Evaluating the Effectiveness of Nasoalveolar Molding in the Management of Children with Unilateral Cleft Lip and Palate: A Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients Included in the Study
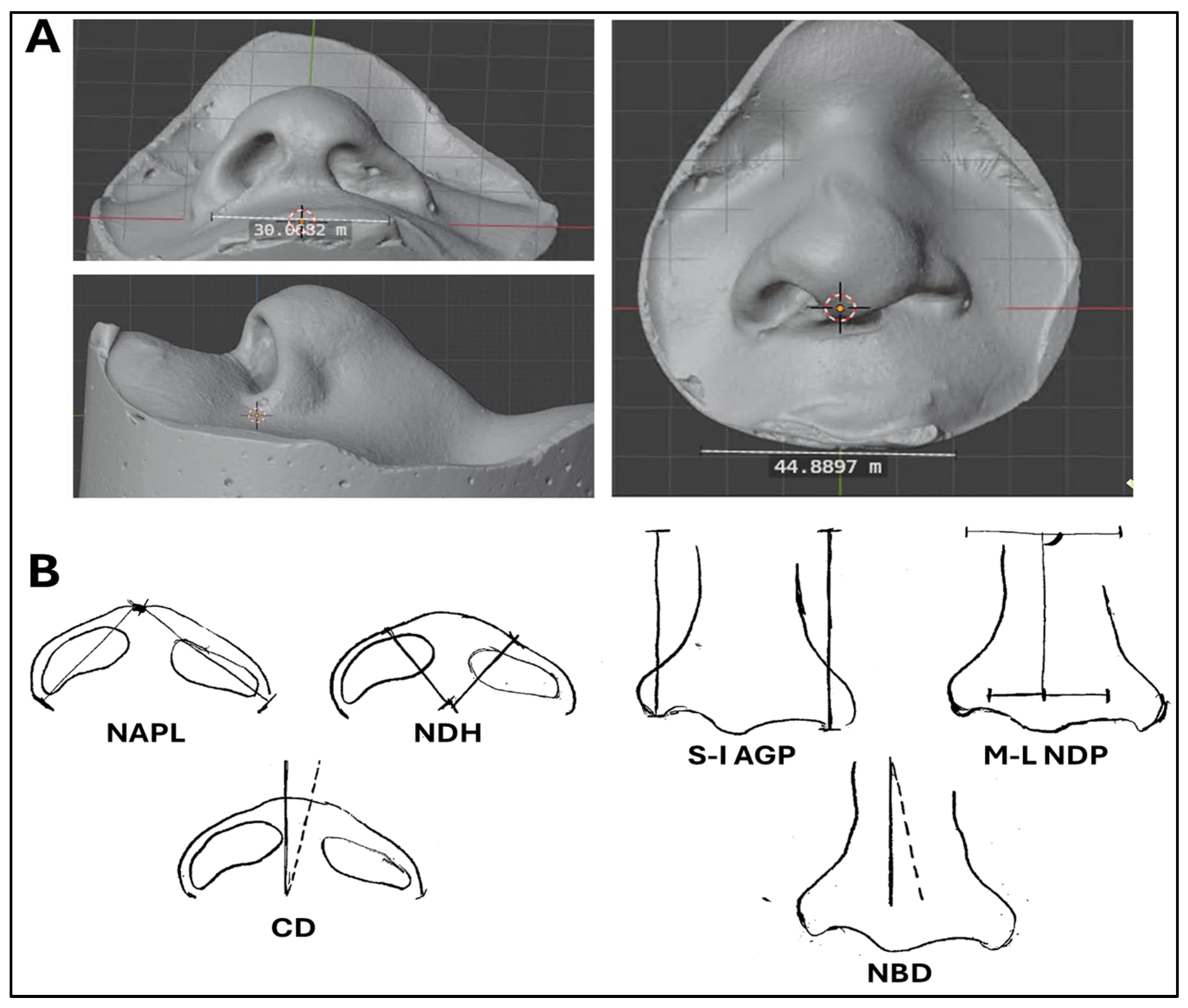
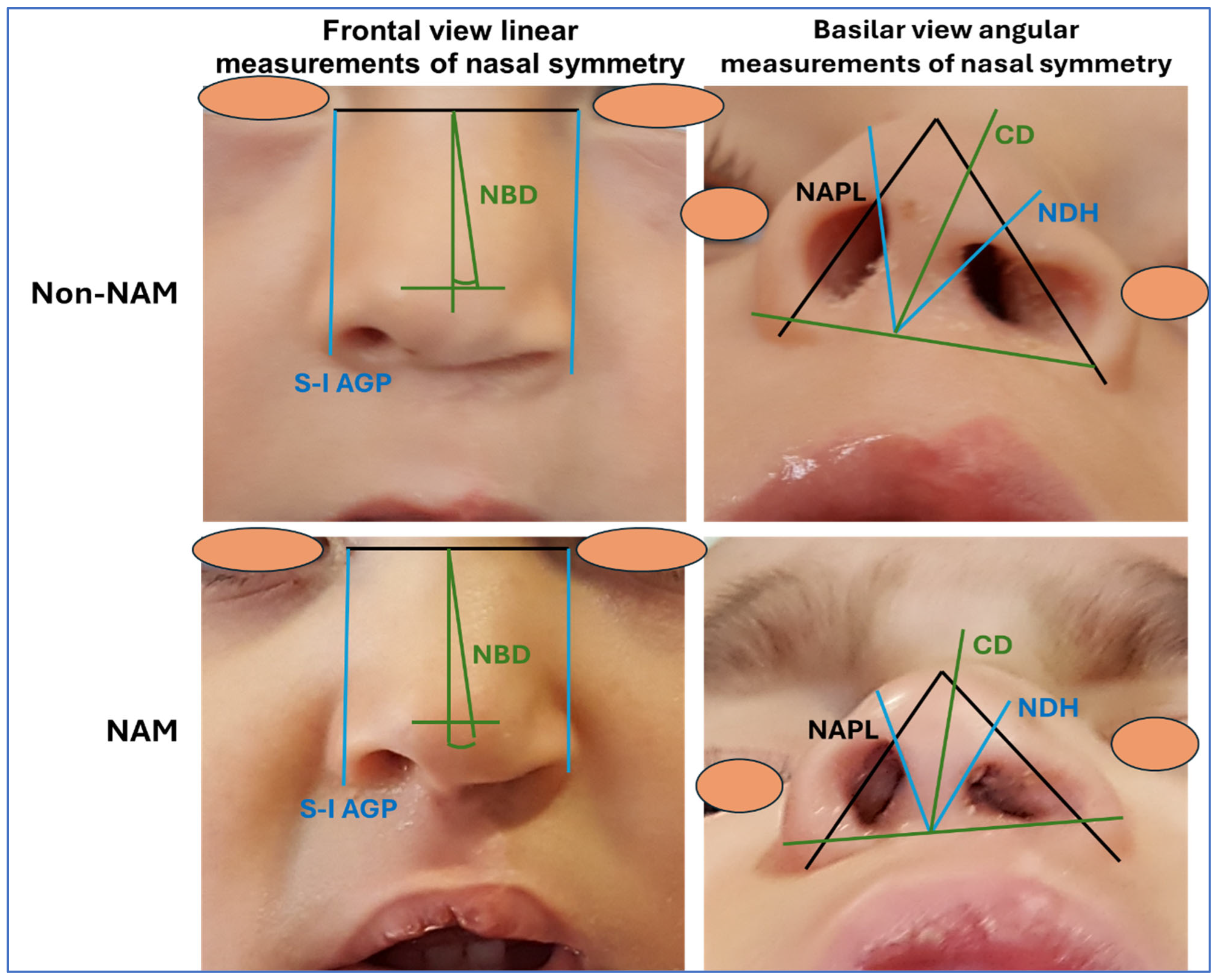
2.2. Obtaining Relevant Parameters of Nasal Symmetry
- Basilar view linear measurements of nasal symmetry: nasal ala projection length (NAPL) and nasal dome height (NDH). The NAPL is the distance between the nasal apex and the alar grooves, measured at the cleft side and at the non-cleft side of the nose. The NDH is the distance between the base of the columella and the points defining the tip of the nose, measured at each side of the nose.
- Basilar view angular measurements of nasal symmetry: columellar deviation (CD). This parameter is quantified by determining the deviation of the columella from the true vertical—the saggital plane of the nose. This measurement was obtained by drawing a line perpendicular to the line connecting the medial canthi of the eyes, and the angle formed between this line and the actual direction of the columella was determined. The ratio of this angular deviation to 90 degrees was calculated.
- Frontal view linear measurements of nasal symmetry: superoinferior alar groove position (S-I AGP) and mediolateral nasal dome position measurement (M-L NDP). The S-I AGP was determined as the distance from an imaginary line joining both medial canthi of the eyes to the alar groove, at each side of the nose (cleft and non-cleft sides). The M-L NDP was determined at each side of the nose as the distance between each alar groove and a vertical line bisecting the intracanthal distance along the horizontal plane.
- Frontal view angular measurements of nasal symmetry: nasal bridge deviation (NBD). This parameter was assessed as the angular deviation of the nasal bridge from the true vertical determined by drawing a plane perpendicular to the line formed by joining the medial canthi. The ratio of this angular measurement to 90 degrees was found and recorded.
2.3. Statistical Analysis
3. Results
3.1. Results of the Linear Measurements of Nasal Symmetry
3.2. Results of the Angular Measurements of Nasal Symmetry
3.3. Generation of a Predicting Model Using Binary Logistic Regression
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CD | Columellar deviation |
| M-L NDP | Nasal dome position |
| NAM | Nasoalveolar molding |
| NAPL | Nasal ala projection length |
| NBD | Nasal bridge deviation |
| NDH | Nasal dome height |
| S-I AGP | Superoinferior alar groove position |
| UCLP | Unilateral cleft lip and palate |
References
- Cornefjord, M.; Källén, K.; Klintö, K.; Stiernman, M.; Wiedel, A.-P.; Becker, M. Birth Prevalence of Cleft Lip and/or Palate—A Register Study of All Children Born in Sweden Years 2000–2020. J. Plast. Surg. Hand Surg. 2025, 60, 120–126. [Google Scholar] [CrossRef]
- Mai, C.T.; Isenburg, J.L.; Canfield, M.A.; Meyer, R.E.; Correa, A.; Alverson, C.J.; Lupo, P.J.; Riehle-Colarusso, T.; Cho, S.J.; Aggarwal, D.; et al. National Population-Based Estimates for Major Birth Defects, 2010–2014. Birth Defects Res. 2019, 111, 1420–1435. [Google Scholar] [CrossRef] [PubMed]
- Campbell, A.; Costello, B.J.; Ruiz, R.L. Cleft Lip and Palate Surgery: An Update of Clinical Outcomes for Primary Repair. Oral Maxillofac. Surg. Clin. N. Am. 2010, 22, 43–58. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, T.-Y.; Gengler, I.; Tollefson, T.T. Rhinoplasty for Patients with Cleft Lip-Palate: Functional and Aesthetic Concerns. Otolaryngol. Clin. N. Am. 2025, 58, 361–377. [Google Scholar] [CrossRef] [PubMed]
- Grayson, B.H.; Maull, D. Nasoalveolar Molding for Infants Born with Clefts of the Lip, Alveolus, and Palate. Semin. Plast. Surg. 2005, 19, 294–301. [Google Scholar] [CrossRef]
- Isaac, K.V.; Tan, R.A.; Ganske, I.M.; Mulliken, J.B. Beware the Alar Base Optical Illusion in Assessment of Unilateral Cleft Lip Nasal Deformity. Plast. Reconstr. Surg. 2019, 143, 1157. [Google Scholar] [CrossRef]
- Harrison, L.M.; Kenyon, L.; Mathew, D.P.; Derderian, C.A.; Hallac, R.R. Alar Asymmetry in Patients with Unilateral Cleft Lip: Implications for Secondary Rhinoplasty. Cleft Palate Craniofac. J. 2024, 61, 1324–1328. [Google Scholar] [CrossRef]
- Ye, J.; Wang, X.; Xiao, M. Current Treatment Progress of Unilateral Cleft Lip Nasal Deformities. Aesthetic Plast. Surg. 2024, 48, 4895–4901. [Google Scholar] [CrossRef]
- Saikia, A.; Muthu, M.S.; Orenuga, O.O.; Mossey, P.; Ousehal, L.; Yan, S.; Campodonico, M.; England, R.; Taylor, S.; Sheeran, P. Systematic Review of Clinical Practice Guidelines for Oral Health in Children with Cleft Lip and Palate. Cleft Palate Craniofac. J. 2022, 59, 800–814. [Google Scholar] [CrossRef]
- Padovano, W.M.; Skolnick, G.B.; Naidoo, S.D.; Snyder-Warwick, A.K.; Patel, K.B. Long-Term Effects of Nasoalveolar Molding in Patients with Unilateral Cleft Lip and Palate: A Systematic Review and Meta-Analysis. Cleft Palate Craniofac. J. 2022, 59, 462–474. [Google Scholar] [CrossRef]
- España-López, A.; Fernández-Valadés, R.; Cubiles, E.; Garzón, I.; Martin-Piedra, M.A.; Carriel, V.; Campos, F.; Martínez-Plaza, A.; Vallejo, D.; Liceras-Liceras, E.; et al. Phase I-IIa Clinical Trial to Evaluate the Safety, Feasibility and Efficacy of the Use of a Palate Mucosa Generated by Tissue Engineering for the Treatment of Children with Cleft Palate: The BIOCLEFT Study Protocol. BMJ Open 2024, 14, e093491. [Google Scholar] [CrossRef]
- Thiruvenkatachari, B.; Chakkaravarthi, S.; Bhuvaraghan, A. Effectiveness of Nasoalveolar Molding Treatment for Babies with Nonsyndromic Complete Unilateral Cleft Lip, Alveolus, and Palate: A Systematic Review and Meta-Analysis. Am. J. Orthod. Dentofac. Orthop. 2025, 168, 2–13.e4. [Google Scholar] [CrossRef]
- van der Heijden, P.; Dijkstra, P.U.; Stellingsma, C.; van der Laan, B.F.; Korsten-Meijer, A.G.W.; Goorhuis-Brouwer, S.M. Limited Evidence for the Effect of Presurgical Nasoalveolar Molding in Unilateral Cleft on Nasal Symmetry: A Call for Unified Research. Plast. Reconstr. Surg. 2013, 131, 62e–71e. [Google Scholar] [CrossRef] [PubMed]
- Esenlik, E.; Gibson, T.; Kassam, S.; Sato, Y.; Garfinkle, J.; Figueroa, A.A.; AlQatami, F.; Runyan, C.; Alperovich, M.; Golinko, M.S.; et al. NAM Therapy-Evidence-Based Results. Cleft Palate Craniofac. J. 2020, 57, 529–531. [Google Scholar] [CrossRef] [PubMed]
- Ahsanuddin, S.; Ahmed, M.; Slowikowski, L.; Heitzler, J. Recent Advances in Nasoalveolar Molding Therapy Using 3D Technology. Craniomaxillofac. Trauma Reconstr. 2022, 15, 387–396. [Google Scholar] [CrossRef]
- Chaudhari, A.A.; Vig, K.; Baganizi, D.R.; Sahu, R.; Dixit, S.; Dennis, V.; Singh, S.R.; Pillai, S.R. Future Prospects for Scaffolding Methods and Biomaterials in Skin Tissue Engineering: A Review. Int. J. Mol. Sci. 2016, 17, 1974. [Google Scholar] [CrossRef]
- Likitkulthanaporn, A.; Boonpratham, S.; Honglertnapakul, Y.; Saengfai, N.N.; Chaweewannakorn, C.; Jongkhum, N.; Peanchitlertkajorn, S. Effects of Nasoalveolar Molding on Nasolabial Aesthetics in Patients with Cleft Lip and Palate during Pre-Adolescence: A Systematic Review and Meta-Analysis of Retrospective Studies. Orthod. Craniofac. Res. 2024, 27, 350–363. [Google Scholar] [CrossRef] [PubMed]
- R, V.; Singhal, R.; Namdev, R.; Kumar, A.; Dayma, C.; Rani, A. Treatment Outcomes of Lip Taping in Patients with Non-Syndromic Cleft Lip and/or Palate: A Systematic Review and Meta-Analysis. Cleft Palate Craniofac. J. 2025, 62, 1281–1293. [Google Scholar] [CrossRef]
- Aminpour, S.; Tollefson, T.T. Recent Advances in Presurgical Molding in Cleft Lip and Palate. Curr. Opin. Otolaryngol. Head Neck Surg. 2008, 16, 339. [Google Scholar] [CrossRef]
- Ndem, I.E.; Kugar, M.; Caruso, D.; Duchesneau, E.; Agala, C.B.; Mehta, N.; Van Aalst, J.; Wood, J.S. A Retrospective Review on the Effects of Nasoalveolar Molding on Infant Weight Gain and Time to Primary Lip Repair in Unilateral and Bilateral Cleft Lip and Palate. J. Craniofac. Surg. 2024, 35, 1652–1655. [Google Scholar] [CrossRef]
- Jahanbin, A.; Alizadeh, F.L.; Bardideh, E.; Sharifi, S.; Nazari, M.S. Does Presurgical Nasoalveolar Molding Reduce the Need for Future Bone Grafting in Cleft Lip and Palate Patients? A Systematic Review and Meta-Analysis. J. Craniofac. Surg. 2022, 33, 2095. [Google Scholar] [CrossRef]
- Abbott, M.M.; Meara, J.G. Nasoalveolar Molding in Cleft Care: Is It Efficacious? Plast. Reconstr. Surg. 2012, 130, 659–666. [Google Scholar] [CrossRef]
- Moon, C.; Nam, I.; An, H.; Hwang, J.-Y.; Sim, S.; Hwang, D.-S. Comparative Analysis of Soft and Hard Tissue Outcomes Following Nasoalveolar Molding in Unilateral and Bilateral Cleft Lip and Palate: A Systematic Review. J. Craniofac. Surg. 2025, 10-1097. [Google Scholar] [CrossRef]
- Grayson, B.H.; Garfinkle, J.S. Early Cleft Management: The Case for Nasoalveolar Molding. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 134. [Google Scholar] [CrossRef] [PubMed]
- Barillas, I.; Dec, W.; Warren, S.M.; Cutting, C.B.; Grayson, B.H. Nasoalveolar Molding Improves Long-Term Nasal Symmetry in Complete Unilateral Cleft Lip-Cleft Palate Patients. Plast. Reconstr. Surg. 2009, 123, 1002–1006. [Google Scholar] [CrossRef]
- Harris, J.K. Primer on Binary Logistic Regression. Fam. Med. Community Health 2021, 9, e001290. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.S.; Henry, B.T.; Scott, M.A. Presurgical Dentofacial Orthopedic Management of the Cleft Patient. Oral Maxillofac. Surg. Clin. N. Am. 2016, 28, 169–176. [Google Scholar] [CrossRef]
- Papadopoulos, M.A.; Koumpridou, E.N.; Vakalis, M.L.; Papageorgiou, S.N. Effectiveness of Pre-Surgical Infant Orthopedic Treatment for Cleft Lip and Palate Patients: A Systematic Review and Meta-Analysis. Orthod. Craniofac. Res. 2012, 15, 207–236. [Google Scholar] [CrossRef]
- Wadde, K.; Chowdhar, A.; Venkatakrishnan, L.; Ghodake, M.; Sachdev, S.S.; Chhapane, A. Protocols in the Management of Cleft Lip and Palate: A Systematic Review. J. Stomatol. Oral Maxillofac. Surg. 2023, 124, 101338. [Google Scholar] [CrossRef] [PubMed]
- Thakur, G.; Bok, E.-Y.; Kim, S.-B.; Jo, C.-H.; Oh, S.-J.; Baek, J.-C.; Park, J.-E.; Kang, Y.-H.; Lee, S.-L.; Kumar, R.; et al. Scaffold-Free 3D Culturing Enhance Pluripotency, Immunomodulatory Factors, and Differentiation Potential of Wharton’s Jelly-Mesenchymal Stem Cells. Eur. J. Cell Biol. 2022, 101, 151245. [Google Scholar] [CrossRef]
- Suhk, J.; Park, J.; Nguyen, A.H. Nasal Analysis and Anatomy: Anthropometric Proportional Assessment in Asians—Aesthetic Balance from Forehead to Chin, Part I. Semin. Plast. Surg. 2015, 29, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-Y.; Lee, H.; Kim, J.-K.; Cho, J.; Park, J.H.; Jung, H.-D.; Jung, Y.-S. Three-Dimensional Analysis of Presurgical Nasoalveolar Molding Outcomes in Patients with Unilateral Cleft Lip and Palate: A Preliminary Study Using LED Surface Scanning Technology. J. Dent. 2024, 151, 105384. [Google Scholar] [CrossRef] [PubMed]
- Chiang, H.; Shah, R.; Washabaugh, C.; Frank-Ito, D.O. Nasal Airway Obstruction in Patients with Cleft Lip Nasal Deformity: A Systematic Review. J. Plast. Reconstr. Aesthetic Surg. JPRAS 2024, 92, 48–60. [Google Scholar] [CrossRef] [PubMed]
| NAPL | NDH | S-I AGP | M-L NDP | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | Females | Males | All | Females | Males | All | Females | Males | All | Females | Males | ||
| Non-NAM | Distance Cleft Side | 17.85 ± 3.58 | 16.75 ± 3.77 | 19.13 ± 3.16 | 9.72 ± 2.69 | 9.22 ± 3.27 | 10.31 ± 1.94 | 25.92 ± 4.89 | 24.79 ± 5.54 | 27.24 ± 4.08 | 7.86 ± 1.66 | 8.14 ± 1.46 | 7.54 ± 1.96 |
| Distance Non-Cleft Side | 16.39 ± 4.24 | 16.4 ± 4.93 | 16.38 ± 3.74 | 13.96 ± 2.28 | 13.58 ± 2.04 | 14.41 ± 2.65 | 27.93 ± 4.22 | 27.87 ± 4.78 | 28 ± 3.93 | 5.06 ± 1.93 | 5.45 ± 2.56 | 4.6 ± 0.76 | |
| Mean Difference Cleft Side vs. Non-Cleft Side | 1.46 ± 3.85 | 0.35 ± 4.67 | 2.76 ± 2.4 | −4.24 ± 2.47 | −4.36 ± 2.37 | −4.1 ± 2.8 | −2.01 ± 3.28 | −3.07 ± 3.21 | −0.76 ± 3.17 | 2.81 ± 2.7 | 2.69 ± 3.62 | 2.94 ± 1.31 | |
| % Difference Cleft vs. Non-Cleft Side | 5.05 ± 11.35 | 2.09 ± 13.51 | 8.49 ± 7.99 | −18.91 ± 11.75 | −21.05 ± 13.24 | −16.41 ± 10.34 | 10.45 ± 52.52 | −10.06 ± 56.8 | 34.38 ± 38.39 | 23.33 ± 44.55 | 5.98 ± 45.71 | 43.57 ± 36.64 | |
| NAM | Distance Cleft Side | 18.89 ± 3.26 | 18.19 ± 3.62 | 19.2 ± 3.16 | 14.29 ± 2.84 | 13.95 ± 2.51 | 14.44 ± 3.04 | 26.63 ± 3.94 | 27.69 ± 3.71 | 26.16 ± 4.07 | 6.82 ± 1.6 | 6.93 ± 2.01 | 6.77 ± 1.47 |
| Distance Non-Cleft Side | 18.74 ± 3.12 | 17.59 ± 3.09 | 19.25 ± 3.09 | 15.13 ± 3.14 | 14.84 ± 3.03 | 15.26 ± 3.28 | 26.97 ± 3.82 | 27.46 ± 3.67 | 26.75 ± 3.98 | 6.45 ± 1.57 | 6.81 ± 2 | 6.3 ± 1.39 | |
| Mean Difference Cleft Side-Non-Cleft Side | 0.15 ± 1.19 | 0.6 ± 1.44 | −0.05 ± 1.05 | −0.84 ± 1.5 | −0.89 ± 1.3 | −0.82 ± 1.61 | −0.34 ± 1.64 | 0.24 ± 1.26 | −0.59 ± 1.75 | 0.36 ± 1.11 | 0.12 ± 0.97 | 0.47 ± 1.18 | |
| % Difference Cleft vs. Non-Cleft Side | 0.33 ± 3.12 | 1.47 ± 3.46 | −0.17 ± 2.94 | −2.81 ± 4.75 | −2.9 ± 4.71 | −2.77 ± 4.93 | 6.27 ± 51.05 | 21.91 ± 47.99 | −0.58 ± 52.31 | 7.83 ± 50.69 | 21.48 ± 50.27 | 1.86 ± 51.31 | |
| Non-NAM vs. NAM | p Value (% Difference) | 0.0259 * | 0.5350 | 0.0104 * | <0.0001 * | 0.0175 * | 0.0001 * | 0.5804 | 0.9015 | 0.2030 | <0.0001 * | 0.0262 * | 0.0012 * |
| CD | NBD | |||||
|---|---|---|---|---|---|---|
| All | Females | Males | All | Females | Males | |
| Non-NAM | 9.62 ± 3.75 | 8.57 ± 4.86 | 10.83 ± 1.47 | 7.38 ± 3.38 | 8.71 ± 1.89 | 5.83 ± 4.22 |
| NAM | 6.39 ± 3.39 | 6.43 ± 3.82 | 6.38 ± 3.32 | 4.61 ± 2.74 | 4.71 ± 2.75 | 4.56 ± 2.83 |
| Non-NAM vs. NAM | 0.0121 * | 0.3829 | 0.0034 * | 0.0216 * | 0.0175 * | 0.6931 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
España-Guerrero, A.; España-Guerrero, E.; Liceras-Liceras, E.; Bullejos-Martínez, E.; Martínez-Plaza, A.; Alaminos, M.; Fernández-Valadés, R.; España-López, A. Evaluating the Effectiveness of Nasoalveolar Molding in the Management of Children with Unilateral Cleft Lip and Palate: A Cohort Study. Dent. J. 2025, 13, 394. https://doi.org/10.3390/dj13090394
España-Guerrero A, España-Guerrero E, Liceras-Liceras E, Bullejos-Martínez E, Martínez-Plaza A, Alaminos M, Fernández-Valadés R, España-López A. Evaluating the Effectiveness of Nasoalveolar Molding in the Management of Children with Unilateral Cleft Lip and Palate: A Cohort Study. Dentistry Journal. 2025; 13(9):394. https://doi.org/10.3390/dj13090394
Chicago/Turabian StyleEspaña-Guerrero, Alba, Enrique España-Guerrero, Esther Liceras-Liceras, Elena Bullejos-Martínez, Adoración Martínez-Plaza, Miguel Alaminos, Ricardo Fernández-Valadés, and Antonio España-López. 2025. "Evaluating the Effectiveness of Nasoalveolar Molding in the Management of Children with Unilateral Cleft Lip and Palate: A Cohort Study" Dentistry Journal 13, no. 9: 394. https://doi.org/10.3390/dj13090394
APA StyleEspaña-Guerrero, A., España-Guerrero, E., Liceras-Liceras, E., Bullejos-Martínez, E., Martínez-Plaza, A., Alaminos, M., Fernández-Valadés, R., & España-López, A. (2025). Evaluating the Effectiveness of Nasoalveolar Molding in the Management of Children with Unilateral Cleft Lip and Palate: A Cohort Study. Dentistry Journal, 13(9), 394. https://doi.org/10.3390/dj13090394








