36 Months’ Clinical Performance of Primary Incisors Restorations Depending on the Type of Restorative Technique Used: A Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
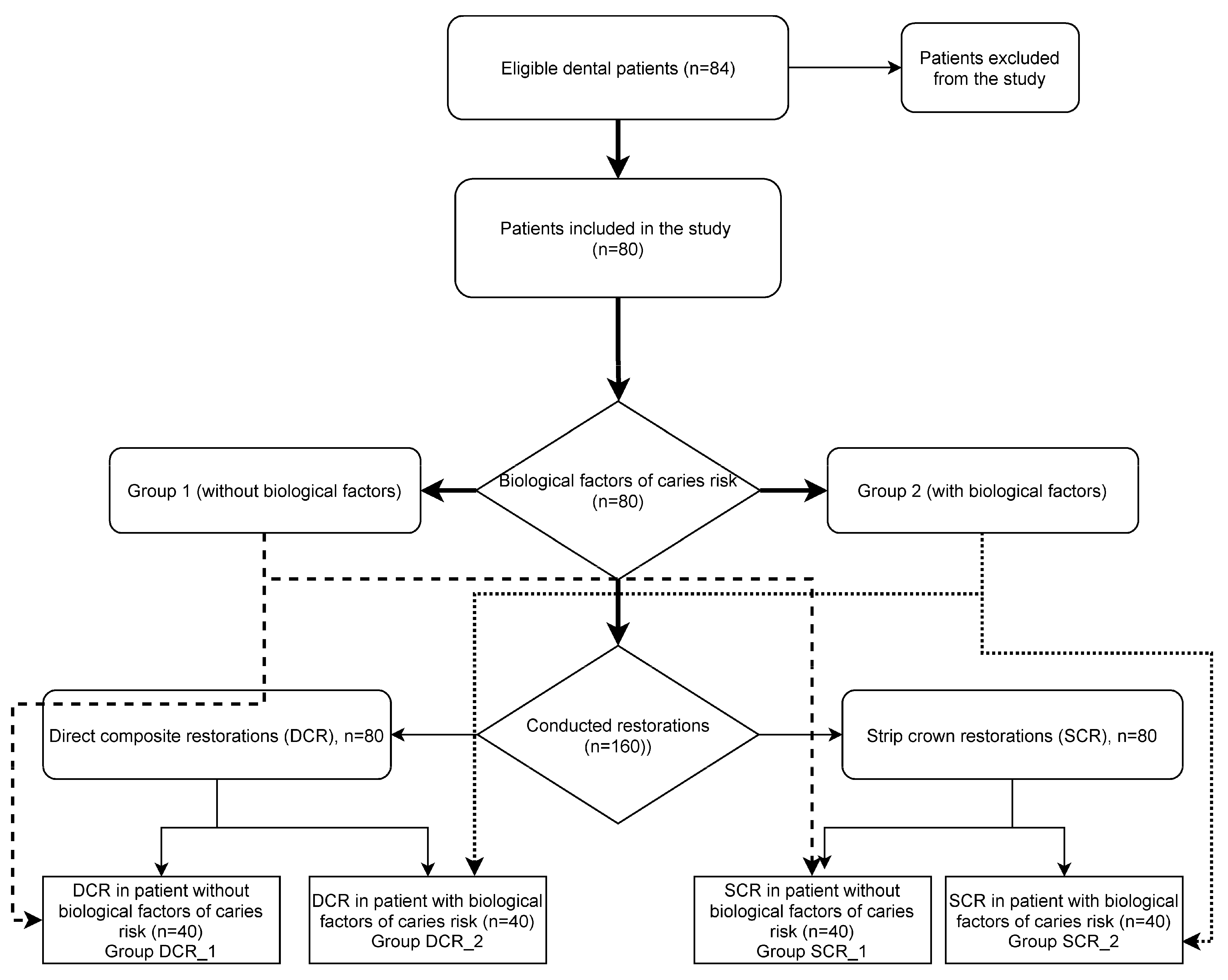
2.1. Study Design
2.2. Inclusion and Exclusion Criteria
2.3. Study Population
2.4. Study Interventions
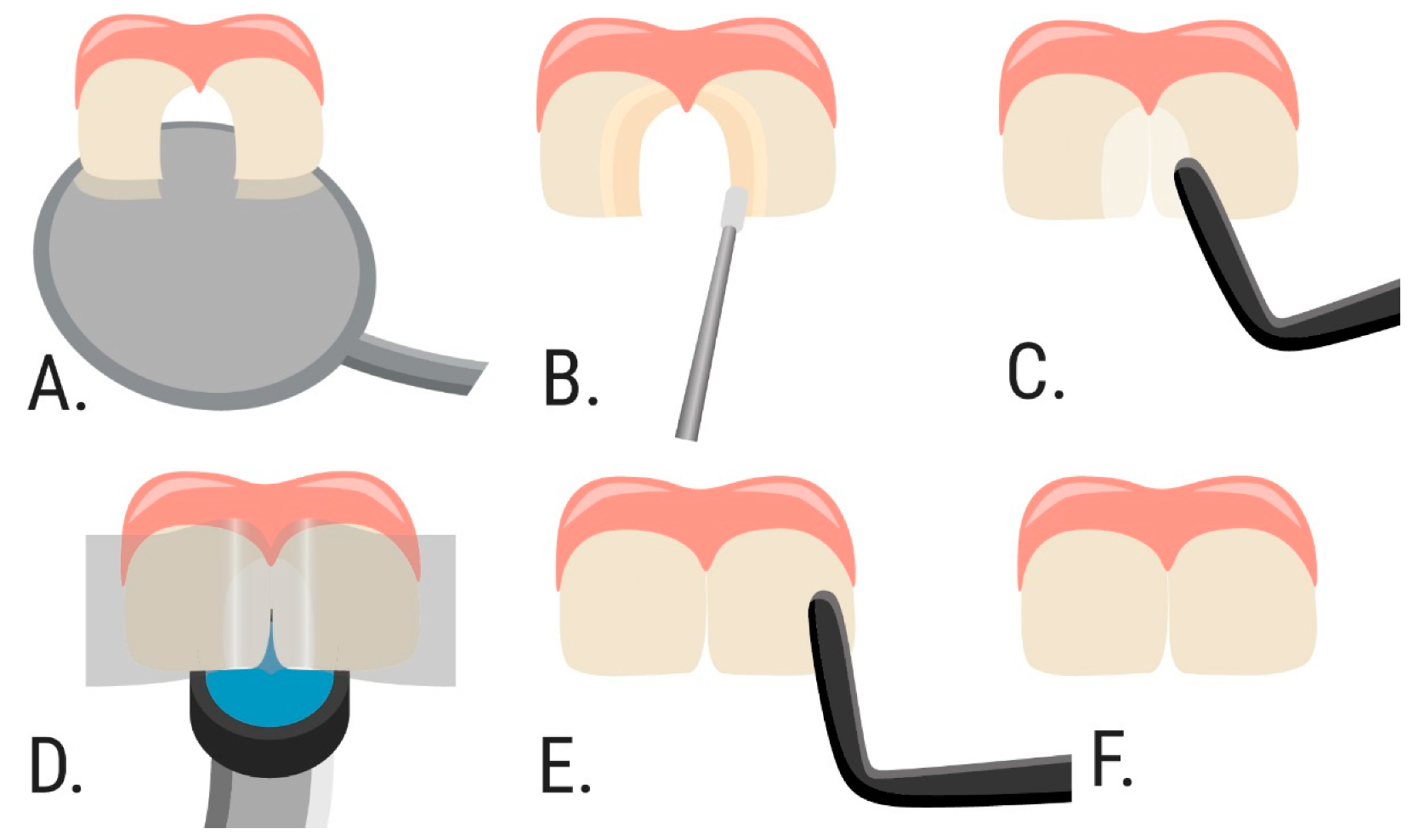
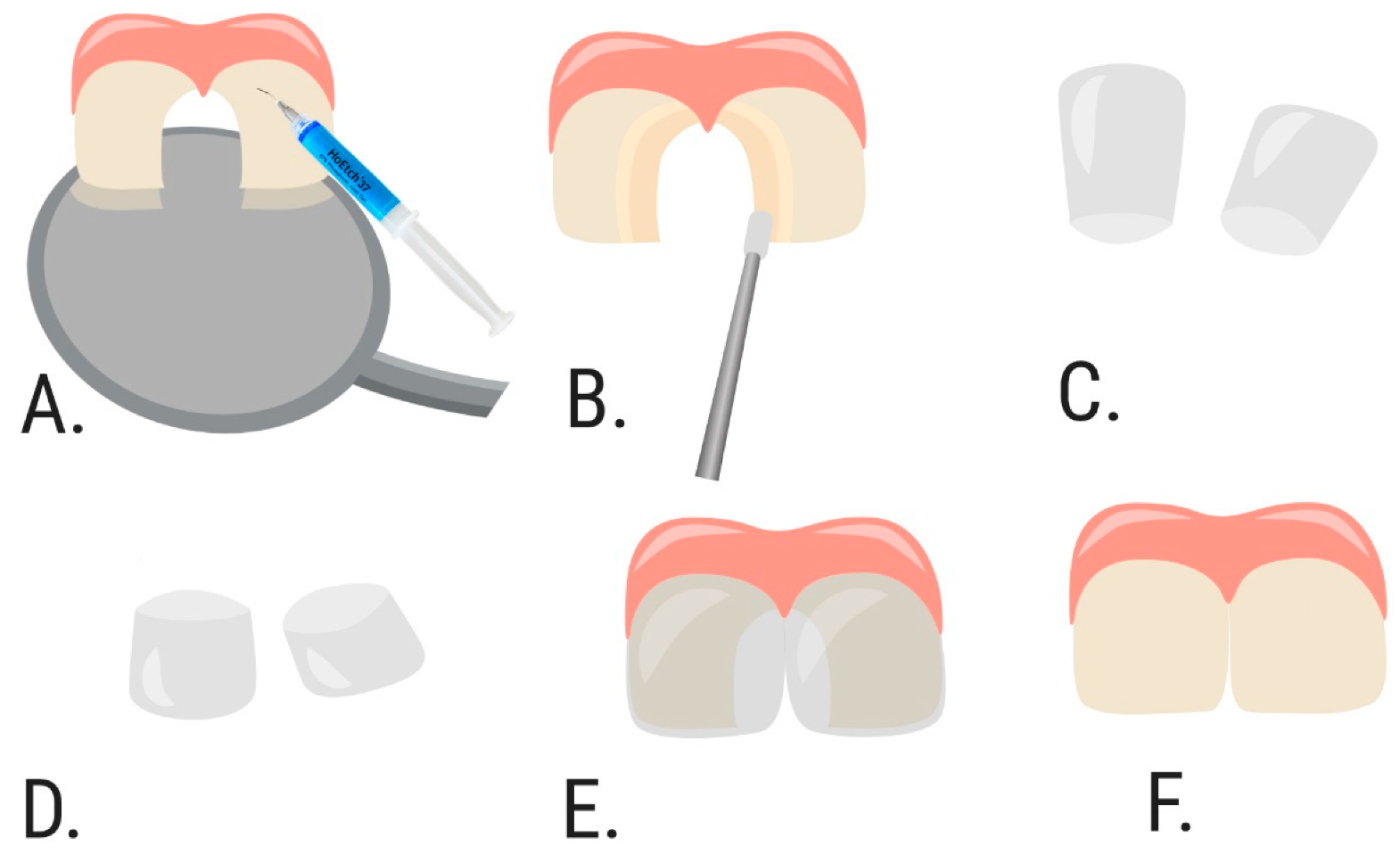
2.5. Treatment Strategy
2.6. Evaluation of the Restorations
2.7. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chen, K.J.; Gao, S.S.; Duangthip, D.; Lo, E.C.M.; Chu, C.H. Prevalence of Early Childhood Caries among 5-Year-Old Children: A Systematic Review. J. Investig. Clin. Dent. 2019, 10, e12376. [Google Scholar] [CrossRef] [Green Version]
- El Tantawi, M.; Folayan, M.O.; Mehaina, M.; Vukovic, A.; Castillo, J.L.; Gaffar, B.O.; Arheiam, A.; Al-Batayneh, O.B.; Kemoli, A.M.; Schroth, R.J.; et al. Prevalence and Data Availability of Early Childhood Caries in 193 United Nations Countries, 2007–2017. Am. J. Public Health 2018, 108, 1066–1072. [Google Scholar] [CrossRef]
- Meyer, F.; Enax, J. Early Childhood Caries: Epidemiology, Aetiology, and Prevention. Int. J. Dent. 2018, 2018, 1415873. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tinanoff, N.; Baez, R.J.; Diaz Guillory, C.; Donly, K.J.; Feldens, C.A.; McGrath, C.; Phantumvanit, P.; Pitts, N.B.; Seow, W.K.; Sharkov, N.; et al. Early Childhood Caries Epidemiology, Aetiology, Risk Assessment, Societal Burden, Management, Education, and Policy: Global Perspective. Int. J. Paediatr. Dent. 2019, 29, 238–248. [Google Scholar] [CrossRef] [PubMed]
- Gavic, L.; Tadin, A.; Mihanovic, I.; Gorseta, K.; Cigic, L. The Role of Parental Anxiety, Depression, and Psychological Stress Level on the Development of Early-Childhood Caries in Children. Int. J. Paediatr. Dent. 2018, 28, 616–623. [Google Scholar] [CrossRef] [PubMed]
- Kazeminia, M.; Abdi, A.; Shohaimi, S.; Jalali, R.; Vaisi-Raygani, A.; Salari, N.; Mohammadi, M. Dental Caries in Primary and Permanent Teeth in Children’s Worldwide, 1995 to 2019: A Systematic Review and Meta-Analysis. Head Face Med. 2020, 16, 22. [Google Scholar] [CrossRef]
- Nobile, C.G.A.; Fortunato, L.; Bianco, A.; Pileggi, C.; Pavia, M. Pattern and Severity of Early Childhood Caries in Southern Italy: A Preschool-Based Cross-Sectional Study. BMC Public Health 2014, 14, 206. [Google Scholar] [CrossRef] [Green Version]
- Bencze, Z.; Mahrouseh, N.; Andrade, C.A.S.; Kovács, N.; Varga, O. The Burden of Early Childhood Caries in Children under 5 Years Old in the European Union and Associated Risk Factors: An Ecological Study. Nutrients 2021, 13, 455. [Google Scholar] [CrossRef]
- Ganesh, A.; Muthu, M.S.; Mohan, A.; Kirubakaran, R. Prevalence of Early Childhood Caries in India-A Systematic Review. Indian J. Pediatr. 2019, 86, 276–286. [Google Scholar] [CrossRef]
- Gorbatova, M.A.; Gorbatova, L.N.; Pastbin, M.U.; Grjibovski, A.M. Urban-Rural Differences in Dental Caries Experience among 6-Year-Old Children in the Russian North. Rural Remote Health 2012, 12, 1999. [Google Scholar]
- Meyer, F.; Karch, A.; Schlinkmann, K.M.; Dreesman, J.; Horn, J.; Rübsamen, N.; Sudradjat, H.; Schubert, R.; Mikolajczyk, R. Sociodemographic Determinants of Spatial Disparities in Early Childhood Caries: An Ecological Analysis in Braunschweig, Germany. Community Dent. Oral Epidemiol. 2017, 45, 442–448. [Google Scholar] [CrossRef]
- Youssefi, M.A.; Afroughi, S. Prevalence and Associated Factors of Dental Caries in Primary Schoolchildren: An Iranian Setting. Int. J. Dent. 2020, 2020, 8731486. [Google Scholar] [CrossRef]
- Eid, S.A.; Khattab, N.M.A.; Elheeny, A.A.H. Untreated Dental Caries Prevalence and Impact on the Quality of Life among 11 To14-Year-Old Egyptian Schoolchildren: A Cross-Sectional Study. BMC Oral Health 2020, 20, 83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuzmina, I.; Smirnova, T.; Lyssenkova, I. Caries Prevalence among children in Russia. In Proceedings of the International Association for Dental Research/American Association for Dental Research/Canadian Association for Dental Research 87th General Session, Miami, FL, USA, 1–4 April 2009; Available online: https://iadr.abstractarchives.com/abstract/2009miami-116642/caries-prevalence-among-children-in-russia (accessed on 6 August 2021).
- Koposova, N.; Eriksen, H.M.; Widström, E.; Handegård, B.H.; Pastbin, M.; Koposov, R. Caries Prevalence and Determinants among 12-Year-Olds in North-West Russia and Northern Norway. Stomatologija 2013, 15, 3–11. [Google Scholar] [PubMed]
- Santamaria, R.M.; Schmoeckel, J.; Basner, R.; Schüler, E.; Splieth, C.H. Caries Trends in the Primary Dentition of 6-to 7-Year-Old Schoolchildren in Germany from 1994 to 2016: Results from the German National Oral Health Surveys in Children. CRE 2019, 53, 659–666. [Google Scholar] [CrossRef]
- Mourad, M.S.; Vielhauer, A.; Splieth, C.H. Kinderzahnheilkunde: 7 Mythen von der Zahnfee. Mon. Kinderheilkd. 2018, 166, 1094–1099. [Google Scholar] [CrossRef]
- American Academy of Pediatric Dentistry. Caries-Risk Assessment and Management for Infants, Children, and Adolescents. The Reference Manual of Pediatric Dentistry. Chicago, Ill.: American Academy of Pediatric Dentistry; 2020:243-7. Available online: https://www.aapd.org/globalassets/media/policies_guidelines/bp_cariesriskassessment.pdf?v=new (accessed on 6 August 2021).
- Campagna, P.; Pinto, L.T.; Lenzi, T.L.; Ardenghi, T.M.; de Oliveira Rocha, R.; Oliveira, M.D.M. Survival and Associated Risk Factors of Composite Restorations in Children with Early Childhood Caries: A Clinical Retrospective Study. Pediatr. Dent. 2018, 40, 210–214. [Google Scholar]
- Mendes da Silva, C.; Figueiredo, M.C.; Casagrande, L.; Larissa Lenzi, T. Survival and Associated Risk Factors of Atraumatic Restorative Treatment Restorations in Children with Early Childhood Caries. J. Dent. Child. (Chic) 2020, 87, 12–17. [Google Scholar]
- Waggoner, W.F. Restoring Primary Anterior Teeth: Updated for 2014. Pediatr. Dent. 2015, 37, 163–170. [Google Scholar] [PubMed]
- Waggoner, W.F.; Nelson, T. Restorative Dentistry for the Primary Dentition. In Pediatric Dentistry, 6th ed.; Nowak, A.J., Christensen, J.R., Mabry, T.R., Townsend, J.A., Wells, M.H., Eds.; Elsevier: Philadelphia, PA, USA, 2019. [Google Scholar]
- Schmoeckel, J.; Gorseta, K.; Splieth, C.H.; Juric, H. How to Intervene in the Caries Process: Early Childhood Caries-A Systematic Review. Caries Res. 2020, 54, 102–112. [Google Scholar] [CrossRef]
- Afrashtehfar, K.I.; Assery, M.K. Five Considerations in Cosmetic and Esthetic Dentistry. J. N. J. Dent. Assoc. 2014, 85, 14–15. [Google Scholar] [PubMed]
- Ashima, G.; Sarabjot, K.B.; Gauba, K.; Mittal, H.C. Zirconia Crowns for Rehabilitation of Decayed Primary Incisors: An Esthetic Alternative. J. Clin. Pediatr. Dent. 2014, 39, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Clark, L.; Wells, M.H.; Harris, E.F.; Lou, J. Comparison of Amount of Primary Tooth Reduction Required for Anterior and Posterior Zirconia and Stainless Steel Crowns. Pediatr. Dent. 2016, 38, 42–46. [Google Scholar] [PubMed]
- Sohrabi, M.; Ghadimi, S.; Seraj, B. Comparison of Microleakage of Pedo Jacket Crowns and Stainless Steel Crowns Cemented with Different Cements. Front. Dent. 2019, 16, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Asl Aminabadi, N.; Najafpour, E.; Erfanparast, L.; Samiei, M.; Haghifar, M.; Sighari Deljavan, A.; Jamali, Z.; Pournaghi Azar, F.; Shokravi, M. Class III Restoration of Anterior Primary Teeth: In Vitro Retention Comparison of Conventional, Modified and Air-Abrasion Treated Preparations. J. Dent. Res. Dent. Clin. Dent. Prospect. 2014, 8, 89–94. [Google Scholar] [CrossRef]
- Schirrmeister, J.F.; Huber, K.; Hellwig, E.; Hahn, P. Two-Year Evaluation of a New Nano-Ceramic Restorative Material. Clin. Oral Investig. 2006, 10, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Sarapultseva, M.; Sarapultsev, A. Flowable Bulk-Fill Materials Compared to Nano Ceramic Composites for Class I Cavities Restorations in Primary Molars: A Two-Year Prospective Case-Control Study. Dent. J. 2019, 7, 94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Academy of Pediatric Dentistry. Pediatric Restorative Dentistry. The Reference Manual of Pediatric Dentistry. Chicago, Ill.: American Academy of Pediatric Dentistry; 2020:371-83. Available online: https://www.aapd.org/globalassets/media/policies_guidelines/bp_restorativedent.pdf (accessed on 6 August 2021).
- Summitt, J.B. Conservative Cavity Preparations. Dent. Clin. N. Am. 2002, 46, 171–184. [Google Scholar] [CrossRef]
- Koc Vural, U.; Meral, E.; Ergin, E.; Gürgan, S. Twenty-Four-Month Clinical Performance of a Glass Hybrid Restorative in Non-Carious Cervical Lesions of Patients with Bruxism: A Split-Mouth, Randomized Clinical Trial. Clin. Oral Investig. 2020, 24, 1229–1238. [Google Scholar] [CrossRef]
- Chandrasekhar, V.; Rudrapati, L.; Badami, V.; Tummala, M. Incremental Techniques in Direct Composite Restoration. J. Conserv. Dent. 2017, 20, 386–391. [Google Scholar] [CrossRef]
- Donly, K.J.; García-Godoy, F. The Use of Resin-Based Composite in Children: An Update. Pediatr. Dent. 2015, 37, 136–143. [Google Scholar]
- Manmontri, C.; Sirinirund, B.; Langkapint, W.; Jiwanarom, S.; Kowan, V.; Tantayanusorn, S.; Nirunsittirat, A. Retrospective Evaluation of the Clinical Outcomes and Patient and Parental Satisfaction with Resin Strip Crowns in Primary Incisors. Pediatr. Dent. 2018, 40, 425–432. [Google Scholar]
- Kupietzky, A.; Waggoner, W.F.; Galea, J. The Clinical and Radiographic Success of Bonded Resin Composite Strip Crowns for Primary Incisors. Pediatr. Dent. 2003, 25, 577–581. [Google Scholar]
- Ram, D.; Fuks, A.B. Clinical Performance of Resin-Bonded Composite Strip Crowns in Primary Incisors: A Retrospective Study. Int. J. Paediatr. Dent. 2006, 16, 49–54. [Google Scholar] [CrossRef]
- Bücher, K.; Metz, I.; Pitchika, V.; Hickel, R.; Kühnisch, J. Survival Characteristics of Composite Restorations in Primary Teeth. Clin. Oral Investig. 2015, 19, 1653–1662. [Google Scholar] [CrossRef] [PubMed]
- Dalpian, D.M.; Gallina, C.S.; Nicoloso, G.F.; Correa, M.B.; Garcia-Godoy, F.; de Araujo, F.B.; Casagrande, L. Patient-and Treatment-Related Factors May Influence the Longevity of Primary Teeth Restorations in High Caries-Risk Children: A University-Based Retrospective Study. Am. J. Dent. 2018, 31, 261–266. [Google Scholar] [PubMed]
- Walia, T.; Salami, A.A.; Bashiri, R.; Hamoodi, O.M.; Rashid, F. A Randomised Controlled Trial of Three Aesthetic Full-Coronal Restorations in Primary Maxillary Teeth. Eur. J. Paediatr. Dent. 2014, 15, 113–118. [Google Scholar]
- Casagrande, L.; Seminario, A.T.; Correa, M.B.; Werle, S.B.; Maltz, M.; Demarco, F.F.; de Araujo, F.B. Longevity and Associated Risk Factors in Adhesive Restorations of Young Permanent Teeth after Complete and Selective Caries Removal: A Retrospective Study. Clin. Oral Investig. 2017, 21, 847–855. [Google Scholar] [CrossRef] [PubMed]
- Al-Sane, M.; Koerber, A.; Montero, M.; Baskaradoss, J.K.; Al-Sarraf, E.; Arab, M. Sociodemographic and Behavioural Determinants of Early Childhood Caries Knowledge among Expectant Mothers in Kuwait. Eur. Arch. Paediatr. Dent. 2020. [Google Scholar] [CrossRef]
- Kubota, Y.; San Pech, N.; Durward, C.; Ogawa, H. Association between Early Childhood Caries and Maternal Factors among 18- to 36-Month-Old Children in a Rural Area of Cambodia. Oral Health Prev. Dent. 2020, 18, 973–980. [Google Scholar] [CrossRef]
- Correa, M.B.; Peres, M.A.; Peres, K.G.; Horta, B.L.; Barros, A.J.; Demarco, F.F. Do Socioeconomic Determinants Affect the Quality of Posterior Dental Restorations? A Multilevel Approach. J. Dent. 2013, 41, 960–967. [Google Scholar] [CrossRef] [PubMed]
- Laegreid, T.; Gjerdet, N.R.; Johansson, A.-K. Extensive Composite Molar Restorations: 3 Years Clinical Evaluation. Acta Odontol. Scand. 2012, 70, 344–352. [Google Scholar] [CrossRef] [PubMed]
- Bayram, M.; Akgöl, B.B.; Üstün, N. Longevity of Posterior Composite Restorations in Children Suffering from Early Childhood Caries-Results from a Retrospective Study. Clin. Oral Investig. 2021, 25, 2867–2876. [Google Scholar] [CrossRef] [PubMed]
- Duhan, H.; Pandit, I.K.; Srivastava, N.; Gugnani, N.; Gupta, M.; Kochhar, G.K. Clinical Comparison of Various Esthetic Restorative Options for Coronal Build-up of Primary Anterior Teeth. Dent. Res. J. (Isfahan) 2015, 12, 574–580. [Google Scholar] [CrossRef]
- Chen, X.X.; Zhong, J.; Yan, W.J.; Zhang, H.M.; Jiang, X.; Huang, Q.; Xue, S.H.; Liu, X.G. Clinical performance of rensin-bonded composite strip crowns in primary incisors. Beijing Da Xue Xue Bao Yi Xue Ban 2020, 52, 907–912. [Google Scholar] [PubMed]
- Srivastava, A.; Gupta, N.; Marleau, A.; Afrashtehfar, K.I. How Do I Manage a Patient with Intrusion of a Permanent Incisor? J. Can. Dent. Assoc. 2014, 80, e50. [Google Scholar] [PubMed]
- Demarco, F.F.; Corrêa, M.B.; Cenci, M.S.; Moraes, R.R.; Opdam, N.J.M. Longevity of Posterior Composite Restorations: Not Only a Matter of Materials. Dent. Mater. 2012, 28, 87–101. [Google Scholar] [CrossRef]
- Lucarotti, P.S.K.; Holder, R.L.; Burke, F.J.T. Outcome of Direct Restorations Placed within the General Dental Services in England and Wales (Part 3): Variation by Dentist Factors. J. Dent. 2005, 33, 827–835. [Google Scholar] [CrossRef]
- Ribeiro, J.F.; Forgerini, T.V.; Pedrotti, D.; Rocha, R.D.O.; Ardenghi, T.M.; Soares, F.Z.M.; Lenzi, T.L. Performance of Resin Composite Restorations in the Primary Dentition: A Retrospective University-Based Study. Int. J. Paediatr. Dent. 2018, 28, 497–503. [Google Scholar] [CrossRef]
- Sullivan, G.M.; Feinn, R. Using Effect Size—or Why the P Value Is Not Enough. J. Grad. Med. Educ. 2012, 4, 279–282. [Google Scholar] [CrossRef] [Green Version]
| Characteristic | Rating | Criteria |
|---|---|---|
| Color match | Alpha Bravo Charlie | Restoration matches adjacent tooth structure in color and translucency Mismatch in within an acceptable range of tooth color and translucency Mismatch is outside the acceptable range |
| Cavosurface marginal discoloration | Alpha Bravo Charlie | Absence of marginal discoloration Presence of marginal discoloration limited and not extended Evident marginal discoloration penetrated toward the pulp chamber |
| Marginal integrity | Alpha Bravo Charlie | Closely adapted no visible crevice Visible crevice, explorer will penetrate Crevice in which dentin is exposed |
| Surface texture | Alpha Bravo Charlie | Smooth surface Slightly rough or pitted can be refinished Rough, cannot be refinished |
| Postoperative sensitivity | Alpha Bravo | Absence of dentinal hypersensitivity Presence of dentinal hypersensitivity |
| Secondary caries | Alpha Bravo | No evidence of caries Caries is evident |
| Fracture | Alpha Bravo | No evidence of fracture Evidence of fracture |
| Group | Criterion | Type of Procedure | Survival Probability | Number of Events, % | 95% CI Lower | 95% CI Upper | R | Mean Survival |
|---|---|---|---|---|---|---|---|---|
| Group 1 | CM | DCR | 0.900 | 10.0 | 0.812 | 0.998 | 0.29 | 34.8 |
| SCR | 0.975 | 2.5 | 0.928 | 1.000 | 3.51 | 36.0 | ||
| CMD | DCR | 0.900 | 10.0 | 0.812 | 0.998 | 0.29 | 34.8 | |
| SCR | 0.975 | 2.5 | 0.928 | 1.000 | 3.47 | 35.7 | ||
| MI | DCR | 0.950 | 5.0 | 0.885 | 1.000 | 1.00 | 35.7 | |
| SCR | 0.950 | 5.0 | 0.885 | 1.000 | 1.00 | 35.7 | ||
| ST | DCR | 0.925 | 7.5 | 0.847 | 1.000 | 0.64 | 35.1 | |
| SCR | 0.950 | 5.0 | 0.885 | 1.000 | 1.56 | 36.0 | ||
| PS | DCR | 1.000 | 0.0 | NA | NA | NA | NA | |
| SCR | 1.000 | 0.0 | NA | NA | NA | NA | ||
| SC | DCR | 0.950 | 5.0 | 0.885 | 1.000 | 0.49 | 36.0 | |
| SCR | 0.975 | 2.5 | 0.928 | 1.000 | 2.03 | 36.0 | ||
| Fr | DCR | 0.975 | 2.5 | 0.928 | 1.000 | 0.99 | 35.7 | |
| SCR | 0.975 | 2.5 | 0.928 | 1.000 | 1.01 | 36.0 | ||
| Group 2 | CM | DCR | 0.900 | 10.0 | 0.812 | 0.998 | 0.29 | 34.8 |
| SCR | 0.975 | 2.5 | 0.928 | 1.000 | 3.47 | 35.7 | ||
| CMD | DCR | 0.875 | 12.5 | 0.778 | 0.984 | 0.25 | 34.5 | |
| SCR | 0.975 | 2.5 | 0.928 | 1.000 | 4.00 | 35.7 | ||
| MI | DCR | 0,875 | 12,5 | 0,778 | 0,984 | 0,59 | 35,7 | |
| SCR | 0.925 | 7.5 | 0.847 | 1.000 | 1.69 | 35.7 | ||
| ST | DCR | 0.900 | 10.0 | 0.812 | 0.998 | 0.71 | 35.1 | |
| SCR | 0.925 | 7.5 | 0.847 | 1.000 | 1.40 | 36.0 | ||
| PS | DCR | 0.950 | 5.0 | 0.885 | 1.000 | 0.50 | 35.7 | |
| SCR | 0.975 | 2.5 | 0.928 | 1.000 | 1.99 | 36.0 | ||
| SC | DCR | 0.900 | 10.0 | 0.812 | 0.998 | 0.28 | 35.7 | |
| SCR | 0.975 | 2.5 | 0.928 | 1.000 | 3.52 | 36.0 | ||
| Fr | DCR | 0.900 | 10.0 | 0.812 | 0.998 | 0.28 | 35.4 | |
| SCR | 0.975 | 2.5 | 0.928 | 1.000 | 3.52 | 36.0 |
| Criterion | Chi-Square Test | p-Value | Power | Sample Size | |
|---|---|---|---|---|---|
| Group 1 vs. Group 2 | CM | 0.0 | 1.0 | 0.025 | >1000 |
| CMD | 0.1 | 0.7 | 0.051 | >1000 | |
| MI | 1.3 | 0.2 | 0.177 | 454 | |
| ST | 0.1 | 0.7 | 0.055 | >1000 | |
| PS | 2.0 | 0.2 | 0.210 | 316 | |
| SC | 0.7 | 0.4 | 0.114 | 880 | |
| Fr | 1.9 | 0.2 | 0.216 | 336 |
| Criterion | Chi-Square Test | p-Value | Power | Sample Size | |
|---|---|---|---|---|---|
| Group 1 vs. Group 2 | CM | 0.0 | 1.0 | 0.025 | >1000 |
| CMD | 0.0 | 1.0 | 0.025 | >1000 | |
| MI | 0.2 | 0.7 | 0.062 | >1000 | |
| ST | 0.2 | 0.6 | 0.062 | >1000 | |
| PS | 1.0 | 0.3 | 0.126 | 628 | |
| SC | 0.0 | 1.0 | 0.025 | >1000 | |
| Fr | 0.0 | 1.0 | 0.025 | >1000 |
| Criterion | Chi-Square Test | p-Value | Power | Sample Size | |
|---|---|---|---|---|---|
| DCR vs. SCR | CM | 1.9 | 0.2 | 0,216 | 336 |
| CMD | 1.9 | 0.2 | 0,216 | 336 | |
| MI | 0.0 | 1.0 | 0,025 | >1000 | |
| ST | 0.2 | 0.6 | 0,062 | >1000 | |
| PS | NA | NA | NA | NA | |
| SC | 0.3 | 0.6 | 0.076 | >1000 | |
| Fr | 0.0 | 1.0 | 0.025 | >1000 |
| Criterion | Chi-Square Test | p-Value | Power | Sample Size | |
|---|---|---|---|---|---|
| DCR vs. SCR | CM | 1.9 | 0.2 | 0.216 | 336 |
| CMD | 2.8 | 0.1 | 0.294 | 226 | |
| MI | 0.5 | 0.5 | 0.099 | >1000 | |
| ST | 0.2 | 0.7 | 0.055 | >1000 | |
| PS | 0.4 | 0.6 | 0.076 | >1000 | |
| SC | 1.9 | 0.2 | 0.216 | 336 | |
| Fr | 1.9 | 0.2 | 0.216 | 336 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sarapultseva, M.; Sarapultsev, A. 36 Months’ Clinical Performance of Primary Incisors Restorations Depending on the Type of Restorative Technique Used: A Randomized Controlled Trial. Dent. J. 2021, 9, 126. https://doi.org/10.3390/dj9110126
Sarapultseva M, Sarapultsev A. 36 Months’ Clinical Performance of Primary Incisors Restorations Depending on the Type of Restorative Technique Used: A Randomized Controlled Trial. Dentistry Journal. 2021; 9(11):126. https://doi.org/10.3390/dj9110126
Chicago/Turabian StyleSarapultseva, Maria, and Alexey Sarapultsev. 2021. "36 Months’ Clinical Performance of Primary Incisors Restorations Depending on the Type of Restorative Technique Used: A Randomized Controlled Trial" Dentistry Journal 9, no. 11: 126. https://doi.org/10.3390/dj9110126
APA StyleSarapultseva, M., & Sarapultsev, A. (2021). 36 Months’ Clinical Performance of Primary Incisors Restorations Depending on the Type of Restorative Technique Used: A Randomized Controlled Trial. Dentistry Journal, 9(11), 126. https://doi.org/10.3390/dj9110126






