Adhesion of Two New Glass Fiber Post Systems Cemented with Self-Adhesive Resin Cements
Abstract
1. Introduction
2. Materials and Methods
2.1. Specimen Preparation
2.2. Cementation of Posts
- Group 1
- FiberSite™ Post system (MegaDental, Partanna, Italy);
- Group 2
- Cytec™ Blanco Post (Hahnenkratt, Königsbach-Stein, Germany).
2.3. Thermal Cycling (Artificial Ageing)
2.3.1. Bond Strength Test
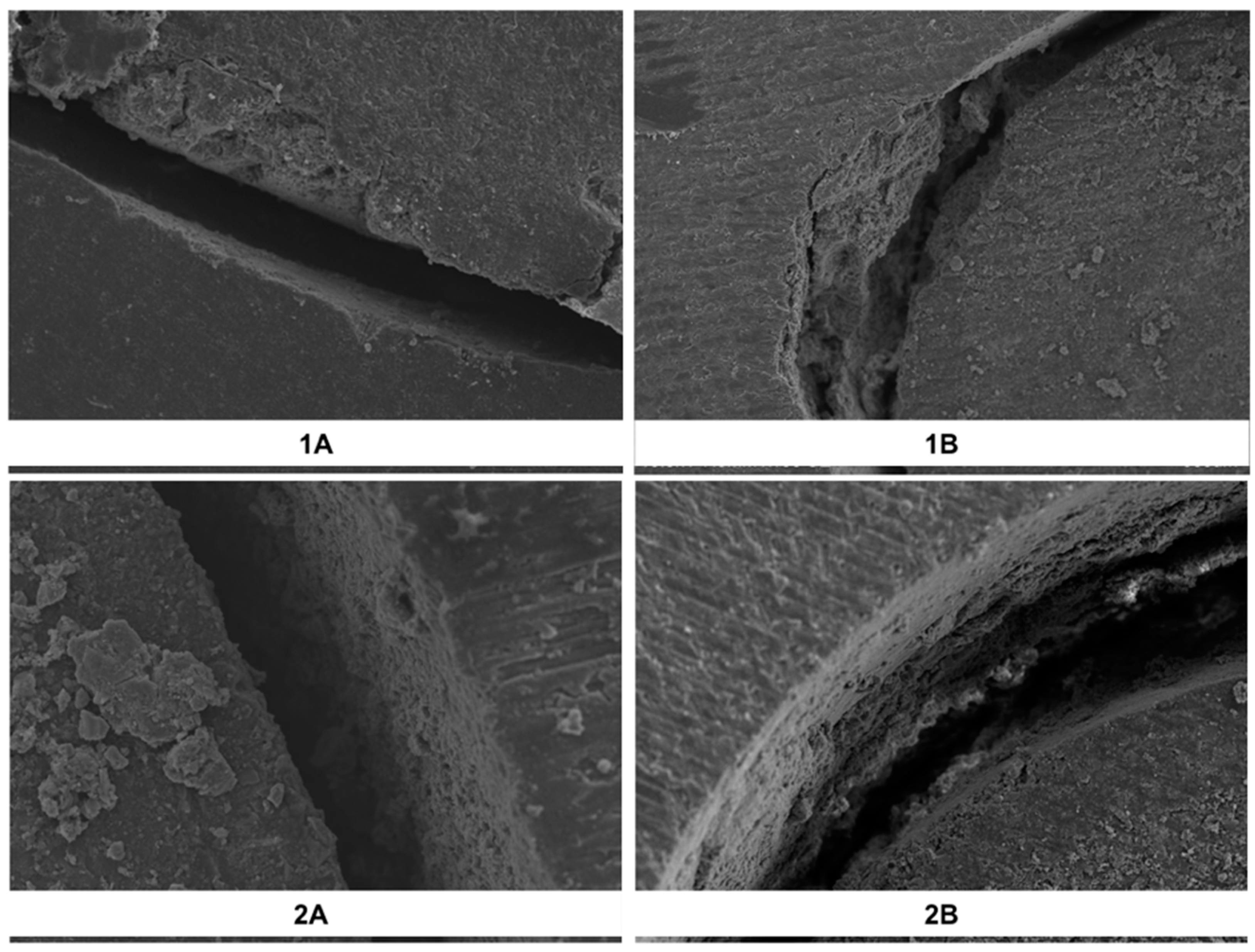
2.3.2. Failure Mode Analysis
2.3.3. Data Analysis
3. Results
3.1. Bond Strength
3.2. Failure Mode
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Katalinić, I.; Glockner, K.; Anić, I. Influence of several root canal disinfection methods on pushout bond strength of self-etch post and core systems. Int. Endod J. 2014, 47, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Matinlinna, J.P. E-glass Fiber Reinforced Composites in Dental Use. Silicon 2012, 4, 73–78. [Google Scholar] [CrossRef]
- Matinlinna, J.P.; Lung, C.Y.K.; Tsoi, J.K.H. Silane adhesion mechanism in dental applications and surface treatments: A review. Dent. Mater. 2018, 34, 13–28. [Google Scholar] [CrossRef] [PubMed]
- Lassila, L.V.; Tanner, J.; Le Bell, A.M.; Narva, K.; Vallittu, P.K. Flexural properties of fiber reinforced root canal posts. Dent. Mater. 2004, 20, 29–36. [Google Scholar] [CrossRef]
- Silva, R.A.; Coutinho, M.; Cardozo, P.I.; Silva, L.A.; Zorzatto, J.R. Conventional dual- cure versus self-adhesive resin cements in dentin bond integrity. J. Appl. Oral. Sci. 2011, 19, 355–362. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sarkis-Onofre, R.; Skupien, J.A.; Cenci, M.S.; Moraes, R.R.; Pereira-Cenci, T. The role of resin cement on bond strenght of glass-fiber posts luted into root canals: A systematic review and meta-analysis of in vitro studies. Oper. Dent. 2014, 39, 31–44. [Google Scholar] [CrossRef]
- Skupien, J.A.; Sarkis-Onofre, R.; Cenci, M.S.; Rotto de Moraes, R.R.; Pereira-Cenci, T. A syystematic review of factors associated with the retention of glass fiber posts. Braz. Oral Res. 2015, 29, 1–8. [Google Scholar]
- International Organization for Standardization ISO/TS 11405:2005. Dental Materials Testing of Adhesion to Tooth Structure; ISO: Geneva, Switzerland, 2005. [Google Scholar]
- Neelakantan, P.; Mohanraj, R.; Chua, E.; Belli, S. Impact of conditioning regimens and time on adhesion of a fiber post to root dentin using two resin cements. J. Adhes. Sci. Tech. 2015, 29, 337–346. [Google Scholar] [CrossRef]
- Sulaiman, T.A.; Abdulmajeed, A.A.; Altitinchi, A.; Ahmed, S.N.; Donovan, T.E. Mechanical properties of resin based cements with different dispensing and mixing methods. J. Prosthet. Dent. 2018, 119, 1007–1013. [Google Scholar] [CrossRef]
- Van Landuyt, K.L.; Snauwaert, J.; De Munck, J.; Peumans, M.; Yoshida, Y.; Poitevin, A.; Coutinho, E.; Suzuki, K.; Lambrechts, P.; Van Meerbeek, B. Systematic review of the chemical composition of contemporary dental adhesives. Biomaterials 2007, 28, 3757–3785. [Google Scholar] [CrossRef]
- Furuichi, T.; Takamizawa, T.; Tsujimoto, A.; Miyazaki, M. Mechanical properties and sliding-impact wear resistance of self-adhesive resin cements. Oper Dent. 2016, 41, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Sokolowski, G.; Szczesio, A.; Bociong, K.; Kaluzinska, K.; Lapinska, B.; Sokolowski, J.; Domarecka, M.; Lukomska-Szymanskom, M. Dental resin cements- the influence of water sorption on contraction stress change and hydrogcopic expansion. Dent. Mater. 2018, 11, 973. [Google Scholar]
- Ilie, N.; Simon, A. Effect of curing mode on the micro-mechanical properties of dual-cured self-adhesive resin cements. Clin. Oral Investig. 2012, 16, 505–512. [Google Scholar] [CrossRef] [PubMed]
- Munck, J.D.; Vargas, M.; Landuyt, K.U.; Hikita, K.; Lambrechts, P.; Van Meerbeek, B. Bonding of an auto-adhesive luting material to enamel and dentin. Dent. Mater. 2004, 20, 963–971. [Google Scholar] [PubMed]
- Monticelli, F.; Osorior, R.; Mazzitelli, C.; Toledano, M. Limited decalcification/diffusion of self-adhesive cements into dentin. J. Dent Res. 2008, 87, 974–979. [Google Scholar] [CrossRef] [PubMed]
- Rohr, N.; Fischer, J. Tooth surface treatment strategies for adhesiv cementation. J. Adv. Prosth. 2017, 9, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Junge, T.; Nicholls, J.I.; Phillips, K.M.; Libman, W.J. Load fatigue of compromised teeth: A comprasion of three luting cements. Int. J. Prosthodont. 1998, 11, 558–564. [Google Scholar]
- Mendoza, D.; Eakle, W.; Kahl, E.; Ho, R. Root reinforcement with a resin bonded preformed post. J. Prosthet. Dent. 1992, 78, 10–14. [Google Scholar] [CrossRef]
- Love, R.M.; Purton, D.G. Retention of posts with resin, glass ionomer and hybrid cements. J. Dent. 1998, 26, 599–602. [Google Scholar] [CrossRef]
- Ferrari, M.; Vichi, A.; Grandini, S.; Goracci, C. Efficacy of a self-curing adhesive-resin cement system on luting glass-fiber posts into root canals: An SEM investigation. Int. Endod. J. 2001, 14, 543–549. [Google Scholar]
- Peumans, M.; Munck, J.; Van Landuyt, K.L.; Poitevin, A.; Lambrechts, P.; Van Meerbeek, B. Eight-year clinical evaluation of a 2-step self-etch adhesive with and without selective enamel etching. Dent. Mater. 2010, 26, 1176–1184. [Google Scholar] [CrossRef]
- Serafino, C.; Gallina, G.; Cumbo, E.; Ferrari, M. Surface debris of canal walls after post space preparation in endodontically treated teeth: A scanning electron microscopic study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2004, 97, 381–387. [Google Scholar] [CrossRef]
- Gu, X.H.; Mao, C.; Liang, C.; Wang, H.M.; Kern, M. Does endodontic post space irrigation affect smear-layer removal and bonding effectiveness? Eur. J. Oral Sci. 2009, 117, 597–603. [Google Scholar] [CrossRef]
- Scotti, N.; Scansetti, M.; Rota, R. Active application of liquid etching agent improves adhesion of fibre posts to intraradicular dentine. Int. Endod. J. 2013, 46, 1039–1045. [Google Scholar] [CrossRef]
- Culhaoglu, A.K.; Ozcan, E.; Kilicarslan, M.A. Effect of boric acid versus conventional irrigation solutions on the bond strenght between fiber post and root dentin. J. Adhes. Dent. 2017, 19, 137–146. [Google Scholar]
- Scotti, N.; Bergantin, E.; Tempesta, R.; Turco, G. Influence of dentin pretreatment with synthetic hydroxyapatite application on the bond strength of fiber posts luted with 10-methacryloyloxydecyl dihydrogen phosphate-containing luting systems. Eur. J. Oral Sci. 2016, 124, 504–509. [Google Scholar] [CrossRef]
- Tay, F.R.; Loushine, R.J.; Lambrechts, P.; Weller, R.N.; Pashley, O.H. Geometric factors affecting denting bonding in root canals: A theoretical modelling aproach. J. Endod. 2005, 31, 584–589. [Google Scholar] [CrossRef]
- Jones, C.J.; Dickson, R.F.; Adam, T. Environmental fatique of reinforced plastics. J. Compos. 1983, 14, 288–293. [Google Scholar] [CrossRef]
- Kasturiarachchi, K.A.; Pritchard, G. Water absorption of glass/epoxy laminates under bending stresses. J. Compos. 1983, 14, 244–250. [Google Scholar] [CrossRef]
- Bouillaguet, S.; Schutt, A.; Alander, P. Hydrothermal and mechanical stresses degrade fiber-matrix interfacial bond strenght in dental fiber-reinforced composites. J. Biomed. Mater. Res. B Appl. Biomater. 2006, 76, 98–105. [Google Scholar] [CrossRef]
- Salz, U.; Bock, R. Testing adhesion of direct restoratives to dental hard tissue- A review. J. Adhes. Dent. 2010, 12, 343–371. [Google Scholar]
- Morresi, A.L.; D’Amario, M.; Capogreco, M.; Gatto, R.; Marzo, G.; D’Arcangelo, C.; Monaco, A. Thermal cycling for restorative materials: Does a standardized protocol exist in laboratory testing? A literature review. J. Mech. Behav. Biomed. Mater. 2014, 29, 295–308. [Google Scholar] [CrossRef]
- Drummond, J.L.; Bapna, M.S. Static and cyclic loadin of fiber-reinforced dental resin. Dent. Mater. 2003, 19, 226–231. [Google Scholar] [CrossRef]
- Meriç, G.; Ryter, E. Effect of thermal cycling on composites reinforced with two differently sized silica glass fibers. Dent. Mater. 2007, 23, 1157–1163. [Google Scholar] [CrossRef]
- Takahashi, H. Effect of calcium salt of 10-methacryloyloxydecyl dihydrogen phosphate produced on the bond durability of one-step self-etch adhesive. Dent. Mater. J. 2014, 33, 394–401. [Google Scholar] [CrossRef]
- Goracci, C.; Grandini, S.; Bossu, M.; Bossu, M.; Bertelli, E.; Ferrari, F. Laboratory assessment of the retentive potential of adhesive posts: A review. J. Dent. 2007, 37, 827–835. [Google Scholar] [CrossRef]
- Drummond, J.L.; Sakaguchi, R.L.; Racean, D.C.; Racean, D.C. Testing mode and surface treatment effects on dentin bonding. J. Biomed. Mater. Res. 1996, 34, 533–541. [Google Scholar] [CrossRef]
- Hunter, A.J.; Feiglin, B.; Williams, J.F. Effects of post placement on endodontically treated teeth. J. Prosthet. Dent. 1989, 62, 166–172. [Google Scholar] [CrossRef]
- Fernandes, A.S.; Dessai, G.S. Factors affecting the fracture resistance of post-core reconstructed teeth: A review. Int. J. Prosthodont. 2001, 14, 355–363. [Google Scholar]
- Adanir, N.; Belli, S. Evaluation of different post lengths’ effect on fracture resistance of a glass fiber post system. Eur. J. Dent. 2008, 2, 23–28. [Google Scholar]
- Cecchin, D.; Farina, A.P.; Guerreiro, C.A.; Carlini-Junior, B. Fracture resistance of roots prosthetically restored with intra-radicular posts of different lengths. J. Oral Rehabil. 2010, 37, 116–122. [Google Scholar] [CrossRef]
| Source | Type III Sum of Squares | df | Mean Square | F | Sig. |
|---|---|---|---|---|---|
| Group (the post system used) | 0.416 | 1 | 0.416 | 2.335 | 0.127 |
| Subgroup (the resin cements) | 4.565 | 1 | 4.565 | 25.645 | <0.001 |
| Group * Subgroup | 0.052 | 1 | 0.052 | 0.290 | 0.591 |
| Resin Cements | FiberSite™ | Cytec™ Blanco | Total |
|---|---|---|---|
| Maxcem™ Elite | 1.435 ± 0.426 | 1.391 ± 0.390 | 1.413 ± 0.408 |
| Panavia™ SA Plus | 1.234 ± 0.405 | 1.142 ± 0.463 | 1.188 ± 0.436 |
| Total | 1.335 ± 0.427 | 1.267 ± 0.445 | 1.301 ± 0.436 |
| Group | Adhesive | Mixed | Cohesive |
|---|---|---|---|
| 1: FiberSite Post system | |||
| Subgroup A | 85 | 0 | 15 |
| Subgroup B | 89.16 | 0.84 | 10 |
| 2: Cytec Blanco Post | |||
| Subgroup A | 83.34 | 0 | 16.66 |
| Subgroup B | 88.34 | 0 | 11.66 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Özlek, E.; Neelakantan, P.; Matinlinna, J.P.; Belli, S.; Ugur, M.; Kavut, I. Adhesion of Two New Glass Fiber Post Systems Cemented with Self-Adhesive Resin Cements. Dent. J. 2019, 7, 80. https://doi.org/10.3390/dj7030080
Özlek E, Neelakantan P, Matinlinna JP, Belli S, Ugur M, Kavut I. Adhesion of Two New Glass Fiber Post Systems Cemented with Self-Adhesive Resin Cements. Dentistry Journal. 2019; 7(3):80. https://doi.org/10.3390/dj7030080
Chicago/Turabian StyleÖzlek, Esin, Prasanna Neelakantan, Jukka Pekka Matinlinna, Sema Belli, Mehmet Ugur, and Idrıs Kavut. 2019. "Adhesion of Two New Glass Fiber Post Systems Cemented with Self-Adhesive Resin Cements" Dentistry Journal 7, no. 3: 80. https://doi.org/10.3390/dj7030080
APA StyleÖzlek, E., Neelakantan, P., Matinlinna, J. P., Belli, S., Ugur, M., & Kavut, I. (2019). Adhesion of Two New Glass Fiber Post Systems Cemented with Self-Adhesive Resin Cements. Dentistry Journal, 7(3), 80. https://doi.org/10.3390/dj7030080






