Retrospective Evaluation of Invisalign® Mandibular Advancement in Growing Patients: Cephalometric, PAR and 3D Molar Displacement Outcomes
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Samples and Eligibility Criteria
- Growing patients with:
- ○
- permanent dentition (Invisalign® Comprehensive Package for teens), or
- ○
- stable early mixed dentition (Invisalign® First), presenting:
- ▪
- mandibular retrognathia (defined using cephalometric criteria, specifically the SNB angle. Values below the normative mean of approximately 80° (±2°), as described by Steiner [21], indicate a posterior mandibular position in relation to the cranial base).
- ▪
- at least 1 total molar Class II relation.
- ▪
- overjet > 5 mm.
- Patients with completed orthodontic treatment with the Invisalign® MA System.
- Individuals with available and complete cephalometric analysis.
- Patients with STL files before, at the end of the initial series of MA aligners, and at the end of the treatment.
- Adult patients.
- Patients with cognitive or neurological alterations.
- Individuals undergoing treatment with anti-inflammatories, analgesics, or psychiatric medication.
2.3. Ethical Principles
2.4. Data Collection Procedures
2.5. Statistical Analysis
3. Results
3.1. Descriptive Statistics for Treatment Duration, Number of Aligners and Refinements
3.2. Skeletal Measures with the Invisalign® Mandibular Advancement
3.3. Dentoalveolar Measures with the Invisalign® Mandibular Advancement
3.4. PAR Index Changes
3.5. Differences in Treatment Outcomes Between Invisalign® First and Invisalign® Comprehensive Package for Teens
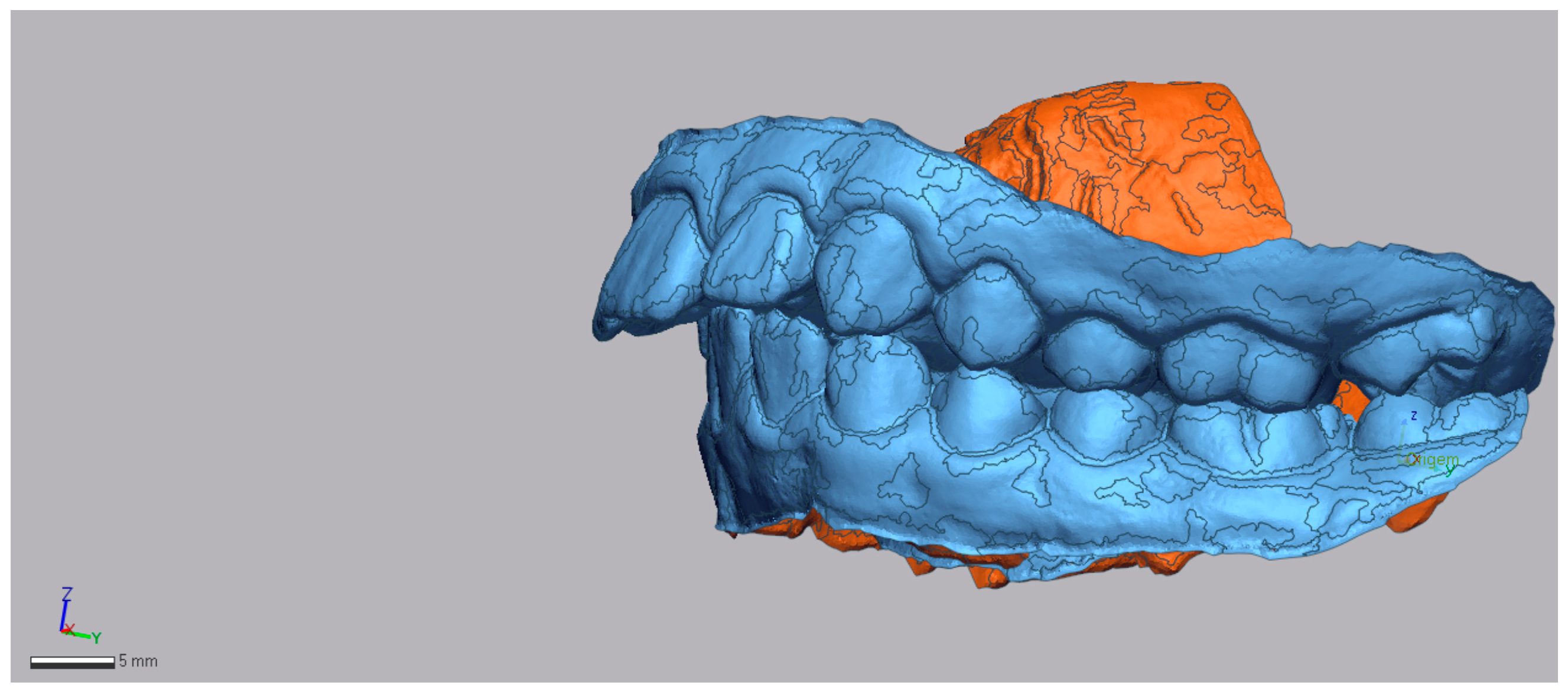
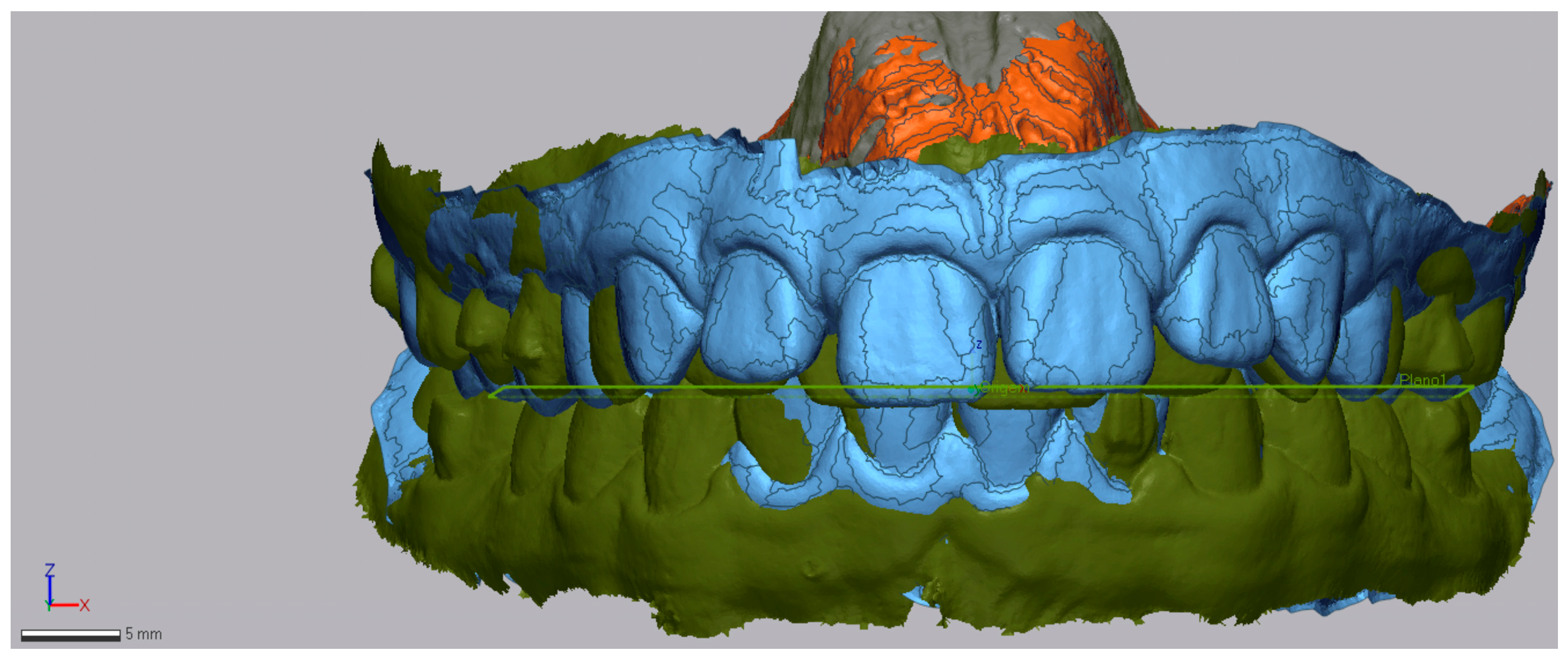
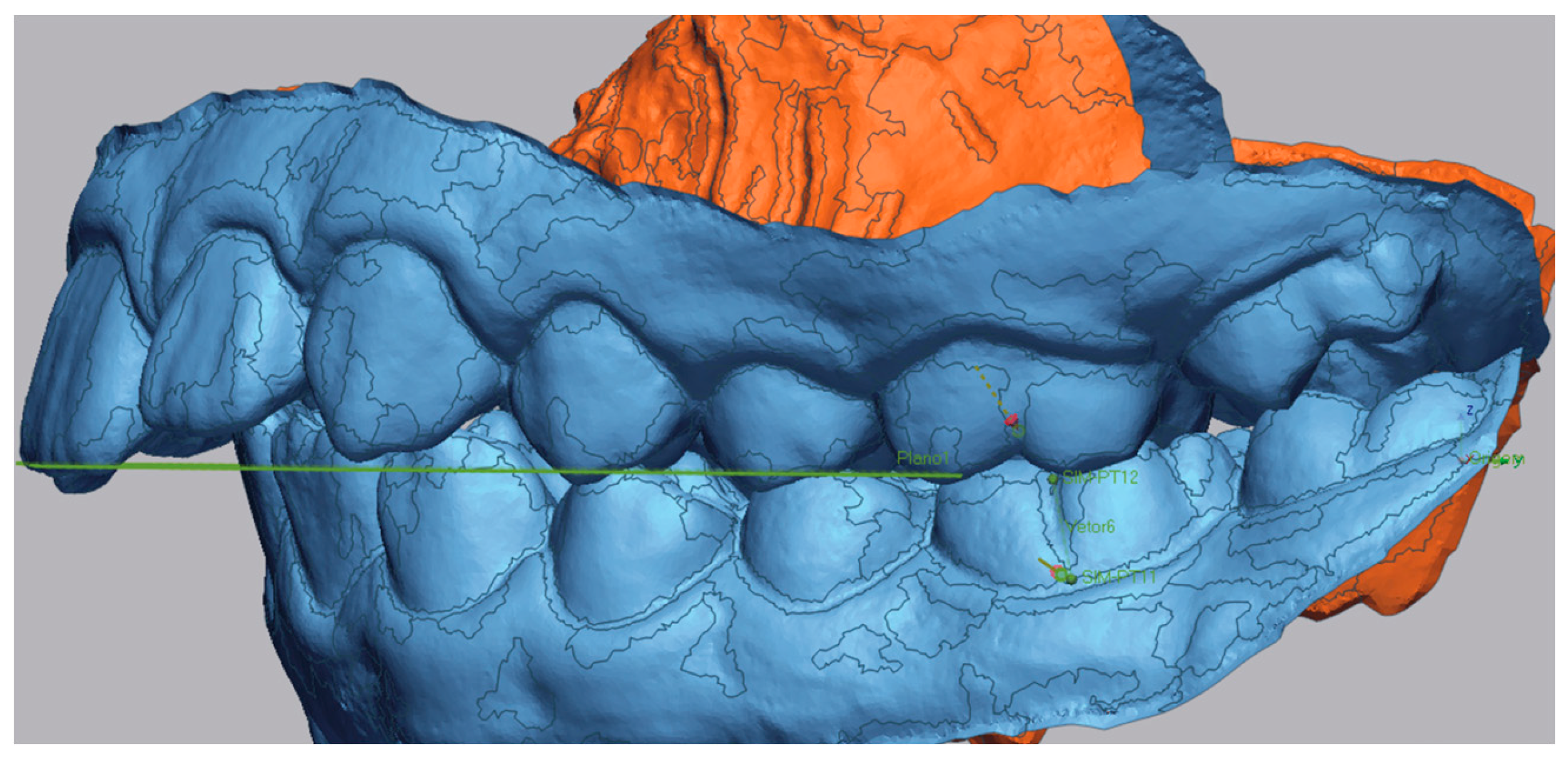
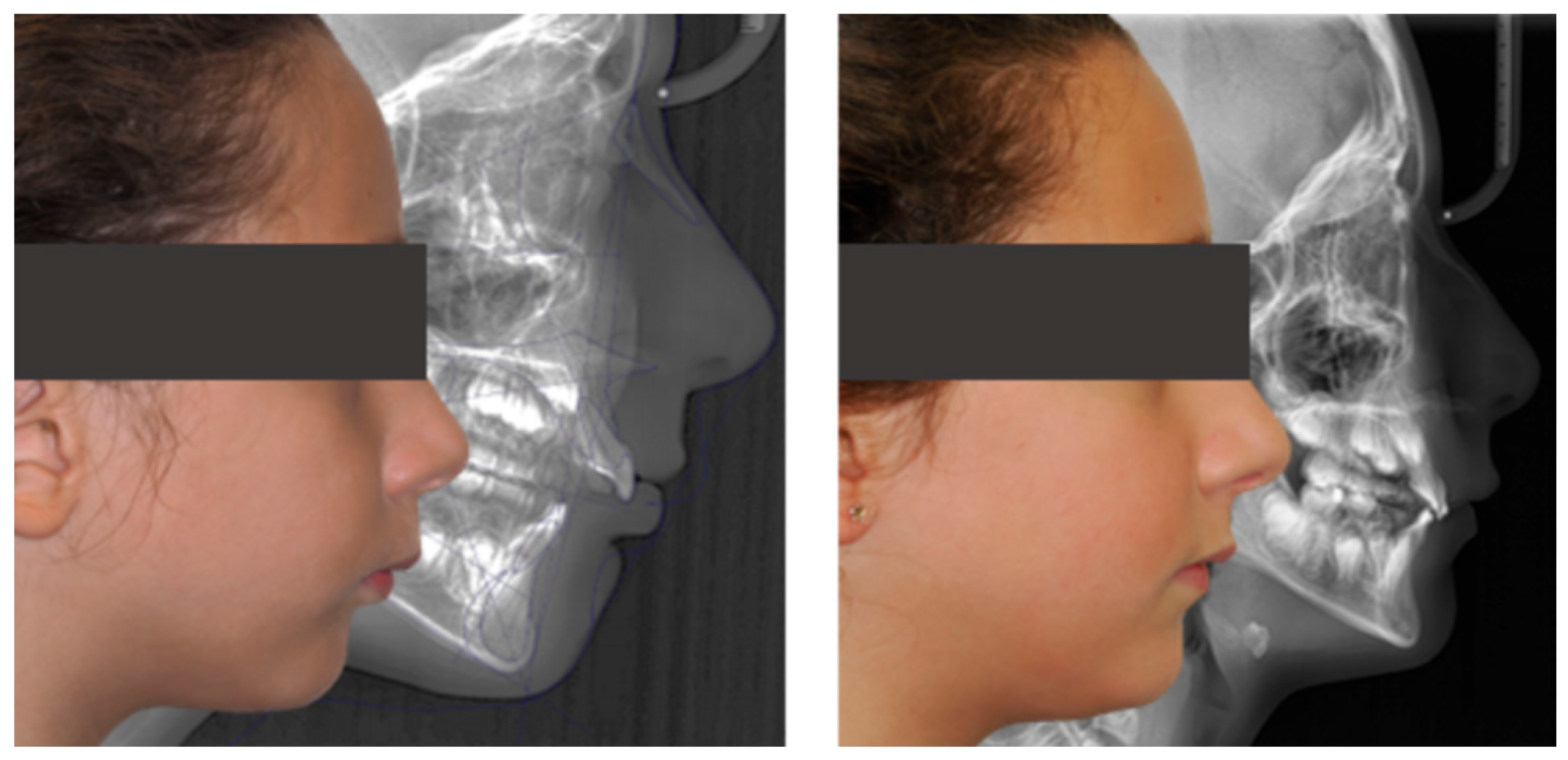
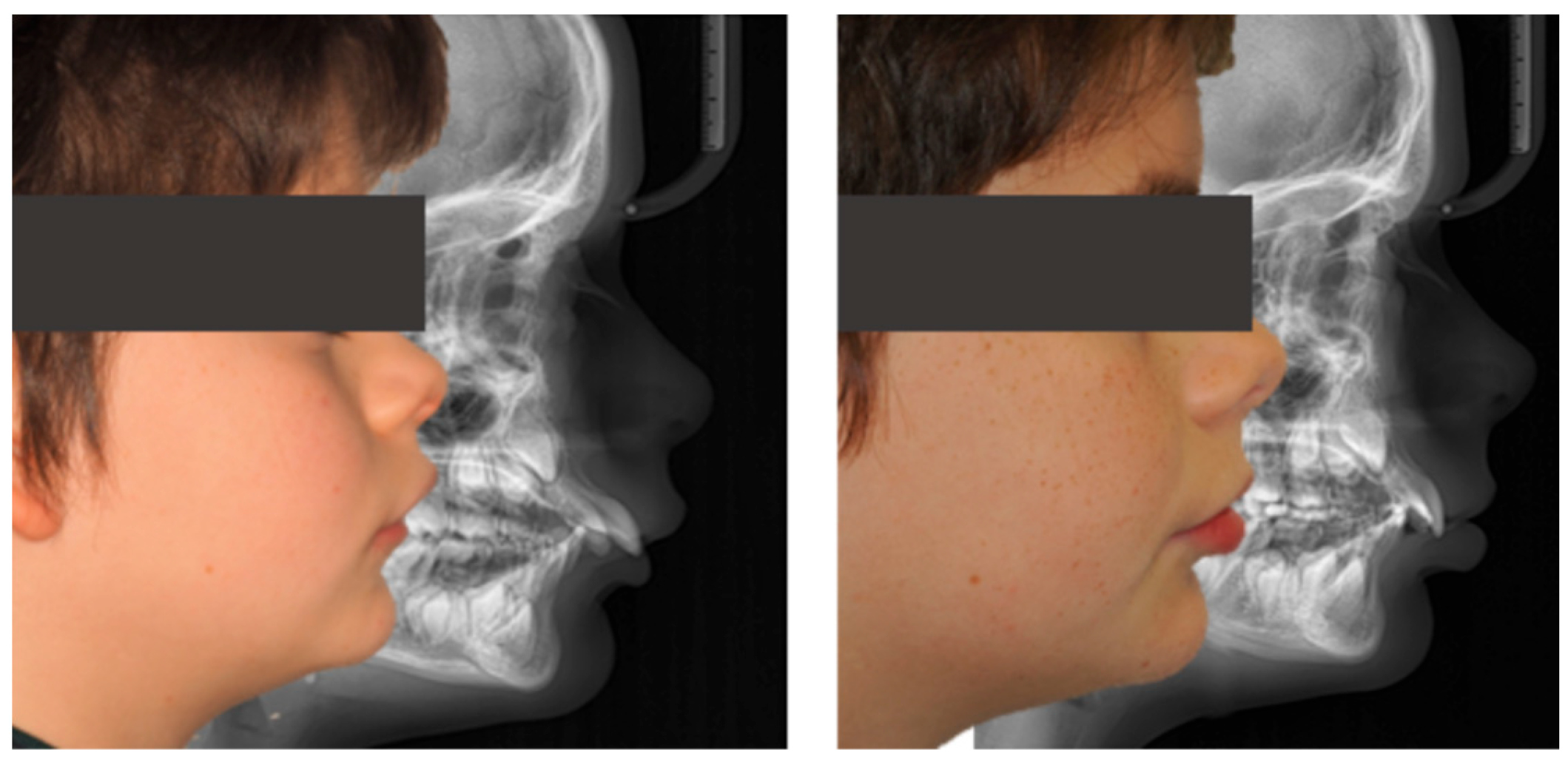
3.6. Representative Clinical Cases
4. Discussion
4.1. Dentoskeletal Changes in Patients with Invisalign® First and Invisalign® Comprehensive Package for Teens
4.2. Dentoalveolar Changes in Patients with Invisalign® First and Invisalign® Comprehensive Package for Teens
4.3. Evaluation of the PAR Index Changes
4.4. Evaluation of L6 Mesialization
4.5. Study Limitations
4.6. Recommendations for Future Studies
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| PAR | Peer Assessment Rating |
| STL | STL file format |
| MA | Mandibular Advancement |
References
- McNamara, J.A., Jr. Components of Class II malocclusion in children 8–10 years of age. Angle Orthod. 1981, 51, 177–202. [Google Scholar]
- Alhammadi, M.S.; Halboub, E.; Fayed, M.S.; Labib, A.; El-Saaidi, C. Global distribution of malocclusion traits: A systematic review. Dent. Press J. Orthod. 2018, 23, 40.e1–40.e10. [Google Scholar] [CrossRef]
- Yue, Z.; Yi, Z.; Liu, X.; Chen, M.; Yin, S.; Liu, Q.; Chen, X.; Hu, J. Comparison of invisalign mandibular advancement and twin-block on upper airway and hyoid bone position improvements for skeletal class II children: A retrospective study. BMC Oral Health 2023, 23, 661. [Google Scholar] [CrossRef]
- Lombardo, E.C.; Lione, R.; Franchi, L.; Gaffuri, F.; Maspero, C.; Cozza, P.; Pavoni, C. Dentoskeletal effects of clear aligner vs twin block—A short-term study of functional appliances. J. Orofac. Orthop. 2024, 85, 317–326. [Google Scholar] [CrossRef] [PubMed]
- Caruso, S.; Nota, A.; Caruso, S.; Severino, M.; Gatto, R.; Meuli, S.; Mattei, A.; Tecco, S. Mandibular advancement with clear aligners in the treatment of skeletal Class II. A retrospective controlled study. Eur. J. Paediatr. Dent. 2021, 22, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Pan, Y.; Lin, T.; Lu, H.; Ai, H.; Mai, Z. Comparison of cephalometric measurements of the Twin Block and A6 appliances in the treatment of Class II malocclusion: A retrospective comparative cohort study. Ann. Transl. Med. 2022, 10, 876. [Google Scholar] [CrossRef] [PubMed]
- Ravera, S.; Castroflorio, T.; Galati, F.; Cugliari, G.; Garino, F.; Deregibus, A.; Quinzi, V. Short term dentoskeletal effects of mandibular advancement clear aligners in Class II growing patients. A prospective controlled study according to STROBE Guidelines. Eur. J. Paediatr. Dent. 2021, 22, 119–124. [Google Scholar] [CrossRef]
- Sabouni, W.; Hansa, I.; Al Ali, S.M.; Adel, S.M.; Vaid, N. Invisalign treatment with mandibular advancement: A retrospective cohort cephalometric appraisal. J. Clin. Imaging Sci. 2022, 12, 42. [Google Scholar] [CrossRef]
- Franchi, L.; Baccetti, T.; McNamara, J.A. Mandibular growth as related to cervical vertebral maturation and body height. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 335–340. [Google Scholar] [CrossRef]
- Baccetti, T.; Franchi, L.; McNamara, J.A. The Cervical Vertebral Maturation (CVM) method for the assessment of optimal treatment timing in dentofacial orthopedics. Semin. Orthod. 2005, 11, 119–129. [Google Scholar] [CrossRef]
- Gu, Y.; McNamara, J.A. Mandibular growth changes and cervical vertebral maturation: A cephalometric implant study. Angle Orthod. 2007, 77, 947–953. [Google Scholar] [CrossRef]
- Vaz, J.; Pinho, T. Skeletal cephalometric modifications in growing patients submitted to functional appliances treatment. Rev. Port. Estomatol. Med. Dent. Cir. Maxilofac. 2017, 58, 153–160. [Google Scholar] [CrossRef]
- Koukou, M.; Damanakis, G.; Tsolakis, A.I. Orthodontic Management of Skeletal Class II Malocclusion with the Invisalign Mandibular Advancement Feature Appliance: A Case Report and Review of the Literature. Case Rep. Dent. 2022, 2022, 7095467. [Google Scholar] [CrossRef] [PubMed]
- Zybutz, T.; Drummond, R.; Lekic, M.; Brownlee, M. Investigation and comparison of patient experiences with removable functional appliances: Invisalign Teen with Mandibular Advancement versus Twin Block. Angle Orthod. 2021, 91, 490–495. [Google Scholar] [CrossRef] [PubMed]
- Pinho, T.; Gonçalves, S.; Rocha, D.; Martins, M.L. Scissor Bite in Growing Patients: Case Report Treated with Clear Aligners. Children 2023, 10, 624. [Google Scholar] [CrossRef]
- Gurgel, M.L.; Ruellas ACde, O.; Bianchi, J.; McNamara, J.A.; Tai, S.; Franchi, L.; Deleat-Besson, R.; Le, C.; Logan, C.; Al Turkestani, N.; et al. Clear aligner mandibular advancement in growing patients with Class II malocclusion. AJO-DO Clin. Companion 2023, 3, 93–109. [Google Scholar] [CrossRef]
- D’Antò, V.; Bucci, R.; De Simone, V.; Ghislanzoni, L.H.; Michelotti, A.; Rongo, R. Evaluation of Tooth Movement Accuracy with Aligners: A Prospective Study. Materials 2022, 15, 2646. [Google Scholar] [CrossRef]
- Wu, Y.; Yu, Q.; Xia, Y.; Wang, B.; Chen, S.; Gu, K.; Zhang, B.; Zhu, M. Does mandibular advancement with clear aligners have the same skeletal and dentoalveolar effects as traditional functional appliances? BMC Oral Health 2023, 23, 65. [Google Scholar] [CrossRef]
- Al Subaie, H.; Alturki, G.; Alsulaimani, F.; Ghoneim, S.; Baeshen, H. Assessment of dental, skeletal, and soft tissue changes following mandibular advancement with Invisalign in skeletal Class II. Saudi Dent. J. 2024, 36, 66–71. [Google Scholar] [CrossRef]
- Camcı, H.; Salmanpour, F. Comparison of skeletal and dentoalveolar effects of two different mandibular advancement methods: Conventional technique vs aesthetic approach. Eur. Oral Res. 2022, 56, 96–101. [Google Scholar] [CrossRef]
- Steiner, C.C.; Hills, B. The use of cephalometrics as an aid to planning and assessing orthodontic treatment. Am. J. Orthod. 1960, 46, 721–735. [Google Scholar] [CrossRef]
- Lanteri, V.; Farronato, G.; Lanteri, C.; Caravita, R.; Cossellu, G. The efficacy of orthodontic treatments for anterior crowding with Invisalign compared with fixed appliances using the Peer Assessment Rating Index. Quintessence Int. 2018, 49, 581–587. [Google Scholar] [CrossRef] [PubMed]
- Dyken, R.A.; Sadowsky, P.L.; Hurst, D. Orthodontic Outcomes Assessment Using the Peer Assessment Rating Index. Angle Orthod. 2001, 71, 164–169. [Google Scholar] [PubMed]
- Freitas, K.M.S.; Freitas, D.S.; Valarelli, F.P.; Freitas, M.R.; Janson, G. PAR evaluation of treated class I extraction patients. Angle Orthod. 2008, 78, 270–274. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Xu, F.; Fang, Y.; Sui, X.; Yao, Y. Comparison of Twin Block appliance and Herbst appliance in the treatment of Class II malocclusion among children: A meta-analysis. BMC Oral Health 2024, 24, 278. [Google Scholar] [CrossRef]
- Cozza, P.; Baccetti, T.; Franchi, L.; De Toffol, L.; McNamara, J.A. Mandibular changes produced by functional appliances in Class II malocclusion: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 599.e1–599.e12. [Google Scholar] [CrossRef]
- Marsico, E.; Gatto, E.; Burrascano, M.; Matarese, G.; Cordasco, G. Effectiveness of orthodontic treatment with functional appliances on mandibular growth in the short term. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 24–36. [Google Scholar] [CrossRef]
- Riedel, R.A. The relation of maxillary structures to cranium in malocclusion and in normal occlusion. Angle Orthod. 1952, 22, 142–145. [Google Scholar]
- McNamara, J.A. Influence of respiratory pattern on craniofacial growth. Angle Orthod. 1981, 51, 269–300. [Google Scholar] [CrossRef]
- Richmond, S.; Shaw, W.C.; Roberts, C.T.; Andrews, M. The PAR Index (Peer Assessment Rating): Methods to determine outcome of orthodontic treatment in terms of improvement and standards. Eur. J. Orthod. 1992, 14, 180–187. [Google Scholar] [CrossRef]
- Pinho, T.; Rocha, D.; Ribeiro, S.; Monteiro, F.; Pascoal, S.; Azevedo, R. Interceptive Treatment with Invisalign® First in Moderate and Severe Cases: A Case Series. Children 2022, 9, 1176. [Google Scholar] [CrossRef]
- Edman Tynelius, G.; Bondemark, L.; Lilja-Karlander, E. A randomized controlled trial of three orthodontic retention methods in Class I four premolar extraction cases—Stability after 2 years in retention. Orthod. Craniofac. Res. 2013, 16, 105–115. [Google Scholar] [CrossRef]
- Tulloch, J.F.C.; Phillips, C.; Proffit, W.R. Benefit of early Class II treatment: Progress report of a two-phase randomized clinical trial. Am. J. Orthod. Dentofac. Orthop. 1998, 113, 62–72. [Google Scholar] [CrossRef]
- Pinho, T.; Melo, D.; Ferreira, S.; Gonçalves, M. Distalization with Clear Aligners: Accuracy, Impact of Mini-Screws, and Clinical Outcomes. Dent. J. 2025, 13, 316. [Google Scholar] [CrossRef]










| Invisalign® Comprehensive Package for Teens Group (n = 10) | Invisalign® First Group (n = 7) | |
|---|---|---|
| n (%) | n (%) | |
| Age (Mean ± SD) | 11.9 ± 2.08 | 8.3 ± 0.95 |
| Age range (years) | 9–16 | 7–10 |
| Gender | ||
| Female | 7 (70.0) | 4 (57.1) |
| Male | 3 (30.0) | 3 (42.9) |
| Initial facial biotype | ||
| Hypodivergent | 3 (30.0) | 1 (14.3) |
| Hyperdivergent | 4 (40.0) | 4 (57.1) |
| Normodivergent | 3 (30.0) | 2 (28.6) |
| Final facial biotype | ||
| Hypodivergent | 2 (20.0) | 1 (14.3) |
| Hyperdivergent | 2 (20.0) | 4 (57.1) |
| Normodivergent | 6 (60.0) | 2 (28.6) |
| Initial right/left molar class | ||
| Class I/II | 1 (10.0) | 0 (0.0) |
| Class II/I | 1 (10.0) | 0 (0.0) |
| Class II/II | 8 (80.0) | 7 (100.0) |
| Final right/left molar class | ||
| Class I/I | 10 (100.0) | 4 (57.1) |
| Class I/II | 0 (0.0) | 1 (14.3) |
| Class II/II | 0 (0.0) | 2 (28.6) |
| Class III/III | 0 (0.0) | |
| Initial Spee Curve | ||
| Normal | 4 (50.0) | 3 (42.9) |
| Deep | 5 (50.0) | 3 (42.9) |
| Inverted | 1 (14.3) | |
| Final Spee Curve | ||
| Normal | 5 (50.0) | 5 (71.4) |
| Deep | 5 (50.0) | 2 (28.6) |
| Teen (n = 10) | First (n = 7) | |||||
|---|---|---|---|---|---|---|
| Min | Max | Mean ± SD | Min | Max | Mean ± SD | |
| Treatment duration (months) | 20 | 36 | 29.70 ± 6.57 | 18 | 18 | 18.0 ± 0.0 |
| Number of aligners | 40 | 67 | 54.40 ± 8.39 | 43 | 62 | 49.29 ± 6.65 |
| Refinements | 1 | 3 | 2.0 ± 0.82 | 1 | 3 | 2.0 ± 0.76 |
| Retention (months) | 12 | 60 | 24 ± 14.97 | 12 | 24 | 15.43 ± 5.86 |
| Stability n (%) | ||||||
| No relapse | 9 (90.0) | 5 (71.4) | ||||
| Relapsed | 1 (10.0) | 2 (28.6) | ||||
| Cohen’s d | ||||||
|---|---|---|---|---|---|---|
| Measure | T0 (Mean ± SD) | TF (Mean ± SD) | Diff (TF–T0) | p | Statistic | IC95% |
| FMA (degree) | 28.57 ± 7.27 | 27.49 ± 6.35 | −1.08 | 0.071 | 0.83 | 0.07–1.67 |
| SNA (degree) | 80.23 ± 3.83 | 79.44 ± 4.43 | −0.79 | 0.089 | 0.49 | 0.32–1.26 |
| SNB (degree) | 74.14 ± 3.16 | 75.19 ± 3.61 | 1.05 | 0.010 | 0.98 | 0.35–1.87 |
| ANB (degree) | 6.10 ± 1.27 | 4.26 ± 1.51 | −1.84 | <0.001 | 0.99 | 0.74–1.31 |
| Wits (mm) | 1.86 ± 0.95 | −0.66 ± 1.94 | −2.52 | 0.006 | 0.77 | 0.39–0.94 |
| Cohen’s d | ||||||
|---|---|---|---|---|---|---|
| Measure/Units | T0 (Mean ± SD) | TF (Mean ± SD) | Diff (TF–T0) | p | Statistic | IC95% |
| FMA (degree) | 25.36 ± 7.25 | 24.43 ± 6.19 | −0.93 | 0.237 | 0.40 | 0.26–1.04 |
| SNA (degree) | 81.29 ± 2.79 | 79.17 ± 2.82 | −2.32 | 0.002 | 1.36 | 0.48–2.21 |
| SNB (degree) | 74.73 ± 1.99 | 75.60 ± 1.99 | 1.03 | 0.026 | 0.84 | 0.09–1.55 |
| ANB (degree) | 6.55 ± 1.53 | 3.60 ± 1.30 | −2.95 | <0.001 | 0.75 | 0.58–1.44 |
| Wits (mm) | 3.12 ± 2.03 | 0.62 ± 2.50 | −2.50 | 0.029 | 0.82 | 0.08–1.53 |
| Cohen’s d | ||||||
|---|---|---|---|---|---|---|
| Measure/Units | T0 (Mean ± SD) | TF (Mean ± SD) | Diff (TF–T0) | p | Statistic | IC95% |
| IMPA (degree) | 93.86 ± 6.82 | 95.60 ± 4.69 | 1.74 | 0.350 | 0.38 | 0.40–1.14 |
| UI/NA (degree) | 24.17 ± 10.69 | 18.86 ± 3.13 | −5.31 | 0.196 | 0.55 | 0.27–1.33 |
| Interincisal angle (degree) | 124.19 ± 14.78 | 128.39 ± 5.79 | 4.20 | 0.415 | 0.33 | 0.44–1.08 |
| Overjet (mm) | 7.73 ± 2.66 | 3.90 ± 1.89 | −3.83 | 0.005 | 1.64 | 0.44–2.78 |
| Overbite (mm) | 3.33 ± 3.10 | 3.96 ± 1.29 | 0.63 | 0.587 | 0.61 | 0.53–0.97 |
| Cohen’s d | ||||||
|---|---|---|---|---|---|---|
| Measure (Unit) | T0 (Mean ± SD) | TF (Mean ± SD) | Diff (TF–T0) | p | Statistic | IC95% |
| IMPA (degree) | 99.79± 6.52 | 97.59 ± 5.11 | −2.20 | 0.084 | 0.61 | 0.08–1.28 |
| UI/NA (degree) | 27.27 ± 6.82 | 20.82 ± 4.17 | −6.54 | 0.002 | 1.38 | 0.48–2.24 |
| Interincisal angle (degree) | 117.39 ± 6.54 | 125.68 ± 4.79 | 8.29 | <0.001 | 1.55 | 0.58–2.45 |
| Overjet (mm) | 8.55 ± 2.84 | 3.17 ± 0.83 | −5.38 | <0.001 | 1.88 | 0.81–2.91 |
| Overbite (mm) | 4.53 ± 1.27 | 3.79 ± 1.25 | −0.74 | 0.070 | 0.65 | 0.05–1.32 |
| Cohen’s d | ||||||
|---|---|---|---|---|---|---|
| Invisalign® System | T0 (Mean ± SD) | TF (Mean ± SD) | Diff (T0–TF) | p | Statistic | IC95% |
| Teen | ||||||
| PAR index | 27.40 ± 4.90 | 3.80 ± 3.33 | 23.60 | <0.001 | 4.44 | 2.33–6.54 |
| First | ||||||
| PAR index | 28.43 ± 6.45 | 9.00 ± 5.69 | 19.43 | <0.001 | 2.73 | 1.04–4.38 |
| Cohen’s d | ||||||
|---|---|---|---|---|---|---|
| Mean ± SD | Mean Diff. | p | Statistic | IC95% | ||
| PAR Index Before | Teen (n = 10) | 27.40 ± 4.90 | 1.03 | 0.713 | 0.85 | 0.79–1.15 |
| First (n = 7) | 28.43 ± 6.45 | |||||
| PAR index After | Teen (n = 10) | 3.80 ± 3.33 | 5.2 | 0.031 | 1.17 | 0.11–2.21 |
| First (n = 7) | 9.00 ± 5.69 | |||||
| Percentage Reduction | Teen (n = 10) | 85.54 ± 13.21 | 17.36 | 0.025 | 1.23 | 0.15–2.27 |
| First (n = 7) | 68.18 ± 15.34 | |||||
| Mesialization of L6 | Teen (n = 10) | 3.57 ± 1.26 | 2.23 | <0.001 | 2.18 | 0.92–3.33 |
| First (n = 7) | 1.34 ± 0.48 | |||||
| Distalization of U6 | Teen (n = 10) | 1.35 ± 0.69 | 0.89 | 0.002 | 1.34 | 0.18–2.45 |
| First (n = 7) | 2.24 ± 0.64 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pinho, T.; Clemente, C.; Castro, I.d.; Gonçalves, M.d.P. Retrospective Evaluation of Invisalign® Mandibular Advancement in Growing Patients: Cephalometric, PAR and 3D Molar Displacement Outcomes. Dent. J. 2025, 13, 517. https://doi.org/10.3390/dj13110517
Pinho T, Clemente C, Castro Id, Gonçalves MdP. Retrospective Evaluation of Invisalign® Mandibular Advancement in Growing Patients: Cephalometric, PAR and 3D Molar Displacement Outcomes. Dentistry Journal. 2025; 13(11):517. https://doi.org/10.3390/dj13110517
Chicago/Turabian StylePinho, Teresa, Carolina Clemente, Inês de Castro, and Maria dos Prazeres Gonçalves. 2025. "Retrospective Evaluation of Invisalign® Mandibular Advancement in Growing Patients: Cephalometric, PAR and 3D Molar Displacement Outcomes" Dentistry Journal 13, no. 11: 517. https://doi.org/10.3390/dj13110517
APA StylePinho, T., Clemente, C., Castro, I. d., & Gonçalves, M. d. P. (2025). Retrospective Evaluation of Invisalign® Mandibular Advancement in Growing Patients: Cephalometric, PAR and 3D Molar Displacement Outcomes. Dentistry Journal, 13(11), 517. https://doi.org/10.3390/dj13110517







