Oral Health Condition of Children Living with HIV
Abstract
:1. Introduction
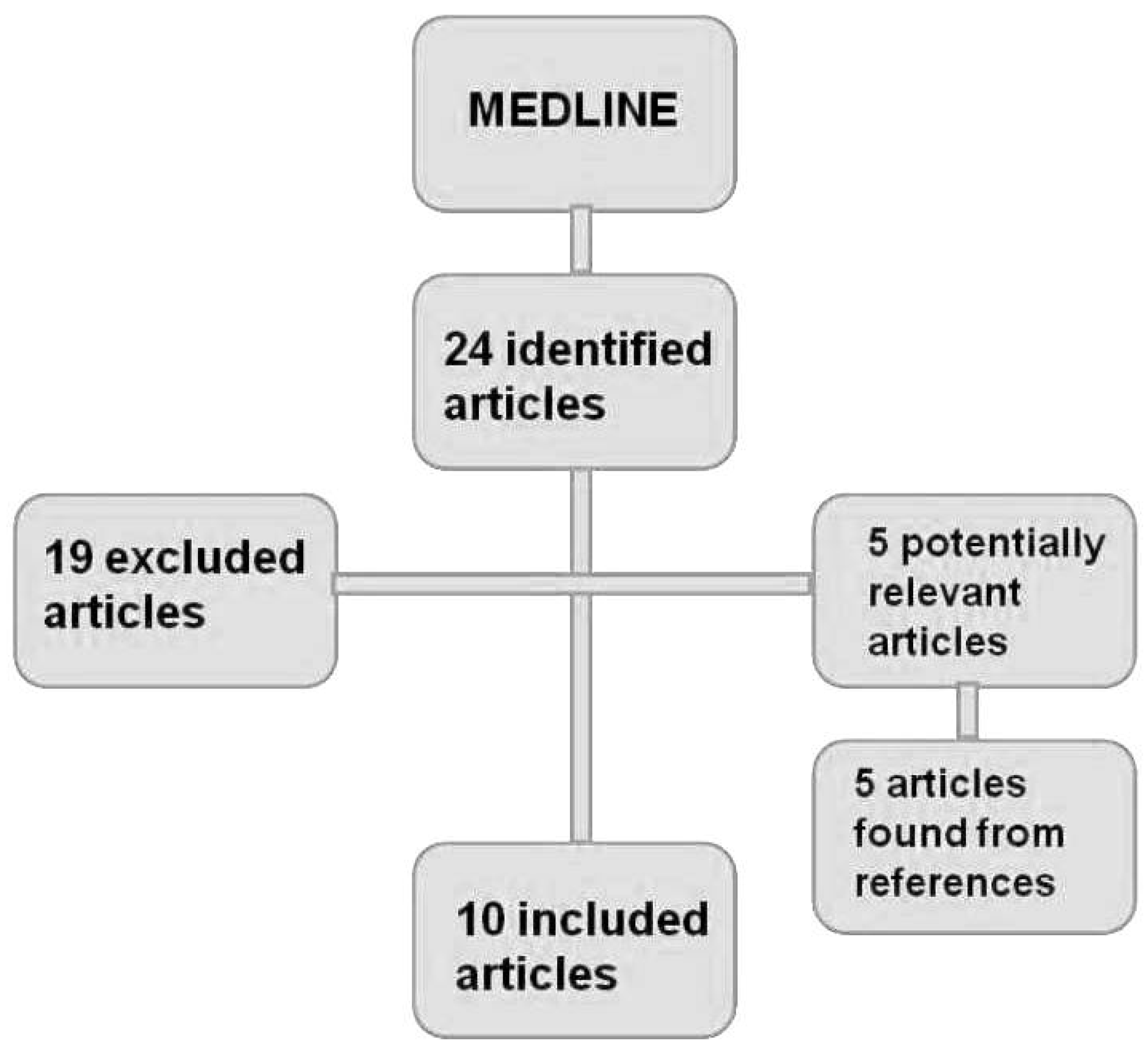
2. Methods
3. Results
| Author (Year) | Aims | Sample and Age Group | Main Results and Conclusions |
|---|---|---|---|
| Portela et al. (2001) [10] | Determining the gingival health condition and its relation with the number of leukocytes and immunosuppression degree. | n = 35 |
|
| Grando et al. (2002) [11] | Evaluating the prevalence of oral manifestations. | n = 184 zero to 13 years old |
|
| Fabro et al. (2002) [5] | Evaluating dental and mucosa conditions. | n = 105 zero to 12 years old |
|
| Ribeiro et al. (2002) [7] | Evaluating if the quality and quantity of biofilm represent important factors in caries activity and gingivitis. | n = 56 zero to 14 years old |
|
| Álvarez Loureiro et al. (2007) [12] | Determining the oral health state of Uruguayan children. | n = 76 one to 17 years old |
|
| Blignaut (2007) [13] | Determining the needs of children’s oral health. | n = 87 three to seven years old |
|
| Dornelas et al. (2008) [6] | Verifying the prevalence of orofacial manifestations and its correlation with immunological classification. | n = 21 two to 12 years old |
|
| Sowole et al. (2009) [14] | Evaluating oral manifestations, the oral health state and the need for treatment. | n = 55 six months to 16 years old |
|
| Kelly et al. (2009) [15] | Determining the risk factors and the prevalence of caries in an HIV-infected children group (GI) and in children without HIV infection (GII). | GI: n = 133; age average 6.8 years old. GII: n = 85; age average 8.1 years old. |
|
| Damle et al. (2010) [16] | Evaluating gingival conditions, caries and lesions in the oral mucosa related to CD4 counting. | n = 234 two to 15 years old |
|
4. Discussion
Conflicts of Interest
References
- Ministério da Saúde (BR); Secretaria de Atenção a Saúde; Departamento de Atenção básica. HIV/AIDS, Hepatites e outras DST. Cadernos de Atenção Básica. Série A; Normas e Manuais Técnicos. n.18; Brasília: Ministério da Saúde, 2006. [Google Scholar]
- Schaurich, D.; Medeiros, H.M.F.; Motta, M.G.C. Vulnerabilidades no viver de crianças com AIDS. Rev. Enferm. UERJ 2007, 15, 284–290. [Google Scholar]
- UNICEF; UNAIDS; World Health Organization. Children and Aids: A stocktaking report. Genebra: UNICEF, 2007. [Google Scholar]
- Ministério da Saúde (BR); Secretaria de Vigilância em Saúde; Programa Nacional de DST e AIDS. Recomendações para terapia Antirretroviral em crianças e Adolescentes infectados pelo HIV. Série Manuais; n.85; Brasília: Ministério da Saúde, 2009. [Google Scholar]
- Ministério da Saúde (BR); Secretaria de Vigilância em Saúde; Programa Nacional de DST e AIDS. Guia de tratamento clínico da infecção pelo HIV em pediatria. 3a ed. Brasília: Ministério da Saúde, 2007. [Google Scholar]
- Fabro, S.M.L.; Ody, E.; Grando, L.J.; Peres, K.G.A.; Rath, I.B.S. Alterações estomatológicas e condições dentais em crianças infectadas pelo HIV. Arq. Odontol. 2002, 38, 163–252. [Google Scholar]
- Dornelas, S.K.L.; Bertazzoli, R.C.B.; Medeiros, M.B.; Biase, R.C.C.G.; Rosa, M.R.D. Manifestações orofaciais e sua correlação com a classificação clínica e imunológica em crianças infectadas pelo HIV em João Pessoa, Paraíba, Brasil. Pesqui. Bras. Odontoped. Clin. Integr. 2008, 8, 179–183. [Google Scholar] [CrossRef]
- Ribeiro, A.A.; Portela, M.; Souza, I.P. Relação entre biofilme, atividade de cárie e gengivite em crianças HIV+. Pesqui. Odontol. Bras. 2002, 16, 44–50. [Google Scholar]
- Cavassani, V.G.S.; Andrade Sobrinho, J.; Homem, M.G.N.; Rapoport, A. Candidíase oral como marcador de prognóstico em pacientes portadores do HIV. Rev. Bras. Otorrinolaringol. 2002, 68, 630–634. [Google Scholar] [CrossRef]
- Machado, F.C.; Souza, I.P.R.; Tura, L.F.R.; Castro, GF. Adesão a um programa de atenção à saúde bucal para crianças e adolescentes infectados pelo HIV e atitude dos responsáveis. Ciênc. saúde coletiva. 2008, 13, 1851–1857. [Google Scholar] [CrossRef]
- Portela, M.B.; Castro, G.F.; Souza, I.P.R.; Silva, R.H.O. Relação entre saúde gengival e condição sistêmica em crianças infectadas pelo HIV. Rev. Bras. Odontol. 2001, 58, 88–91. [Google Scholar]
- Grando, L.J.; Yurgel, L.S.; Machado, D.C.; Silva, C.L.; Menezes, M.; Picolli, C. Manifestações estomatológicas, contagem de linfócitos T-CD4+ e carga viral de crianças brasileiras e norte americanas infectadas pelo HIV. Pesqui. Odontol. Bras. 2002, 16, 18–25. [Google Scholar]
- lvarez Loureiro, L.A.; Hermida, L.; Cuitiño, E. Situación de salud oral de los niños uruguayos portadores del vírus de la inmunodeficiencia humana. Arch. Pediatr. Urug. 2007, 78, 23–28. [Google Scholar]
- Blignaut, E. Oral health needs of HIV/AIDS orphans in Gauteng, South Africa. AIDS Care 2007, 19, 532–538. [Google Scholar] [CrossRef]
- Sowole, C.A.; Orenuga, O.O.; Naidoo, S. Access to oral health care and treatment needs of HIV positive paediatric patients. Pesq. Bras. Odontoped. Clin. Integr. 2009, 9, 141–146. [Google Scholar] [CrossRef]
- Kelly, A.; Soares, L.F.; Pomarico, L.; Souza, I.P.R. Risco e atividade de cárie em crianças com e sem infecção pelo HIV. RGO 2009, 57, 217–222. [Google Scholar]
- Damle, S.G.; Jetpurwala, A.K.; Saini, S.; Gupta, P. Evaluation of oral health status as an indicator of disease progression in HIV positive children. Pesq. Bras. Odontoped. Clin. Integr. 2010, 10, 151–156. [Google Scholar] [CrossRef]
- Organização Mundial da Saúde. Levantamento Básico em Saúde Bucal, 4th ed.São Paulo: Santos, Brazil, 1999. [Google Scholar]
- Vieira, T.R.; Péret, A.C.A.; Péret Filho, L.A. Alterações periodontais associadas às doenças sistêmicas em crianças e adolescentes. Rev. Paul. Pediatr. 2010, 28, 237–243. [Google Scholar] [CrossRef]
- Alves, F.B.T.; Czlusniak, G.D.; Dal‘Maso, A.M.S.; Shimizu, K.H.; Verri, M.A. Lesões estomatológicas em crianças HIV positivas e suas implicações clínicas. Arq. Odontol. 2009, 45, 191–198. [Google Scholar]
- Favalessa, O.C.; Martins, M.A.; Hahn, R.C. Aspectos micológicos e suscetibilidade in vitro de leveduras do gênero Candida em pacientes HIV-positivos provenientes do Estado de Mato Grosso. Rev. Soc. Bras. Med. Trop. 2010, 43, 673–677. [Google Scholar] [CrossRef]
- Chimenos, E.; Lopez, P.D. Fármacos antifúngicos utilizados em el tratamiento de la micosis. Med. Oral. 1998, 3, 78–90. [Google Scholar]
- Guggenheimer, J.; Moore, P.A. Xerostomia: etiology, recognition and treatment. J. Am. Dent. Assoc. 2003, 134, 61–69. [Google Scholar] [CrossRef]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Rovaris, N.S.; Martins, L.G.T.; Traebert, J. Oral Health Condition of Children Living with HIV. Dent. J. 2014, 2, 1-10. https://doi.org/10.3390/dj2010001
Rovaris NS, Martins LGT, Traebert J. Oral Health Condition of Children Living with HIV. Dentistry Journal. 2014; 2(1):1-10. https://doi.org/10.3390/dj2010001
Chicago/Turabian StyleRovaris, Natália Spillere, Luiz Gustavo Teixeira Martins, and Jefferson Traebert. 2014. "Oral Health Condition of Children Living with HIV" Dentistry Journal 2, no. 1: 1-10. https://doi.org/10.3390/dj2010001
APA StyleRovaris, N. S., Martins, L. G. T., & Traebert, J. (2014). Oral Health Condition of Children Living with HIV. Dentistry Journal, 2(1), 1-10. https://doi.org/10.3390/dj2010001




