabi (Brassica oleracea) | 1769 | |
| Swiss chard (Beta vulgaris subsp. maritima) | 1512 [1024–2000] | |
| Leaf chicory (Cichorium intybus) | 1452 | |
| Beetroot (Beta vulgaris subsp. vulgaris) | 1300 [644–1950] | |
| Black radish (Raphanus raphanistrum subsp. sativus) | 1271 [667–1878] | |
| Mustard greens (Brassica juncea) | 1160 | |
| Medium NO3− content (100 to 1000 mg·kg−1) | Curly kale (Brassica oleracea Acephala Group) | 987 [792–1181] |
| Broccoli raab (Brassica rapa) | 905 | |
| Pumpkin (Cucurbita pepo) | 692 [445–939] | |
| Turnip (Brassica rapa subsp. rapa) | 684 [307–1062] | |
| Endive (Cichorium endivia) | 663 | |
| Cabbage (Brassica oleracea var. capitata) | 503 [85–920] | |
| Green beans (Phaseolus vulgaris) | 496 [449–585] | |
| Green onion (Allium fistulosum) | 485 [99–870] | |
| Courgette (Cucurbita pepo) | 416 | |
| Fennel (Foeniculum vulgare) | 363 | |
| Asparagus (Asparagus officinalis) | 355 [145–479] | |
| Cauliflower (Brassica oleracea var. botrytis) | 331 [104–559] | |
| Savoy cabbage (Brassica oleracea Savoy Cabbage Group) | 324 | |
| Aubergine (Solanum melongena) | 314 | |
| Broccoli (Brassica oleracea var. italica) | 300 [145–477] | |
| Carrot (Daucus carota subsp. sativus) | 300 [121–480] | |
| Cucumber (Cucumis sativus) | 240 [124–384] | |
| Potato (Solanum tuberosum) | 220 [81–713] | |
| Garlic (Allium sativum) | 183 [34–455] | |
| Artichokes (Cynara scolymus) | 174 | |
| Sweet pepper (Capsicum annuum) | 117 [93–140] | |
| Green pepper (Capsicum annuum) | 111 [76–159] | |
| Low NO3− content (<100 mg·kg−1) | Onion (Allium cepa) | 87 [23–235] |
| Tomato (Solanum lycopersicum) | 69 [27–170] |
| NO3− Vegetable Intervention | NO3− Content/Serving Portion Administered | Subjects | Duration of Administration | Trial Features | Effects | Study |
|---|---|---|---|---|---|---|
| White beetroot bread (Beta vulgaris L) Red beetroot bread (Beta vulgaris L) | 99 mg·200 g−1 112 mg·200 g−1 | 14 healthy individuals | single intake | Randomized Placebo-controlled Single-blind Crossover | ↑ NO synthesis after 1 h of ingestion (through urinary NOx) ↓ 24 h ambulatory SBP and DBP | Hobbs et al. [38] |
| Beetroot bread (Beta vulgaris L) | 68 mg·200 g−1 | 23 healthy individuals | single intake | Randomized Placebo-controlled Open-label Crossover | ↑ NO synthesis after 1 h of ingestion (through plasma and urinary NO3− and NO2−) ↓ iAUC (0–6 h after beet bread ingestion) for DBP ↑ iAUC (0–6 h after beet bread ingestion) for endothelium-independent microvascular vasodilation | Hobbs et al. [39] |
| Beetroot juice (Beta vulgaris L) | 403 mg·70 mL−1 | 24 overweight older individuals | 3 weeks | Randomized Placebo-controlled | ↓ daily resting DBP at home | Jajja et al. [40] |
| 400 mg·250 mL−1 | 68 hypertensive individuals | 4 weeks | Randomized Placebo-controlled Double-blind Crossover | ↑ NO synthesis (by plasma and salivary NO3−, NO2− and plasma cGMP) ↓ home, clinic and 24 h ambulatorial SBP and DBP, and arterial stiffness (through reduction of PWV and AIx) ↑ endothelial function (through increased brachial artery diameter and time to peak dilatation after FMD) | Kapil et al. [41] | |
| 100 mg·100 mL−1 | 40 healthy individuals | single intake | Randomized Placebo-controlled Double-blind Crossover | ↑ NO synthesis (by urinary NO3− and NO2−) No significant relationships between urinary NO3− and NO2− concentration and body mass after intervention were observed | Baião et al. [42] | |
| 800 mg·200 mL−1 | 14 non-hypertensive obese individuals | single intake | Randomized Placebo-controlled Crossover | ↑ NO synthesis (through plasma NOx) ↓ ambulatory SBP following 1–6 h of moderate-intensity aerobic exercise | Bezerra et al. [43] | |
| Beetroot gel (Beta vulgaris L) | 390 mg·100 g−1 | 5 healthy individuals | single intake | - | ↑ NO synthesis (through plasma NO2−) ↓ ambulatory SBP, DBP and HR | Silva et al. [44] |
| Beetroot cereal bar (Beta vulgaris L) | 589 mg·60 g−1 | women with 2 risk factors for CVD | 3 weeks | Randomized Placebo-controlled Double-blind Crossover | ↑ NO synthesis (through plasma NO3− and NO2−) ↓ clinical DBP and SBP ↓ arterial stiffness (through reductions in AP, AIx, aoSP, aoPP, arterial age and PWV) ↑ endothelial function (through increased CVC peaks and AUC) | Baião et al. [45] |
| Spinach (Spinacia oleracea) | 220 mg·250 g−1 | 26 healthy individuals | single intake | Randomized Placebo-controlled Crossover | ↑ NO synthesis (through salivary NO3− and NO2−) ↑ large artery elasticity index ↓ pulse pressure, SBP, estimated cardiac ejection time, estimated cardiac output, estimated stroke volume and total vascular impedance | Liu et al. [46] |
| 182 mg·200 g−1 | 30 healthy individuals | single intake | Randomized Placebo-controlled Crossover | ↑ NO synthesis (through plasma RXNO, NO2− and NOx) ↑ ↑ endothelial function (through increases brachial artery diameter dilatation after FMD) ↓ ambulatory SBP and pulse pressure | Bondonno et al. [47] | |
| 800 mg·365 g−1 | 18 healthy individuals | single intake | Semi randomized Crossover | ↑ NO synthesis (through plasma NO3− and NO2−) ↓ ambulatory DBP and SBP | Jonvik et al. [48] | |
| Red spinach (Amaranthus dubius) | 1000 mg·90 mg−1 | 15 healthy individuals | single intake | Placebo-controlled Double-blind Crossover | ↑ NO synthesis (through plasma NO2− and NOx) ↑ endothelial function (through increased reactive hyperemia and calf blood flow) | Haun et al. [49] |
| Rocket (Euruca vesicaria ssp. Sativa) | 800 mg·196 g−1 | 18 healthy individuals | single intake | Semi randomized Crossover | ↑ NO synthesis (through plasma NO3− and NO2−) ↓ DBP and SBP | Jonvik et al. [48] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
dos Santos Baião, D.; Vieira Teixeira da Silva, D.; Margaret Flosi Paschoalin, V. A Narrative Review on Dietary Strategies to Provide Nitric Oxide as a Non-Drug Cardiovascular Disease Therapy: Beetroot Formulations—A Smart Nutritional Intervention. Foods 2021, 10, 859. https://doi.org/10.3390/foods10040859
dos Santos Baião D, Vieira Teixeira da Silva D, Margaret Flosi Paschoalin V. A Narrative Review on Dietary Strategies to Provide Nitric Oxide as a Non-Drug Cardiovascular Disease Therapy: Beetroot Formulations—A Smart Nutritional Intervention. Foods. 2021; 10(4):859. https://doi.org/10.3390/foods10040859
Chicago/Turabian Styledos Santos Baião, Diego, Davi Vieira Teixeira da Silva, and Vania Margaret Flosi Paschoalin. 2021. "A Narrative Review on Dietary Strategies to Provide Nitric Oxide as a Non-Drug Cardiovascular Disease Therapy: Beetroot Formulations—A Smart Nutritional Intervention" Foods 10, no. 4: 859. https://doi.org/10.3390/foods10040859
APA Styledos Santos Baião, D., Vieira Teixeira da Silva, D., & Margaret Flosi Paschoalin, V. (2021). A Narrative Review on Dietary Strategies to Provide Nitric Oxide as a Non-Drug Cardiovascular Disease Therapy: Beetroot Formulations—A Smart Nutritional Intervention. Foods, 10(4), 859. https://doi.org/10.3390/foods10040859








