Contemporary Magnetic Removable Partial Denture Utilizing a Novel Ultra-Thin Magnetic Attachment System
Abstract
1. Introduction
2. Materials and Methods
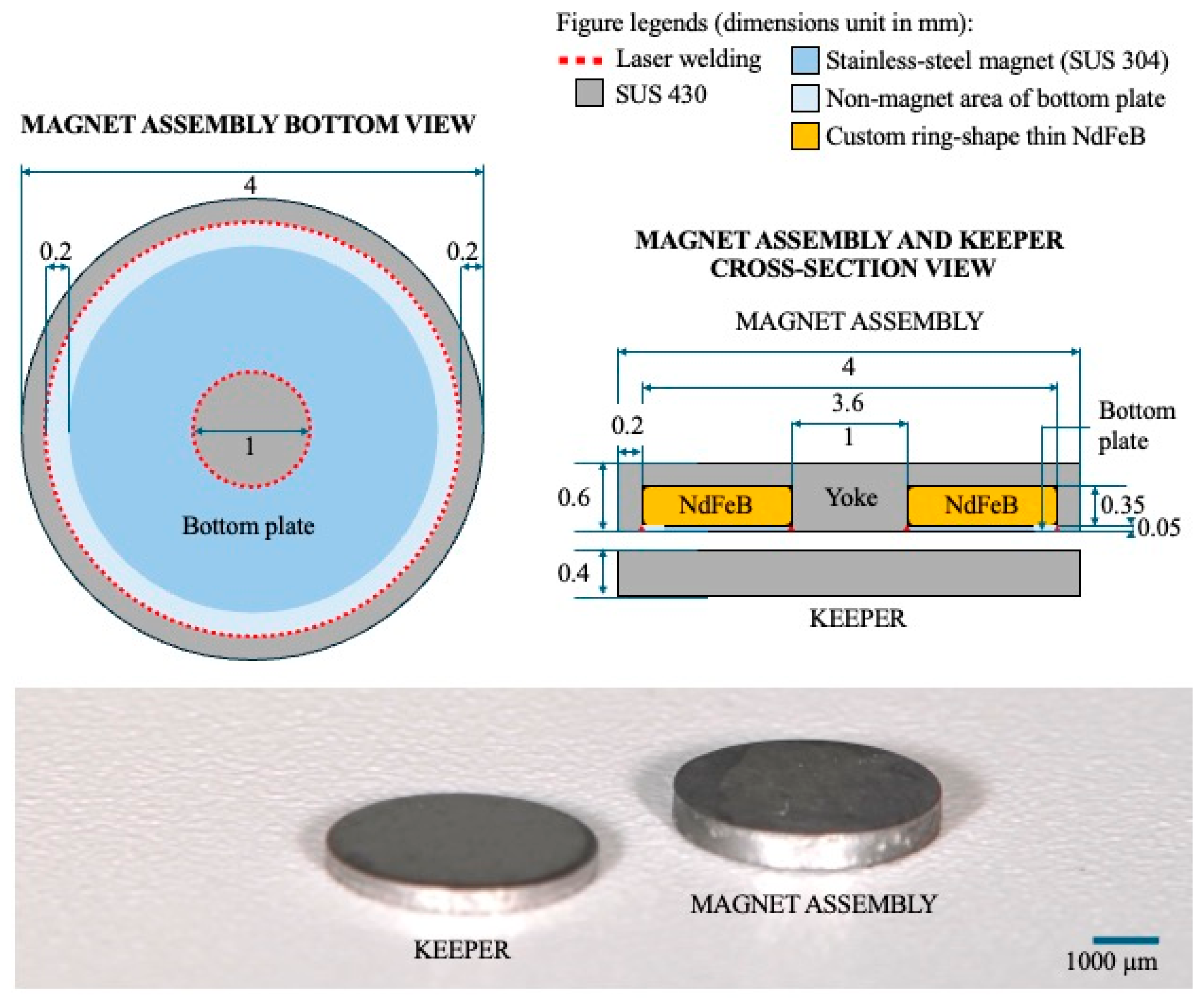
2.1. Magnetic Attachment
2.2. Fabrication of a UTMA-Retained MTPD
2.3. Evaluations
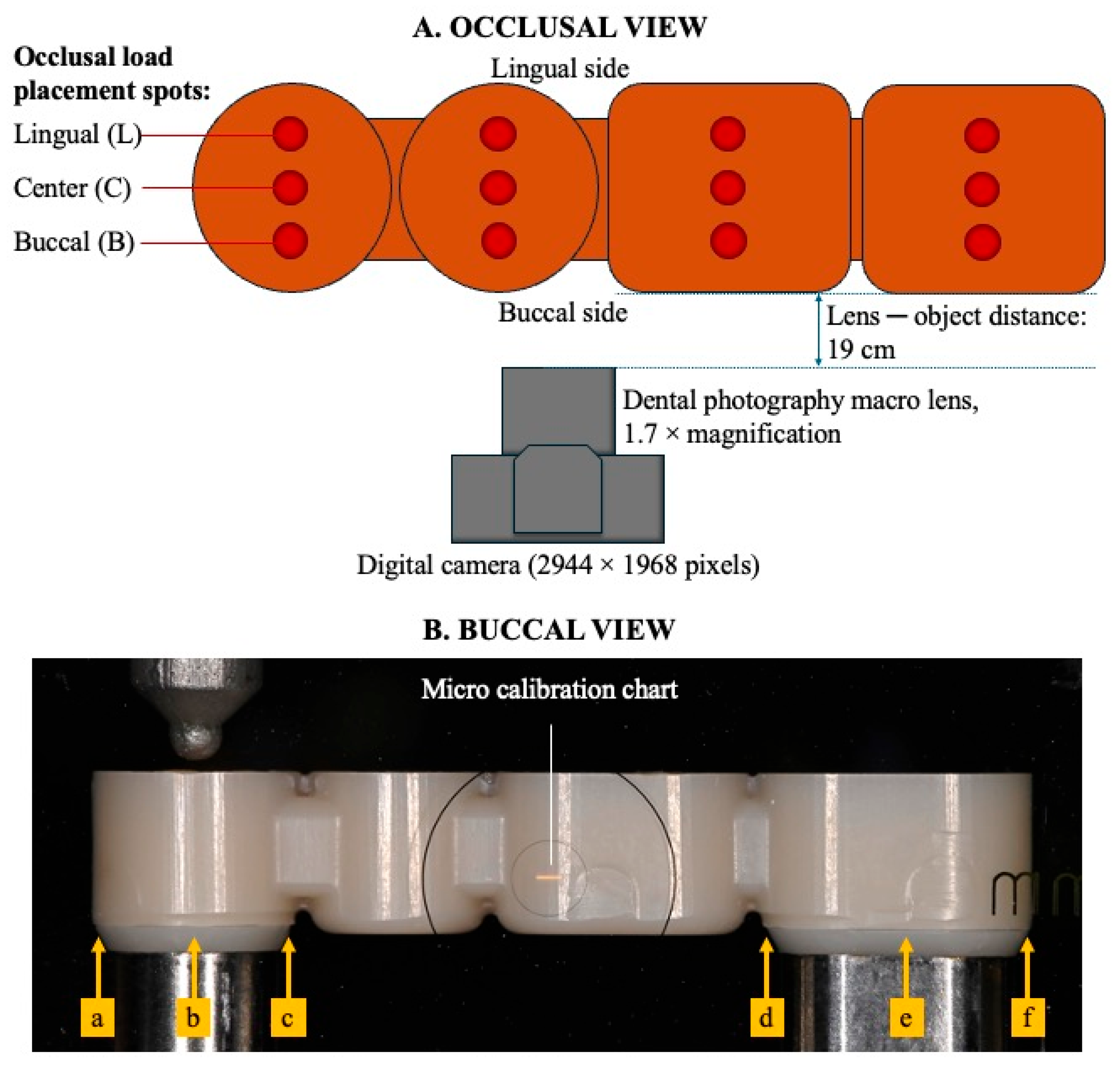
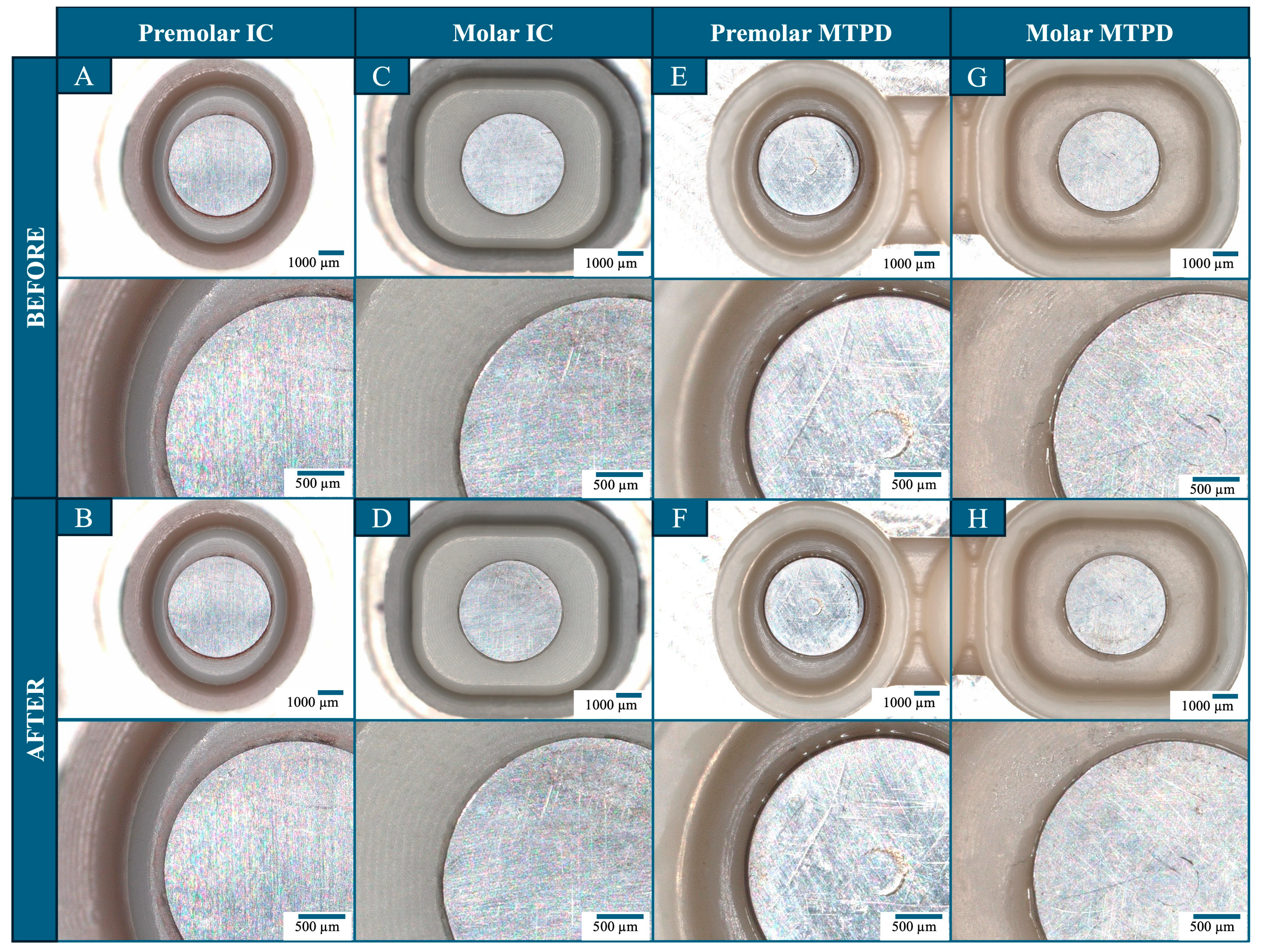
2.3.1. Accuracy
2.3.2. Retentive Force of the UTMA
2.3.3. Retentive Force and Stability of the MTPD
2.3.4. Durability Test
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- -
- Contemporary MTPDs utilizing UTMAs fabricated using a digital workflow exhibit favorable properties.
- -
- The novel UTMA system possesses an adequate retentive force despite its thin structure and provides a broad opportunity for utilization in prosthodontic treatment.
- -
- The assembly might be considered to be a feasible dental prosthesis due to its constant retentive force, adequate stability under loaded conditions, and durable properties.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| MA | Magnet assembly |
| KP | Keeper |
| UTMA | Ultra-thin magnetic attachment |
| MTPD | Magnet-retained telescopic partial denture |
| IC | Inner crown |
| OC | Outer crown |
References
- Ai, M.; Shiau, Y. New Magnetic Applications in Clinical Dentistry; Quintessence Publishing: Tokyo, Japan, 2004. [Google Scholar]
- Tanaka, Y.; Aita, H.; Ishigami, T.; Ichikawa, T.; Ohkawa, S.; Ohkubo, C.; Masumi, S.; Minakuchi, S.; Takada, Y.; Tanaka, J. New Dental Magnetic Attachment, 1st ed.; Ishiyaku Publishers: Tokyo, Japan, 2016. [Google Scholar]
- Gonda, T.; Maeda, Y. Why Are Magnetic Attachments Popular in Japan and Other Asian Countries? Jpn. Dent. Sci. Rev. 2011, 47, 124–130. [Google Scholar] [CrossRef]
- Okuda, H.; Okuda, H.; Maeda, T.; Inoue, H.; Kawano, A.; Unezaki, Y.; Kuremoto, K. Use of Magnetic Attachments in Dentures : Analysis of an 8-Year Longitudinal Study. Prosthodont. Res. Pract. 2004, 3, 8–14. [Google Scholar] [CrossRef]
- Makihara, E.; Masumi, S.; Arita, M.; Yagi, M. Clinical Application of Removable Bridge Prosthese with Magnotelescopic Crown. In Proceedings of the Japanese Society of Magnetic Applications in Dentistry, Online, 3 March 2008. [Google Scholar]
- Tanaka, Y.; Nakamura, Y.; Hoshiai, K. General Remarks Concerning Magnetic Attachments in Dentistry. Proc. Jpn. Acad. Ser. B 2002, 78, 97–105. [Google Scholar] [CrossRef]
- Akin, H.; Emre Coskun, M.; Topcuoglu, T.; Kemal Ozdemir, A. Can Laser Welding Stop Corrosion of New Generation Magnetic Attachment Systems? Mater. Res. Innov. 2011, 15, 66–69. [Google Scholar] [CrossRef]
- Boeckler, A.F.; Morton, D.; Ehring, C.; Setz, J.M. Mechanical Properties of Magnetic Attachments for Removable Prostheses on Teeth and Implants. J. Prosthodont. 2008, 17, 608–615. [Google Scholar] [CrossRef]
- Putra Wigianto, A.Y.; Ishida, Y.; Matsuda, T.; Goto, T.; Watanabe, M.; Ichikawa, T. Novel Magnetic Attachment System Manufactured Using High-Frequency Heat Treatment and Stamp Technique: Introduction and Basic Performance. Dent. J. 2022, 10, 75. [Google Scholar] [CrossRef] [PubMed]
- Arnold, C.; Hey, J.; Schweyen, R.; Setz, J.M. Accuracy of CAD-CAM-Fabricated Removable Partial Dentures. J. Prosthet. Dent. 2018, 119, 586–592. [Google Scholar] [CrossRef]
- Suganna, M.; Kausher, H.; Tarek Ahmed, S.; Sultan Alharbi, H.; Faraj Alsubaie, B.; Ds, A.; Haleem, S.; Meer Rownaq Ali, A.B. Contemporary Evidence of CAD-CAM in Dentistry: A Systematic Review. Cureus 2022, 14, e31687. [Google Scholar] [CrossRef]
- Magnetic Attachment Explanation Video|Japanese Society of Magnetic Dentistry. Available online: http://jsmad.jp/maexpl (accessed on 25 March 2024).
- ISO 13017; Dentistry—Magnetic Attachments. ISO: Geneva, Switzerland, 2020.
- Takeuchi, S.; Sato, Y.; Nathanson, D.; Kitagawa, N.; Kinoshita, Y.; Kajita, T. Novel Removable Keeper System for Magnetic Attachments on Overdenture Abutments. Showa Univ. J. Med. Sci. 2015, 27, 137–142. [Google Scholar] [CrossRef]
- Ogura, I.; Sugawara, Y.; Nagata, K.; Watanabe, M. Artifact on MR Imaging by a Dental Magnetic Attachment Keeper: Preliminary Study on a New Keeper Removable Phantom. Oral Sci. Int. 2019, 16, 25–28. [Google Scholar] [CrossRef]
- Mathew, C.A.; Maller, S. Maheshwaran Interactions between Magnetic Resonance Imaging and Dental Material. J. Pharm. Bioallied Sci. 2013, 5, S113–S116. [Google Scholar] [CrossRef]
- Papadiochou, S.; Pissiotis, A.L. Marginal Adaptation and CAD-CAM Technology: A Systematic Review of Restorative Material and Fabrication Techniques. J. Prosthet. Dent. 2018, 119, 545–551. [Google Scholar] [CrossRef]
- Basker, R.M.; Davenport, J.C.; Thomason, J.M. Prosthetic Treatment of the Edentulous Patient, 5th ed.; Wiley-Blackwell: Oxford, UK, 2011; ISBN 978-1-4051-9261-3. [Google Scholar]
- Arnold, C.; Hey, J.; Setz, J.M.; Boeckler, A.F.; Schweyen, R. Retention Force of Removable Partial Dentures with Different Double Crowns. Clin. Oral Investig. 2018, 22, 1641–1649. [Google Scholar] [CrossRef] [PubMed]
- Pigozzo, M.N.; Mesquita, M.F.; Henriques, G.E.P.; Vaz, L.G. The Service Life of Implant-Retained Overdenture Attachment Systems. J. Prosthet. Dent. 2009, 102, 74–80. [Google Scholar] [CrossRef]
- Stančić, I.; Jelenković, A. Retention of Telescopic Denture in Elderly Patients with Maximum Partially Edentulous Arch. Gerodontology 2008, 25, 162–167. [Google Scholar] [CrossRef] [PubMed]
- Kamel, A.; Badr, A.; Fekry, G.; Tsoi, J. Parameters Affecting the Retention Force of CAD/CAM Telescopic Crowns: A Focused Review of In Vitro Studies. JCM 2021, 10, 4429. [Google Scholar] [CrossRef] [PubMed]
- Grossmann, A.-C.; Hassel, A.J.; Schilling, O.; Lehmann, F.; Koob, A.; Rammelsberg, P. Treatment with Double Crown-Retained Removable Partial Dentures and Oral Health-Related Quality of Life in Middle- and High-Aged Patients. Int. J. Prosthodont. 2007, 20, 576–578. [Google Scholar]
- Stober, T.; Danner, D.; Bömicke, W.; Hassel, A.J. Improvement of Oral Health-Related Quality-of-Life by Use of Different Kinds of Double-Crown-Retained Removable Partial Dentures. Acta Odontol. Scand. 2016, 74, 1–6. [Google Scholar] [CrossRef]
- Choong, E.K.M.; Shu, X.; Leung, K.C.M.; Lo, E.C.M. Oral Health-Related Quality of Life (OHRQoL) after Rehabilitation with Removable Partial Dentures (RPDs): A Systematic Review and Meta-Analysis. J. Dent. 2022, 127, 104351. [Google Scholar] [CrossRef]
- Nakagawa, S.; Torii, K.; Tanaka, M. Effects of Taper and Space Settings of Telescopic Ce-TZP/A Crowns on Retentive Force and Settling. Dent. Mater. J. 2017, 36, 230–235. [Google Scholar] [CrossRef]
- Schwindling, F.S.; Stober, T.; Rustemeier, R.; Schmitter, M.; Rues, S. Retention Behavior of Double-Crown Attachments with Zirconia Primary and Secondary Crowns. Dent. Mater. 2016, 32, 695–702. [Google Scholar] [CrossRef] [PubMed]
- Elkabbany, A.; Kern, M.; Elkhadem, A.H.; Wille, S.; Amer, A.A.; Chaar, M.S. Retention of Metallic and Non-Metallic Double-Crown-Retained Mandibular Overdentures on Implants: An in-Vitro Study. J. Prosthodont. Res. 2020, 64, 384–390. [Google Scholar] [CrossRef] [PubMed]
- Yoshikawa, Y.; Torii, K.; Tanaka, M. Influence of the Number of Insertions and Removals of Telescopic Zirconia/Alumina Crowns on Retentive Force and Settling. Dent. Mater. J. 2019, 38, 671–677. [Google Scholar] [CrossRef]
- Kusumadewi, A.-N.; Damayanti, L.; Risdiana, R. Factors Affecting the Attractive Force of Dental Magnetic Attachment: A Literature Review for Guiding Dentists in Clinical Application. Int. J. Dent. 2022, 2022, 9711285. [Google Scholar] [CrossRef]
- Saygili, G.; Sahmali, S. Retentive Forces of Two Magnetic Systems Compared with Two Precision Attachments. J. Oral Sci. 1998, 40, 61–64. [Google Scholar] [CrossRef] [PubMed]
- Setz, J.; Lee, S.H.; Engel, E. Retention of Prefabricated Attachments for Implant Stabilized Overdentures in the Edentulous Mandible: An in Vitro Study. J. Prosthet. Dent. 1998, 80, 323–329. [Google Scholar] [CrossRef]
- Leem, H.-W.; Cho, I.-H.; Lee, J.-H.; Choi, Y.-S. A Study on the Changes in Attractive Force of Magnetic Attachments for Overdenture. J. Adv. Prosthodont. 2016, 8, 9–15. [Google Scholar] [CrossRef]



| UTMA | MTPD Retentive Force (N) | |||
|---|---|---|---|---|
| Magnetic Field Strength (mT) | Retentive Force (N) | Sample No. | Baseline (Mean ± SD) | After Durability Test (Mean ± SD) |
| 156.00 | 3.12 | 1 | 6.78 ± 0.24 | 5.97 ± 0.05 |
| 158.83 | 3.02 | |||
| 181.07 | 3.21 | 2 | 7.26 ± 0.12 | 7.1 ± 0.02 |
| 153.87 | 3.32 | |||
| 163.07 | 3.04 | 3 | 5.82 ± 0.03 | 5.66 ± 0.02 |
| 174.22 | 3.62 | |||
| 133.50 | 3.41 | 4 | 7.05 ± 0.02 | 7.44 ± 0.01 |
| 138.40 | 3.31 | |||
| 160.50 | 3.22 | 5 | 7.41 ± 0.07 | 7.12 ± 0.05 |
| 127.77 | 3.21 | |||
| 154.72 ± 17.13 | 3.25 ± 0.18 | 6.86 ± 0.63 | 6.66 ± 0.79 | |
| Load-Bearing Area | Before/After Durability Test | Measured Locations (Min–Max Values in µm) | ||||||
|---|---|---|---|---|---|---|---|---|
| a | b | c | d | e | f | |||
| Premolar | L | before | 0 | 0 | 0 | 19–29 | 32–55 | 25–52 |
| after | 0 | 0 | 0 | 18–41 | 33–63 | 26–45 | ||
| C | before | 0 | 0 | 0 | 0 | 0 | 0 | |
| after | 0 | 0 | 0 | 0 | 0 | 0 | ||
| B | before | 0 | 0 | 0 | 0 | 0 | 0 | |
| after | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Molar | L | before | 0–67 | 0–53 | 0–36 | 0 | 0 | 0 |
| after | 0–63 | 0–53 | 0–25 | 0 | 0 | 0 | ||
| C | before | 0 | 0 | 0 | 0 | 0 | 0 | |
| after | 0 | 0 | 0 | 0 | 0 | 0 | ||
| B | before | 0 | 0 | 0 | 0 | 0 | 0 | |
| after | 0 | 0 | 0 | 0 | 0 | 0 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Putra Wigianto, A.Y.; Ishida, Y.; Kamoi, K.; Goto, T.; Sekine, K.; Watanabe, M.; Ichikawa, T. Contemporary Magnetic Removable Partial Denture Utilizing a Novel Ultra-Thin Magnetic Attachment System. Dent. J. 2025, 13, 278. https://doi.org/10.3390/dj13070278
Putra Wigianto AY, Ishida Y, Kamoi K, Goto T, Sekine K, Watanabe M, Ichikawa T. Contemporary Magnetic Removable Partial Denture Utilizing a Novel Ultra-Thin Magnetic Attachment System. Dentistry Journal. 2025; 13(7):278. https://doi.org/10.3390/dj13070278
Chicago/Turabian StylePutra Wigianto, Adityakrisna Yoshi, Yuichi Ishida, Kohei Kamoi, Takaharu Goto, Kazumitsu Sekine, Megumi Watanabe, and Tetsuo Ichikawa. 2025. "Contemporary Magnetic Removable Partial Denture Utilizing a Novel Ultra-Thin Magnetic Attachment System" Dentistry Journal 13, no. 7: 278. https://doi.org/10.3390/dj13070278
APA StylePutra Wigianto, A. Y., Ishida, Y., Kamoi, K., Goto, T., Sekine, K., Watanabe, M., & Ichikawa, T. (2025). Contemporary Magnetic Removable Partial Denture Utilizing a Novel Ultra-Thin Magnetic Attachment System. Dentistry Journal, 13(7), 278. https://doi.org/10.3390/dj13070278





