1. Introduction
Ontogenetically, alveolar bone formation is closely linked to tooth eruption [
1]. Tooth agenesis or ankyloses result in absent or reduced growth of the alveolar process [
2,
3]. Conversely, the loss of a tooth triggers a remodeling reaction as part of the healing process, involving various degrees of alveolar bone resorption, especially affecting the buccal lamella: The bundle bone is primarily vascularized by the periodontal membrane of the tooth. Therefore, this part of the alveolar bone is compromised by the extraction, to such an extent that the buccal lamella is insufficiently nourished, leading to its total or partial resorption [
4,
5]. Bone resorption of up to an average width of 50% [
6] or 3.8 mm [
7] has been reported. Losses in height of 2 mm to 4 mm [
5,
8] or 1.24 mm on average [
7] have also been measured. However, this resorption process is highly variable and not fully predictable [
9]. A substantial 0.5% to 1% of the alveolar ridge volume is lost as the result of it [
10]. A higher degree of resorption is to be expected in the presence of flap formation, thin soft tissue biotype and prominent roots, especially with frontal teeth in buccal position [
7,
11]. Immediate implant placement does not necessarily prevent resorption of the alveolar ridge [
12].
These resorption processes have a negative impact on the subsequent implant-based rehabilitation. By the targeted use of guided bone regeneration (GBR) techniques, it has been attempted for many years now to preserve the alveolar ridge in all its dimensions [
11,
13]. The most simple and, from an ontogenetic perspective, most physiological approach to the prevention of alveolar ridge resorption is to naturally preserve the inflammation-free dental root—if possible. Techniques for submucosal vital and non-vital root retention have already been described [
14]. Salama [
15] demonstrated that the so-called root submergence technique (RST) preserves the natural periodontium, thereby completely preventing bone resorption. Von Arx
et al. [
16] have recently published a new method to preserve the alveolar ridge after posttraumatic ankylosis and external root resorption by leaving the de-crowned root fragments. Davarpanah and Szmukler [
17] published a case series of five patients showing that immediately placed implants where direct implant contact with ankylosed tooth fragments was ensured, were preserved without any signs of abnormal changes over a follow-up period of two years. Hürzeler
et al. [
18] also demonstrated that the intentional preservation of the coronal buccal root portion can help to ensure the physiological preservation of labial and buccal bone structures if the implant is placed in contact to this natural tooth fragment (shield). However, this approach is associated with certain risks, such as the formation of a peri-implant periodontal membrane [
19] or the development of peri-implant infections, as well as resorption associated with the usual biological long-term complications that may occur. These occur especially in the presence of pre-exiting or developing periodontal or endodontic infections or inflammations of the retained tooth fragments. To date, no experiences with the use of a modified technique, not involving simultaneous implantation for alveolar ridge resorption prevention, have been published. Thus, delayed implantation could be an alternative approach to preserve the buccal lamella over a prolonged period of time and to reduce the above-mentioned risks and complications. The case presentations detailed below are intended to illustrate how, by leaving a buccal root segment, lamellar bone resorption can virtually be eliminated. The possibilities and limitations are presented and discussed.
2. Clinical Concept, Procedures and Indications
With the root submergence technique (RST), submucosal root retention can virtually eliminate bone resorption [
15]. Based on this concept, the retention and stabilization of the coronal and buccal bundle bone and the retention of the periodontal membrane by retaining a coronal tooth fragment (so-called “socket shield”), including adequate blood supply, can be expected. To ensure complication-free healing, special attention should be paid to wound stabilization: stabilization of the clot with a criss-cross suture is optimized by placing a collagen cone with integrated collagen membrane, such as collagen sponge with integrated membrane (Parasorb Sombrero
®, Resorba, Nurnberg, Germany) into the tooth socket. Depending on the individual treatment plan of a patient, there is the option to either wait for two to six months to allow for the formation of new bone, followed by implantation, or to leave the site without subsequent second procedure.
Therefore, potential indications for such techniques include their use as part of the (delayed) late implantation approach or the optimisation of pontic support in crown-bridge reconstructions or to improve the prosthesis base for removable dentures. As general contraindications, the usual restrictions for oral surgical procedures (bisphosphonate medication, immunosuppression, radiation therapy, anticoagulation, etc.) apply. Local contraindications include an absent buccal lamella, which develops for instance after vertical root fractures or periodontitis.
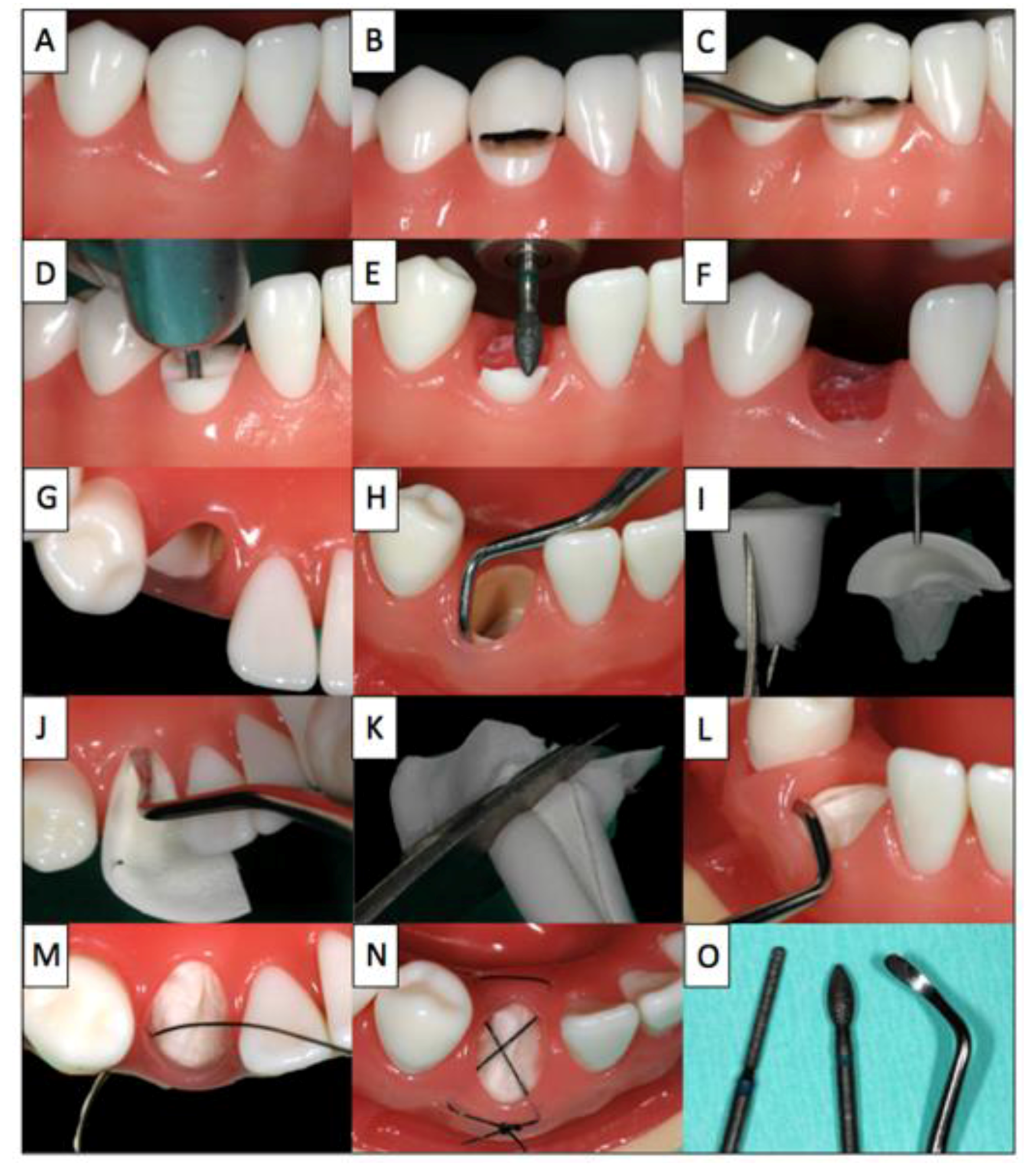
A step-by-step illustration of the proposed procedure using a model illustrating the extraction and treatment of tooth 43 is given in
Figure 1:
Figure 1.
The step-by-step procedure illustrated on a model (Frasaco GmbH, Tettnang, Germany).
Figure 1.
The step-by-step procedure illustrated on a model (Frasaco GmbH, Tettnang, Germany).
Firstly, the hopeless tooth is split supragingivally (B) and the crown fragment is carefully dislocated and removed using a suitable instrument (C). Then, the root is separated vertically in a ratio between 1:3 and 2:3 (D). The smaller, buccal root fragment is retained and the larger lingual root fragment is removed in a manner that spares bone and soft tissue to the greatest possible extent. The height of the buccal socket shield is reduced to the level of the bone (E,F) and the gingiva overlying the retained buccal root fragment is tunnelled by 2 mm (H) to allow the insertion of the collagen cone (I,L) into the tooth socket and placement of the membrane part of the collagen cone under the buccal mucosa. Finally, the collagen cone is secured with a criss-cross suture (M,N). For this intervention, only the following instruments are required: periotome, Black’s excavator, gingival scissors, needle holder and surgical forceps as well as diamond drill (O). After the procedure, patients rinse with 0.2% chlorhexidine mouthwash two to three times daily for one minute over a period of at least ten days. During this time, mechanical oral hygiene is avoided in the affected area and only restarted after the follow-up examination and suture removal after ten days. Anti-inflammatory drugs (e.g., Mefenacid 500mg tid) are prescribed as needed. Typically, no antibiotics are prescribed (exemption: systemic diseases, shielding etc.). Each patient was informed verbally and in writing about the treatment and the materials used as well as the associated pre- and post-operative risks and gave their written consent to the use of the collected data and photos.
3. Case Presentations
3.1. Case 1
Medical history: A 60-year-old woman, non-smoker, in good general condition, no systemic illness, not on regular medication.
Extra-oral findings: The patient’s facial features were symmetrical with deep smile lines. On inspection and palpation, no abnormalities detected.
Local intra-oral findings 1st quadrant: Fixed reconstruction of teeth 13/12/11 with a bridge (metal-fused-to-ceramic), implant-supported cantilever bridge 14/15/16, diastema between 14 and 13.
X-ray: The dental radiography showed a translucency at the crown margin of tooth 13. The axis of the endodontic post was not in line the root canal axis and there was an apical osteolysis at the tip of the root.
Diagnosis: Secondary root caries on tooth 13 in the region of the distal crown edge and suspected root perforation as well as apical periodontitis.
Prognosis: Root 13 was considered irrational to treat.
Treatment plan: Cutting of the bridge distal of abutment 12 and partial root extraction of tooth 13, prevention of alveolar ridge resorption using the socket shield technique, late implantation at region 13 (Nobel Biocare Replace
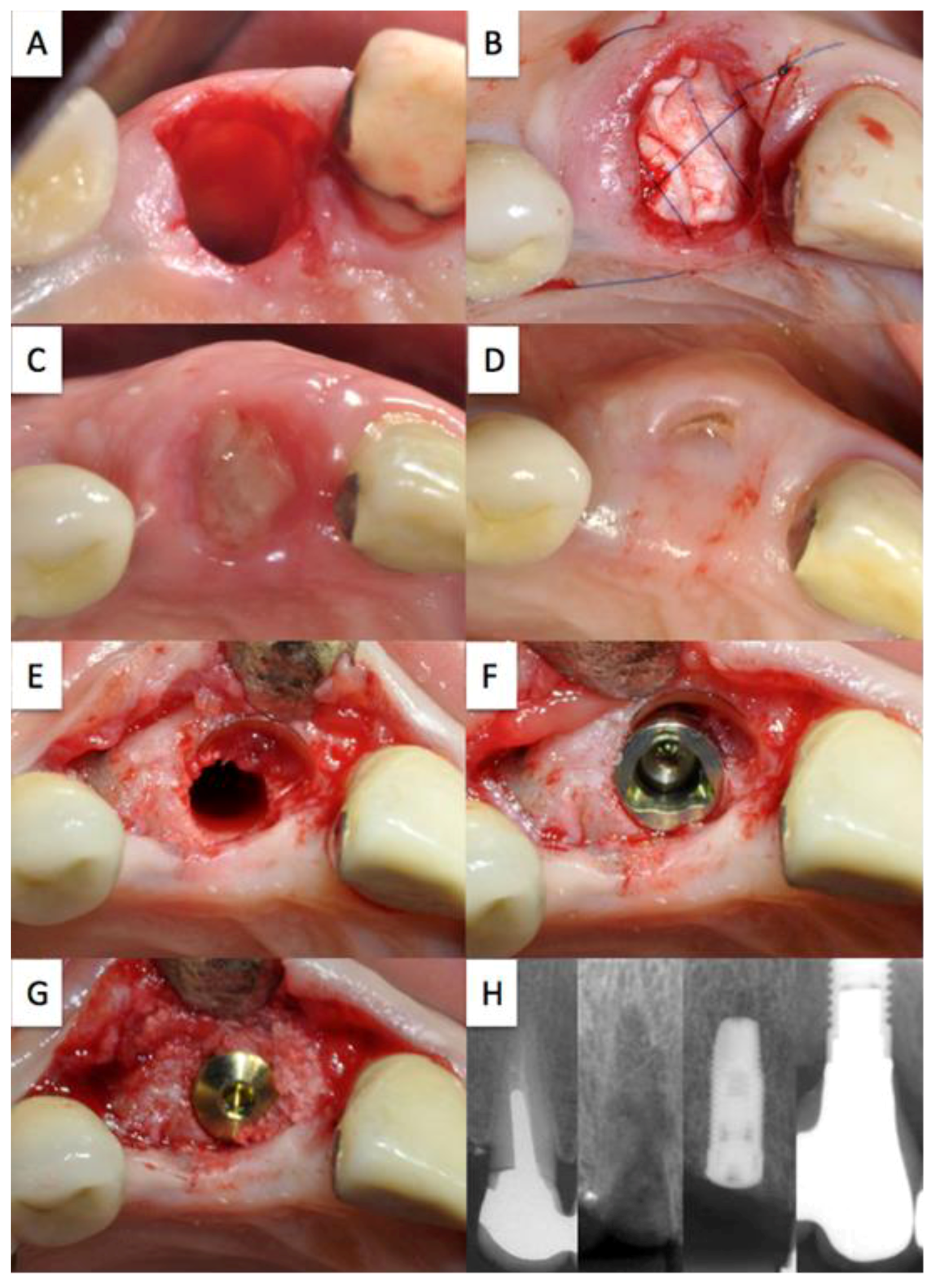
®). The treatment is depicted in
Figure 2.
Status post extraction with retention of the shortened and reduced root fragment (A); Absorbable cone inserted into the extraction socket secured with criss-cross suture (B); healing course following suture removal after 10 days (C); possible perforation of the buccal mucosa by the socket shield (D); completely preserved buccal bundle bone with re-entry (E); optimum, slightly palatial shift of the implant, jumping distance between implant and socket shield was filled with Bio-oss® (G); pre-operative X-ray control, with socket shield in the healing phase, with inserted implant, with screwed crown (H).
3.2. Case 2
Medical history: A 28-year-old woman, smoker, in good general condition, no systemic illness, not on regular medication.
Dental history: A schoolyard fall resulted in necrosis with consecutive root canal treatment of tooth 11. Despite apicoectomy, the apical osteolysis did not heal completely.
Extra-oral findings: The patient’s facial expression was symmetrical with deep smile lines. On inspection and palpation no abnormalities were detected.
Intra-oral local findings: Dentition restored. Root canal treated tooth 11 with intrinsic discoloration of the crown.
X-ray: Periapical radiolucency at tooth 11.
Diagnosis: Tooth 11 with apical periodontitis and minimal thickness of the remaining dentin as well as chromatic aberration.
Prognosis: Root 13 was considered irrational to re-treat.
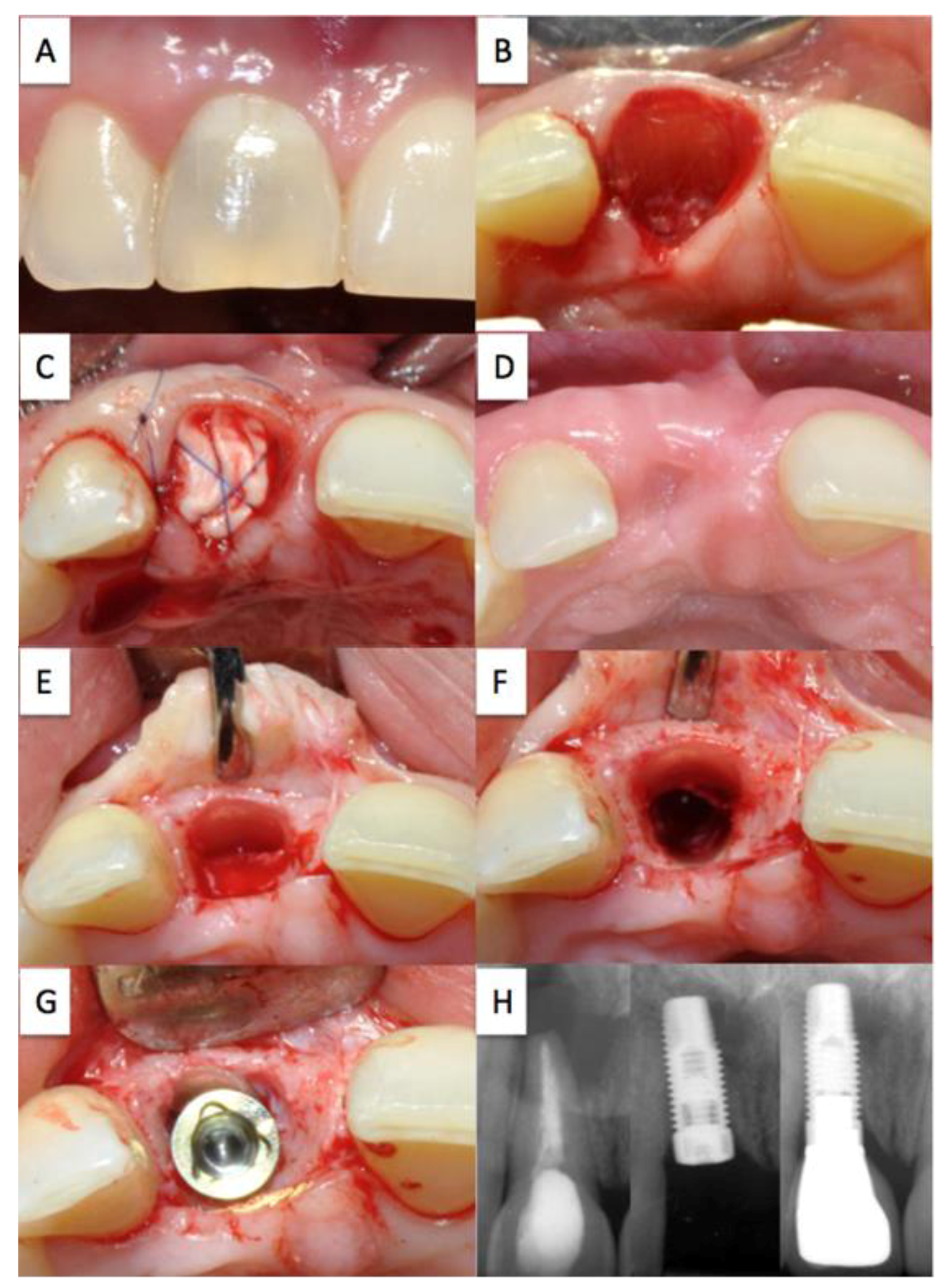
Treatment plan: Partial extraction of tooth 11 (A), prevention of alveolar ridge resorption using the socket shield technique (B,C,D), late implantation (G) of a titanium implant (Nobel Biocare Replace
®). The treatment is depicted in
Figure 3.
Chromatic aberration of the crown of the root-treated tooth 11 (A); Status post extraction with retention of the shortened and reduced root fragment (B); absorbable cone inserted into the extraction socket secured with criss-cross suture (C); healing course following suture removal after 30 days (D); completely preserved buccal bundle bone with re-entry (E); view after preparation of the implant site (F); optimum position of the implant with slight palatial shift (G); preoperative X-ray control (left), with inserted implant (middle), screwed crown (right) (H).
3.3. Case 3
Medical history: A 28-year-old woman, non-smoker, in good general condition, no systemic illness, not on regular medication.
Dental history: Orthodontic treatment during youth resulted in necrosis of teeth 13 and 22, 23. Root canal treatment with consecutive discoloration of tooth 22. Status post apicoectomy of tooth 22 with retrograde filling (1995).
Extra-oral findings: The patient’s facial expression was symmetrical with deep smile lines. On inspection and palpation no abnormalities detected.
Intra-oral local findings: Dentition restored. Endodontically treated teeth 13, 22 and 23. Discoloration of the dental crown 22.
X-ray: Periapical radiolucency at tooth 22.
Diagnosis: Tooth 22 with apical periodontitis and minimal thickness of the remaining dentin as well as chromatic aberration.
Prognosis: Root 22 was considered irrational to re-treat.
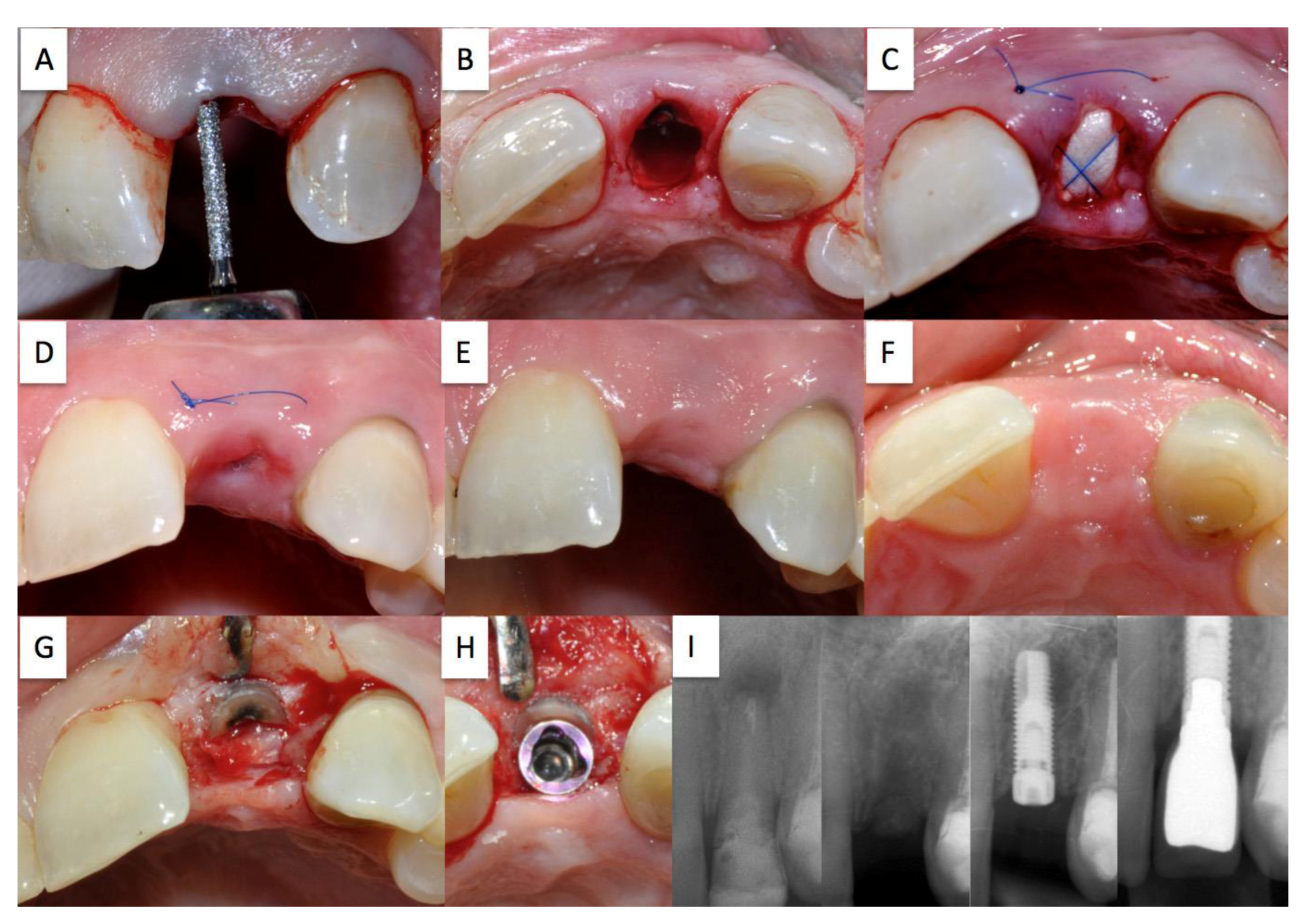
Treatment plan: Partial extraction of tooth 22 (A), prevention of the alveolar ridge resorption using the socket shield technique (B,C,D), late implantation (G) of a titanium implant (Nobel Biocare Replace
®). The treatment is depicted in
Figure 4.
De-epithelialisation of the wound margins with a diamond polisher (A); status post extraction with retention of the shortened and reduced root fragment (B); Absorbable cone inserted into the extraction socket secured with criss-cross suture (C); healing course following suture removal after 10 days (D); buccal view of the healing course after 30 days (E); occlusal view of the healing course after 30 days with intact buccal soft tissue contour (F); completely preserved buccal bundle bone with re-entry (G); optimum, slightly palatial shift of the implant (H); preoperative X-ray control, with socket shield in the healing phase, with inserted implant, with screwed crown (I).
4. Discussion
Apart from affecting the aesthetic outcome, alveolar ridge atrophy after tooth extraction has, above all, a negative impact on the subsequent prosthetic or implant restoration [
20,
21]. In recent years, several scientific studies on socket preservation have been published. True to the motto “when we take something out, we should put something back in” [
22], studies have been carried out where fresh extraction sockets were filled and covered with various bone substitutes and membranes [
23].
Ideally, a method for the prevention of alveolar ridge resorption should be a cost-effective and minimally invasive, with only minimal material requirements. However, these criteria are not entirely met by any of the methods available today. Moreover, the goal of complete preservation of the alveolar ridge after tooth extraction has not even been reached with sophisticated techniques [
24]. Thus, the quest for simple concepts with predictable results is still on today’s research agenda.
It has been known for some time that to retain root fragments
in situ covered by mucosa represents an alternative technique for alveolar ridge preservation [
25,
26]. Studies showed for de-crowned root fragments not only adequate bone volume preservation but also vertical bone growth in a coronal direction [
3,
27]. Therefore, the targeted retention of root fragments appears to be the only approach capable of achieving complete alveolar ridge preservation. Three pilot cases were documented to proof alveolar ridge preservation based on subepithelially retained root fragments. Since later implant placement was intended, only the oral root fragment was removed and the buccal root fragment, just large enough to meet the minimum requirements, was preserved. With this approach it was attempted to enable the maintain of the bone at the prospective implant site, while the buccal bundle bone, which is very thin and consequently at high risk of resorption, was retained [
5,
28]. The lingual portions of the bundle bone are thicker and less prone to atrophy. In addition, delicate anatomical structures, such as blood vessels and nerves, are found especially in the lateral tooth area of the lower jaw, so that the general use of a lingual socket shield technique appears to be too demanding and risky. In the case reports presented above, a minimally invasive flap was created to expose the surgical site and the root fragment during the subsequent implantation procedure (re-entry). To prevent further compromise of the blood supply to the vestibular bone, relief incisions were kept to a minimum [
29]. Complete preservation of the buccal lamellar bone was observed intra-operatively in all three cases. By reducing the buccal socket shield to a thickness of less than 1 mm and its corono-apical extension to one third of the former root length, the largest possible osseous implant bed was created, while the dentin-implant interface [
30], the long-term behaviour of which has not been studied sufficiently, was minimized. However, these changes were not quantified or measured, e.g., by DVT, as part of these case reports.
Even so, the clinical outcomes show that the presented modified socket shield technique essentially meets the expectations for an ideal method for preventing alveolar ridge resorption and minimal material requirements (collagen cone/membrane). It may even be possible to do without any of these materials. Studies investigating this modification and their results are still pending.
It needs to be highlighted that the presented partial extraction is technique-sensitive and associated with the risk of displacement of the buccal root fragment, or even the buccal lamellar bone. Already at the time of extraction, the root fragment should be reduced along its vertical axis to the level of the height of the alveolar ridge to prevent perforation of the buccal mucosa during the healing period. Should the root fragment become exposed despite this preventative measure, height reduction and tissue freshening can be performed during follow-up visits. The buccal shield should be thinned in its horizontal dimension to a height of less than 1 mm to ensure that the former tooth socket is filled with a maximum amount of bone and only minimal dentin at the time of re-opening. In other words, it should be attempted to achieve an implant position where all boundaries are formed by bone, since, according to current and established principles of osseointegration [
31], only direct bone-implant contact without fibrous tissue or other dental materials is accepted as a successful implant interface. If this is the case, complete osseointegration of the implant will be achieved and the formation of a fibrous tissue sheath around the implant [
18,
19], can be avoided. Here again it has to be mentioned as a limitation that such data could not be collected as part of this case series. Furthermore, the long-term behavior of the buccal shield has not yet been completely clarified. Warrer
et al. [
32] showed in 1993 that new cement is deposited on the aspect of the dentin shield facing the former socket. This cement layer should be regarded as a protection against resorption by osteoclasts [
33]; however, data in support of this view are not yet available. Periodontal membrane formation around the implant may occur when the implant-root interface has a loose structure and a larger gap is left [
34], and when the periodontal ligament of the root fragment is in contact [
32] with the cement-coated implant surface.
It is indisputable that the buccal shield protects the integrity of the buccal bundle bone and serves as a guiding structure when placing the implant in the optimum position with a slight palatinal shift during the re-entry procedure. Future controlled studies should focus on this treatment modality, even without the use of any additional materials like a collagen sponge, to minimize the technical efforts. It should also be tested, whether the root fragments should be removed or, if persisting, may lead to long-term remodeling or resorption effects.