Reliability and Validity of the Arabic Version of a Questionnaire Assessing Pain, Discomfort and Related Jaw Function Impairment after Extraction of Primary Teeth in Children
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Size Calculation
2.2. Questionnaire Description
2.2.1. Forward Translation
2.2.2. Backward Translation
2.3. Pilot Study
2.4. Reliability Tests
2.5. Validity Tests
3. Results
3.1. Internal Consistency
3.2. Criterion Validity
3.3. Content Validity
3.4. Factor Analysis
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Merskey, H.A.F.D.; Bonica, J.J.; Carmon, A.; Dubner, R.; Kerr, F.W.L.; Lindblom, U.; Mumford, J.M.; Nathan, P.W.; Noordenbos, W.; Pagni, C.A.; et al. Pain terms: A list with definitions and notes on usage. Recommended by the IASP Subcommittee on Taxonomy. Pain 1979, 6, 249. [Google Scholar]
- Young, K.D. Pediatric procedural pain. Ann. Emerg. Med. 2005, 45, 160–171. [Google Scholar] [CrossRef]
- Wondimu, B.; Dahllöf, G. Attitudes of Swedish dentists to pain and pain management during dental treatment of children and adolescents. Eur. J. Paediatr. Dent. 2005, 6, 66–72. [Google Scholar] [PubMed]
- Hla, T.K.; Hegarty, M.K.; Russell, P.; Drake-Brockman, T.F.; Ramgolam, A.; Von Ungern-Sternberg, B.S. Perception of Pediatric Pain: A comparison of postoperative pain assessments between child, parent, nurse, and independent observer. Pediatric Anesth. 2014, 24, 1127–1131. [Google Scholar]
- Kimberlin, C.L.; Winterstein, A.G. Validity and reliability of measurement instruments used in research. Am. J. Health Pharm. 2008, 65, 2276–2284. [Google Scholar] [CrossRef] [PubMed]
- Streiner, D.L.; Norman, G.R.; Cairney, J. Health Measurement Scales: A Practical Guide to Their Development and Use, 5th ed.; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- Merkel, S.I.; Voepel-Lewis, T.; Shayevitz, J.R.; Malviya, S. The FLACC: A behavioral scale for scoring postoperative pain in young children. Pediatric Nurs. 1997, 23, 293–297. [Google Scholar]
- Downie, W.W.; Leatham, P.A.; Rhind, V.M.; Wright, V.; Branco, J.A.; Anderson, J.A. Studies with pain rating scales. Ann. Rheum. Dis. 1978, 37, 378–381. [Google Scholar] [CrossRef] [PubMed]
- Garra, G.; Singer, A.J.; Taira, B.R.; Chohan, J.; Cardoz, H.; Chisena, E.; Thode, H.C. Validation of the Wong-Baker FACES Pain Rating Scale in Pediatric Emergency Department Patients. Acad. Emerg. Med. 2010, 17, 50–54. [Google Scholar] [CrossRef] [PubMed]
- McGrath, P.A.; Seifert, C.E.; Speechley, K.N.; Booth, J.C.; Stitt, L.; Gibson, M.C. A new analogue scale for assessing children’s pain: An initial validation study. Pain 1996, 64, 435–443. [Google Scholar] [CrossRef]
- Naoumova, J.; Kjellberg, H.; Mohlin, B.; Kurol, J. Pain, discomfort, and use of analgesics following the extraction of primary canines in children with palatally displaced canines. Int. J. Paediatr. Dent. 2011, 22, 17–26. [Google Scholar] [CrossRef]
- Stegenga, B.; De Bont, L.G.; De Leeuw, R.; Boering, G. Assessment of mandibular function impairment associated with temporomandibular joint osteoarthrosis and internal derangement. J. Orofac. Pain 1993, 7, 183–195. [Google Scholar]
- Feldmann, I.; List, T.; John, M.T.; Bondemark, L. Reliability of a Questionnaire Assessing Experiences of Adolescents in Orthodontic Treatment. Angle Orthod. 2007, 77, 311–317. [Google Scholar] [CrossRef]
- Campbell, C.M.; Edwards, R.R. Ethnic differences in pain and pain management. Pain Manag. 2012, 2, 219–230. [Google Scholar] [CrossRef]
- Hair, J.; Black, W.; Babin, B. Multivariate Data Analysis, 7th ed.; Pearson Education Limited: Harlow, Essex, UK, 2014. [Google Scholar]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the Process of Cross-Cultural Adaptation of Self-Report Measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef]
- Hilton, C.E. The importance of pretesting questionnaires: A field research example of cognitive pretesting the Exercise referral Quality of Life Scale (ER-QLS). Int. J. Soc. Res. Methodol. 2015, 20, 21–34. [Google Scholar] [CrossRef]
- Nunnally, J.C. Psychometric Theory, 2nd ed.; McGraw-Hill: New York, NY, USA, 1978. [Google Scholar]
- Streiner, D.L. Starting at the Beginning: An Introduction to Coefficient Alpha and Internal Consistency. J. Personal. Assess. 2003, 80, 99–103. [Google Scholar] [CrossRef]
- Waltz, C.F.; Strickland, O.L.; Lenz, E.R. Measurement in Nursing and Health Research, 5th ed.; Springer Publishing Company: New York, NY, USA, 2010. [Google Scholar]
- Almanasreh, E.; Moles, R.J.; Chen, T.F. Evaluation of methods used for estimating content validity. Res. Soc. Adm. Pharm. 2019, 15, 214–221. [Google Scholar] [CrossRef]
- Lynn, M.R. Determination and Quantification of Content Validity. Nurs. Res. 1986, 35, 382–385. [Google Scholar] [CrossRef]
- Polit, D.F.; Beck, C.T.; Owen, S.V. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res. Nurs. Health 2007, 30, 459–467. [Google Scholar] [CrossRef]
- Wright, G.Z.; Weinberger, S.J.; Marti, R.; Plotzke, O. The effectiveness of infiltration anesthesia in the mandibular primary molar region. Pediatric Dent. 1991, 13, 278–283. [Google Scholar]
- Bailey, B.; Gravel, J.; Daoust, R. Reliability of the visual analog scale in children with acute pain in the emergency department. Pain 2012, 153, 839–842. [Google Scholar] [CrossRef]
- Suhr, D.D. Exploratory or confirmatory factor analysis? In Proceedings of the SAS Users Group International Conference (SUGI31), San Francisco, CA, USA, 26–29 March 2006.
- Williams, B.; Onsman, A.; Brown, T. Exploratory factor analysis: A five-step guide for novices. Australas. J. Paramed. 2010, 8. [Google Scholar] [CrossRef]
- Maccallum, R.C.; Widaman, K.F.; Preacher, K.J.; Hong, S. Sample Size in Factor Analysis: The Role of Model Error. Multivar. Behav. Res. 2001, 36, 611–637. [Google Scholar] [CrossRef]
- Hogarty, K.Y.; Hines, C.V.; Kromrey, J.D.; Ferron, J.M.; Mumford, K.R. The Quality of Factor Solutions in Exploratory Factor Analysis: The Influence of Sample Size, Communality, and Overdetermination. Educ. Psychol. Meas. 2005, 65, 202–226. [Google Scholar] [CrossRef]
- De Tovar, C.; Von Baeyer, C.L.; Wood, C.; Alibeu, J.-P.; Houfani, M.; Arvieux, C. Postoperative Self-Report of Pain in Children: Interscale Agreement, Response to Analgesic, and Preference for a Faces Scale and a Visual Analogue Scale. Pain Res. Manag. 2010, 15, 163–168. [Google Scholar] [CrossRef]
- Grant, J.S.; Davis, L.L. Selection and use of content experts for instrument development. Res. Nurs. Health 1997, 20, 269–274. [Google Scholar] [CrossRef]
- Bijur, P.E.; Silver, W.; Gallagher, E.J. Reliability of the Visual Analog Scale for Measurement of Acute Pain. Acad. Emerg. Med. 2001, 8, 1153–1157. [Google Scholar] [CrossRef]
- Beyer, J.E.; McGrath, P.; Berde, C.B. Discordance between self-report and behavioral pain measures in children aged 3–7 years after surgery. J. Pain Symptom Manag. 1990, 5, 350–356. [Google Scholar] [CrossRef]
- Corah, N.L. Development of a Dental Anxiety Scale. J. Dent. Res. 1969, 48, 596. [Google Scholar] [CrossRef] [PubMed]
- Sjögren, A.; Arnrup, K.; Jensen, C.; Knutsson, I.; Huggare, J. Pain and fear in connection to orthodontic extractions of deciduous canines. Int. J. Paediatr. Dent. 2010, 20, 193–200. [Google Scholar] [CrossRef]
- Versloot, J.; Veerkamp, J.S.J.; Hoogstraten, J. Dental Discomfort Questionnaire: Assessment of dental discomfort and/or pain in very young children. Community Dent. Oral Epidemiol. 2006, 34, 47–52. [Google Scholar] [CrossRef] [PubMed]
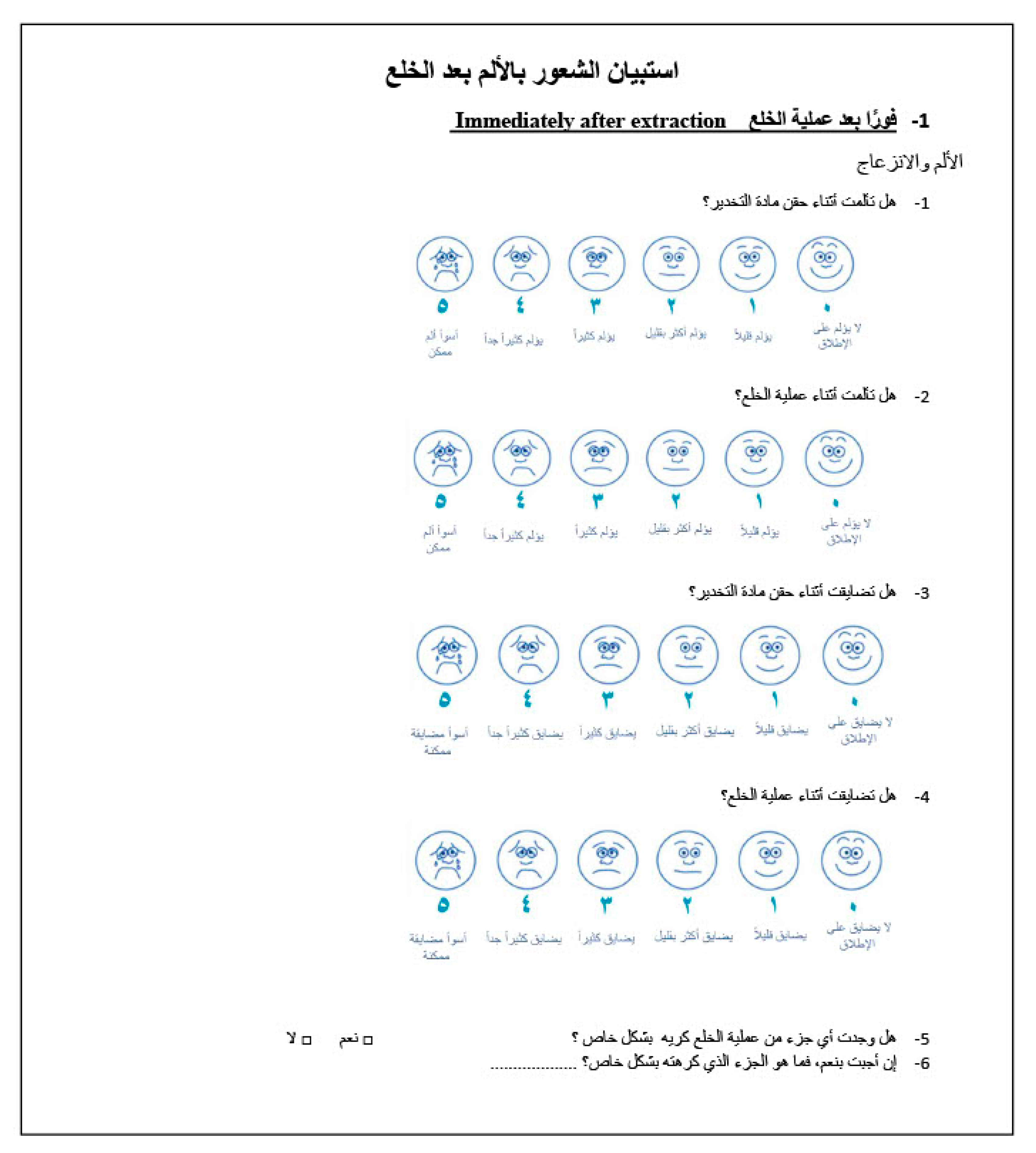
| 1. Immediately after extraction | 1 فورًا بعد عملية الخلع |
| 1.1 Pain during injection | 1.1 هل تألمت أثناء حقن مادة التخدير؟ |
| 1.2 Pain during extraction | 1.2 هل تألمت أثناء عملية الخلع؟ |
| 1.3 Discomfort during injection | 1.3 هل تضايقت أثناء حقن مادة التخدير؟ |
| 1.4 Discomfort during extraction | 1.4 هل تضايقت أثناء عملية الخلع؟ |
| 1.5 Was any part of the extraction particularly unpleasant? | 1. 5 هل وجدت أي جزء من عملية الخلع كريه بشكل خاص؟ |
| 1.6 If so, explain which part was particularly unpleasant | 1.6 إن أجبت بنعم، فما هو الجزء الذي كرهته بشكل خاص؟ |
| 2. First evening after extraction | 2 المساء الأول بعد عملية الخلع |
| 2.1 Pain from extraction site * | 2.1 هل عندك ألم من مكان الخلع الآن ؟ |
| 2.2 Discomfort from extraction site * | 2.2 هل مكان الخلع يضايقك الآن ؟ |
| 2.3 Analgesic consumption * | 2.3 هل تناولت مسكنات للألم؟ |
| 2.4 Kind of analgesics * | 2.4إن أجبت بنعم، فما هو نوع مسكنات الألم التي استخدمتها ؟ |
| 3. One week after extraction | 3 بعد أسبوع من عملية الخلع |
| 3.1 Pain from extraction site * | 3.1هل عندك ألم من مكان الخلع الآن ؟ |
| 3.2 Discomfort from extraction site * | 3.2هل مكان الخلع يضايقك الآن ؟ |
| 3.3 Analgesic consumption last week * | 3.3هل تناولت مسكنات للألم خلال الأسبوع الماضي؟ |
| 3.4 Number of days using analgesics | 3.4إن أجبت بنعم، فكم عدد الأيام التي تناولت فيها مسكنات الألم؟ |
| 3.5 Use of non-prescription drugs | 3.5هل كان الدواء بدون وصفة طبية؟ |
| 3.6 Kind of analgesic * | 3.6 إن أجبت بنعم، فماهونوع مسكن الألم الذي استخدمته؟ |
| 3.7 Use of prescription drugs | 3.7هل كان الدواء بوصفة طبية؟ |
| 3.8 Kind of analgesic | 3.8 إن أجبت بنعم، فماهونوع مسكن الألم الذي استخدمته؟ |
| 3.9 School absence | 3.9هل تغيبت عن المدرسة الأسبوع الماضي بسبب الألم في مكان الخلع؟ |
| 3.10 Number of days | 3.10 إن أجبت بنعم، فكم عدد الأيام التي تغيبت فيها عن المدرسة؟ |
| 3.11 Leisure activities refrain | 3.11 هل امتنعت عن القيام بالأنشطة الترفيهية الأسبوع الماضي بسبب الألم في مكان الخلع؟ |
| 3.12 Number of days | 3.12 إن أجبت بنعم، فما هي الأنشطة التي امتنعت عن القيام بها؟ |
| 3.13 Sleep disturbance | 3.13 هل اضطرب نومك في الأسبوع الماضي بسبب الألم في مكان الخلع؟ |
| 4. Jaw-function impairment after one week | 4
الخلل الوظيفي للفك
إذا كانت لديك صعوبات بعد الخلع، فإلى أي مدى كان تأثيرها على كل مما يلي؟ |
| 4.1 Leisure | 4.1 وقت فراغك |
| 4.2 Speech | 4.2 كلامك |
| 4.3 To take a big bite | 4.3 تناول لقمة كبيرة |
| 4.4 To chew hard food | 4.4 مضغ الطعام القاسي |
| 4.5 To chew soft food | 4.5 مضغ الطعام الليّن |
| 4.6 School work | 4.6 الواجبات المدرسية |
| 4.7 To drink | 4.7 الشرب |
| 4.8 To laugh | 4.8 الضحك |
| 4.9 To chew on extraction site | 4.9 مضغ الطعام مكان الخلع |
| 4.10 To yawn | 4.10 التثاؤب |
| Observations | 1. Comfort | 2. Mild Discomfort | 3. Moderately Painful | 4. Painful |
|---|---|---|---|---|
| Sounds | No sounds indicating pain | Nonspecific sounds; possibly indicating pain | Specific verbal complaints, e.g., “ow”, raising voice | Verbal complaints indicating intense pain, e.g., screaming, sobbing |
| Eyes | No eye signs of discomfort | Eyes wide, showing concern, but no tears | Watery eyes and/or flinching eyes | Crying, tears running down face |
| Motor | Hands relaxed; no apparent body tenseness | Hands show some distress or tension, grasping chair due to discomfort, muscular tension | Random movements of arms or body without aggressive intention to make physical contact, grimace, twitch | Movements of hands trying to make aggressive physical contact, e.g., punching, pulling head away |
| vs. SEM | vs. VAS | |
|---|---|---|
| Questionnaire Local Anesthesia Scores | r = 0.36 | r = 0.63 |
| (p = 0.0097) | (p < 0.0001) | |
| weak correlation | strong correlation | |
| Questionnaire Extraction Scores | r = 0.48 | r = 0.77 |
| (p = 0.0004) | (p < 0.0001) | |
| moderate correlation | strong correlation | |
| Total Score | r = 0.36 | r = 0.75 |
| (p = 0.01) | (p < 0.0001) | |
| weak correlation | strong correlation |
| Items | Expert 1 | Expert 2 | Expert 3 | Expert 4 | Expert 5 | Number in Agreement | Item CVI |
|---|---|---|---|---|---|---|---|
| Questions immediately after extraction | |||||||
| 1.1 | X | X | X | X | X | 5 | 1 |
| 1.2 | X | X | X | X | X | 5 | 1 |
| 1.3 | X | X | X | X | - | 4 | 0.8 |
| 1.4 | X | X | X | X | X | 5 | 1 |
| 1.5 | X | - | - | X | X | 3 | 0.6 |
| 1.6 | X | X | X | X | X | 5 | 1 |
| Questions first evening after extraction | |||||||
| 2.1 | X | X | X | X | X | 5 | 1 |
| 2.2 | X | X | X | X | X | 5 | 1 |
| 2.3 | X | - | X | X | X | 4 | 0.8 |
| 2.4 | X | X | X | X | X | 5 | 1 |
| Questions one week after extraction | |||||||
| 3.1 | X | - | X | X | X | 4 | 0.8 |
| 3.2 | X | - | X | X | X | 4 | 0.8 |
| 3.3 | X | - | X | X | X | 4 | 0.8 |
| 3.4 | X | X | X | X | - | 4 | 0.8 |
| 3.5 | X | X | - | X | X | 4 | 0.8 |
| 3.6 | X | X | X | X | X | 5 | 1 |
| 3.7 | X | X | - | X | X | 4 | 0.8 |
| 3.8 | X | X | - | X | X | 4 | 0.8 |
| 3.9 | X | - | X | X | X | 4 | 0.8 |
| 3.10 | X | X | X | X | X | 5 | 1 |
| 3.11 | X | X | X | X | - | 4 | 0.8 |
| 3.12 | X | X | X | X | X | 5 | 1 |
| 3.13 | X | X | X | X | X | 5 | 1 |
| Functional Jaw impairment after 1 week | |||||||
| 4.1 | X | X | - | X | X | 4 | 0.8 |
| 4.2 | X | X | X | X | X | 5 | 1 |
| 4.3 | X | X | X | X | X | 5 | 1 |
| 4.4 | X | X | X | X | X | 5 | 1 |
| 4.5 | X | X | X | X | X | 5 | 1 |
| 4.6 | X | X | X | X | - | 4 | 0.8 |
| 4.7 | X | X | X | X | X | 5 | 1 |
| 4.8 | X | X | X | X | X | 5 | 1 |
| 4.9 | X | X | X | X | X | 5 | 1 |
| 4.10 | X | X | X | X | X | 5 | 1 |
| Proportion relevant | 1 | 0.81 | 0.84 | 1 | 0.87 | Mean I-CVI = 0.90 Mean expert proportion = 0.90 | |
| 15 items with factor loading >0.5 | Factor 1 | Factor 2 | Factor 3 | Factor 4 |
| 3.3 Analgesics (after 1 week) | 0.97601 | 0.08083 | 0.04242 | −0.03450 |
| 3.4 Number of days taking analgesics (after 1 week) | 0.94949 | 0.04214 | 0.14526 | 0.03189 |
| 3.5 Nonprescription drugs (after 1 week) | 0.97539 | 0.08983 | 0.05328 | −0.01819 |
| 3.6 Kind of analgesics (after 1 week) | 0.88750 | 0.23602 | −0.04188 | 0.05994 |
| 3.2 Discomfort from extraction site (after 1 week) | 0.01886 | 0.67665 | 0.13159 | 0.00716 |
| 4.1 Leisure | 0.12581 | 0.85896 | 0.04080 | 0.06984 |
| 4.2 Speech | 0.18339 | 0.66459 | 0.39500 | 0.12720 |
| 4.6 School work | 0.14400 | 0.85807 | −0.01563 | −0.13424 |
| 4.4 To chew hard food | −0.00090 | 0.21960 | 0.80151 | 0.06150 |
| 4.5 To chew soft food | 0.12383 | −0.12429 | 0.77466 | −0.04103 |
| 4.9 To chew on extraction site | 0.00057 | 0.43592 | 0.75448 | −0.02718 |
| 1.1 Pain with local anesthesia | −0.13831 | 0.00163 | −0.04434 | 0.58476 |
| 1.2 Pain with extraction | 0.04441 | 0.22440 | −0.06731 | 0.78819 |
| 1.3 Discomfort with LA | 0.08652 | −0.12778 | −0.01373 | 0.53109 |
| 1.4 Discomfort with extraction | 0.04587 | 0.00012 | 0.16412 | 0.79893 |
| Eigen Value | 4.3768 | 2.6250 | 1.9073 | 1.5497 |
| % of explained variance | 29.18 | 17.50 | 12.72 | 10.33 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naaman, R.; El-Housseiny, A.A.; Alamoudi, N.; Helal, N.; Sahhaf, R. Reliability and Validity of the Arabic Version of a Questionnaire Assessing Pain, Discomfort and Related Jaw Function Impairment after Extraction of Primary Teeth in Children. Dent. J. 2020, 8, 120. https://doi.org/10.3390/dj8040120
Naaman R, El-Housseiny AA, Alamoudi N, Helal N, Sahhaf R. Reliability and Validity of the Arabic Version of a Questionnaire Assessing Pain, Discomfort and Related Jaw Function Impairment after Extraction of Primary Teeth in Children. Dentistry Journal. 2020; 8(4):120. https://doi.org/10.3390/dj8040120
Chicago/Turabian StyleNaaman, Reem, Azza A. El-Housseiny, Najlaa Alamoudi, Narmin Helal, and Rahaf Sahhaf. 2020. "Reliability and Validity of the Arabic Version of a Questionnaire Assessing Pain, Discomfort and Related Jaw Function Impairment after Extraction of Primary Teeth in Children" Dentistry Journal 8, no. 4: 120. https://doi.org/10.3390/dj8040120
APA StyleNaaman, R., El-Housseiny, A. A., Alamoudi, N., Helal, N., & Sahhaf, R. (2020). Reliability and Validity of the Arabic Version of a Questionnaire Assessing Pain, Discomfort and Related Jaw Function Impairment after Extraction of Primary Teeth in Children. Dentistry Journal, 8(4), 120. https://doi.org/10.3390/dj8040120





