Characteristics of Patients Discontinuing Care
Abstract
1. Introduction
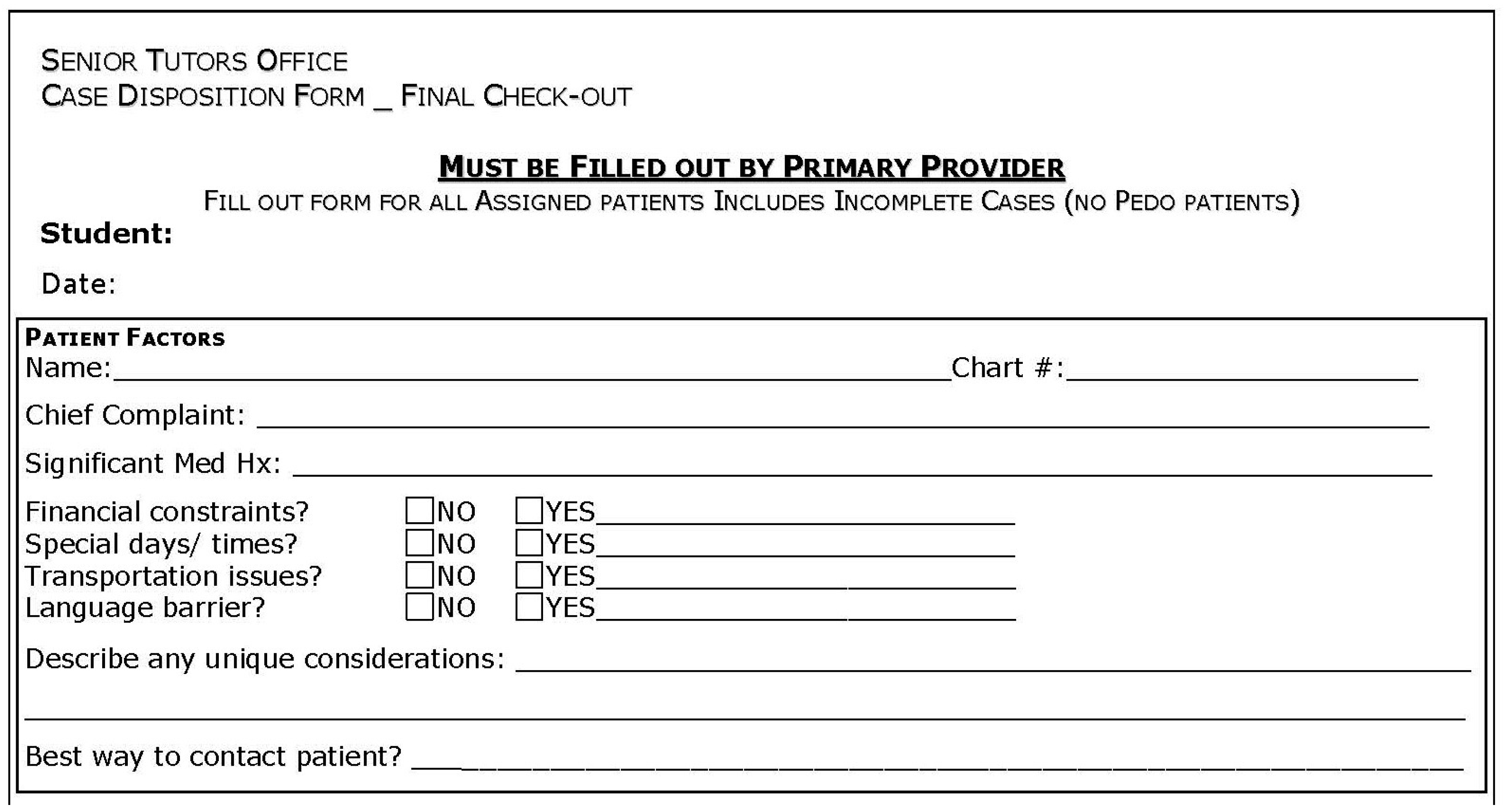
2. Methods
3. Results
4. Discussion
5. Conclusions
Author Statement
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- IOM (Institute of Medicine) and NRC (National Research Council). Improving Access to Oral Health Care for Vulnerable and Underserved Populations; The National Academies Press: Washington, DC, USA, 2011. [Google Scholar]
- Allareddy, V.; Rampa, S.; Lee, M.K.; Allareddy, V.; Nalliah, R.P. Hospital-based emergency department visits involving dental conditions: Profile and predictors of poor outcomes and resource utilization. J. Am. Dent. Assoc. 2014, 145, 331–337. [Google Scholar] [CrossRef] [PubMed]
- Singhal, A.; Caplan, D.J.; Jones, M.P.; Momany, E.T.; Kuthy, R.A.; Buresh, C.T.; Isman, R.; Damiano, P.C. Eliminating Medicaid adult dental coverage in California led to increased dental emergency visits and associated costs. Health Aff. (Millwood) 2015, 34, 749–756. [Google Scholar] [CrossRef] [PubMed]
- Jones, E.; Shi, L.; Hayashi, A.S.; Sharma, R.; Daly, C.; Ngo-Metzger, Q. Access to oral health care: The role of federally qualified health centers in addressing disparities and expanding access. Am. J. Public Health 2013, 103, 488–493. [Google Scholar] [CrossRef] [PubMed]
- Commission on Dental Accreditation. DDS/DMD Programs—US. Available online: http://www.ada.org/en/coda/find-a-program/search-dental-programs/dds-dmd-programs (accessed on 23 July 2015).
- Commission on Dental Accreditation. Accreditation Standards for Dental Education Programs; American Dental Association: Chicago, IL, USA, 2013. [Google Scholar]
- Tavernier, L.A.; Connor, P.D.; Gates, D.; Wan, J.Y. Does exposure to medically underserved areas during training influence eventual choice of practice location? Med. Educ. 2003, 37, 299–304. [Google Scholar] [CrossRef]
- Ebn Ahmady, A.; Pakkhesal, M.; Zafarmand, A.H.; Lando, H.A. Patient satisfaction surveys in dental school clinics: A review and comparison. J. Dent. Educ. 2015, 79, 388–393. [Google Scholar]
- Woods, C.D. Self-reported mental illness in a dental school clinic population. J. Dent. Educ. 2003, 67, 500–504. [Google Scholar] [PubMed]
- Ilgen, M.; Edwards, P.; Kleinberg, F.; Bohnert, A.S.; Barry, K.; Blow, F.C. The prevalence of substance use among patients at a dental school clinic in Michigan. J. Am. Dent. Assoc. 2012, 143, 890–896. [Google Scholar] [CrossRef]
- Corrigan, D.M.; Walker, M.P.; Liu, Y.; Mitchell, T.V. Factors influencing patients seeking oral health care in the oncology dental support clinic at an urban university dental school setting. Spec. Care Dent. 2014, 34, 106–113. [Google Scholar] [CrossRef]
- Kellogg, S.D.; Gobetti, J.P. Hypertension in a dental school patient population. J. Dent. Educ. 2004, 68, 956–964. [Google Scholar]
- Manski, R.J.; Macek, M.D.; Brown, E.; Carper, K.V.; Cohen, L.A.; Vargas, C. Dental service mix among working-age adults in the United States, 1999 and 2009. J. Public Health Dent. 2014, 74, 102–109. [Google Scholar] [CrossRef]
- Maxwell, N.I.; Shah, S.; Dooley, D.; Henshaw, M.; Bowen, D.J. Oral health among residents of publicly supported housing in Boston. J. Urban Health 2014, 91, 809–821. [Google Scholar] [CrossRef] [PubMed]
- John, D.A.; de Castro, A.B.; Duran, B.; Martin, D.P. Nativity and occupational class disparities in uninsurance and routine preventive care use among Asian Americans. J. Immigr. Minor. Health 2013, 15, 1011–1022. [Google Scholar] [CrossRef] [PubMed]
- Skillman, S.M.; Doescher, M.P.; Mouradian, W.E.; Brunson, D.K. The challenge to delivering oral health services in rural America. J. Public Health Dent. 2010, 70 (Suppl. 1), S49–S57. [Google Scholar] [CrossRef] [PubMed]
- Massachusetts Department of Public Health, Office of Oral Health. The Status of Oral Disease in Massachusetts: A Great Unmet Need 2009; Department of Public Health: Boston, MA, USA, 2009.
- Massachusetts Medicaid Policy Institute. The Governor’s FY 2015 Budget Proposal for MassHealth (Medicaid) and Health Reform Programs. March 2014. Available online: http://www.massbudget.org/reports/pdf/FY-2015_H2_Budget-Brief_FINAL.pdf (accessed on 4 September 2015).
- Yarbrough, C.; Nasseh, K.; Vujicic, M. Why Adults Forgo Dental Care: Evidence from a New National Survey; ADA Health Policy Institute: Chicago, IL, USA, November 2014. [Google Scholar]
- Seerig, L.M.; Nascimento, G.G.; Peres, M.A.; Horta, B.L.; Demarco, F.F. Tooth loss in adults and income: Systematic review and meta-analysis. J. Dent. 2015, 43, 1051–1059. [Google Scholar] [CrossRef]
- Nasseh, K.; Vujicic, M. Health reform in Massachusetts increased adult dental care use, particularly among the poor. Health Aff. (Millwood) 2013, 32, 1639–1645. [Google Scholar] [CrossRef]
- Sun, B.C.; Chi, D.L.; Schwarz, E.; Milgrom, P.; Yagapen, A.; Malveau, S.; Chen, Z.; Chan, B.; Danner, S.; Owen, E.; et al. Emergency department visits for nontraumatic dental problems: A mixed-methods study. Am. J. Public Health 2015, 105, 947–955. [Google Scholar] [CrossRef]
- Limited English Proficiency Individuals in the United States: Number, Share, Growth, and Linguistic Diversity; Migration Policy Institute: Washington, DC, USA, December 2011.
- Flores, G.; Tomany-Korman, S.C. The language spoken at home and disparities in medical and dental health, access to care, and use of services in US children. Pediatrics 2008, 121, e1703–e1714. [Google Scholar] [CrossRef]
- Simon, L.; Hum, L.; Nalliah, R.P. Access to Interpreter Services at United States Dental Schools. J. Dent. Educ. 2016, 80, 51–57. [Google Scholar]
- Migration Policy Institute National Center on Immigrant Integration Policy. MPI Limited English Proficient Census Data and MPI LEP Data Brief. Mass Legal Services Website. Available online: http://www.masslegalservices.org/content/mpi-limited-english-proficient-census-data-and-mpi-lep-data-brief (accessed on 9 July 2015).
- Isaac, C.; Behar-Horenstein, L.; Lee, B.; Catalanotto, F. Impact of reflective writing assignments on dental students’ views of cultural competence and diversity. J. Dent. Educ. 2015, 79, 312–321. [Google Scholar]
- Victoroff, K.Z.; Williams, K.A.; Lalumandier, J. Dental students’ reflections on their experiences with a diverse patient population. J. Dent. Educ. 2013, 77, 982–989. [Google Scholar]
- Alrqiq, H.M.; Scott, T.E.; Mascarenhas, A.K. Evaluating a Cultural Competency Curriculum: Changes in Dental Students’ Perceived Awareness, Knowledge, and Skills. J. Dent. Educ. 2015, 79, 1009–1015. [Google Scholar]
- Habibian, M.; Seirawan, H.; Mulligan, R. Dental students’ attitudes toward underserved populations across four years of dental school. J. Dent. Educ. 2011, 75, 1020–1029. [Google Scholar] [PubMed]
- Hewlett, E.R.; Davidson, P.L.; Nakazono, T.T.; Baumeister, S.E.; Carreon, D.C.; Freed, J.R. Effect of school environment on dental students’ perceptions of cultural competency curricula and preparedness to care for diverse populations. J. Dent. Educ. 2007, 71, 810–818. [Google Scholar]
- Holyfield, L.J.; Miller, B.H. A tool for assessing cultural competence training in dental education. J. Dent. Educ. 2013, 77, 990–997. [Google Scholar]
- Itaya, L.E.; Glassman, P.; Gregorczyk, S.; Bailit, H.L. Dental school patients with limited English proficiency: The California experience. J. Dent. Educ. 2009, 73, 1055–1064. [Google Scholar] [PubMed]
- Nápoles, A.M.; Santoyo-Olsson, J.; Karliner, L.S.; O’Brien, H.; Gregorich, S.E.; Pérez-Stable, E.J. Clinician ratings of interpreter mediated visits in underserved primary care settings with ad hoc, in-person professional, and video conferencing modes. J. Health Care Poor Underserved 2010, 21, 301–317. [Google Scholar] [CrossRef] [PubMed]
- Flores, G. The impact of medical interpreter services on the quality of health care: A systematic review. Med. Care Res. Rev. 2005, 62, 255–299. [Google Scholar] [CrossRef] [PubMed]
- Okunseri, C.; Bajorunaite, R.; Mehta, J.; Hodgson, B.; Iacopino, A.M. Factors associated with receipt of preventive dental treatment procedures among adult patients at a dental training school in Wisconsin, 2001–2002. Gend. Med. 2009, 6, 272–276. [Google Scholar] [CrossRef] [PubMed]
- Nowak, A.J.; Casamassimo, P.S. The dental home: A primary care oral health concept. J. Am. Dent. Assoc. 2002, 133, 93–98. [Google Scholar] [CrossRef]
- Adibi, S.S.; Chaluparambil, J.; Chambers, S.K.; Estes, K.; Valenza, J.A.; Walji, M.F. Assessing the delivery of comprehensive care at a dental school. Tex. Dent. J. 2012, 129, 1267–1275. [Google Scholar]
- Patrick, D.; Polanowicz, J.; Bartlett, C. Health Professions Data Series: Dentist 2012; Executive Office of Health and Human Services Massachusetts Department of Public Health: Boston, MA, USA, November 2014.
- Wu, B.; Hybels, C.; Liang, J.; Landerman, L.; Plassman, B. Social stratification and tooth loss among middle-aged and older Americans from 1988 to 2004. Community Dent. Oral Epidemiol. 2014, 42, 495–502. [Google Scholar] [CrossRef] [PubMed]
| Sample | Number (%) | Continuing Care | Not Continuing Care | p Value |
|---|---|---|---|---|
| Total sample size | 1894 | 1391 | 503 | |
| Patients with transportation barriers | 118 (6.23%) | 74 (5.3%) | 44 (8.7%) | 0.006 * |
| Patients with time limitations | 290 (15.3%) | 220 (15.8%) | 70 (13.9%) | 0.31 |
| Patients with linguistic barriers | 151 (7.97%) | 85 (6.1%) | 65 (12.9%) | <0.001 * |
| Patients with financial barriers | 570 (30.1%) | 348 (25%) | 222 (44.1%) | <0.001 * |
| Language | Number (%) |
|---|---|
| Total patients with limited English proficiency | 151 |
| Spanish | 65 (43.05) |
| Portuguese | 34 (22.52) |
| Russian | 5 (3.31) |
| Mandarin | 4 (2.65) |
| Haitian Kreyol | 4 (2.65) |
| Hindi | 2 (1.32) |
| Cantonese | 2 (1.32) |
| Italian | 2 (1.32) |
| Korean | 2 (1.32) |
| Japanese | 2 (1.32) |
| Romanian | 2 (1.32) |
| Arabic | 1 (0.66) |
| American Sign Language (ASL) | 1 (0.66) |
| Barrier | Significance of Association with Continued Care (Chi-Squared Test) | OR (95% CI) |
|---|---|---|
| Financial barrier | <0.001 * | 0.454 (0.365–0.564) * |
| Time limitation | 0.310 | - |
| Transportation barrier | 0.006 * | 0.737 (0.493–1.10) |
| Linguistic barrier | <0.001 * | 0.545 (0.384–0.774) * |
| Chief Complaint | Financial Constraints | Time Constraints | Transportation Constraints | Language Barrier | Continuing Care? | Transfer Out of Predoc | Recall | Totals |
|---|---|---|---|---|---|---|---|---|
| (none) | 317 | 161 | 60 | 76 | 845 | 47 | 447 | 1953 |
| Broken Tooth | 1 | 1 | 0 | 0 | 3 | 0 | 1 | 6 |
| Bruxism | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 |
| Crown | 55 | 28 | 6 | 16 | 123 | 7 | 67 | 302 |
| Dentures | 41 | 11 | 17 | 15 | 92 | 6 | 45 | 227 |
| Extraction | 2 | 2 | 1 | 0 | 4 | 0 | 4 | 13 |
| Filling | 34 | 22 | 7 | 5 | 79 | 3 | 39 | 189 |
| FPD | 16 | 5 | 0 | 2 | 19 | 3 | 7 | 52 |
| Hypertension, Diabetes | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 2 |
| Implant | 21 | 21 | 8 | 9 | 94 | 8 | 39 | 200 |
| Missing Tooth | 12 | 8 | 4 | 3 | 25 | 0 | 14 | 66 |
| Pain | 44 | 18 | 9 | 14 | 59 | 5 | 27 | 176 |
| Periodontal Disease | 5 | 1 | 1 | 1 | 8 | 0 | 6 | 22 |
| Prophy | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 2 |
| RCT | 7 | 1 | 0 | 2 | 8 | 1 | 5 | 24 |
| RPD | 15 | 10 | 5 | 8 | 28 | 1 | 12 | 79 |
| Sealants | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 2 |
| Veneers | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Totals | 570 | 290 | 118 | 151 | 1391 | 81 | 715 | 3316 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Simon, L.; Singh Dhaliwal, G.; Liu, C.-H.J.; Sharma, P.; Thomas, S.; Bettag, S.; Weber, K.G.; Timothé, P.; Nalliah, R.P. Characteristics of Patients Discontinuing Care. Dent. J. 2019, 7, 31. https://doi.org/10.3390/dj7020031
Simon L, Singh Dhaliwal G, Liu C-HJ, Sharma P, Thomas S, Bettag S, Weber KG, Timothé P, Nalliah RP. Characteristics of Patients Discontinuing Care. Dentistry Journal. 2019; 7(2):31. https://doi.org/10.3390/dj7020031
Chicago/Turabian StyleSimon, Lisa, Gurmukh Singh Dhaliwal, Chieh-Han Jeffrey Liu, Pranshu Sharma, Shernel Thomas, Sarah Bettag, Katherine G. Weber, Peggy Timothé, and Romesh P. Nalliah. 2019. "Characteristics of Patients Discontinuing Care" Dentistry Journal 7, no. 2: 31. https://doi.org/10.3390/dj7020031
APA StyleSimon, L., Singh Dhaliwal, G., Liu, C.-H. J., Sharma, P., Thomas, S., Bettag, S., Weber, K. G., Timothé, P., & Nalliah, R. P. (2019). Characteristics of Patients Discontinuing Care. Dentistry Journal, 7(2), 31. https://doi.org/10.3390/dj7020031





