An In-Vitro Analysis of Microleakage of Self-Adhesive Fissure Sealant vs. Conventional and GIC Fissure Sealants
Abstract
:1. Introduction
- Marginal adaptation of a self-adhesive composite is similar to the conventional resin-based fissure sealant.
- Pre-treatment of enamel (etching) has no influence on microleakage of a self-adhesive composite.
- Marginal adaptation of a self-adhesive composite is similar to the thermo-light cured glass ionomer fissure sealant.
2. Materials and Methods
2.1. Sample Preparation
2.2. Specimen Aging
2.3. Assessment of Microleakage
2.4. Assessment of Sealant Retention and Microleakage (Dye Penetration)
- Complete retention.
- Partial loss.
- Complete loss.
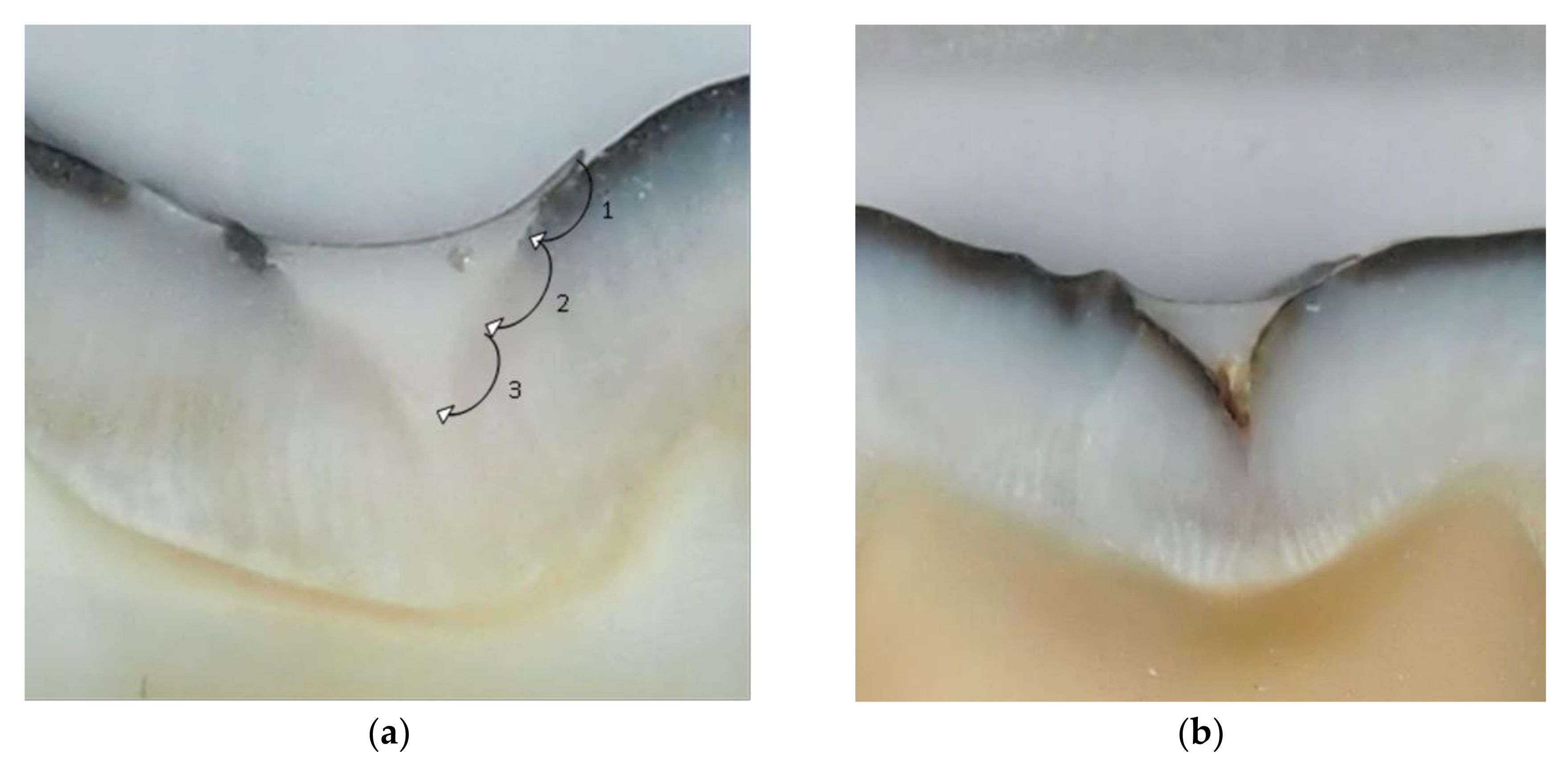
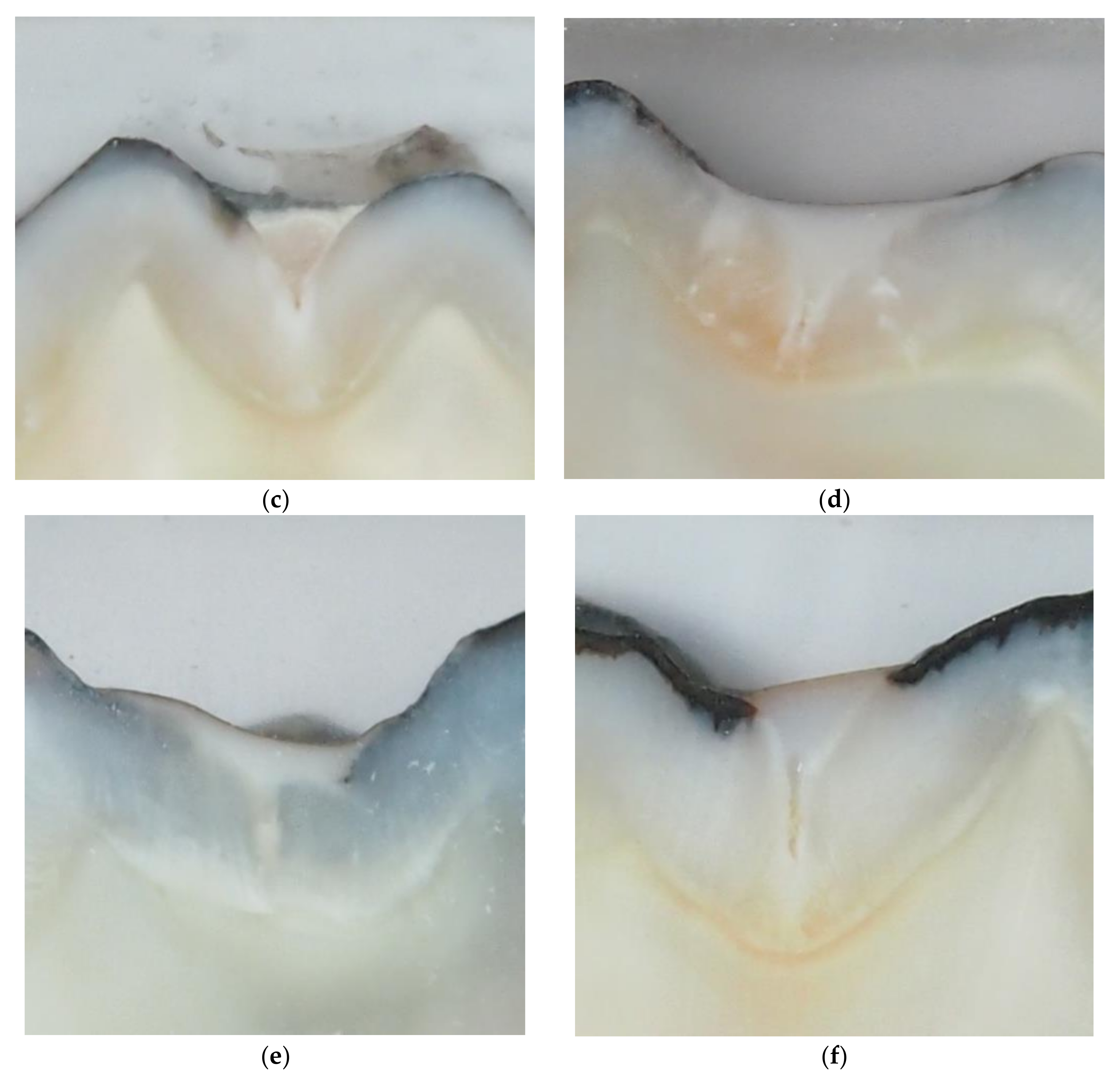
- 0-no evidence of dye penetration;
- 1-dye penetration of less than 1/3 from the margin of restoration;
- 2-dye penetration of more than 1/3 and less than 2/3 from the margin of restoration;
- 3-dye penetration of more than 2/3 from the margin of restoration.
2.5. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Ahovuo-Saloranta, A.; Forss, H.; Walsh, T.; Nordblad, A.; Mäkelä, M.; Worthington, H.V. Pit and fissure sealants for preventing dental decay in permanent teeth. Cochrane Database Syst. Rev. 2017, 7, CD001830. [Google Scholar] [CrossRef]
- Alirezaei, M.; Bagherian, A.; Sarraf Shirazi, A. Glass ionomer cements as fissure sealing materials: Yes or no?: A systematic review and meta-analysis. J. Am. Dent. Assoc. 2018, 149, 640–649. [Google Scholar] [CrossRef] [PubMed]
- Vichi, A.; Margvelashvili, M.; Goracci, C.; Papacchini, F.; Ferrari, M. Bonding and sealing ability of a new self-adhering flowable composite resin in class I restorations. Clin. Oral Investig. 2013, 17, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Unterbrink, G.L.; Liebenberg, W.H. Flowable resin composites as “filled adhesives”: Literature review and clinical recommendations. Quintessence Int. 1999, 30, 249–257. [Google Scholar] [PubMed]
- Attar, N.; Tam, L.E.; McComb, D. Flow, strength, stiffness and radiopacity of flowable resin composites. J. Can. Dent. Assoc. 2003, 69, 516–521. [Google Scholar]
- Bektas, O.O.; Eren, D.; Akin, E.G.; Akin, H. Evaluation of a self-adhering flowable composite in terms of micro-shear bond strength and microleakage. Acta Odontol. Scand. 2013, 271, 541–546. [Google Scholar] [CrossRef] [PubMed]
- Peterson, J.; Rizk, M.; Hoch, M.; Wiegand, A. Bonding performance of self-adhesive flowable composites to enamel, dentin and a nano-hybrid composite. Odontology 2018, 106, 171–180. [Google Scholar] [CrossRef]
- Rangappa, A.; Srinivasulu, J.; Rangaswamy, V.; Eregowda, S.; Lakshminarasimhaiah, V.; Lingareddy, U. Comparative evaluation of bond strength of self-adhering flowable composites to the dentin prepared with different burs: An in vitro study. J. Conserv. Dent. 2018, 21, 618–621. [Google Scholar] [CrossRef] [PubMed]
- Colombo, M.; Dagna, A.; Molino, D.; Poggio, C.; Maiolatesi, D.; Pietrocola, G. Bacterial adhesion on fissure sealants: Effects of exposure to acidic drink. J. Clin. Exp. Dent. 2018, 10, e574–e578. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Shi, Y.; Li, T.; Pan, Y.; Cui, Y.; Xia, W. Adhesive interfacial characteristics and the related bonding performance of four self-etching adhesives with different functional monomers applied to dentin. J. Dent. 2017, 62, 72–80. [Google Scholar] [CrossRef] [PubMed]
- Jokstad, A. Secondary caries and microleakage. Dent. Mater. 2016, 32, 11–25. [Google Scholar] [CrossRef] [PubMed]
- Gorseta, K.; Borzabadi-Farahani, A.; Moshaverinia, A.; Glavina, D.; Lynch, E. Effect of different thermo-light polymerization on flexural strength of two glass ionomer cements and a glass carbomer cement. J. Prosthet. Dent. 2017, 118, 102–107. [Google Scholar] [CrossRef] [PubMed]
- Gavic, L.; Gorseta, K.; Borzabadi-Farahani, A.; Tadin, A.; Glavina, D.; van Duinen, R.N.; Lynch, E. Influence of thermo-light curing with dental light-curing units on the microhardness of glass-Ionomer cements. Int. J. Periodontics Restor. Dent. 2016, 36, 425–430. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Cobb, E. A silver staining technique for investigating wear of restorative dental composites. J. Biomed. Mater. Res. 1981, 15, 343–348. [Google Scholar] [CrossRef]
- Oberholzer, T.G.; Du Preez, I.C.; Kidd, M. Effect of LED curing on the microleakage shear bond strength and surface hardness of a resin-based composite restoration. Biomaterials 2005, 26, 3981–3986. [Google Scholar] [CrossRef] [PubMed]
- Simonsen, R.J. Cost effectiveness of pit and fissure sealant at 10 years. Quintessence Int. 1989, 20, 75–82. [Google Scholar]
- Germán-Cecilia, C.; Gallego Reyes, S.M.; Péez Silva, A.; Serna Muñ, C.; Ortiz-Ruiz, A.J. Microleakage of conventional light-cure resin-based fissure sealant and resin-modified glass ionomer sealant after application of a fluoride varnish on demineralized enamel. PLoS ONE 2018, 13, e0208856. [Google Scholar]
- Rengo, C.; Goracci, C.; Juloski, J.; Chieffi, N.; Giovannetti, A.; Vichi, A.; Ferrari, M. Influence of phosphoric acid etching on microleakage of a self-etch adhesive and a self-adhering composite. Aust. Dent. J. 2012, 57, 220–226. [Google Scholar] [CrossRef]
- Eliades, A.; Birpou, E.; Eliades, T.; Eliades, G. Self-adhesive restoratives as pit and fissure sealants: A comparative laboratory study. Dent. Mater. 2013, 29, 752–762. [Google Scholar] [CrossRef] [PubMed]
- Celik, E.U.; Kucukyilmaz, E.; Savas, S. Effect of different surface pre-treatment methods on the microleakage of two different self-adhesive composites in Class V cavities. Eur. J. Paediatr. Dent. 2015, 16, 33–38. [Google Scholar]
- Pavan, S.; dos Santos, P.H.; Berger, S.; Bedran-Russo, A.K. The effect of dentin pretreatment on the microtensile bond strength of self-adhesive resin cements. J. Prosthet. Dent. 2010, 104, 258–264. [Google Scholar] [CrossRef]
- Radovic, I.; Monticelli, F.; Goracci, C.; Vulicevic, Z.R.; Ferrari, M. Self-adhesive resin cements: A literature review. J. Adhes. Dent. 2008, 10, 251–258. [Google Scholar] [PubMed]
- Gönülol, N.; Ertan Ertaş, E.; Yılmaz, A.; Çankaya, S. Effect of thermal aging on microleakage of current flowable composite resins. J. Dent. Sci. 2015, 10, 376–382. [Google Scholar] [CrossRef]
- Gorseta, K.; Glavina, D.; Skrinjaric, I. Influence of ultrasonic excitation and heat application on the microleakage of glass ionomer cements. Aust. Dent. J. 2012, 57, 453–457. [Google Scholar] [CrossRef] [PubMed]
- Ak, A.T.; Alpoz, A.R. Effect of saliva contamination on microleakage of three different pit and fissure sealants. Eur. J. Paediatr. Dent. 2010, 11, 93–96. [Google Scholar]
| Maximum Dye Penetration Score | G1, Helioseal F | G2, Constic | G3, Constic + Etch | G4, Equia + Varnish | G5, Equia + Thermo-Light Curing |
|---|---|---|---|---|---|
| 0 | 1 | 4 | 3 | 2 | 7 |
| 1 | 2 | 4 | 1 | 1 | 2 |
| 2 | 1 | 0 | 1 | 3 | 0 |
| 3 | 6 | 2 | 5 | 4 | 1 |
| Total | 10 | 10 | 10 | 10 | 10 |
| Helioseal F | Constic | Constic + Etching | Equia Fill + Varnish | Equia Fill + Heat (TLC) * | |
|---|---|---|---|---|---|
| Helioseal F | - | 0.037 | 0.505 | 0.489 | 0.004 |
| Constic | 0.037 | - | 0.473 | 0.116 | 0.206 |
| Constic + etching | 0.505 | 0.473 | - | 0.388 | 0.071 |
| Equia Fill + varnish | 0.489 | 0.116 | 0.387 | - | 0.016 |
| Equia Fill + heat | 0.004 | 0.206 | 0.071 | 0.016 | - |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gorseta, K.; Borzabadi-Farahani, A.; Vrazic, T.; Glavina, D. An In-Vitro Analysis of Microleakage of Self-Adhesive Fissure Sealant vs. Conventional and GIC Fissure Sealants. Dent. J. 2019, 7, 32. https://doi.org/10.3390/dj7020032
Gorseta K, Borzabadi-Farahani A, Vrazic T, Glavina D. An In-Vitro Analysis of Microleakage of Self-Adhesive Fissure Sealant vs. Conventional and GIC Fissure Sealants. Dentistry Journal. 2019; 7(2):32. https://doi.org/10.3390/dj7020032
Chicago/Turabian StyleGorseta, Kristina, Ali Borzabadi-Farahani, Tara Vrazic, and Domagoj Glavina. 2019. "An In-Vitro Analysis of Microleakage of Self-Adhesive Fissure Sealant vs. Conventional and GIC Fissure Sealants" Dentistry Journal 7, no. 2: 32. https://doi.org/10.3390/dj7020032
APA StyleGorseta, K., Borzabadi-Farahani, A., Vrazic, T., & Glavina, D. (2019). An In-Vitro Analysis of Microleakage of Self-Adhesive Fissure Sealant vs. Conventional and GIC Fissure Sealants. Dentistry Journal, 7(2), 32. https://doi.org/10.3390/dj7020032








