Dental Rehabilitation for Free Fibula Flap-Reconstructed Mandible with Scar Contracture: A Technical Note
Abstract
1. Introduction
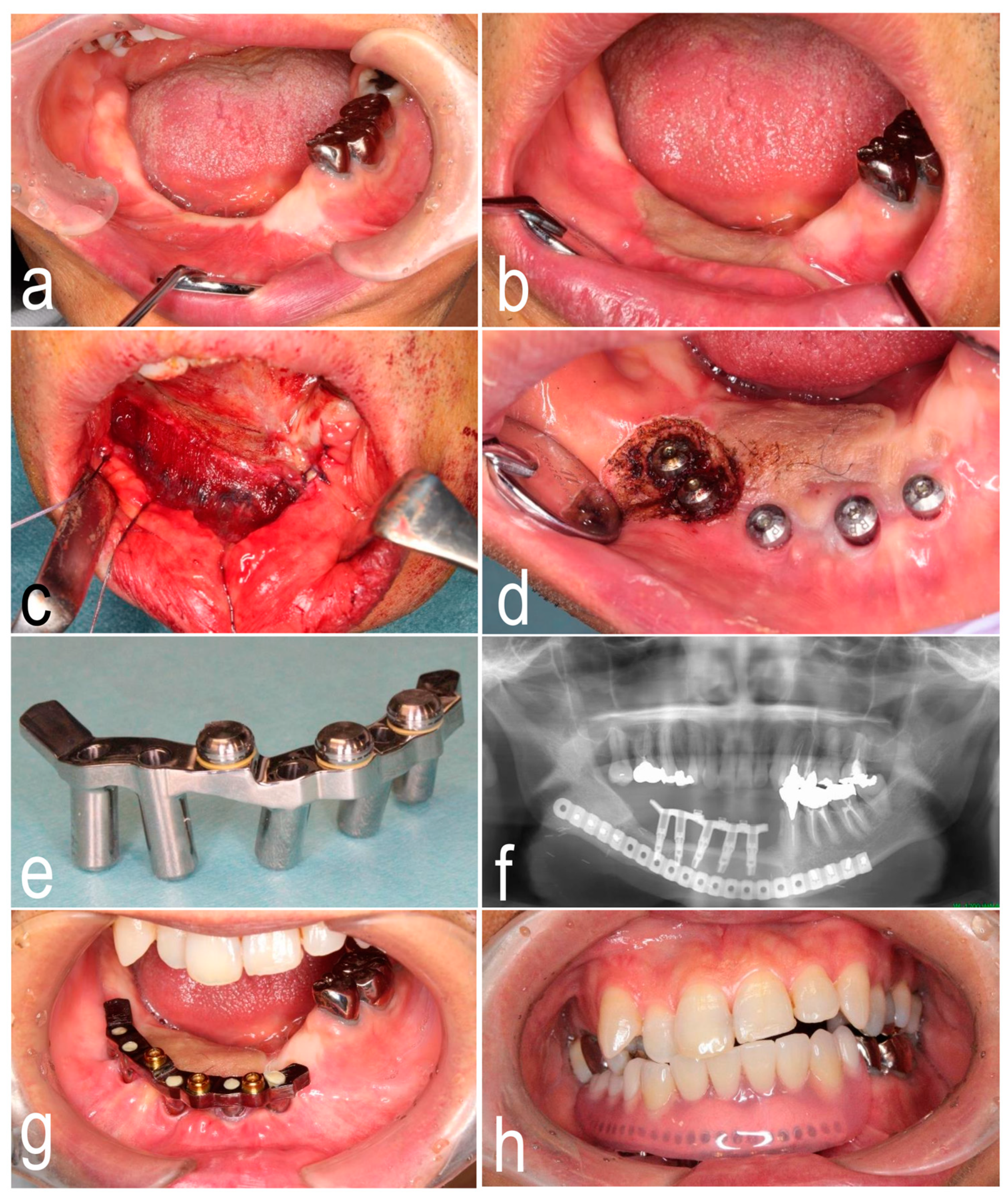
2. Case Presentation
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Burgess, M.; Leung, M.; Chellapah, A.; Clark, J.R.; Batstone, M.D. Osseointegrated implants into a variety of composite free flaps: A comparative analysis. Head Neck 2017, 39, 443–447. [Google Scholar] [CrossRef] [PubMed]
- Meloni, S.M.; Tallarico, M.; De Riu, G.; Pisano, M.; Deledda, A.; Lolli, F.M.; Massarelli, O.; Tullio, A. Guided implant surgery after free-flap reconstruction: Four-year results from a prospective clinical trial. J. Craniomaxillofac. Surg. 2015, 43, 1348–1355. [Google Scholar] [CrossRef] [PubMed]
- Patel, N.; Patel, D.; Kwok, J. New approach to improve the keratinised peri-implant soft tissues in patients with intraoral osteocutaneous reconstruction using a free flap. Br. J. Oral. Maxillofac. Surg. 2017, 55, 732–733. [Google Scholar] [CrossRef] [PubMed]
- Lauritano, D.; Grassi, R.; di Stasio, D.; Lucchese, A.; Petruzzi, M. Successful mandible rehabilitation of lower incisors with one-piece implants. J. Med. Case Rep. 2014, 8, 406. [Google Scholar] [CrossRef] [PubMed]
- Klesper, B.; Wahn, J.; Koebke, J. Comparisons of bone volumes and densities relating to osseointegrated implants in microvascularly reconstructed mandibles: A study of cadaveric radius and fibula bones. J. Craniomaxillofac. Surg. 2000, 28, 110–115. [Google Scholar] [CrossRef] [PubMed]
- Möhlhenrich, S.C.; Kniha, K.; Elvers, D.; Ayoub, N.; Goloborodko, E.; Hölzle, F.; Modabber, A. Intraosseous stability of dental implants in free revascularized fibula and iliac crest bone flaps. J. Craniomaxillofac. Surg. 2016, 44, 1935–1939. [Google Scholar] [CrossRef] [PubMed]
- Sarukawa, S.; Noguchi, T.; Oh-iwa, I.; Sunaga, A.; Uda, H.; Kusama, M.; Sugawara, Y. Bare bone graft with vascularised iliac crest for mandibular reconstruction. J. Craniomaxillofac. Surg. 2012, 40, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.M.; Wallace, C.G.; Tsai, C.Y.; Shen, Y.F.; Hsu, Y.M.; Wei, F.C. Dental implant outcome after primary implantation into double-barreled fibula osteoseptocutaneous free flap-reconstructed mandible. Plast. Reconstr. Surg. 2011, 128, 1220–1228. [Google Scholar] [CrossRef] [PubMed]
- Bassetti, R.G.; Stähli, A.; Bassetti, M.A.; Sculean, A. Soft tissue augmentation around osseointegrated and uncovered dental implants: A systematic review. Clin. Oral. Investig. 2017, 21, 53–70. [Google Scholar] [CrossRef] [PubMed]
- Fang, W.; Ma, W.; Ma, W.G.; Liu, B.L. A new submerged split-thickness skin graft technique to rebuild peri-implant keratinized soft tissue in composite flap reconstructed mandible or maxilla. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 2012, 113, 4–9. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, J.; Suzuki, H.; Murata, M.; Kakei, Y.; Ri, S.; Umeda, M.; Komori, T. Clinical evaluation of application of polyglycolic acid sheet and fibrin glue spray for partial glossectomy. J. Oral. Maxillofac. Surg. 2013, 71, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Yonezawa, H.; Yamada, S.; Yanamoto, S.; Yoshitomi, I.; Kawasaki, G.; Umeda, M. Effect of polyglycolic acid sheets with fibrin glue (MCFP technique) on the healing of wounds after partial resection of the border of the tongue in rabbits: A preliminary study. Br. J. Oral. Maxillofac. Surg. 2012, 50, 459–463. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.V.; Ebenezer, S.; Kämmerer, P.W.; Jacob, P.C.; Kuriakose, M.A.; Hedne, N.; Wagner, W.; Al-Nawas, B. Implants in free fibula flap supporting dental rehabilitation—Implant and peri-implant related outcomes of a randomized clinical trial. J. Craniomaxillofac. Surg. 2016, 44, 1849–1858. [Google Scholar] [CrossRef] [PubMed]
- Anne-Gaëlle, B.; Samuel, S.; Julie, B.; Renaud, L.; Pierre, B. Dental implant placement after mandibular reconstruction by microvascular free fibula flap: Current knowledge and remaining questions. Oral. Oncol. 2011, 47, 1099–1104. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.V.; Jacob, P.C.; Kuriakose, M.A. Sub-Periosteal Dissection with Denture-Guided Epithelial Regeneration: A Novel Method for peri-Implant Soft Tissue Management in Reconstructed Mandibles. J. Maxillofac. Oral. Surg. 2016, 15, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Kibe, T.; Koga, T.; Nishihara, K.; Fuchigami, T.; Yoshimura, T.; Taguchi, T.; Nakamura, N. Examination of the early wound healing process under different wound dressing conditions. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 2017, 123, 310–319. [Google Scholar] [CrossRef] [PubMed]
- Inokuchi, S.; Rokutanda, S.; Yanamoto, S.; Naruse, T.; Sakamoto, Y.; Umeda, M. Experimental study and clinical application of polyglycolic acid sheet with fibrin glue for oral soft tissue surgery. J. Oral. Maxillofac. Surg. Med. Pathol. 2017, 29, 295–300. [Google Scholar] [CrossRef]
- Rokutanda, S.; Yanamoto, S.; Yamada, S.; Naruse, T.; Inokuchi, S.; Umeda, M. Application of polyglycolic acid sheets and fibrin glue spray to bone surfaces during oral surgery: A case series. J. Oral. Maxillofac. Surg. 2015, 73, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Okuyama, K.; Yanamoto, S.; Naruse, T.; Sakamoto, Y.; Rokutanda, S.; Ohba, S.; Asahina, I.; Umeda, M. Clinical complications in the application of polyglycolic acid sheets with fibrin glue after resection of mucosal lesions in oral cavity. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 2018, 125, 541–546. [Google Scholar] [CrossRef]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akashi, M.; Matsumoto, K.; Takeda, D.; Yamashita, J.; Yatagai, N.; Hashikawa, K.; Komori, T. Dental Rehabilitation for Free Fibula Flap-Reconstructed Mandible with Scar Contracture: A Technical Note. Dent. J. 2019, 7, 65. https://doi.org/10.3390/dj7030065
Akashi M, Matsumoto K, Takeda D, Yamashita J, Yatagai N, Hashikawa K, Komori T. Dental Rehabilitation for Free Fibula Flap-Reconstructed Mandible with Scar Contracture: A Technical Note. Dentistry Journal. 2019; 7(3):65. https://doi.org/10.3390/dj7030065
Chicago/Turabian StyleAkashi, Masaya, Kousuke Matsumoto, Daisuke Takeda, Junya Yamashita, Nanae Yatagai, Kazunobu Hashikawa, and Takahide Komori. 2019. "Dental Rehabilitation for Free Fibula Flap-Reconstructed Mandible with Scar Contracture: A Technical Note" Dentistry Journal 7, no. 3: 65. https://doi.org/10.3390/dj7030065
APA StyleAkashi, M., Matsumoto, K., Takeda, D., Yamashita, J., Yatagai, N., Hashikawa, K., & Komori, T. (2019). Dental Rehabilitation for Free Fibula Flap-Reconstructed Mandible with Scar Contracture: A Technical Note. Dentistry Journal, 7(3), 65. https://doi.org/10.3390/dj7030065




