Augmented Reality in Implant and Tooth-Supported Prosthodontics Practice and Education: A Scoping Review
Abstract
1. Introduction
- Precise fit of restorations: Crowns, bridges, dentures, and implants must align perfectly with the patient’s existing teeth and gums [6]. Even the slightest inaccuracy can lead to discomfort, improper function, or long-term complications.
- Preservation of oral health: Misaligned restorations can create undue pressure on certain teeth, leading to wear, fractures, or even loss of natural teeth. Proper spatial accuracy prevents these issues [10].
1.1. The Rise of AR in Implant and Tooth-Supported Prosthodontics
1.2. AR in Dental Education: A Paradigm Shift
1.3. Aim of This Scoping Review
2. Materials and Methods
2.1. Design
2.2. Objective
2.3. Search Strategy
- Population: Dental professionals and students engaging with AR for ITSP.
- Concept: AR applications in ITSP practice and education.
- Context: Peer-reviewed journals, clinical trials, in vitro studies, technical reports [43]. Publication date: January 2015–July 2025 (to capture AR advancements).
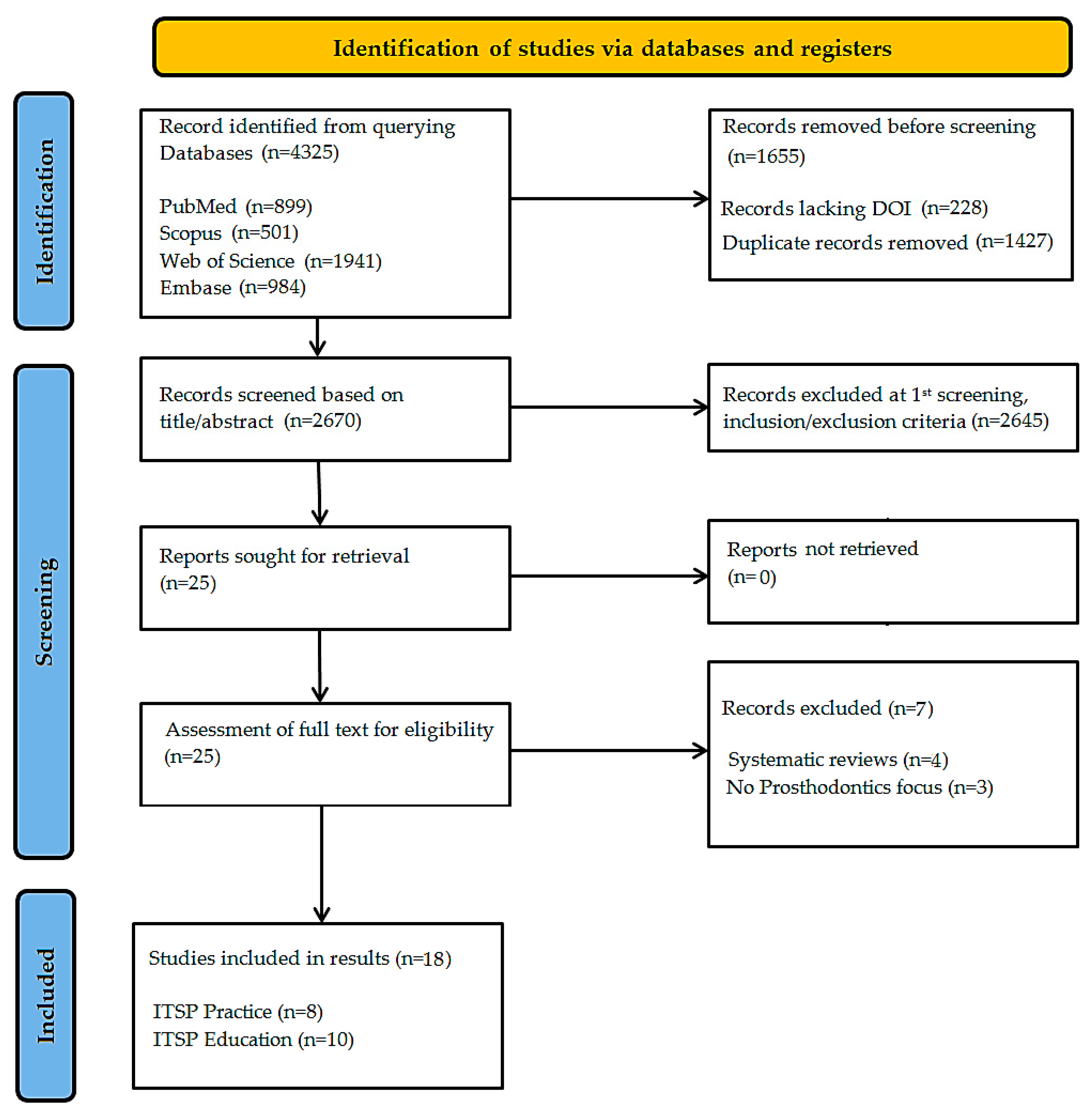
- Initial hits: 4325 records (4097 after removing entries without DOIs).
- Post-deduplication: 2670 unique articles.
- Title/abstract screening excluded 2645 records, leaving 25 for full-text review.
- Final included studies: 18.
2.4. Eligibility Criteria
2.5. Source Selection Process
2.6. Evaluation of Source Quality
3. Results
3.1. Study Selection
3.2. Examination of Included Studies
3.3. Evidence of Augmented Reality in Implant and Tooth-Supported Prosthodontics
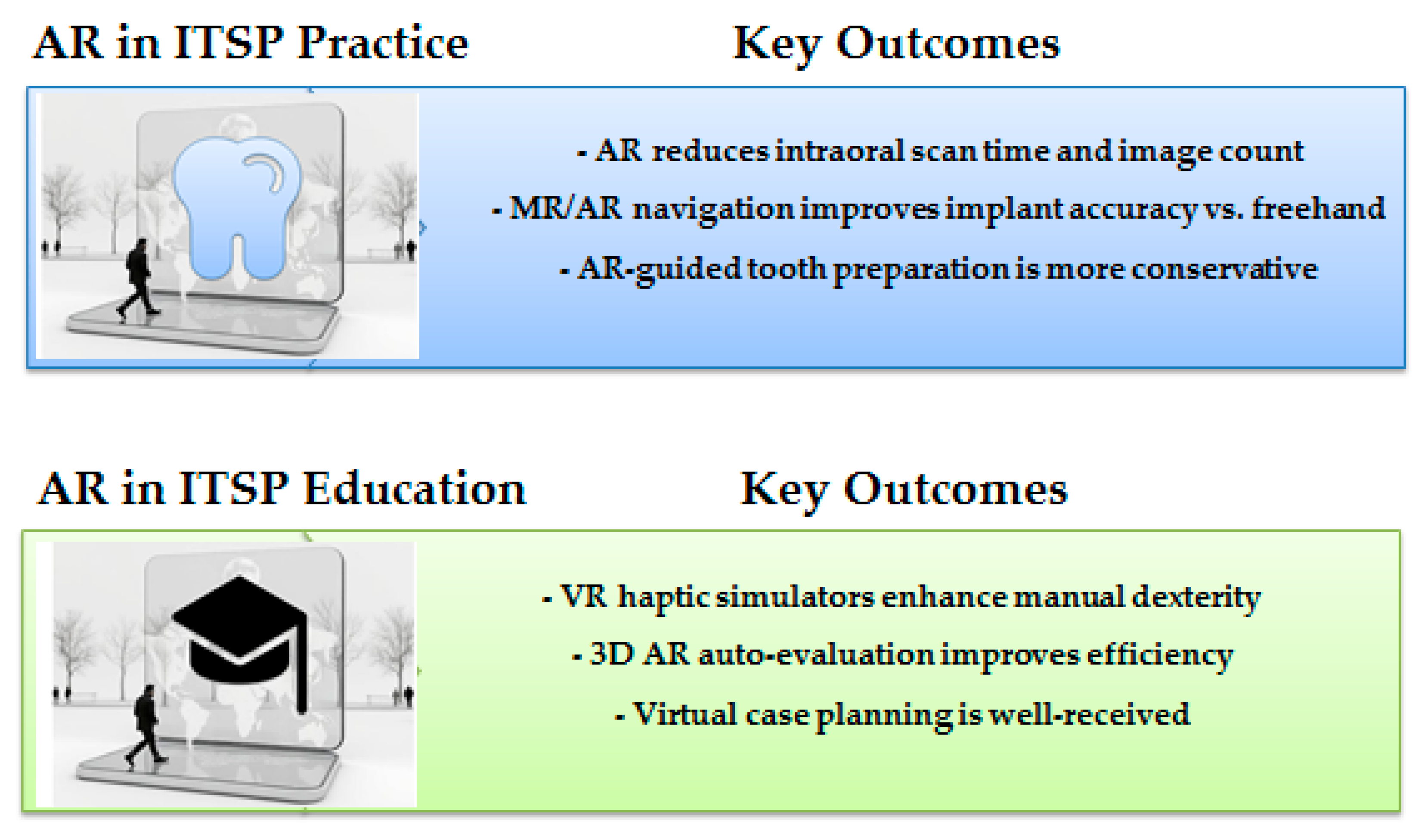
3.3.1. Augmented Reality in ITSP Practice
- 1.
- Intraoral Scanning & Digital Impressions
- Alharbi & Osman (2024) [44] conducted a clinical pilot study comparing AR-assisted intraoral scanning (IOS) with conventional IOS. Their findings demonstrated that AR-assisted scanning reduced scan time by 19 s (44 s vs. 63 s, p < 0.001) and decreased the number of images captured (836 vs. 1209, p < 0.001) without compromising trueness (RMSE comparison, p > 0.05) [44].
- 2.
- Implant Placement Accuracy
- Liu et al. (2023) [45] developed a mixed reality (MR)-based navigation system for dental implants, reporting significantly lower deviations compared to freehand placement:
- ○
- Entry deviation: 0.69 ± 0.25 mm (MR) vs. 1.57 ± 0.50 mm (freehand, p = 0.000)
- ○
- Angular deviation: 1.85 ± 0.61° (MR) vs. 4.93 ± 1.65° (freehand, p = 0.000) [45].
- Tao et al. (2024) compared AR-based dynamic navigation (ARDN) with conventional dynamic navigation (DN), finding no significant differences in coronal/apical deviations but higher angular deviation with ARDN (3.72 ± 2.13° vs. 3.1 ± 1.56°, p = 0.02) [46].
- Lin et al. (2015) integrated AR with surgical templates, reducing deviations in fully edentulous mandibles (entry: 0.50 ± 0.33 mm; apex: 0.96 ± 0.36 mm; angle: 2.70 ± 1.55°) [49].
- Pellegrino et al. (2019) reported entry deviations of 0.53 mm and 0.46 mm in two AR-guided implant cases, with angular deviations of 3.05° and 2.19°, confirming feasibility [50].
- Shusterman et al. (2024) demonstrated high accuracy (0.42 mm entry deviation, 1.85° angular deviation) in a mixed reality-based dynamic navigation (MR-DN) system [51].
- 3.
- Tooth Preparation & Crown Design
- Obispo et al. (2023) found that AR-guided tooth preparation resulted in more conservative and predictable crown preparations compared to freehand techniques (p = 0.0001 for volumetric reduction) [47].
- Kihara et al. (2024) evaluated AR head-mounted displays (HMDs) for tooth preparation, showing that cross-sectional AR visualization reduced over-reduction and improved angle adjustment (p < 0.05) [48].
3.3.2. Augmented Reality in ITSP Education
- 1.
- Preclinical Training & Skill Acquisition
- Daud et al. (2023) found that virtual reality haptic simulators (VRHS) improved manual dexterity, with students strongly agreeing (76%) that VRHS should supplement traditional training [52].
- Mai et al. (2025) introduced a 3D AR auto-evaluation algorithm for tooth preparation, showing high reliability (ICC = 0.75–0.95) and reduced evaluation time (10.5 s vs. 2 h for manual scoring) [53].
- Grad et al. (2023) compared 3D-printed models vs. AR models (HoloLens) for occlusal anatomy reconstruction, finding 3D-printed models more accurate (Hmax = 630 µm, p = 0.004) but AR useful for visualization [54].
- 2.
- Virtual Simulation & Feedback Systems
- Özdemir et al. (2021) highlighted virtual articulators and occlusal records as valuable tools for dynamic occlusion analysis in prosthodontic education [55].
- Li et al. (2021) reviewed dental simulators, noting their potential in preclinical training but emphasizing limitations in force feedback and realism [56].
- Mansoory et al. (2022) demonstrated VR-enhanced learning in the neutral zone and teeth arrangement, with higher student performance (16.92 ± 1.12) vs. traditional methods (16.14 ± 1.18, p < 0.05) [57].
- 3.
- Radiographic & Prosthetic Case Planning
- Alsufyani et al. (2023) compared VR-based panoramic anatomy training with lectures, finding lectures superior in landmark identification but VR highly engaging (student satisfaction = 4.66/5) [58].
- Arora et al. (2023) reported that haptic simulators improved crown preparation skills, though conventional typodont training yielded better results in later trials (p < 0.05) [59].
- Hsu & Chang (2025) found that Simodont haptic simulator performance predicted conventional crown preparation success (OR = 5.6, p < 0.001), particularly in male students [60].
- Liebermann et al. (2024) assessed a virtual prosthetic case planning environment (VCPE), with 87% of students recommending its integration into curricula [61].
4. Discussion: The Benefits and Challenges of Augmented Reality in Implant and Tooth-Supported Prosthodontics Practice and Education
4.1. AR in ITSP Practice: Efficiency vs. Barriers
4.1.1. Intraoral Scanning and Digital Workflows
4.1.2. Implant Placement Accuracy
4.1.3. Tooth Preparation and Prosthodontic Applications
4.1.4. Challenges in Clinical Integration
- Cost and Accessibility: High expenses for AR devices (e.g., Magic Leap, HoloLens) deter widespread use, as reported by Alharbi & Osman (2024) [44]. This economic constraint represents a significant practical limitation that current technology and the present literature, as synthesized in this review, cannot fully overcome. It suggests that without market changes or subsidized models, AR remains largely inaccessible for many individual practices and educational institutions, particularly in resource-limited regions, thereby potentially exacerbating existing disparities in access to advanced digital care.
- Technical Limitations: Discrepancies between virtual planning and real-world execution, particularly in dynamic surgical environments, as noted by Joachim et al. [66].
- Lack of Multi-Center Trials: Few studies compare AR to conventional methods in large-scale clinical settings, resulting in significant research gaps.
4.2. AR in ITSP Education: Enhanced Learning with Adaptation Challenges
4.2.1. Haptic Simulators and Skill Acquisition
4.2.2. Three-Dimensional Auto-Evaluation and Virtual Patients
4.2.3. Scalability and Cost-Effectiveness
4.3. Future Directions and Research Gaps
- 1.
- Integration with Digital Workflows, AI, and Other Tools
- AI-driven AR: The potential synergy between AR and artificial intelligence (AI) is particularly promising; the deeper interdisciplinary integration of AR with artificial intelligence (AI) and other digital technologies is a key future direction. AI algorithms could analyze real-time AR data during a procedure to provide predictive guidance, anomaly detection, and automated adjustment suggestions, enhancing both precision and safety [70]. AI-driven analysis of real-time AR data can deliver automated feedback, ultimately creating a fully interoperable digital workflow from diagnosis to execution [71,72].
- Miniaturized AR Devices: Smart glasses (e.g., HoloLens 2) may improve ergonomics but require validation in clinical trials [44].
- 2.
- Standardization and Multi-Center Validation
- Optimal Display Type: No consensus exists on head-mounted vs. projector-based AR [Research Gaps].
- Standardized Validation Frameworks: A critical gap for translation. A central and recurring theme identified across the included studies is the conspicuous absence of uniform validation frameworks and metrics for AR technologies. This heterogeneity, evident in the diverse outcome measures and experimental designs summarized in Table 3, presents a significant barrier to the field’s maturation. The lack of standardized protocols (e.g., ISO standards for quantifying implant deviation, task completion time in educational settings) fundamentally impedes the direct comparison of results across different AR systems [73]. Consequently, it remains challenging to establish universal benchmarks for the reliability, validity, and clinical efficacy of AR applications. This scoping review itself is limited in its ability to perform cross-study quantitative synthesis precisely because of this methodological heterogeneity. Therefore, a paramount priority for future research must be the community-driven development and adoption of standardized validation frameworks. This is a prerequisite for robust multi-center trials, meaningful meta-analyses, and ultimately, the evidence-based clinical adoption of AR in ITSP.
- 3.
- Educational Innovations
- Adaptive Learning Curves: AI-powered AR could personalize training based on student performance [Future Directions].
- Blended Learning Models: Combining AR with 3D-printed models improves transition to clinical practice [36].
4.4. Limitations of This Scoping Review
5. Conclusions: Mapping the Unique Landscape of AR in ITSP—A Scoping Review’s Contribution
- For Clinicians & Practices: AR in implant and tooth-supported prosthodontics practice enhances precision in implants and tooth prep but needs refinement for angular accuracy. Prioritize investment with a phased integration, using AR initially as a supplemental tool to verify static guides or enhance intraoral scanning efficiency, rather than a complete replacement for conventional methods.
- For Educators & Institutions: AR in implant and tooth-supported prosthodontics education improves skill training and grading efficiency but cannot fully replace human models. Integrate AR/VR haptic simulators (e.g., Simodont) as a supplemental tool in preclinical curricula to accelerate skill acquisition and provide objective, automated assessment. Develop blended learning models that combine AR visualization with 3D-printed patient-specific models to ensure a smooth transition to clinical practice.
- Prioritizing RCTs that validate AR’s efficacy in prosthodontic-specific tasks like crown and bridge preparation.
- Developing standardized validation protocols tailored to ITSP outcomes (e.g., marginal fit, occlusal accuracy).
- Conducting cost–benefit analyses and development of more affordable solutions to improve accessibility and mitigate the risk of widening global inequities in digital dental care.
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| AR | Augmented reality |
| ITSP | Implant and tooth-supported prosthodontics |
| PRISMA-ScR | Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews |
| RCT | Randomized controlled trial |
| CAD/CAM | Computer-aided design/computer-aided manufacturing |
| 3D | Three-dimensional |
| DSD | Digital smile design |
| AI | Artificial intelligence |
| MR | Mixed reality |
| MeSH | Medical Subject Headings |
| PICO | Patient/Problem, Intervention, Comparison, and Outcome. |
| PCC | Population, Concept, Context |
| JBI | Joanna Briggs Institute |
References
- Gawali, N.; Shah, P.P.; Gowdar, I.M.; Bhavsar, K.A.; Giri, D.; Laddha, R. The Evolution of Digital Dentistry: A Comprehensive Review. J. Pharm. Bioallied Sci. 2024, 16 (Suppl. S3), S1920–S1922. [Google Scholar] [CrossRef]
- Elmarakeby, A.M.; Alrashed, A.; Zahr, A.; Alanazi, F.; Alazmi, G.; Abulsaud, H.; Alsulami, R.; Jafar, S.; Albalawi, S.; AlRosini, S.; et al. The Transformative Impact of Digital Technologies on Modern Dentistry: A Narrative Review of the Applications and Benefits. JOHS 2025, 5, 24–30. [Google Scholar] [CrossRef]
- Singi, S.R.; Sathe, S.; Reche, A.R.; Sibal, A.; Mantri, N. Extended Arm of Precision in Prosthodontics: Artificial Intelligence. Cureus 2022, 14, 11. [Google Scholar] [CrossRef]
- Jamjoom, F.Z.; Kim, D.-G.; McGlumphy, E.A.; Lee, D.J.; Yilmaz, B. Positional Accuracy of a Prosthetic Treatment Plan Incorporated into a Cone Beam Computed Tomography Scan Using Surface Scan Registration. J. Prosthet. Dent. 2018, 120, 367–374. [Google Scholar] [CrossRef]
- Wakam, R.; Riom, S.; Leroy, M.; Dehurtevent, M. Impact of Spatial Representation on the Quality of Prosthodontic Procedures. Eur. J. Dent. Educ. 2025, 29, 219–227. [Google Scholar] [CrossRef]
- May, K.B.; Edge, M.J.; Russell, M.M.; Razzoog, M.E.; Lang, B.R. The Precision of Fit at the Implant Prosthodontic Interface. J. Prosthet. Dent. 1997, 77, 497–502. [Google Scholar] [CrossRef]
- Aldowish, A.F.; Alsubaie, M.N.; Alabdulrazzaq, S.S.; Alsaykhan, D.B.; Alamri, A.K.; Alhatem, L.M.; Algoufi, J.F.; Alayed, S.S.; Aljadani, S.S.; Alashjai, A.M.; et al. Occlusion and Its Role in the Long-Term Success of Dental Restorations: A Literature Review. Cureus 2024, 16, 11. [Google Scholar] [CrossRef]
- Abduo, J.; Tennant, M.; McGeachie, J. Lateral Occlusion Schemes in Natural and Minimally Restored Permanent Dentition: A Systematic Review. J. Oral Rehabil. 2013, 40, 788–802. [Google Scholar] [CrossRef]
- Silvester, C.M.; Kullmer, O.; Hillson, S. A Dental Revolution: The Association between Occlusion and Chewing Behaviour. PLoS ONE 2021, 16, e0261404. [Google Scholar] [CrossRef]
- Schwendicke, F.; Krois, J. Precision Dentistry—What It Is, Where It Fails (yet), and How to Get There. Clin. Oral Investig. 2022, 26, 3395–3403. [Google Scholar] [CrossRef]
- Patras, M.; Kourtis, S.; Sykaras, N. Creating Natural-Looking Removable Prostheses: Combining Art and Science to Imitate Nature. J. Esthet. Restor. Dent. 2012, 24, 160–168. [Google Scholar] [CrossRef]
- Fiorillo, L.; D’Amico, C.; Gorassini, F.; Varrà, M.; Parbonetti, E.; Varrà, S.; Ronsivalle, V.; Cervino, G. Innovating Prosthodontic Rehabilitation: A Streamlined Two-Step Technique for Mobile Denture Fabrication. Prosthesis 2024, 6, 527–539. [Google Scholar] [CrossRef]
- Park, C. A Comprehensive Narrative Review Exploring the Current Landscape of Digital Complete Denture Technology and Advancements. Heliyon 2025, 11, e41870. [Google Scholar] [CrossRef]
- Yeslam, H.E.; Freifrau Von Maltzahn, N.; Nassar, H.M. Revolutionizing CAD/CAM-Based Restorative Dental Processes and Materials with Artificial Intelligence: A Concise Narrative Review. PeerJ 2024, 12, e17793. [Google Scholar] [CrossRef]
- Cioloca Holban, C.; Tatarciuc, M.; Vitalariu, A.M.; Vasluianu, R.-I.; Antohe, M.; Diaconu, D.A.; Stamatin, O.; Dima, A.M. Three-Dimensional Printing and CAD/CAM Milling in Prosthodontics: A Scoping Review of Key Metrics Towards Future Perspectives. J. Clin. Med. 2025, 14, 4837. [Google Scholar] [CrossRef]
- Mangano, F.G.; Yang, K.R.; Lerner, H.; Admakin, O.; Mangano, C. Artificial Intelligence and Mixed Reality for Dental Implant Planning: A Technical Note. Clin. Implant Dent. Relat. Res. 2024, 26, 942–953. [Google Scholar] [CrossRef]
- Puleio, F.; Tosco, V.; Pirri, R.; Simeone, M.; Monterubbianesi, R.; Lo Giudice, G.; Lo Giudice, R. Augmented Reality in Dentistry: Enhancing Precision in Clinical Procedures—A Systematic Review. Clin. Pract. 2024, 14, 2267–2283. [Google Scholar] [CrossRef]
- Mai, H.-N.; Dam, V.V.; Lee, D.-H. Accuracy of Augmented Reality–Assisted Navigation in Dental Implant Surgery: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2023, 25, e42040. [Google Scholar] [CrossRef]
- Lobo, S.; Argolinha, I.; Machado, V.; Botelho, J.; Rua, J.; Li, J.; Mendes, J.J. Advances in Digital Technologies in Dental Medicine: Enhancing Precision in Virtual Articulators. JCM 2025, 14, 1495. [Google Scholar] [CrossRef]
- Huang, Y.; Hu, Y.; Chan, U.; Lai, P.; Sun, Y.; Dai, J.; Cheng, X.; Yang, X. Student Perceptions toward Virtual Reality Training in Dental Implant Education. PeerJ 2023, 11, e14857. [Google Scholar] [CrossRef]
- Neoa, K.C.P.; Tanb, Q.W.; Sivakumarc, I.; Buzayand, M.M. Full Mouth Rehabilitation of Failed Implants Prosthesis: A Case Report. AOS 2023, 18, 51–62. [Google Scholar] [CrossRef]
- Avila-Ortiz, G.; Vegh, D.; Mukaddam, K.; Galindo-Moreno, P.; Pjetursson, B.; Payer, M. Treatment Alternatives for the Rehabilitation of the Posterior Edentulous Maxilla. Periodontology 2000 2023, 93, 183–204. [Google Scholar] [CrossRef]
- Katić, D.; Spengler, P.; Bodenstedt, S.; Castrillon-Oberndorfer, G.; Seeberger, R.; Hoffmann, J.; Dillmann, R.; Speidel, S. A System for Context-Aware Intraoperative Augmented Reality in Dental Implant Surgery. Int. J. CARS 2015, 10, 101–108. [Google Scholar] [CrossRef]
- Shen, Y.; Wang, S.; Shen, Y.; Hu, J. The Application of Augmented Reality Technology in Perioperative Visual Guidance: Technological Advances and Innovation Challenges. Sensors 2024, 24, 7363. [Google Scholar] [CrossRef]
- Mosch, R.; Alevizakos, V.; Ströbele, D.A.; Schiller, M.; Von See, C. Exploring Augmented Reality for Dental Implant Surgery: Feasibility of Using Smartphones as Navigation Tools. Clin. Amp. Exp. Dent. Res. 2025, 11, e70110. [Google Scholar] [CrossRef]
- Alikhasi, M.; Yousefi, P.; Afrashtehfar, K.I. Smile Design. Dent. Clin. N. Am. 2022, 66, 477–487. [Google Scholar] [CrossRef]
- Yue, Z.; Luo, Z.; Hou, J.; Zhang, H. Application of 3D Digital Smile Design Based on Virtual Articulation Analysis in Esthetic Dentistry: A Technique. J. Prosthet. Dent. 2025, 133, 24–30. [Google Scholar] [CrossRef]
- Ahmed, W.M.; Azhari, A.A.; Sedayo, L.; Alhaid, A.; Alhandar, R.; Almalki, A.; Jahlan, A.; Almutairi, A.; Kheder, W. Mapping the Landscape of the Digital Workflow of Esthetic Veneers from Design to Cementation: A Systematic Review. Dent. J. 2024, 12, 28. [Google Scholar] [CrossRef]
- Fayad, M.I.; Ahmed, M.A.; Kothayer, M.; Aboelnagga, M.M.; Essa, E.E.S.F.; Abu-Hammad, O.; Moussa, R. Innovations Driving the Future of Maxillofacial Prosthetics, Part I: The Technological Leap in Maxillofacial Rehabilitation. Eur. J. Dent. 2025. [Google Scholar] [CrossRef]
- Sengupta, C.; Singh, R.K.; Gorde, K.; Kamble, A.D.; Bomble, N.A.; Kamat, A.R. AI-Driven Digital Prosthodontics—A Paradigm Shift in Prosthetic Rehabilitation. J. Neonatal Surg. 2025, 14, 233–238. [Google Scholar] [CrossRef]
- Sun, Y. Prosthesis Repair of Oral Implants Based on Artificial Intelligenc’e Finite Element Analysis. SLAS Technol. 2024, 29, 100226. [Google Scholar] [CrossRef]
- Dzyuba, N.; Jandu, J.; Yates, J.; Kushnerev, E. Virtual and Augmented Reality in Dental Education: The Good, the Bad and the Better. Eur. J. Dent. Educ. 2025, 29, 497–515. [Google Scholar] [CrossRef]
- Lin, P.-Y.; Chen, T.-C.; Lin, C.-J.; Huang, C.-C.; Tsai, Y.-H.; Tsai, Y.-L.; Wang, C.-Y. The Use of Augmented Reality (AR) and Virtual Reality (VR) in Dental Surgery Education and Practice: A Narrative Review. J. Dent. Sci. 2024, 19, S91–S101. [Google Scholar] [CrossRef]
- Leung, A.L.-S.; Yeung, C.; Chu, S.; Wong, A.W.-Y.; Yu, O.Y.; Chu, C.-H. Use of Computer Simulation in Dental Training with Special Reference to Simodont. Dent. J. 2021, 9, 125. [Google Scholar] [CrossRef]
- Hsu, M.-H.; Yang, H.-W.; Liu, C.-M.; Chen, C.-J.; Chang, Y.-C. Clinical Relevant Haptic Simulation Learning and Training in Tooth Preparation. J. Dent. Sci. 2022, 17, 1454–1457. [Google Scholar] [CrossRef] [PubMed]
- Towers, A.; Dixon, J.; Field, J.; Martin, R.; Martin, N. Combining Virtual Reality and 3D-printed Models to Simulate Patient-specific Dental Operative Procedures—A Study Exploring Student Perceptions. Eur. J. Dent. Educ. 2022, 26, 393–403. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; He, Y.; Chen, Y.; Liu, J.; Jin, Q.; Xu, S.; Fu, X.; Qiao, J.; Yu, B.; Niu, F. Virtual Reality and Three-Dimensional Printed Models Improve the Morphological Understanding in Learning Mandibular Sagittal Split Ramus Osteotomy: A Randomized Controlled Study. Front. Surg. 2021, 8, 705532. [Google Scholar] [CrossRef]
- Durham, M.; Engel, B.; Ferrill, T.; Halford, J.; Singh, T.P.; Gladwell, M. Digitally Augmented Learning in Implant Dentistry. Oral Maxillofac. Surg. Clin. N. Am. 2019, 31, 387–398. [Google Scholar] [CrossRef]
- Chahartangi, F.; Zarifsanaiey, N.; Mehrabi, M.; Ghoochani, B.Z. Integrating Augmented Reality Virtual Patients into Healthcare Training: A Scoping Review of Learning Design and Technical Requirements. PLoS ONE 2025, 20, e0324740. [Google Scholar] [CrossRef]
- Koolivand, H.; Shooreshi, M.M.; Safari-Faramani, R.; Borji, M.; Mansoory, M.S.; Moradpoor, H.; Bahrami, M.; Azizi, S.M. Comparison of the Effectiveness of Virtual Reality-Based Education and Conventional Teaching Methods in Dental Education: A Systematic Review. BMC Med. Educ. 2024, 24, 8. [Google Scholar] [CrossRef]
- Fu, Y.; Chu, F.; Lu, X.; Wang, C.; Xiao, N.; Jiang, J.; Zheng, J.; Jiang, H. Assessment and Evaluation of Online Education and Virtual Simulation Technology in Dental Education: A Cross-Sectional Survey. BMC Med. Educ. 2024, 24, 191. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Peters, M.D.; Godfrey, C.; McInerney, P.; Munn, Z.; Tricco, A.C.; Khalil, H. Scoping Reviews. In JBI Manual for Evidence Synthesis; Aromataris, E., Lockwood, C., Porritt, K., Pilla, B., Jordan, Z., Eds.; JBI: Adelaide, Australia, 2024; ISBN 9780648848820. [Google Scholar]
- Alharbi, N.M.; Osman, R.B. Augmented Reality Assisted Intraoral Scanning of Mandibular Arch: A Proof-of-Concept Pilot Clinical Study. J. Dent. 2024, 150, 105351. [Google Scholar] [CrossRef]
- Liu, L.; Wang, X.; Guan, M.; Fan, Y.; Yang, Z.; Li, D.; Bai, Y.; Li, H. A Mixed Reality-Based Navigation Method for Dental Implant Navigation Method: A Pilot Study. Comput. Biol. Med. 2023, 154, 106568. [Google Scholar] [CrossRef] [PubMed]
- Tao, B.; Fan, X.; Wang, F.; Chen, X.; Shen, Y.; Wu, Y. Comparison of the Accuracy of Dental Implant Placement Using Dynamic and Augmented Reality-Based Dynamic Navigation: An In Vitro Study. J. Dent. Sci. 2024, 19, 196–202. [Google Scholar] [CrossRef]
- Obispo, C.; Gragera, T.; Giovannini, G.; Zubizarreta-Macho, Á.; Aragoneses Lamas, J.M. Influence of Augmented Reality Appliances on Tooth Preparation Designs—An In Vitro Study. JPM 2023, 14, 37. [Google Scholar] [CrossRef] [PubMed]
- Kihara, T.; Keller, A.; Ogawa, T.; Armand, M.; Martin-Gomez, A. Evaluating the Feasibility of Using Augmented Reality for Tooth Preparation. J. Dent. 2024, 148, 105217. [Google Scholar] [CrossRef]
- Lin, Y.; Yau, H.; Wang, I.; Zheng, C.; Chung, K. A Novel Dental Implant Guided Surgery Based on Integration of Surgical Template and Augmented Reality. Clin. Implant Dent. Relat. Res. 2015, 17, 543–553. [Google Scholar] [CrossRef]
- Pellegrino, G.; Mangano, C.; Mangano, R.; Ferri, A.; Taraschi, V.; Marchetti, C. Augmented Reality for Dental Implantology: A Pilot Clinical Report of Two Cases. BMC Oral Health 2019, 19, 158. [Google Scholar] [CrossRef]
- Shusterman, A.; Nashef, R.; Tecco, S.; Mangano, C.; Mangano, F. Implant Placement Using Mixed Reality-Based Dynamic Navigation: A Proof of Concept. J. Dent. 2024, 149, 105256. [Google Scholar] [CrossRef]
- Daud, A.; Matoug-Elwerfelli, M.; Daas, H.; Zahra, D.; Ali, K. Enhancing Learning Experiences in Pre-Clinical Restorative Dentistry: The Impact of Virtual Reality Haptic Simulators. BMC Med. Educ. 2023, 23, 948. [Google Scholar] [CrossRef]
- Mai, H.-N.; Kim, Y.-G.; Cho, S.-H.; Joda, T.; Lee, D.-H. Enhancing Dental Education with a 3D Point Cloud Comparison and Augmented Reality for Auto-Evaluation of Fixed Prosthodontic Practice: An In Vitro Study. J. Dent. 2025, 153, 105493. [Google Scholar] [CrossRef]
- Grad, P.; Przeklasa-Bierowiec, A.M.; Malinowski, K.P.; Witowski, J.; Proniewska, K.; Tatoń, G. Application of HoloLens -based Augmented Reality and Three-dimensional Printed Anatomical Tooth Reference Models in Dental Education. Anat. Sci. Ed. 2023, 16, 743–755. [Google Scholar] [CrossRef]
- Özdemir, G.; Albayrak, B.; Yüzbaşioğlu, E.; Ölçer Us, Y. Virtual Articulators, Virtual Occlusal Records and Virtual Patients in Dentistry. J. Exp. Clin. Med. 2021, 38, 129–135. [Google Scholar] [CrossRef]
- Li, Y.; Ye, H.; Ye, F.; Liu, Y.; Lv, L.; Zhang, P.; Zhang, X.; Zhou, Y. The Current Situation and Future Prospects of Simulators in Dental Education. J. Med. Internet Res. 2021, 23, e23635. [Google Scholar] [CrossRef]
- Mansoory, M.S.; Azizi, S.M.; Mirhosseini, F.; Yousefi, D.; Moradpoor, H. A Study to Investigate the Effectiveness of the Application of Virtual Reality Technology in Dental Education. BMC Med. Educ. 2022, 22, 457. [Google Scholar] [CrossRef]
- Alsufyani, N.; Alnamlah, S.; Mutaieb, S.; Alageel, R.; AlQarni, M.; Bukhari, A.; Alhajri, M.; AlSubaie, A.; Alabdulkarim, M.; Faden, A. Virtual Reality Simulation of Panoramic Radiographic Anatomy for Dental Students. J. Dent. Educ. 2023, 87, 1200–1209. [Google Scholar] [CrossRef]
- Arora, O.; Sivaswamy, V.; Ahmed, N.; Ganapathy, D. Effectiveness of Digital Visualization in Teaching Crown Preparation to Predoctoral Dental Students—A Pilot Study. J. Popul. Ther. Clin. Pharmacol. 2023, 30, 168–173. [Google Scholar] [CrossRef]
- Hsu, M.-H.; Chang, Y.-C. Prediction of Dental Students’ Pre-Clinical Crown Preparation Performances by a Virtual Reality Haptic-Based Dental Simulator. J. Dent. Sci. 2025, 20, 2301–2306. [Google Scholar] [CrossRef]
- Liebermann, A.; Bjelopavlovic, M.; Rauch, A.; Schlenz, M.A.; Erdelt, K. Assessment of a Virtual Prosthetic Case Planning Environment for Dental Education—A Multicentric Analysis. Eur. J. Dent. Educ. 2024, 28, 275–286. [Google Scholar] [CrossRef]
- Najeeb, M.; Islam, S. Artificial Intelligence (AI) in Restorative Dentistry: Current Trends and Future Prospects. BMC Oral Health 2025, 25, 592. [Google Scholar] [CrossRef]
- Alghauli, M.A.; Aljohani, W.; Almutairi, S.; Aljohani, R.; Alqutaibi, A.Y. Advancements in Digital Data Acquisition and CAD Technology in Dentistry: Innovation, Clinical Impact, and Promising Integration of Artificial Intelligence. Clin. Ehealth 2025, 8, 32–52. [Google Scholar] [CrossRef]
- Elhag, H.H.M.; Rao, G.K.L.; Noor, S.N.F.B.M.; Zakaria, M.N.B.; Mokhtar, N.B. Augmented Reality in Dental Implants: A Systematic Review. JCDR 2024, 18, ZE20–ZE25. [Google Scholar] [CrossRef]
- Lal, A.; Nooruddin, A.; Umer, F. Concerns Regarding Deployment of AI-Based Applications in Dentistry—A Review. BDJ Open 2025, 11, 27. [Google Scholar] [CrossRef]
- Joachim, M.V.; Miloro, M. The Evolution of Virtual Surgical Planning in Craniomaxillofacial Surgery: A Comprehensive Review. J. Oral Maxillofac. Surg. 2025, 83, 294–306. [Google Scholar] [CrossRef]
- Felszeghy, S.; Mutluay, M.; Liukkonen, M.; Flacco, N.; Bakr, M.M.; Rampf, S.; Schick, S.; Mushtaq, F.; Sittoni-Pino, M.F.; Ackerman, K.; et al. Benefits and Challenges of the Integration of Haptics-enhanced Virtual Reality Training Within Dental Curricula. J. Dent. Educ. 2025, 89, 1070–1083. [Google Scholar] [CrossRef] [PubMed]
- Langove, S.A.; Khan, A. Automated Grading and Feedback Systems: Reducing Teacher Workload and Improving Student Performance. J. Asian Dev. Stud. 2024, 13, 202–212. [Google Scholar] [CrossRef]
- Khalid, T.; Yaqoob, H.; Syed, F.A.; Kazmi, S.M.R. Assessing Availability and Trainees’ Perceptions of Simulation and Augmented Reality in Prosthodontics Postgraduate Education in Pakistan: A Cross-Sectional Study. BMC Med. Educ. 2024, 24, 1541. [Google Scholar] [CrossRef]
- Wang, B.; Zheng, Y.; Han, X.; Kong, L.; Xiao, G.; Xiao, Z.; Chen, S. A Systematic Literature Review on Integrating AI-Powered Smart Glasses into Digital Health Management for Proactive Healthcare Solutions. npj Digit. Med. 2025, 8, 410. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Gómez-Polo, M.; Vyas, S.; Barmak, A.B.; Gallucci, G.O.; Att, W.; Özcan, M.; Krishnamurthy, V.R. Artificial Intelligence Models for Tooth-Supported Fixed and Removable Prosthodontics: A Systematic Review. J. Prosthet. Dent. 2023, 129, 276–292. [Google Scholar] [CrossRef]
- Schwendicke, F.; Samek, W.; Krois, J. Artificial Intelligence in Dentistry: Chances and Challenges. J. Dent. Res. 2020, 99, 769–774. [Google Scholar] [CrossRef] [PubMed]
- Arunjaroensuk, S.; Yotpibulwong, T.; Fu, P.-S.; Wang, J.-C.; Hung, C.-C.; Mattheos, N.; Pimkhaokham, A. Implant Position Accuracy Using Dynamic Computer-Assisted Implant Surgery (CAIS) Combined with Augmented Reality: A Randomized Controlled Clinical Trial. J. Dent. Sci. 2024, 19, S44–S50. [Google Scholar] [CrossRef] [PubMed]
| Category | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Study Designs | - RCTs, cohort studies, case–control studies, quasi-experimental studies, technical reports. | - Editorials, opinion pieces, letters. - Non-English studies *. - Pediatric and animal studies. |
| Population | - Dental professionals (dentists, prosthodontists, technicians). - Dental students (undergraduate/postgraduate). - AR applications in prosthodontics (implants, crowns, dentures) or prosthodontic education. | - Non-dental populations. - AR applications in other domains and dentistry specialties (e.g., orthodontics, endodontics). |
| Concept | - AR in ITSP practice: Implant placement, crown prep, intraoral scanning, and occlusal analysis. - AR in ITSP Education: Preclinical training, virtual simulations, skill assessment. | - Non-prosthodontic AR uses. - Hardware-focused studies without prosthodontic application. |
| Context | - Peer-reviewed journals, clinical trials, in vitro studies, technical reports. - Publication date: 2015–2025. | - Studies without empirical data (e.g., theoretical frameworks). - Duplicate publications. |
| Other | - Studies where AR is the primary intervention. | - General digital dentistry tools without AR. - Insufficient methodological detail. |
| Study (Year) | Study Type/Design | Extraction Focus |
|---|---|---|
| Alharbi & Osman (2024) [44] | Pilot clinical study | AR-assisted intraoral scanning efficiency |
| Liu et al. (2023) [45] | In vitro randomized study | MR-based implant navigation accuracy |
| Tao et al. (2024) [46] | In vitro comparative study | ARDN vs. DN implant accuracy |
| Obispo et al. (2023) [47] | In vitro controlled experiment | AR-guided tooth preparation precision |
| Kihara et al. (2024) [48] | Experimental comparative study (n = 24) | AR HMDs for tooth preparation safety |
| Lin et al. (2015) [49] | In vitro feasibility study | AR + surgical template for implants |
| Pellegrino et al. (2019) [50] | Case report (clinical pilot, n = 2) | HoloLens for implant navigation |
| Shusterman et al. (2024) [51] | Proof-of-concept clinical case | MR-DN system feasibility |
| Daud et al. (2023) [52] | Interventional study (n = 23) | VR haptic simulators in pre-clinical training |
| Mai et al. (2025) [53] | In vitro validation study | 3D AR auto-evaluation algorithm |
| Grad et al. (2023) [54] | Mixed-methods study (quant + qual) | AR vs. 3D-printed models for anatomy |
| Özdemir et al. (2021) [55] | Review | Virtual articulators in education |
| Li et al. (2021) [56] | Review | VR simulators in dental education |
| Mansoory et al. (2022) [57] | RCT (educational intervention, n = 50) | VR effectiveness in prosthodontic training |
| Alsufyani et al. (2023) [58] | Educational simulation study (n = 69) | VR vs. lectures for radiographic anatomy |
| Arora et al. (2023) [59] | Comparative educational study (n = 24) | Haptic vs. conventional crown preparation |
| Hsu & Chang (2025) [60] | Retrospective cohort (n = 84) | Simodont predictive validity |
| Liebermann et al. (2024) [61] | Mixed-methods study (survey + evaluation) | Virtual prosthetic case planning usability |
| Study (Year) | AR Device/Software | Application | Outcome Measures | Key Findings |
|---|---|---|---|---|
| AR in ITSP Practice | ||||
| Alharbi & Osman (2024) [44] | Magic Leap 2 (ML2) | Intraoral scanning | Scan time, image count, trueness (RMSE) | AR reduced scan time (44 s vs. 63 s) and images (836 vs. 1209) (p < 0.001). |
| Liu et al. (2023) [45] | HoloLens + NDI Polaris tracking | Implant placement | Entry/apex/angular deviations | MR navigation reduced deviations (entry: 0.69 mm vs. 1.57 mm, p = 0.000). |
| Tao et al. (2024) [46] | AR-based dynamic navigation (ARDN) | Implant placement | Coronal/apical/angular deviations | ARDN had higher angular deviation (3.72° vs. 3.1°, p = 0.02). |
| Obispo et al. (2023) [47] | AR appliance | Tooth preparation for crowns | Volumetric reduction, RMS alignment | AR improved precision (p = 0.0001) and conservatism. |
| Kihara et al. (2024) [48] | AR head-mounted display (HMD) | Tooth preparation | Over-reduction, angle accuracy | Cross-sectional AR reduced over-reduction (p < 0.05). |
| Lin et al. (2015) [49] | AR head-mounted display | Implant placement with surgical template | Entry/apex/angular/depth deviations | AR reduced deviations (entry: 0.50 mm, angle: 2.70°). |
| Pellegrino et al. (2019) [50] | HoloLens | Implant placement | Entry/apex/angular deviations | Feasibility confirmed (entry: 0.53 mm, angle: 3.05°). |
| Shusterman et al. (2024) [51] | ANNA® (MR-DN system) | Implant placement | 3D entry/apex deviations, angle | High accuracy (entry: 0.42 mm, angle: 1.85°). |
| AR in ITSP Education | ||||
| Daud et al. (2023) [52] | VR haptic simulator (unspecified) | Preclinical restorative training | Student perceptions, skill improvement | 76% of students endorsed VR for supplemental training. |
| Mai et al. (2025) [53] | 3D AR auto-evaluation algorithm | Tooth preparation evaluation | RMSE, time efficiency, user satisfaction | Reduced evaluation time (10.5 s vs. 2 h) (ICC = 0.75–0.95). |
| Grad et al. (2023) [54] | Microsoft HoloLens | Dental anatomy reconstruction | Hausdorff distance (Hmax) | 3D-printed models outperformed AR (630 µm vs. AR, p = 0.004). |
| Özdemir et al. (2021) [55] | Virtual articulators | Occlusion analysis | Subjective usability | Enhanced dynamic occlusion teaching. |
| Li et al. (2021) [56] | VR simulators (multiple) | Preclinical skill training | Literature review | VR useful but limited by force feedback realism. |
| Mansoory et al. (2022) [57] | VR technology EKEN 4KUHD | Neutral zone/teeth arrangement | Test scores, student feedback | VR group scored higher (16.92 vs. 16.14, p < 0.05). |
| Alsufyani et al. (2023) [58] | VR panoramic anatomy software | Radiographic anatomy training | Landmark identification, satisfaction | Lecture-based outperformed VR (p < 0.005), but VR was engaging. |
| Arora et al. (2023) [59] | Virteasy haptic simulator | Crown preparation training | Preparation quality | Haptic simulators improved skills but conventional was better later (p < 0.05). |
| Hsu & Chang (2025) [60] | Simodont haptic simulator | Crown preparation prediction | Correlation with phantom head test | Simodont predicted success (OR = 5.6, p < 0.001). |
| Liebermann et al. (2024) [61] | Virtual prosthetic case planning app | Prosthetic case planning | Lecturer/student feedback | 87% recommended integration into curricula. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosu, S.N.; Tatarciuc, M.S.; Vitalariu, A.M.; Lupu, I.-C.; Diaconu, D.A.; Vasluianu, R.-I.; Holban, C.C.; Dima, A.M. Augmented Reality in Implant and Tooth-Supported Prosthodontics Practice and Education: A Scoping Review. Dent. J. 2025, 13, 435. https://doi.org/10.3390/dj13090435
Rosu SN, Tatarciuc MS, Vitalariu AM, Lupu I-C, Diaconu DA, Vasluianu R-I, Holban CC, Dima AM. Augmented Reality in Implant and Tooth-Supported Prosthodontics Practice and Education: A Scoping Review. Dentistry Journal. 2025; 13(9):435. https://doi.org/10.3390/dj13090435
Chicago/Turabian StyleRosu, Sorana Nicoleta, Monica Silvia Tatarciuc, Anca Mihaela Vitalariu, Iulian-Costin Lupu, Diana Antonela Diaconu, Roxana-Ionela Vasluianu, Catalina Cioloca Holban, and Ana Maria Dima. 2025. "Augmented Reality in Implant and Tooth-Supported Prosthodontics Practice and Education: A Scoping Review" Dentistry Journal 13, no. 9: 435. https://doi.org/10.3390/dj13090435
APA StyleRosu, S. N., Tatarciuc, M. S., Vitalariu, A. M., Lupu, I.-C., Diaconu, D. A., Vasluianu, R.-I., Holban, C. C., & Dima, A. M. (2025). Augmented Reality in Implant and Tooth-Supported Prosthodontics Practice and Education: A Scoping Review. Dentistry Journal, 13(9), 435. https://doi.org/10.3390/dj13090435







