Prevalence of Peri-Implantitis: A Multi-Centered Cross-Sectional Study on 248 Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
- Bleeding on probing and/or presence of exudate/suppuration;
- Peri-implant bone loss greater than 0.2 mm/year, according to Albrektsson et al. 1986 [7];
- ≥1 mm pocket depth compared with previous examinations.
2.2. Study Population
2.3. Clinical Examination
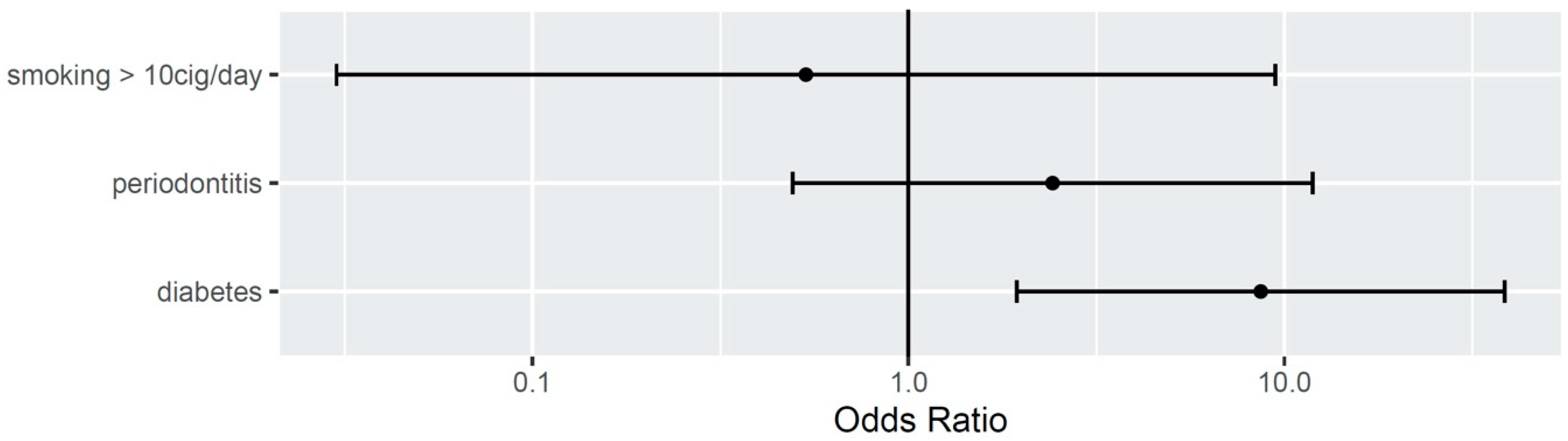
- Systemic risk factors (smoking, history of periodontitis and diabetes);
- Implant characteristics and manufacturer;
- Date of implant insertion and loading;
- X-ray at prosthetic loading;
- Keratinized tissue;
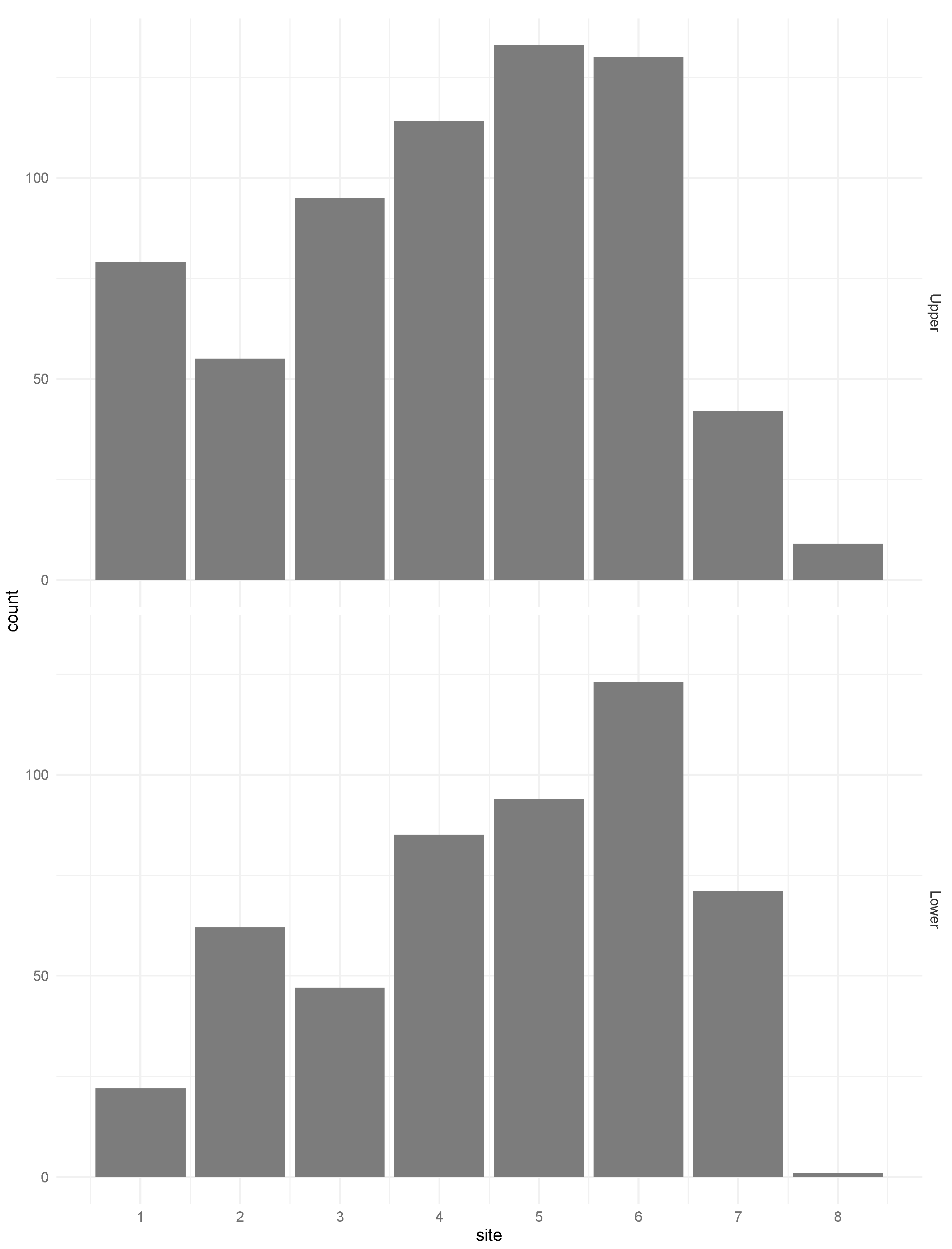
- Probing depth assessed at 6 aspects around each implant;
- Recession, defined as implant neck exposure or worst;
- Plaque index;
- Bleeding on probing;
- X-ray where required (once a year or in case of bleeding on probing associated with increased probing);
- Recall visit dates;
- Type of retention of the prosthesis (cemented/screwed).
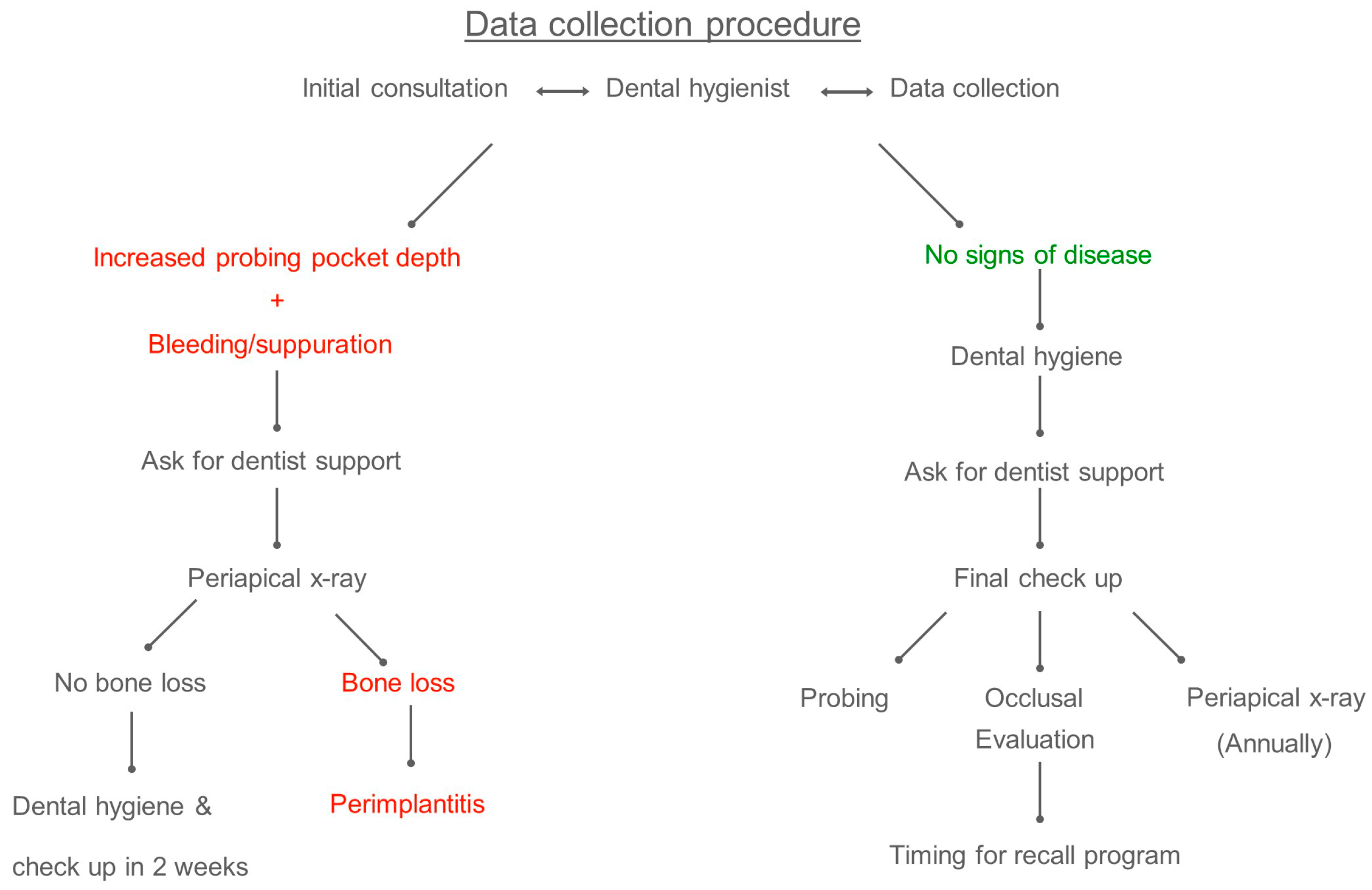
- If there were no signs of disease, the hygienist carried out the dental hygiene procedure, involving the use of ultrasonic devices, titanium scalers, air-flow powder and polishing. The dental hygienist later called the dentist for a final check-up evaluation. The dentist performed a complete clinical inspection. Every implant was probed again and occlusal evaluation was performed with 40µ articulation paper (occlusal contact required) (Arti-check, Bausch) and with 8µ (Hanel Shimstock Foil, Coltene) (no contact needed). Occlusal adjustment was performed when needed. Peri-apical X-rays of the implants were taken annually. At the end of the procedure, the timing for recall appointment was decided.
- If the dental hygienist registered bleeding or suppuration on probing with increased pocket depth, he/she asked for dentist support. The dentist took a peri-apical X-ray of the implant(s) involved: if there was greater than expected bone loss with respect to the last periapical X-ray, the implant was considered affected by peri-implantitis and the relative treatment plan was discussed. Otherwise, the dental hygiene was performed, and a follow-up visit was scheduled in 2 weeks. (see Figure 1).
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Moraschini, V.; Poubel, L.A.; Ferreira, V.F.; Barboza Edos, S. Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: A systematic review. Int. J. Oral Maxillofac. Surg. 2015, 44, 377–388. [Google Scholar] [CrossRef]
- Pjetursson, B.E.; Asgeirsson, A.G.; Zwahlen, M.; Sailer, I. Improvements in implant dentistry over the last decade: Comparison of survival and complication rates in older and newer publications. Int. J. Oral Maxillofac. Implants 2014, 29, 308–324. [Google Scholar] [CrossRef] [PubMed]
- Berglundh, T.; Armitage, G.; Araújo, M.G.; Avila-Ortiz, G.; Blanco, J.; Camargo, P.M.; Chen, S.; Cochran, D.; Derks, J.; Figuero, E.; et al. Peri-implant diseases and conditions: Consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Clin. Periodontol. 2018, 89, S313–S318. [Google Scholar] [CrossRef] [PubMed]
- Meyle, J.; Casado, P.; Fourmousis, I.; Kumar, P.; Quirynen, M.; Salvi, G.E. General genetic and acquired risk factors, and prevalence of peri-implant diseases—Consensus report of working group 1. Int. Dent. J. 2019, 69 (Suppl. 2), 3–6. [Google Scholar] [CrossRef] [PubMed]
- Derks, J.; Tomasi, C. Peri-implant health and disease. A systematic review of current epidemiology. J. Clin. Periodontol. 2015, 42 (Suppl. 16), S158–S171. [Google Scholar] [CrossRef]
- Heitz-MayfieldL, J.; Mombelli, A. The therapy of peri-implantitis: A systematic review. Int. J. Oral Maxillofac. Implants 2014, 29, 325–345. [Google Scholar] [CrossRef]
- Albrektsson, T.; Zarb, G.; Worthington, P.; Eriksson, A.R. The long-term efficacy of currently used dental implants: A review and proposed criteria of success. Int. J. Oral Maxillofac. Implants 1986, 2, 11–25. [Google Scholar]
- Pjetursson, B.E.; Valente, N.A.; Strasding, M.; Zwahlen, M.; Liu, S.; Sailer, I. A systematic review of the survival and complication rates of zirconia-ceramic and metal-ceramic single crowns. Clin. Oral Implants Res. 2018, 29 (Suppl. 16), 199–214. [Google Scholar] [CrossRef]
- Zhuang, L.F.; Watt, R.M.; Mattheos, N.; Si, M.S.; Lai, H.C.; Lang, N.P. Periodontal and peri-implant microbiota in patients with healthy and inflamed periodontal and peri-implant tissues. Clin. Oral Implants Res. 2016, 27, 13–21. [Google Scholar] [CrossRef]
- Dreyer, H.; Grischke, J.; Tiede, C.; Eberhard, J.; Schweitzer, A.; Toikkanen, S.E.; Glöckner, S.; Krause, G.; Stiesch, M. Epidemiology and risk factors of peri-implantitis: A systematic review. J. Periodontal Res. 2018, 53, 657–681. [Google Scholar] [CrossRef]
- Koldsland, O.C.; Scheie, A.A.; Aass, A.M. Prevalence of peri-implantitis related to severity of the disease with different degrees of bone loss. J. Periodontol. 2010, 81, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Renvert, S.; Hirooka, H.; Polyzois, I.; Kelekis Cholakis, A.; Wang, H.-L. Working Group 3. Diagnosis and non-surgical treatment of peri-implant diseases and maintenance care of patients with dental implants—Consensus report of working group 3. Int. Dent. J. 2019, 69, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Wilson, T.G. The Positive Relationship Between Excess Cement and Peri-Implant Disease: A Prospective Clinical Endoscopic Study. J. Periodontol. 2009, 80, 1388–1392. [Google Scholar] [CrossRef] [PubMed]
- Korsch, M.; Marten, S.; Dotisch, A.; Jauregui, R.; Pieper, D.; Obst, U. Effect of dental cements on peri-implant microbial community: Comparison of the microbial communities inhabiting the peri-implant tissue when using different luting cements. Clin. Oral Implant Res. 2016, 27, e161–e166. [Google Scholar] [CrossRef]
- Javed, F.; Romanos, G.E. Chronic hyperglycemia as a risk factor in implant therapy. Periodontology 2000 2019, 81, 57–63. [Google Scholar] [CrossRef]
- Javed, F.; Rahman, I.; Romanos, G.E. Tobacco-product usage as a risk factor for dental implants. Periodontology 2000 2019, 81, 48–56. [Google Scholar] [CrossRef]
- Lin, C.Y.; Chen, Z.; Pan, W.L.; Wang, H.-L. The effect of supportive care in preventing peri-implant diseases and implant loss: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2019, 30, 714–724. [Google Scholar] [CrossRef]
- Monje, A.; Wang, H.-L.; Nart, J. Association of preventive maintenance therapy compliance and peri-implant diseases: A cross-sectional study. J. Periodontol. 2017, 88, 1030–1041. [Google Scholar] [CrossRef]
- Roccuzzo, M.; Layton, D.M.; Roccuzzo, A.; Heitz-Mayfield, L.J. Clinical outcomes of peri-implantitis treatment and supportive care: A systematic review. Clin. Oral Implants Res. 2018, 29 (Suppl. 16), 331–350. [Google Scholar] [CrossRef]
- Rösing, C.K.; Fiorini, T.; Haas, A.N.; Muniz, F.W.M.G.; Oppermann, R.V.; Susin, C. The impact of maintenance on peri-implant health. Braz. Oral Res. 2019, 33 (Suppl. 1), e074. [Google Scholar]
- Del Fabbro, M.; Nevins, M.; Venturoli, D.; Weinstein, R.; Testori, T. Clinically oriented patient maintenance protocol: A clinical consensus of experts. Int. J. Periodontics Restor. Dent. 2018, 38, 281–288. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weinstein, T.; Clauser, T.; Del Fabbro, M.; Deflorian, M.; Parenti, A.; Taschieri, S.; Testori, T.; Francetti, L. Prevalence of Peri-Implantitis: A Multi-Centered Cross-Sectional Study on 248 Patients. Dent. J. 2020, 8, 80. https://doi.org/10.3390/dj8030080
Weinstein T, Clauser T, Del Fabbro M, Deflorian M, Parenti A, Taschieri S, Testori T, Francetti L. Prevalence of Peri-Implantitis: A Multi-Centered Cross-Sectional Study on 248 Patients. Dentistry Journal. 2020; 8(3):80. https://doi.org/10.3390/dj8030080
Chicago/Turabian StyleWeinstein, Tommaso, Tommaso Clauser, Massimo Del Fabbro, Matteo Deflorian, Andrea Parenti, Silvio Taschieri, Tiziano Testori, and Luca Francetti. 2020. "Prevalence of Peri-Implantitis: A Multi-Centered Cross-Sectional Study on 248 Patients" Dentistry Journal 8, no. 3: 80. https://doi.org/10.3390/dj8030080
APA StyleWeinstein, T., Clauser, T., Del Fabbro, M., Deflorian, M., Parenti, A., Taschieri, S., Testori, T., & Francetti, L. (2020). Prevalence of Peri-Implantitis: A Multi-Centered Cross-Sectional Study on 248 Patients. Dentistry Journal, 8(3), 80. https://doi.org/10.3390/dj8030080






