Bond Strength of Nanocomposite Hard Liner to CAD-CAM Milled, 3D Printed, and Conventionally Fabricated Denture Base Resins
Abstract
1. Introduction
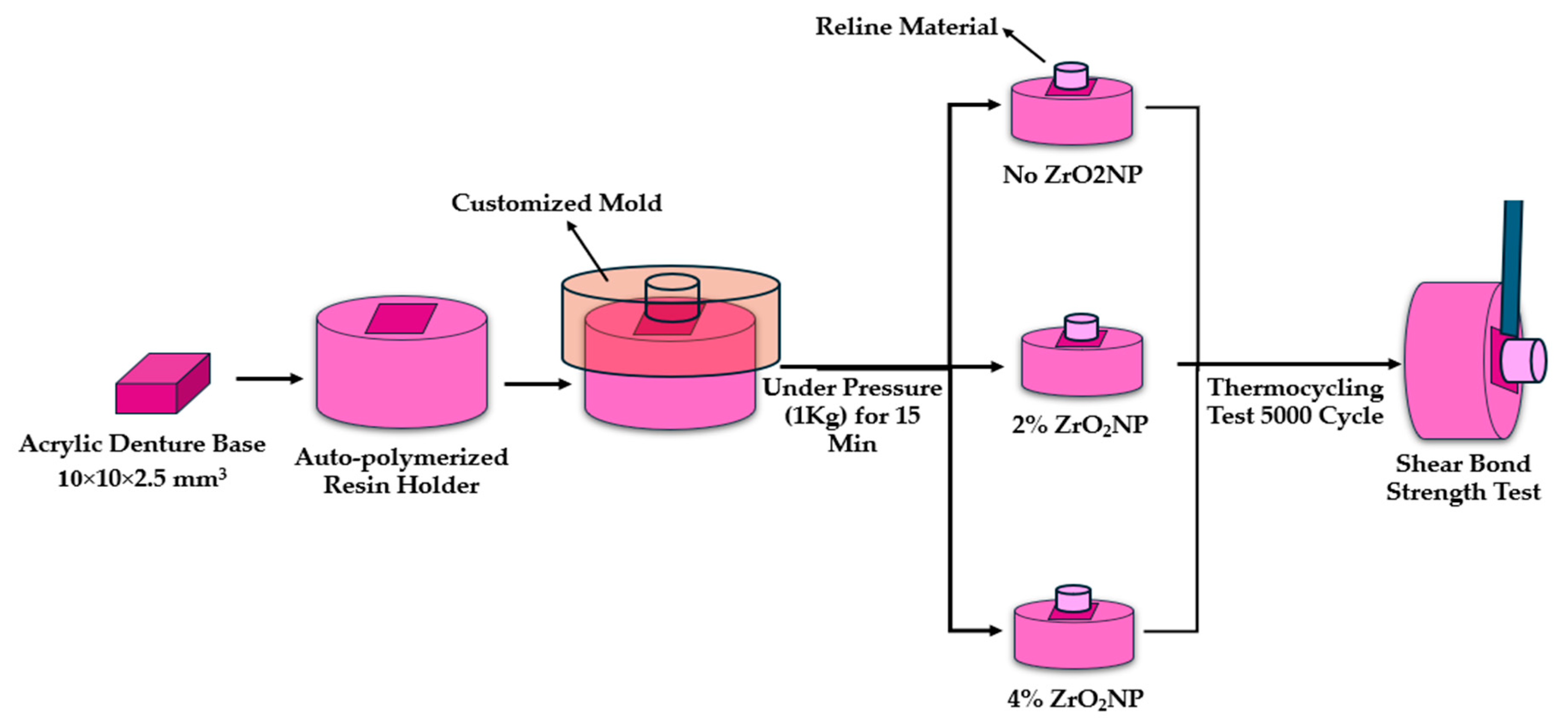
2. Materials and Methods
3. Results
3.1. SBS
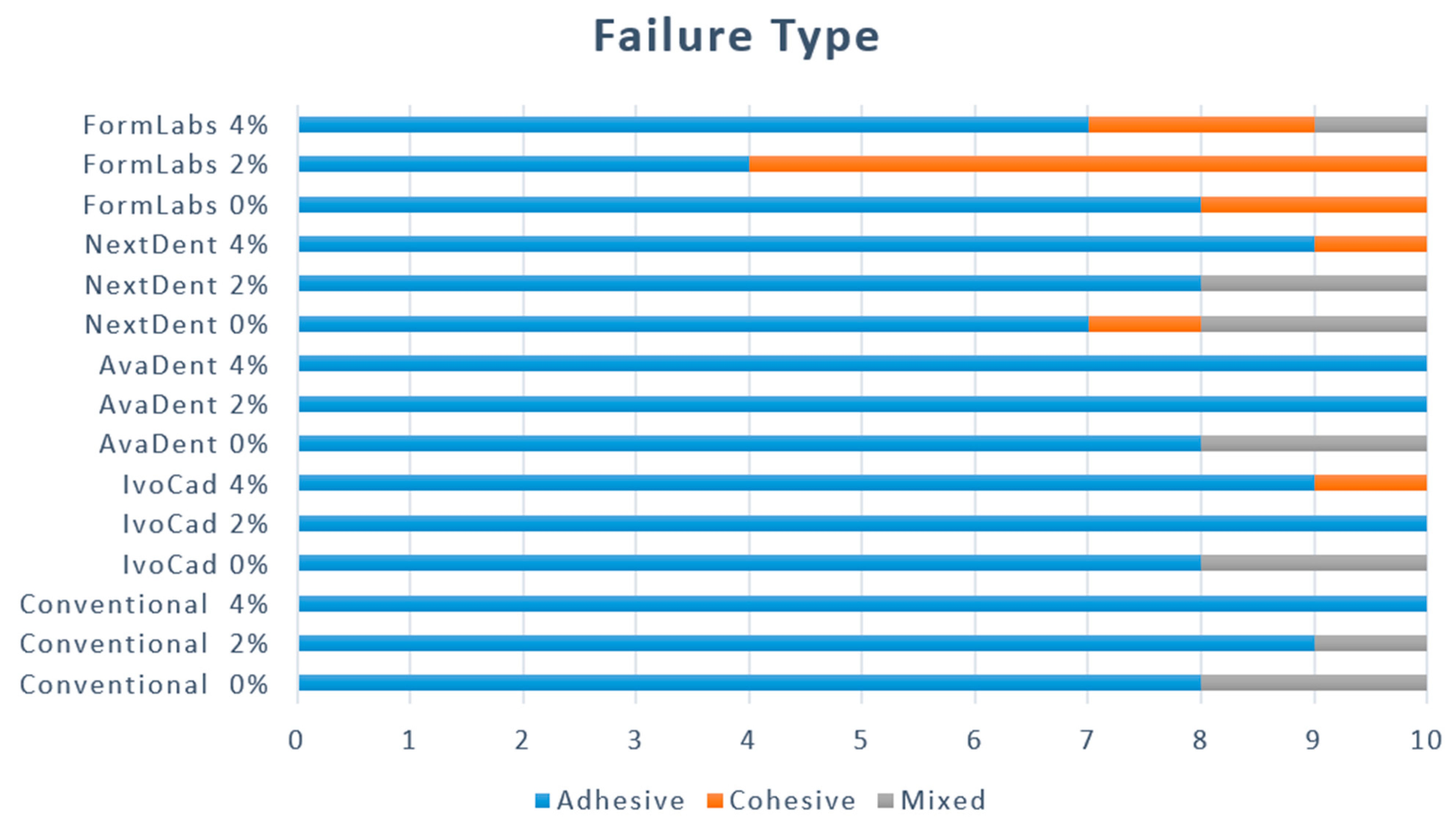
3.2. Type of Failure
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chen, J.; Ahmad, R.; Li, W.; Swain, M.; Li, Q. Biomechanics of oral mucosa. J. R. Soc. Interface 2015, 12, 20150325. [Google Scholar] [CrossRef]
- Leles, C.R.; Machado, A.L.; Vergani, C.E.; Giampaolo, E.T.; Pavarina, A.C. Bonding strength between a hard chairside reline resin and a denture base material as influenced by surface treatment. J. Oral Rehabil. 2001, 28, 1153–1157. [Google Scholar] [CrossRef]
- Lau, M.; Amarnath, G.S.; Muddugangadhar, B.C.; Swetha, M.U.; Das, K.A.A.K. Tensile and shear bond strength of hard and soft denture relining materials to the conventional heat cured acrylic denture base resin: An In-vitro study. J. Int. Oral Health JIOH 2014, 6, 55–61. [Google Scholar] [PubMed]
- Murata, H.; Seo, R.S.; Hamada, T.; Polyzois, G.L.; Frangou, M.J. Dynamic mechanical properties of hard, direct denture reline resins. J. Prosthet. Dent. 2007, 98, 319–326. [Google Scholar] [CrossRef]
- Kreve, S.; Dos Reis, A.C. Denture Liners: A Systematic Review Relative to Adhesion and Mechanical Properties. Sci. World J. 2019, 2019, e6913080. [Google Scholar] [CrossRef] [PubMed]
- Machado, A.L.; Breeding, L.C.; Vergani, C.E.; da Cruz Perez, L.E. Hardness and surface roughness of reline and denture base acrylic resins after repeated disinfection procedures. J. Prosthet. Dent. 2009, 102, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Ataol, A.S.; Ergun, G.; Cekic-Nagas, I.; Alas, M.O.; Genc, R. The effects of adding fluorescent carbon nanoparticles on various mechanical properties of denture liners. Dent. Mater. J. 2021, 40, 573–583. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, Y.; Chai, J. Shear bond strength of denture reline polymers to denture base polymers. Int. J. Prosthodont. 2001, 14, 271–275. [Google Scholar]
- Choi, J.E.; Ng, T.E.; Leong, C.K.Y.; Kim, H.; Li, P.; Waddell, J.N. Adhesive evaluation of three types of resilient denture liners bonded to heat-polymerized, autopolymerized, or CAD-CAM acrylic resin denture bases. J. Prosthet. Dent. 2018, 120, 699–705. [Google Scholar] [CrossRef]
- Al Taweel, S.M.; Al-Otaibi, H.N.; Labban, N.; AlFouzan, A.; Shehri, H.A. Soft Denture Liner Adhesion to Conventional and CAD/CAM Processed Poly(Methyl Methacrylate) Acrylic Denture Resins-An In-Vitro Study. Materials 2021, 14, 6614. [Google Scholar] [CrossRef]
- Ansarifard, E.; Zareshahrabadi, Z.; Sarafraz, N.; Zomorodian, K. Evaluation of Antimicrobial and Antibiofilm Activities of Copper Oxide Nanoparticles within Soft Denture Liners against Oral Pathogens. Bioinorg. Chem. Appl. 2021, 2021, 9939275. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Rahman, H.K.; Al-Sammaraie, S.A.S. Effect of Adding Magnesium Oxide Nanoparticles on the Antimicrobial Activity of a Denture Soft Liner. Polytech. J. 2020, 10, 132–137. [Google Scholar] [CrossRef]
- Habibzadeh, S.; Omidvaran, A.; Eskandarion, S.; Shamshiri, A.R. Effect of Incorporation of Silver Nanoparticles on the Tensile Bond Strength of a Long term Soft Denture Liner. Eur. J. Dent. 2020, 14, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Khattar, A.; Alghafli, J.A.; Muheef, M.A.; Alsalem, A.M.; Al-Dubays, M.A.; AlHussain, H.M.; AlShoalah, H.M.; Khan, S.Q.; AlEraky, D.M.; Gad, M.M. Antibiofilm Activity of 3D-Printed Nanocomposite Resin: Impact of ZrO2 Nanoparticles. Nanomaterials 2023, 13, 591. [Google Scholar] [CrossRef] [PubMed]
- Ergun, G.; Ataol, A.S.; Şahi, N.Z.; Saraç, N.; Baygar, T.; Uğur, A. Antibiofilm Evaluation of Two Different Denture Liners Incorporated with Zirconium Oxide Nanoparticles. Cumhur. Dent. J. 2022, 25, 9–19. [Google Scholar] [CrossRef]
- Abdulrazzaq Naji, S.; Al-azzawi, M.A. Effect of Zirconium Oxide-Titanium Dioxide Nanoparticles on Mechanical and Physical Properties of Soft Denture Lining Materials. J. Nanostruct. 2022, 12, 34–44. [Google Scholar]
- Gad, M.M.; Albazroun, Z.; Aldajani, F.; Elakel, A.M.; El Zayat, M.; Akhtar, S.; Khan, S.Q.; Ali, S.; Rahoma, A.M. Repair Bond Strength of Conventionally and Digitally Fabricated Denture Base Resins to Auto-Polymerized Acrylic Resin: Surface Treatment Effects In Vitro. Materials 2022, 15, 9062. [Google Scholar] [CrossRef]
- Gad, M.M.; Bahgat, H.A.; Edrees, M.F.; Alhumaidan, A.; Khan, S.Q.; Ayad, N.M. Antifungal Activities and Some Surface Characteristics of Denture Soft Liners Containing Silicon Dioxide Nanoparticles. J. Int. Soc. Prev. Community Dent. 2022, 12, 109–116. [Google Scholar] [CrossRef]
- Qaw, M.S.; Abushowmi, T.H.; Almaskin, D.F.; AlZaher, Z.A.; Gad, M.M.; Al-Harbi, F.A.; Abualsaud, R.; Ammar, M.M. A Novel Approach to Improve Repair Bond Strength of Repaired Acrylic Resin: An in Vitro Study on the Shear Bond Strength. J. Prosthodont. 2020, 29, 323–333. [Google Scholar] [CrossRef]
- Mutluay, M.M.; Ruyter, I.E. Evaluation of bond strength of soft relining materials to denture base polymers. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2007, 23, 1373–1381. [Google Scholar] [CrossRef]
- Aydin, A.K.; Terzioğlu, H.; Akinay, A.E.; Ulubayram, K.; Hasirci, N. Bond strength and failure analysis of lining materials to denture resin. Dent. Mater. Off. Publ. Acad. Dent. Mater. 1999, 15, 211–218. [Google Scholar] [CrossRef]
- McCabe, J.F.; Carrick, T.E.; Kamohara, H. Adhesive bond strength and compliance for denture soft lining materials. Biomaterials 2002, 23, 1347–1352. [Google Scholar] [CrossRef]
- Amin, W.M.; Fletcher, A.M.; Ritchie, G.M. The nature of the interface between polymethyl methacrylate denture base materials and soft lining materials. J. Dent. 1981, 9, 336–346. [Google Scholar] [CrossRef]
- al-Athel, M.S.; Jagger, R.G. Effect of test method on the bond strength of a silicone resilient denture lining material. J. Prosthet. Dent. 1996, 76, 535–540. [Google Scholar] [CrossRef] [PubMed]
- Wemken, G.; Burkhardt, F.; Spies, B.C.; Kleinvogel, L.; Adali, U.; Sterzenbach, G.; Beuer, F.; Wesemann, C. Bond strength of conventional, subtractive, and additive manufactured denture bases to soft and hard relining materials. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2021, 37, 928–938. [Google Scholar] [CrossRef] [PubMed]
- Koseoglu, M.; Tugut, F.; Akin, H. Tensile bond strength of soft and hard relining materials to conventional and additively manufactured denture-base materials. J. Prosthodont. 2023, 32 (Suppl. S1), 74–80. [Google Scholar] [CrossRef] [PubMed]
- Gad, M.M.; Fouda, S.M.; Alshammary, H.; Altayyar, R.; Elakel, A.; Nassar, E.A.; Khan, S.Q.; Rahoma, A.M.; Elhagali, A.F.; Özcan, M.; et al. Influence of different printing orientations and post-polymerization time on the translucency of three-dimensional (3D) printed denture base resins. J. Prosthodont. 2024. Available online: https://onlinelibrary-wiley-com.library.iau.edu.sa/doi/abs/10.1111/jopr.13866 (accessed on 11 June 2024).
- Yacob, N.; Ahmad, N.A.; Safii, S.H.; Yunus, N.; Abdul Razak, F. Is microbial adhesion affected by the build orientation of a 3-dimensionally printed denture base resin? J. Prosthet. Dent. 2023, 130, 131.e1–131.e7. [Google Scholar] [CrossRef] [PubMed]
- Yan, S.; Zhou, J.L.; Zhang, R.J.; Tan, F.B. Evaluation of the influence of different build angles on the surface characteristics, accuracy, and dimensional stability of the complete denture base printed by digital light processing. Heliyon 2024, 10, e24095. [Google Scholar] [CrossRef]
- Takahashi, Y.; Chai, J. Assessment of shear bond strength between three denture reline materials and a denture base acrylic resin. Int. J. Prosthodont. 2001, 14, 531–535. [Google Scholar]
- Park, S.J.; Lee, J.S. Effect of surface treatment on shear bond strength of relining material and 3D-printed denture base. J. Adv. Prosthodont. 2022, 14, 262–272. [Google Scholar] [CrossRef]
- Palmer, D.S.; Barco, M.T.; Billy, E.J. Temperature extremes produced orally by hot and cold liquids. J. Prosthet. Dent. 1992, 67, 325–327. [Google Scholar] [CrossRef]
- Takahashi, Y.; Chai, J.; Kawaguchi, M. Effect of water sorption on the resistance to plastic deformation of a denture base material relined with four different denture reline materials. Int. J. Prosthodont. 1998, 11, 49–54. [Google Scholar] [PubMed]
- Gale, M.S.; Darvell, B.W. Thermal cycling procedures for laboratory testing of dental restorations. J. Dent. 1999, 27, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Minami, H.; Suzuki, S.; Minesaki, Y.; Kurashige, H.; Tanaka, T. In vitro evaluation of the influence of repairing condition of denture base resin on the bonding of autopolymerizing resins. J. Prosthet. Dent. 2004, 91, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Lassila, L.V.J.; Mutluay, M.M.; Tezvergil-Mutluay, A.; Vallittu, P.K. Bond strength of soft liners to fiber-reinforced denture-base resin. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2010, 19, 620–624. [Google Scholar] [CrossRef] [PubMed]
- Palitsch, A.; Hannig, M.; Ferger, P.; Balkenhol, M. Bonding of acrylic denture teeth to MMA/PMMA and light-curing denture base materials: The role of conditioning liquids. J. Dent. 2012, 40, 210–221. [Google Scholar] [CrossRef]
- do Carmo Viotto, H.E.; Silva, M.D.D.; Nunes, T.S.B.S.; Coelho, S.R.G.; Pero, A.C. Effect of repair methods and materials on the flexural strength of 3D-printed denture base resin. J. Adv. Prosthodont. 2022, 14, 305–314. [Google Scholar] [CrossRef]
- Jeong, K.W.; Kim, S.H. Influence of surface treatments and repair materials on the shear bond strength of CAD/CAM provisional restorations. J. Adv. Prosthodont. 2019, 11, 95–104. [Google Scholar] [CrossRef]
- Prpić, V.; Schauperl, Z.; Ćatić, A.; Dulčić, N.; Čimić, S. Comparison of Mechanical Properties of 3D-Printed, CAD/CAM, and Conventional Denture Base Materials. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2020, 29, 524–528. [Google Scholar] [CrossRef]
- Alfaraj, A.; Chu, T.M.G.; Alouthah, H.; Yang, C.C.; Lin, W.S. Tensile bond strength of auto-polymerizing and heat-polymerizing denture reliners on the conventional and CAD-CAM denture base materials. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2023, 32 (Suppl. S1), 87–95. [Google Scholar] [CrossRef]
- Pereira, A.L.C.; Troconis, C.C.M.; Curinga, M.R.S.; Curinga, M.A.S.E.; Barão, V.A.R.; Carreiro, A.D.F.P. Bond strength between denture lining material and CAD-CAM denture base resin: A systematic review and meta-analysis. J. Prosthet. Dent. 2023, in press. [CrossRef] [PubMed]
- Kulak-Ozkan, Y.; Sertgoz, A.; Gedik, H. Effect of thermocycling on tensile bond strength of six silicone-based, resilient denture liners. J. Prosthet. Dent. 2003, 89, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Awad, A.N.; Cho, S.H.; Kesterke, M.J.; Chen, J.H. Comparison of tensile bond strength of denture reline materials on denture bases fabricated with CAD-CAM technology. J. Prosthet. Dent. 2023, 129, 616–622. [Google Scholar] [CrossRef] [PubMed]
- Vallittu, P.K.; Ruyter, I.E. Swelling of poly(methyl methacrylate) resin at the repair joint. Int. J. Prosthodont. 1997, 10, 254–258. [Google Scholar] [PubMed]
- Alcântara, C.S.; Macêdo AFC de Gurgel, B.C.V.; Jorge, J.H.; Neppelenbroek, K.H.; Urban, V.M. Peel bond strength of resilient liner modified by the addition of antimicrobial agents to denture base acrylic resin. J. Appl. Oral Sci. 2012, 20, 607–612. [Google Scholar] [CrossRef][Green Version]
- Zidan, S.; Silikas, N.; Haider, J.; Alhotan, A.; Jahantigh, J.; Yates, J. Assessing Tensile Bond Strength Between Denture Teeth and Nano-Zirconia Impregnated PMMA Denture Base. Int. J. Nanomed. 2020, 15, 9611–9625. [Google Scholar] [CrossRef]
- Yang, Q.; Zheng, W.; Zhao, Y.; Shi, Y.; Wang, Y.; Sun, H.; Xu, X. Advancing dentin remineralization: Exploring amorphous calcium phosphate and its stabilizers in biomimetic approaches. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2024, 40, 1282–1295. [Google Scholar] [CrossRef]
- Yasser, A.D.; Abdul Fatah, N. The Effect of Addition of Zirconium Nano Particles on Antifungal Activity and Some Properties of Soft Denture Lining Material. J. Baghdad. Coll. Dent. 2017, 29, 27–32. [Google Scholar] [CrossRef]
- Fadhil Al-Tu’ma, A.; Dhubyan Mohammed Zaki, Z.; Ahmed, R.; Kamil Abbood, S.; Abdul Kadhim Ruhaima, A.; Jamal Hamoodah, Z.; SAbed, A.; Vpavlova, I. Inhibitory Effect of ZrO2NPs on Candida Albicans in Heat-Cured Acrylic-Based Soft Lining Material. J. Nanostruct. 2022, 12, 771–773. [Google Scholar]

| Materials (Brand Name) | Composition | Specimens Fabrication Method |
|---|---|---|
| Heat polymerized resin (HP) (Major Base.20, Major Prodotti Dentari Spa, Momcalieri, Italy) | Powder: Polymer (PMMA) þ initiator (benzoyl peroxide [BPO]) (0.5%) þ pigments (salts of cadmium or iron or organic dyes) Liquid: Monomer (MMA) þ cross-linking agent (Ethylene glycol dimethacrylate [EGDMA] 10%) þ inhibitor (hydroquinone) | Specimens fabricated conventionally via heat polymerization (heat water bath with increased temperature up to 74 °C for 90-min. followed by 100 °C for 30 min. |
| IvoCad (IvoCad, Ivoclar Vivadent, Schaan, Liechtenstein) | Prepolymerized PMMA discs 50–100% methyl methacrylate 2.5–10% 1,4-butanediol dimethacrylate | The pre-polymerized discs were mounted on a cutting saw ((Isomet 5000 Linear Precision Saw, Buehler Ltd., Bluff, IL, USA) to cut the specimens to the required dimensions using a diamond saw |
| AvaDent (AvaDent Digital Dental Solutions, Scottsdale, AZ, USA) | Prepolymerized PMMA (PMMA 99.5%, pigments < 1.0%) | |
| NextDent Denture 3D+ NextDent B.V., Soesterberg, The Netherlands | Ester-based monomer; Bisacylphosphine oxide (BAPO) phenylbis (2,4,6- trimethylbenzoyl)-phosphine oxide (Omnirad 819) | NextDent 5100 3D printer was used to print specimens with 50 µm Printing layer thickness and 0-degree printing orientation. After printing, specimens were post-cured using LC-3DPrint Box machine for 30-min. at 60 °C temperature |
| Formlabs Denture Base Resin LP Formlabs Inc., Somerville, MA, USA | 55–75% w/w urethane dimethacrylate, 15–25% w/w methacrylate monomers, and <0.9% w/w phenyl bis(2,4,6-trimethylbenzoyl)-phosphine oxide | Form 2 printer was used to print specimens with 50 µm Printing layer thickness and 0-degree printing orientation. After printing, specimens were post-cured using FormCure machine for 30-min. at 60 °C temperature |
| Hard Denture Reline GC AMERICA INC, Alsip, IL, USA | Isobutyl methacrylate dibenzoyl peroxide | Powder/liquid ratio is 15 mg powder to 6 mL liquid |
| Denture Base Resin and Code | Relining/NPs % | p-Value | |||
|---|---|---|---|---|---|
| 0% | 2% | 4% | |||
| Conventional | Heat-polymerized acrylic resin (HP) | 34.9 (11.9) a | 32.9 (9.1) MPa | 32.5 (16.4) | 0.912 |
| Milled | IvoCad (IVO) | 43.2 (6.9) A | 36.1 (10.1) B | 24.9 (8.1) A,B | 0.001 * |
| AvaDent (AVA) | 51.8 (13.3) a,b,c,A,B | 36.9 (12.3) B | 26.1 (15.9) A | 0.003 * | |
| 3D printed | FormLabs (FL) | 29.7 (9.2) b | 22.9 (12.5) | 20.0 (9.9) | 0.164 |
| NextDent (ND) | 31.1 (11.9) c | 22.9 (12.5) | 29.7 (15.5) | 0.689 | |
| 0.000 * | 0.033 * | 0.372 | |||
| Type III Sum of Squares | Df | Mean Square | F | p | |
|---|---|---|---|---|---|
| Intercept | 137,622.914 | 1 | 137,622.914 | 975.214 | 0.000 * |
| material * concentration | 8325.627 | 14 | 594.688 | 4.214 | 0.000 * |
| Error | 16,934.495 | 120 | 141.121 | ||
| Total | 162,883.037 | 135 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Albazroun, Z.; Alabdullatif, A.; Aldehaileb, S.; Alhalimi, F.; Alshahrani, F.A.; Khan, S.Q.; Fouda, S.M.; AlRumaih, H.S.; Gad, M.M. Bond Strength of Nanocomposite Hard Liner to CAD-CAM Milled, 3D Printed, and Conventionally Fabricated Denture Base Resins. Dent. J. 2024, 12, 275. https://doi.org/10.3390/dj12090275
Albazroun Z, Alabdullatif A, Aldehaileb S, Alhalimi F, Alshahrani FA, Khan SQ, Fouda SM, AlRumaih HS, Gad MM. Bond Strength of Nanocomposite Hard Liner to CAD-CAM Milled, 3D Printed, and Conventionally Fabricated Denture Base Resins. Dentistry Journal. 2024; 12(9):275. https://doi.org/10.3390/dj12090275
Chicago/Turabian StyleAlbazroun, Zainab, Atheer Alabdullatif, Sarah Aldehaileb, Ferdoos Alhalimi, Faris A. Alshahrani, Soban Q. Khan, Shaimaa M. Fouda, Hamad S. AlRumaih, and Mohammed M. Gad. 2024. "Bond Strength of Nanocomposite Hard Liner to CAD-CAM Milled, 3D Printed, and Conventionally Fabricated Denture Base Resins" Dentistry Journal 12, no. 9: 275. https://doi.org/10.3390/dj12090275
APA StyleAlbazroun, Z., Alabdullatif, A., Aldehaileb, S., Alhalimi, F., Alshahrani, F. A., Khan, S. Q., Fouda, S. M., AlRumaih, H. S., & Gad, M. M. (2024). Bond Strength of Nanocomposite Hard Liner to CAD-CAM Milled, 3D Printed, and Conventionally Fabricated Denture Base Resins. Dentistry Journal, 12(9), 275. https://doi.org/10.3390/dj12090275








