Osseous Healing in Surgically Prepared Bone Defects Using Different Grafting Materials: An Experimental Study in Pigs
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
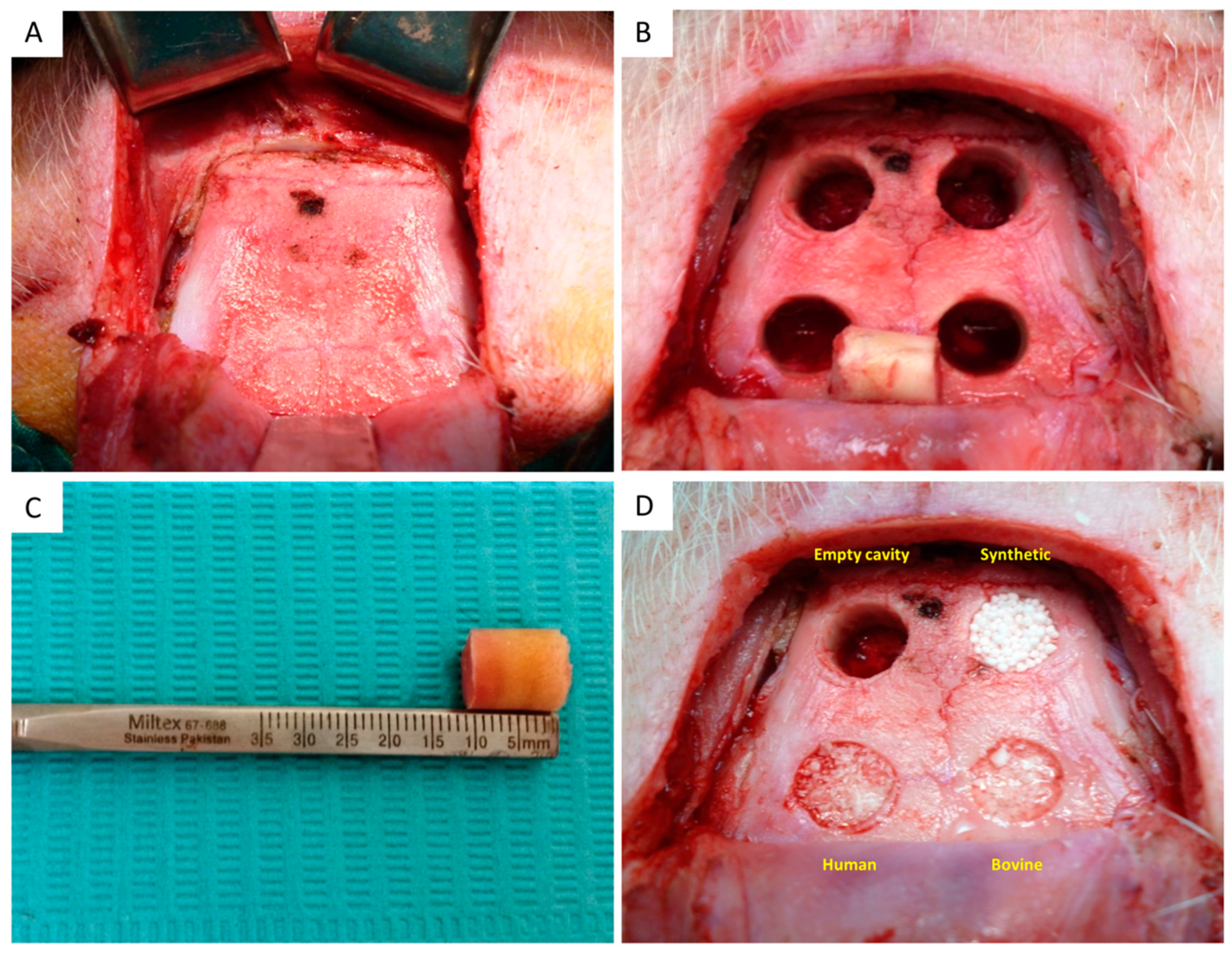
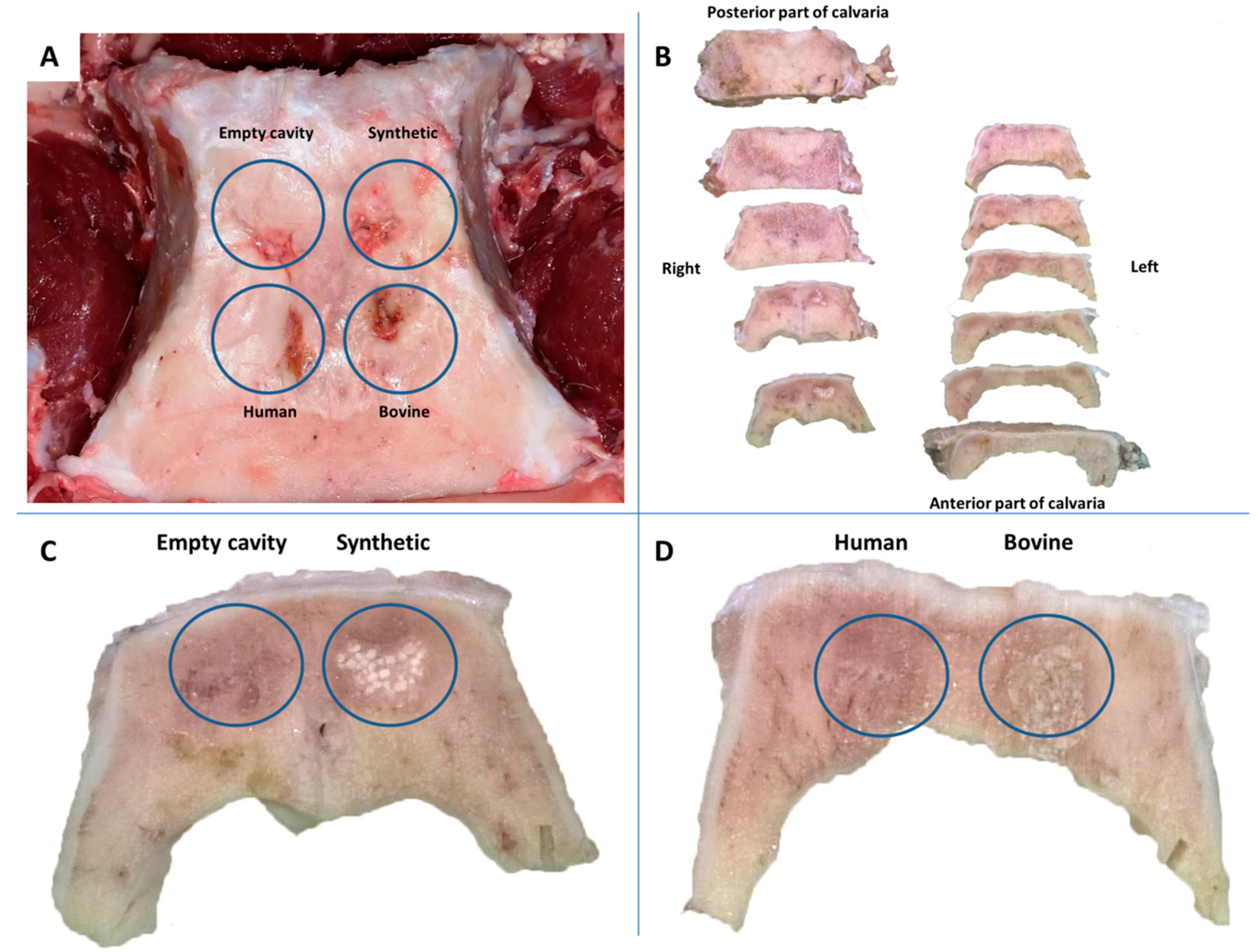
2.2. Surgical Procedure and Experimental Design
2.3. Sacrifice of Animals
2.4. Histologic Analysis
2.5. Histomorphometric Analysis
2.6. Statistical Analysis
3. Results
3.1. Overall
3.2. Histology
3.3. Histomorphometry
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Chiapasco, M.; Casentini, P.; Zaniboni, M. Bone augmentation procedures in implant dentistry. Int. J. Oral Maxillofac. Implants 2009, 24, 237–259. [Google Scholar]
- Damien, C.J.; Parsons, J.R. Bone graft and bone graft substitutes: A review of current technology and applications. J. Appl. Biomater. 1991, 2, 187–208. [Google Scholar] [CrossRef]
- Wang, W.; Yeung, K.W. Bone grafts and biomaterials substitutes for bone defect repair: A review. Bioact. Mater. 2017, 2, 224–247. [Google Scholar] [CrossRef]
- Buser, D.; Dula, K.; Hess, D.; Hirt, H.P.; Belser, U.C. Localized ridge augmentation with autografts and barrier membranes. Periodontol. 2000 1999, 19, 151–163. [Google Scholar] [CrossRef]
- Misch, C.M. Autogenous Bone: Is It Still the Gold Standard? Implant Dent. 2010, 19, 361. [Google Scholar] [CrossRef]
- Titsinides, S.; Agrogiannis, G.; Karatzas, T. Bone grafting materials in dentoalveolar reconstruction: A comprehensive review. Jpn. Dent. Sci. Rev. 2019, 55, 26–32. [Google Scholar] [CrossRef]
- Owen, G.R.; Dard, M.; Larjava, H. Hydoxyapatite/beta-tricalcium phosphate biphasic ceramics as regenerative material for the repair of complex bone defects. J. Biomed. Mater. Res. B Appl. Biomater. 2018, 106, 2493–2512. [Google Scholar] [CrossRef]
- Yuan, H.; Van Den Doel, M.; Li, S.; Van Blitterswijk, C.A.; De Groot, K.; De Bruijn, J.D. A comparison of the osteoinductive potential of two calcium phosphate ceramics implanted intramuscularly in goats. J. Mater. Sci. Mater. Med. 2002, 13, 1271–1275. [Google Scholar] [CrossRef]
- Moore, W.R.; Graves, S.E.; Bain, G.I. Synthetic bone graft substitutes. ANZ J. Surg. 2001, 71, 354–361. [Google Scholar] [CrossRef]
- Tovar, N.; Jimbo, R.; Gangolli, R.; Perez, L.; Manne, L.; Yoo, D.; Lorenzoni, F.; Witek, L.; Coelho, P.G. Evaluation of bone response to various anorganic bovine bone xenografts: An experimental calvaria defect study. Int. J. Oral Maxillofac. Surg. 2014, 43, 251–260. [Google Scholar] [CrossRef]
- Wiltfang, J.; Kloss, F.R.; Kessler, P.; Nkenke, E.; Schultze-Mosgau, S.; Zimmermann, R.; Schlegel, K.A. Effects of platelet-rich plasma on bone healing in combination with autogenous bone and bone substitutes in critical-size defects. An animal experiment. Clin. Oral Implants Res. 2004, 15, 187–193. [Google Scholar] [CrossRef]
- Li, Y.; Chen, S.K.; Li, L.; Qin, L.; Wang, X.L.; Lai, Y.X. Bone defect animal models for testing efficacy of bone substitute biomaterials. J. Orthop. Transl. 2015, 16, 95–104. [Google Scholar] [CrossRef]
- Schmitz, J.P.; Hollinger, J.O. The critical size defect as an experimental model for craniomandibulofacial nonunions. Clin. Orthop. Relat. Res. 1986, 205, 299–308. [Google Scholar] [CrossRef]
- Kahnberg, K.E. Restoration of mandibular jaw defects in the rabbit by subperiosteally implanted Teflon® mantle leaf. Int. J. Oral Maxillofac. Surg. 1979, 8, 449–456. [Google Scholar] [CrossRef]
- Schlegel, K.A.; Lang, F.J.; Donath, K.; Kulow, J.T.; Wiltfang, J. The monocortical critical size bone defect as an alternative experimental model in testing bone substitute materials. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 102, 7–13. [Google Scholar] [CrossRef]
- Leventis, M.; Agrogiannis, G.; Fairbairn, P.; Vasiliadis, O.; Papavasileiou, D.; Theodoropoulou, E.; Horowitz, R.; Kalyvas, D. Evaluation of an In Situ Hardening β-Tricalcium Phosphate Graft Material for Alveolar Ridge Preservation. A Histomorphometric Animal Study in Pigs. Dent. J. 2018, 6, 27. [Google Scholar] [CrossRef]
- Leventis, M.; Fairbairn, P.; Mangham, C.; Galanos, A.; Vasiliadis, O.; Papavasileiou, D. Bone Healing in Rabbit Calvaria Defects Using a Synthetic Bone Substitute: A Histological and Micro-CT Comparative Study. Materials 2018, 17, 2004. [Google Scholar] [CrossRef]
- Kakar, A.; Rao, B.H.S.; Hegde, S.; Deshpande, N.; Lindner, A.; Nagursky, H.; Patney, A.; Mahajan, H. Ridge preservation using an in situ hardening biphasic calcium phosphate (β-TCP/HA) bone graft substitute-a clinical, radiological, and histological study. Int. J. Implant Dent. 2017, 3, 25. [Google Scholar] [CrossRef]
- Jambhekar, S.; Kernen, F.; Bidra, A.S. Clinical and histologic outcomes of socket grafting after flapless tooth extraction: A systematic review of randomized controlled clinical trials. J. Prosthet. Dent. 2015, 113, 371–382. [Google Scholar] [CrossRef]
- Leventis, M.D.; Fairbairn, P.; Dontas, I.; Faratzis, G.; Valavanis, K.D.; Khaldi, L.; Kostakis, G.; Eleftheriadis, E. Biological response to β-tricalcium phosphate/calcium sulfate synthetic graft material: An experimental study. Implant Dent. 2014, 23, 37–43. [Google Scholar] [CrossRef]
- Yang, H.L.; Zhu, X.S.; Chen, L.; Chen, C.M.; Mangham, D.C.; Coulton, L.A.; Aiken, S.S. Bone healing response to a synthetic calcium sulfate/β-tricalcium phosphate graft material in a sheep vertebral body defect model. J. Biomed. Mater. Res. B Appl. Biomater. 2012, 100, 1911–1921. [Google Scholar] [CrossRef]
- Eleftheriadis, E.; Leventis, M.D.; Tosios, K.I.; Faratzis, G.; Titsinidis, S.; Eleftheriadi, I.; Dontas, I. Osteogenic activity of β-tricalcium phosphate in a hydroxyl sulphate matrix and demineralized bone matrix: A histological study in rabbit mandible. J. Oral Sci. 2010, 52, 377–384. [Google Scholar] [CrossRef]
- Podaropoulos, L.; Veis, A.A.; Papadimitriou, S.; Alexandridis, C.; Kalyvas, D. Bone regeneration using beta-tricalcium phosphate in a calcium sulfate matrix. J. Oral Implantol. 2009, 35, 28–36. [Google Scholar] [CrossRef]
- Hong, J.Y.; Lee, J.S.; Pang, E.K.; Jung, U.W.; Choi, S.H.; Kim, C.K. Impact of different synthetic bone fillers on healing of extraction sockets: An experimental study in dogs. Clin. Oral Implants Res. 2014, 25, e30–e37. [Google Scholar] [CrossRef]
- Jensen, S.S.; Broggini, N.; Hjørting-Hansen, E.; Schenk, R.; Buser, D. Bone healing and graft resorption of autograft, anorganic bovine bone and beta-tricalcium phosphate. A histologic and histomorphometric study in the mandibles of minipigs. Clin. Oral Implants Res. 2006, 17, 237–243. [Google Scholar] [CrossRef]
- Stavropoulos, A.; Kostopoulos, L.; Nyengaard, J.R.; Karring, T. Deproteinized bovine bone (Bio-Oss) and bioactive glass (Biogran) arrest bone formation when used as an adjunct to guided tissue regeneration (GTR): An experimental study in the rat. J. Clin. Periodontol. 2003, 30, 636–643. [Google Scholar] [CrossRef]
- Carmagnola, D.; Adriaens, P.; Berglundh, T. Healing of human extraction sockets filled with Bio-Oss. Clin. Oral Implants Res. 2003, 14, 137–143. [Google Scholar] [CrossRef]
- Baker-LePain, J.C.; Nakamura, M.C.; Lane, N.E. Effects of inflammation on bone: An update. Curr. Opin. Rheumatol. 2011, 23, 389–395. [Google Scholar] [CrossRef]
- Lacey, D.C.; Simmons, P.J.; Graves, S.E.; Hamilton, J.A. Proinflammatory cytokines inhibit osteogenic differentiation from stem cells: Implications for bone repair during inflammation. Osteoarthr. Cartil. 2009, 17, 735–742. [Google Scholar] [CrossRef]
- Chan, H.L.; Lin, G.H.; Fu, J.H.; Wang, H.L. Alterations in bone quality after socket preservation with grafting materials: A systematic review. Int. J. Oral Maxillofac. Implants 2013, 28, 710–720. [Google Scholar] [CrossRef]
- Zerbo, I.R.; Zijderveld, S.A.; de Boer, A.; Bronckers, A.L.; de Lange, G.; ten Bruggenkate, C.M.; Burger, E.H. Histomorphometry of human sinus floor augmentation using a porous β-tricalcium phosphate: A prospective study. Clin. Oral Implants Res. 2004, 15, 724–732. [Google Scholar] [CrossRef]
- Artzi, Z.; Weinreb, M.; Givol, N.; Rohrer, M.D.; Nemcovsky, C.E.; Prasad, H.S.; Tal, H. Biomaterial Resorption Rate and Healing Site Morphology of Inorganic Bovine Bone and β-Tricalcium Phosphate in the Canine: A 24-month Longitudinal Histologic Study and Morphometric Analysis. Int. J. Oral Maxillofac. Implants 2004, 19, 357–368. [Google Scholar]
- Mordenfeld, A.; Hallman, M.; Johansson, C.B.; Albrektsson, T. Histological and histomorphometrical analyses of biopsies harvested 11 years after maxillary sinus floor augmentation with deproteinized bovine and autogenous bone. Clin. Oral Implants Res. 2010, 21, 961–970. [Google Scholar] [CrossRef]
- Xu, X.; Sohn, D.S.; Kim, H.G.; Lee, S.J.; Moon, Y.S. Comparative histomorphometric analysis of maxillary sinus augmentation with deproteinized bovine bone and demineralized particulate human tooth graft: An experimental study in rabbits. Implant Dent. 2018, 27, 324–331. [Google Scholar] [CrossRef]
- Stevenson, S.; Horowitz, M. The response to bone allografts. J. Bone Joint Surg. Am. 1992, 74, 939–950. [Google Scholar] [CrossRef]
- Khan, S.N.; Cammisa, F.P., Jr.; Sandhu, H.S.; Diwan, A.D.; Girardi, F.P.; Lane, J.M. The biology of bone grafting. J. Am. Acad. Orthop. Surg. 2005, 13, 77–86. [Google Scholar] [CrossRef]
- Steiner, G. After Mineralization, Mineralized Freeze-Dried Bone Allograft Particles Are Exfoliated but not Resorbed. 2019. Available online: https://www.preprints.org/manuscript/201904.0271/v1 (accessed on 10 November 2019).
- Laurito, D.; Lollobrigida, M.; Gianno, F.; Bosco, S.; Lamazza, L.; De Biase, A. Alveolar ridge preservation with nc-HA and d-PTFE membrane: A clinical, histologic, and histomorphometric study. Int. J. Periodont. Restor. Dent. 2017, 37, 283–290. [Google Scholar] [CrossRef] [PubMed]

| Graft | Characteristics | Granule Size (mm) |
|---|---|---|
| Bio-Oss | Bovine, deproteinized bone mineral | 1–2 |
| Calc-i-oss | Synthetic, phase-pure beta-tricalcium phosphate | 1–1.6 |
| Demokritos | Human, freeze-dried, mineralized, and lyophilized cancellous bone allograft | 1–2 |
| 8 Weeks | 12 Weeks | |||
| Group | Mean | SD | Mean | SD |
| Control | 34.81 | 7.98 | 44.80 | 0.60 |
| Synthetic | 34.11 | 20.21 | 47.25 | 1.12 |
| Bovine | 32.08 | 11.95 | 39.14 | 1.10 |
| Human | 29.20 | 9.55 | 35.08 | 0.93 |
| Group comparison | p value | |||
| 8 weeks | 12 weeks | |||
| Control Synthetic | 0.858 | 0.005 | ||
| Control Human | 0.179 | 0.001 | ||
| Control Bovine | 0.541 | 0.001 | ||
| Synthetic Bovine | 0.693 | 0.002 | ||
| Synthetic Human | 0.315 | 0.001 | ||
| Bovine Human | 0.583 | 0.001 | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Titsinides, S.; Karatzas, T.; Perrea, D.; Eleftheriadis, E.; Podaropoulos, L.; Kalyvas, D.; Katopodis, C.; Agrogiannis, G. Osseous Healing in Surgically Prepared Bone Defects Using Different Grafting Materials: An Experimental Study in Pigs. Dent. J. 2020, 8, 7. https://doi.org/10.3390/dj8010007
Titsinides S, Karatzas T, Perrea D, Eleftheriadis E, Podaropoulos L, Kalyvas D, Katopodis C, Agrogiannis G. Osseous Healing in Surgically Prepared Bone Defects Using Different Grafting Materials: An Experimental Study in Pigs. Dentistry Journal. 2020; 8(1):7. https://doi.org/10.3390/dj8010007
Chicago/Turabian StyleTitsinides, Savvas, Theodore Karatzas, Despoina Perrea, Efstathios Eleftheriadis, Leonidas Podaropoulos, Demos Kalyvas, Christos Katopodis, and George Agrogiannis. 2020. "Osseous Healing in Surgically Prepared Bone Defects Using Different Grafting Materials: An Experimental Study in Pigs" Dentistry Journal 8, no. 1: 7. https://doi.org/10.3390/dj8010007
APA StyleTitsinides, S., Karatzas, T., Perrea, D., Eleftheriadis, E., Podaropoulos, L., Kalyvas, D., Katopodis, C., & Agrogiannis, G. (2020). Osseous Healing in Surgically Prepared Bone Defects Using Different Grafting Materials: An Experimental Study in Pigs. Dentistry Journal, 8(1), 7. https://doi.org/10.3390/dj8010007





