Superficial Temporal Artery Perforator Flap: Indications, Surgical Outcomes, and Donor Site Morbidity
Abstract
1. Introduction
2. Materials and Methods
Surgical Technique
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Ethics Statement/Confirmation of Patients’ Permission
References
- Mustarde, J.C. Cheek rotation skin flap to the lower eyelid. In Grabb’s Encyclopedia of Flaps; Strauch, B., Ed.; Little Brown: Boston, MA, USA, 1990; p. 51. [Google Scholar]
- Dolen, U.C.; Baltu, Y.; Aydin, O. Subunit Reconstruction of Mid-Facial Defects With Free Style Facial Perforator Flaps. J. Craniofac. Surg. 2018, 29, 1574–1577. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.H.; Wei, F.C. Microsurgical free flap in head and neck reconstruction. Head Neck 2010, 32, 1236–1245. [Google Scholar] [CrossRef] [PubMed]
- Esposito, L.; Razzano, S.; Lo Faro, C.; Dell’Aversana Orabona, G.; Schonauer, F. Pinna fillet flap after advanced external ear tumor resection. JPRAS Open 2016, 8, 9–13. [Google Scholar] [CrossRef][Green Version]
- Massarelli, O.; Vaira, L.A.; Gobbi, R.; Dell’aversana Orabona, G.; De Riu, G. Reconstruction of full-thickness cheek defect with chimeric facial artery free flap: A case report. Microsurgery 2018, 38, 427–431. [Google Scholar] [CrossRef] [PubMed]
- Snow, S.N.; Stiff, M.; Lambert, D.; Tsoi, C.; Mohs, F.E. Freehand technique to harvest partial-thickness skin to repair superficial facial defects. Dermatol. Surg. 1995, 21, 153–157. [Google Scholar] [CrossRef] [PubMed]
- Pipkorn, P.; Rosenquist, K.; Zenga, J. Functional considerations in oral cavity reconstruction. Curr. Opin. Otolaryngol. Head Neck Surg. 2018, 26, 326–333. [Google Scholar] [CrossRef] [PubMed]
- Kajikawa, A.; Ueda, K. Bilateral eyebrow reconstruction using a unilateral extended superficial temporal artery flap. Ann. Plast. Surg. 2003, 50, 416–419. [Google Scholar] [CrossRef] [PubMed]
- Kilinc, H.; Geyik, Y.; Aytekin, A.H. Double-skin paddled superficial temporofascial flap for the reconstruction of full-thickness cheek defect. J. Craniofac. Surg. 2013, 24, e92–e95. [Google Scholar] [CrossRef] [PubMed]
- Small, J.O.; Leonard, A.G. Posterior superficial temporal artery island flap for intra-oral reconstruction: A case report. Br. J. Plast. Surg. 1985, 38, 488–491. [Google Scholar] [CrossRef]
- Uchinuma, E.; Sakurai, H.; Shioya, N. Anterofrontal superficial temporal artery island flap for full-thickness eyelid reconstruction. Ann. Plast. Surg. 1989, 23, 433–436. [Google Scholar] [CrossRef] [PubMed]
- Scaglioni, M.F.; Suami, H.; Brandozzi, G.; Dusi, D.; Chang, E.I. Cadaveric dissection and clinical experience with 20 consecutive tunneled pedicled superficial temporal artery perforator (STAP) flaps for ear reconstruction. Microsurgery 2015, 35, 190–195. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.P.; Lai, C.S.; Tsai, C.C.; Lin, T.M.; Lin, S.D. Total upper lip reconstruction with a free temporal scalp flap: Long-term follow-up. Head Neck 2003, 25, 602–605. [Google Scholar] [CrossRef] [PubMed]
- Tan, O.; Atik, B.; Ergen, D. Temporal flap variations for craniofacial reconstruction. Plast. Reconstr. Surg. 2007, 119, 152e–163e. [Google Scholar] [CrossRef] [PubMed]
- Algan, S.; Kara, M.; Cinal, H.; Barin, E.Z.; Inaloz, A.; Tan, O. The Temporal Artery Island Flap: A Good Reconstructive Option for Small to Medium-Sized Facial Defects. J. Oral. Maxillofac. Surg. 2018, 76, 894–899. [Google Scholar] [CrossRef] [PubMed]
- Dunham, T.V. A Method for Obtaining a Skin-Flap from the Scalp and a Permanent Buried Vascular Pedicle for Covering Defects of the Face. Ann. Surg. 1893, 17, 677–679. [Google Scholar] [PubMed]
- Elbanoby, T.M.; Elbatawy, A.; Aly, G.M.; Ayad, W.; Helmy, Y.; Helmy, E.; Sholkamy, K.; Dahshan, H.; Al-Hady, A. Bifurcated Superficial Temporal Artery Island Flap for the Reconstruction of a Periorbital Burn: An Innovation. Plast. Reconstr. Surg. Glob. Open 2016, 4, e748. [Google Scholar] [CrossRef] [PubMed]
- Lyons, G.B.; Milroy, B.C.; Lendvay, P.G.; Teston, L.M. Upper lip reconstruction: Use of the free superficial temporal artery hair-bearing flap. Br. J. Plast. Surg. 1989, 42, 333–336. [Google Scholar] [CrossRef]
- Ceran, F.; Sagir, M.; Saglam, O.; Pilanci, O.; Kuvat, S.V. Eyebrow reconstruction after tumor excision by using superficial temporal artery island flap. J. Craniofac. Surg. 2014, 25, 2263–2264. [Google Scholar] [CrossRef] [PubMed]
- Elbanoby, T.M.; Zidan, S.M.; Elbatawy, A.M.; Aly, G.M.; Sholkamy, K. Superficial temporal artery flap for reconstruction of complex facial defects: A new algorithm. Arch. Plast. Surg. 2018, 45, 118–127. [Google Scholar] [CrossRef] [PubMed]
- Ozdemir, R.; Sungur, N.; Sensoz, O.; Uysal, A.C.; Ulusoy, M.G.; Ortak, T.; Baran, C.N. Reconstruction of facial defects with superficial temporal artery island flaps: A donor site with various alternatives. Plast. Reconstr. Surg. 2002, 109, 1528–1535. [Google Scholar] [CrossRef] [PubMed]


| Patient | Demographics | Motivation to Surgery | Surgical Procedure Associated to Cover the Defect | Surgical Procedure Associated to Reduce Donor Site Morbidity | Clinical Condition Associated | Donor Site Closure | Further Refinements Procedure | Size of the Flap |
|---|---|---|---|---|---|---|---|---|
| Case 1 | 72 y.o. (M) | Microsurgical flap failure | Local advancement flap to reduce graft size | Hypertension | Skin graft | 15 × 7 cm | ||
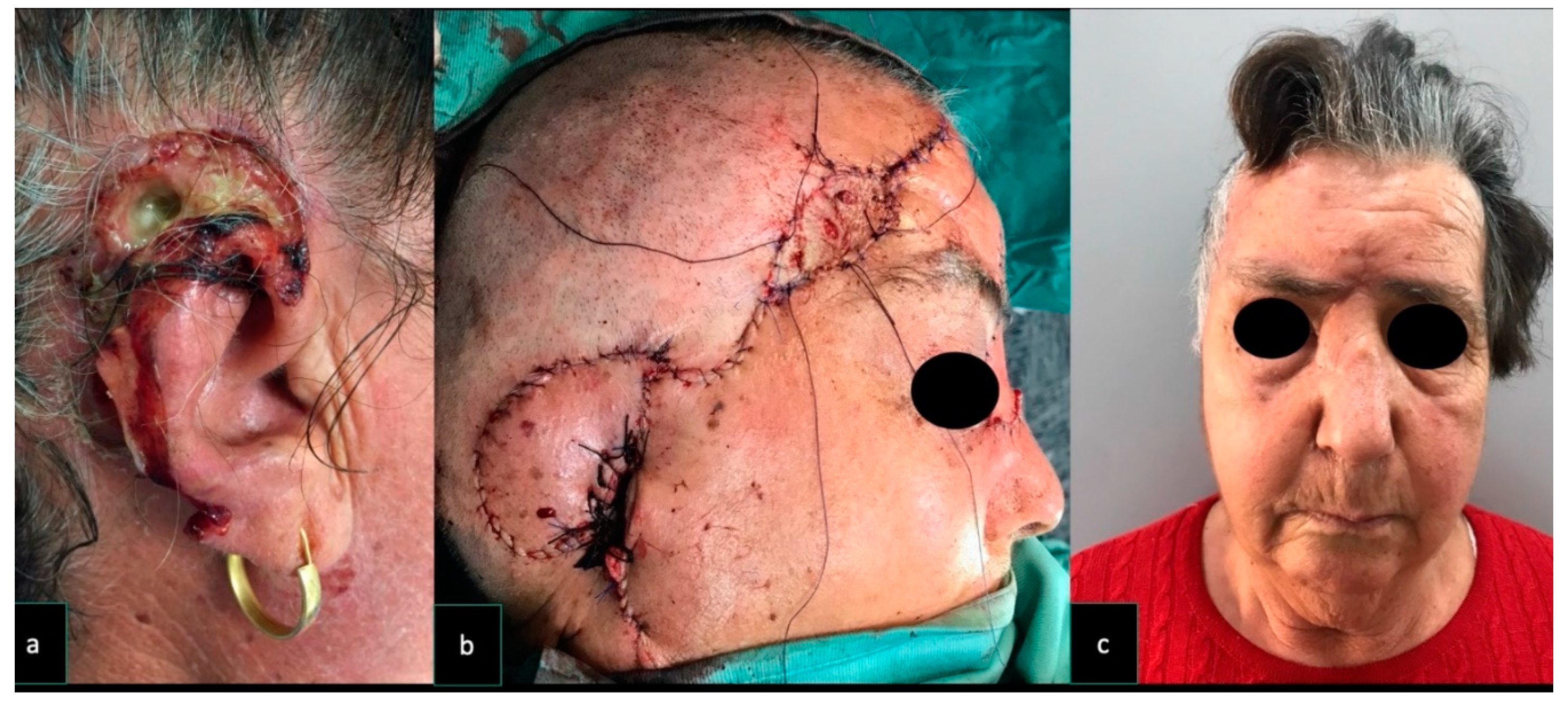
| Case 2 | 76 y.o. (F) | Ear squamous carcinoma | Local advancement flap to reduce graft size | Hypertension; diabetes | Skin graft | 9 × 7 cm | ||
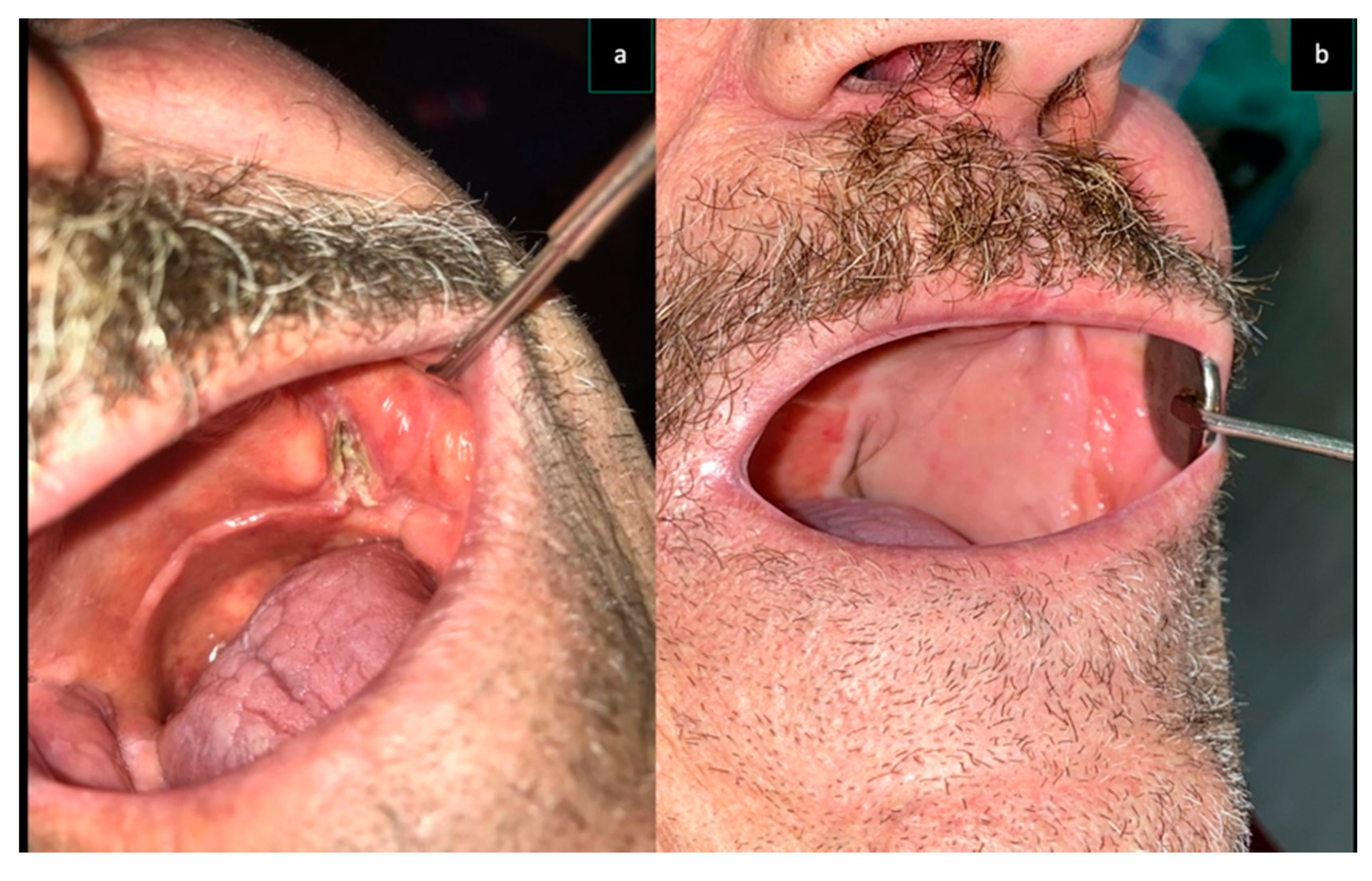
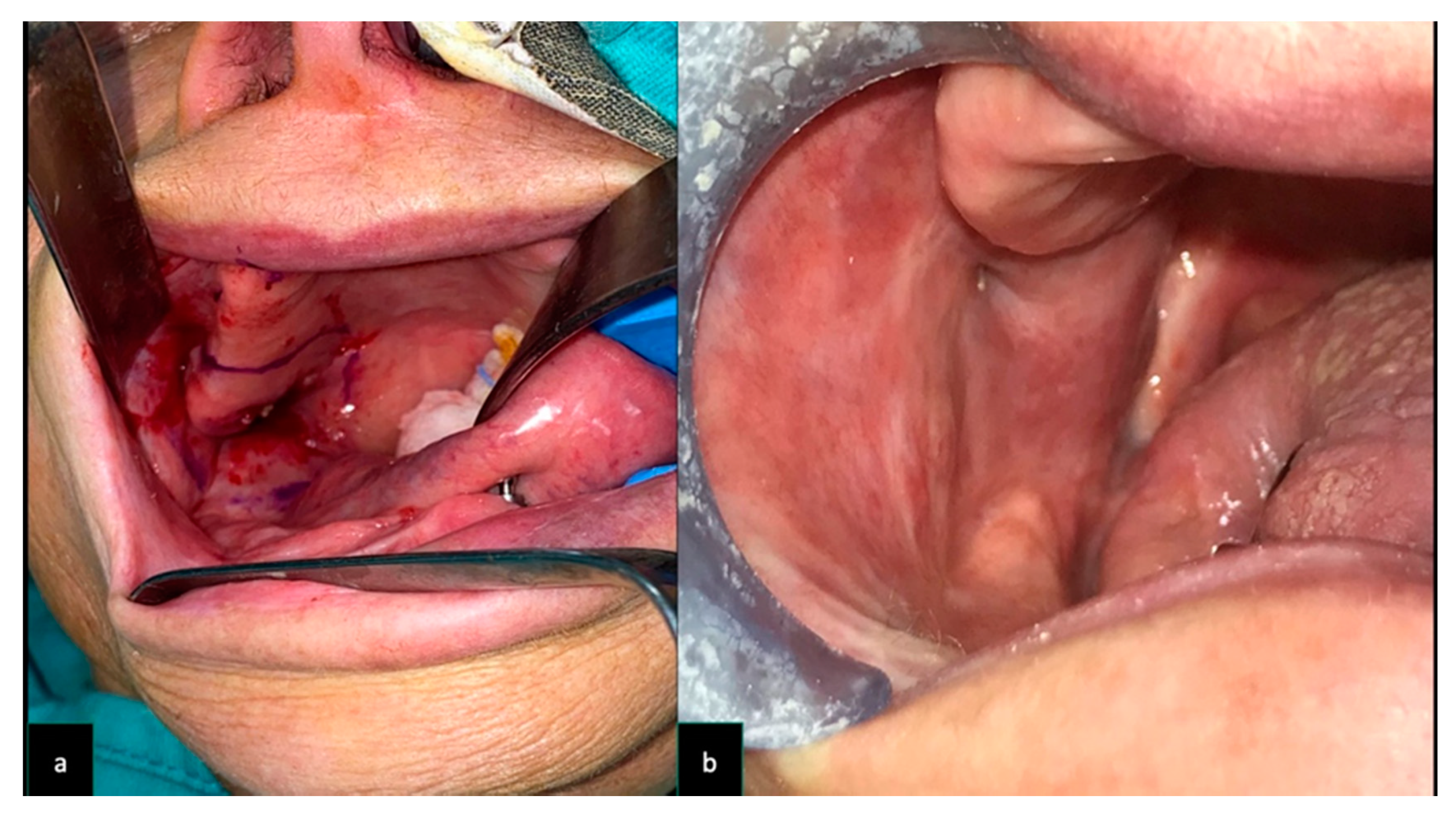
| Case 3 | 74 y.o. (M) | L tuber maxillae carcinoma | Local advancement flap to reduce graft size | Neck depleted vessel, previous RT; hypertension | Skin graft | HA injection on the grafted site; surgical eyebrow touch up | 7 × 7 cm | |
| Case 4 | 62 y.o. (M) | L maxillary cancer | RFFF for the internal lining | Hypertension; diabetes | Synthetic acellular dermal regeneration template | 7 × 7 cm | ||
| Case 5 | 78 y.o. (M) | Partial microsurgical flap failure | Local advancement flap to have direct closure | Diabetes | Direct closure | 5 × 5 cm | ||
| Case 6 | 79 y.o. (F) | R tuber maxillae carcinoma | Forehead lift | Neck depleted vessel, previous RT | Skin graft | 9 × 9 cm | ||
| Case 7 | 87 y.o. (M) | R Cheek/nasal side wall/eyelid (skin) squamous cell carcinoma | Glabellar flap and upper eyelid flap | Local rotational flap to reduce graft size | Hypercolesterolemia | Skin graft | 5 × 5 cm | |
| Case 8 | 72 y.o. (M) | R Cheek BCC | Local advancement flap to have direct closure | Direct closure | 4 × 4 cm | |||
| Case 9 | 82 y.o. (M) | R Cheek BCC | Local advancement flap to reduce graft size | Neck depleted vessel, previous RT | Skin graft | 5 × 4 cm |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rauso, R.; Nicoletti, G.F.; Sesenna, E.; Lo Faro, C.; Chirico, F.; Fragola, R.; Lo Giudice, G.; Tartaro, G. Superficial Temporal Artery Perforator Flap: Indications, Surgical Outcomes, and Donor Site Morbidity. Dent. J. 2020, 8, 117. https://doi.org/10.3390/dj8040117
Rauso R, Nicoletti GF, Sesenna E, Lo Faro C, Chirico F, Fragola R, Lo Giudice G, Tartaro G. Superficial Temporal Artery Perforator Flap: Indications, Surgical Outcomes, and Donor Site Morbidity. Dentistry Journal. 2020; 8(4):117. https://doi.org/10.3390/dj8040117
Chicago/Turabian StyleRauso, Raffaele, Giovanni Francesco Nicoletti, Enrico Sesenna, Carmelo Lo Faro, Fabrizio Chirico, Romolo Fragola, Giorgio Lo Giudice, and Gianpaolo Tartaro. 2020. "Superficial Temporal Artery Perforator Flap: Indications, Surgical Outcomes, and Donor Site Morbidity" Dentistry Journal 8, no. 4: 117. https://doi.org/10.3390/dj8040117
APA StyleRauso, R., Nicoletti, G. F., Sesenna, E., Lo Faro, C., Chirico, F., Fragola, R., Lo Giudice, G., & Tartaro, G. (2020). Superficial Temporal Artery Perforator Flap: Indications, Surgical Outcomes, and Donor Site Morbidity. Dentistry Journal, 8(4), 117. https://doi.org/10.3390/dj8040117







