A Scoping Review of the Oral Health Status, Oral Health Behaviours and Interventions to Improve the Oral Health of Children and Young People in Care and Care Leavers
Abstract
1. Introduction
2. Materials and Methods
- (1)
- What is the prevalence of dental diseases among children and adolescents in care and care leavers?
- (2)
- What are the oral health behaviours of children and adolescents in care/care leavers?
- (3)
- What interventions have been developed for oral health promotion and improvement of care for children and adolescents in care/care leavers?
2.1. Inclusion and Exclusion Criteria
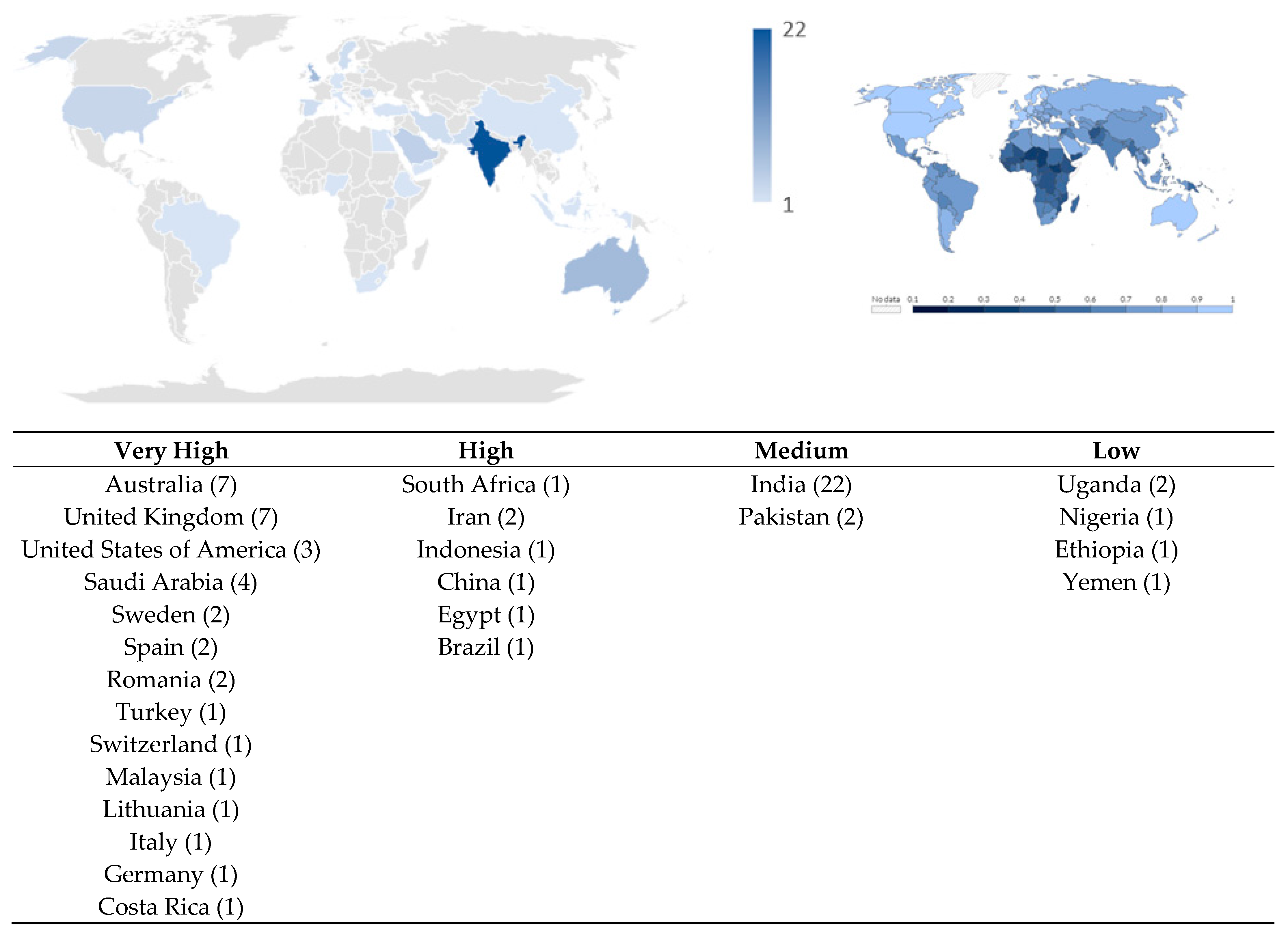
2.2. Search Strategy
2.3. Study Records
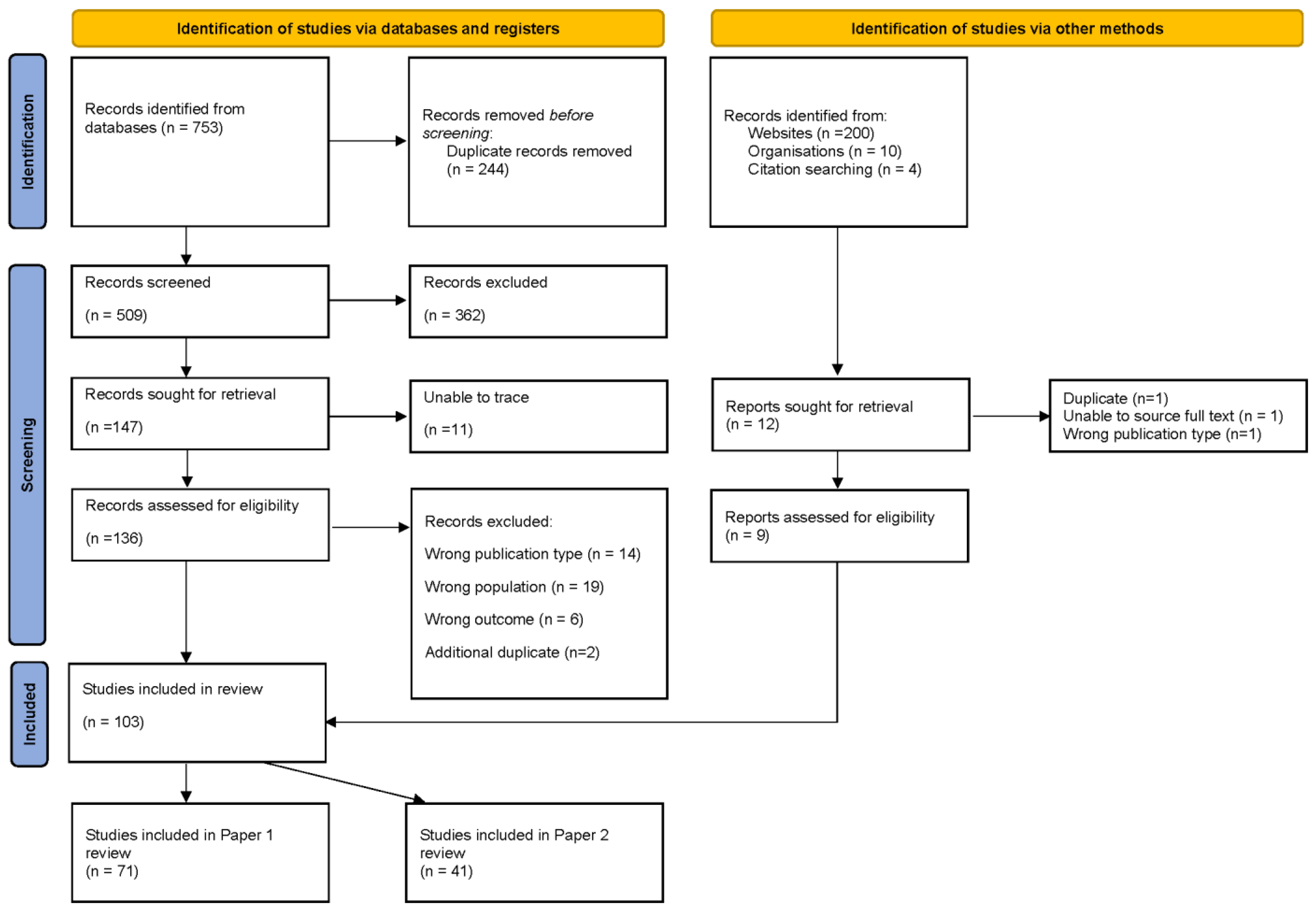
2.3.1. Data Management/Selection Process
2.3.2. Data Extraction
2.3.3. Data Synthesis
2.3.4. Patient and Public Involvement (PPI)
3. Results
3.1. What Is the Prevalence of Dental Diseases among Children and Adolescents in Care and Care Leavers?
3.1.1. Dental Caries
3.1.2. Periodontal Disease
3.1.3. Oral Hygiene
3.1.4. Dental Trauma
3.1.5. Occlusion and Orthodontic Treatment Need
3.1.6. Temporomandibular Disorders
3.1.7. Tooth Surface Loss
3.1.8. Soft Tissue Pathologies
3.1.9. Oral Health-Related Quality of Life
3.2. What Are the Oral Health Behaviours of Children and Adolescents in Care/Care Leavers?
3.2.1. Oral Health Self-Care Behaviours
3.2.2. Oral Health Knowledge and Perceptions
3.3. What Interventions Have Been Developed for Oral Health Promotion/Care for Children/Adolescents in Care/Care Leavers?
3.3.1. Oral Health Education
3.3.2. Supervised Toothbrushing
3.3.3. Dental Treatment or Preventative Care
4. Discussion
4.1. Statement of Principle Findings
4.2. Comparison with Existing Literature
4.3. Implications for Clinical Practice, Education and Policy
4.4. Strengths and Limitations of the Scoping Review
4.5. Unanswered Questions and Future Research Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Search Strategy
| 1 | (child* or youth* or adolescen* or teen* or young people).tw. |
| 2 | care leaver*.tw. |
| 3 | leaving care.tw. |
| 4 | (transit* adj3 (care or services)).tw. |
| 5 | child* in care.tw. |
| 6 | looked after child* .tw. |
| 7 | accommodated child.tw. |
| 8 | (“out of home care” or “out of home placement”).tw. |
| 9 | kinship care.tw. |
| 10 | ((adoption or adopted) adj3 child*).tw. |
| 11 | adopted child/ |
| 12 | (custod* adj3 care).tw. |
| 13 | orphan*tw. |
| 14 | (placement adj3 care).tw. |
| 15 | public care.tw. |
| 16 | (foster adj1 (care* or home* or family or parent*)).tw. |
| 17 | (institutional* adj3 (care or home*)).tw. |
| 18 | (group adj1 home*).tw. |
| 19 | (residential adj3 (care or home* or facilit*)).tw. |
| 20 | (welfare adj3 (care or system*)).tw. |
| 21 | statutory care.tw. |
| 22 | (care ajd3 local authority).tw. |
| 23 | care order*tw. |
| 24 | (substitute adj1 (care or famil*)).tw. |
| 25 | special guardian*.tw. |
| 26 | Kafalah.tw. |
| 27 | (unaccompanied adj3 asylum).tw. |
| 28 | (unaccompanied adj3 refugee*).tw. |
| 29 | (“Children Act 1989” or “Children Northern Ireland Order 1995” or “Children Scotland Act 1995”).tw. |
| 30 | or/5–29 |
| 31 | dental health/ |
| 32 | dental procedure/ |
| 33 | exp tooth disease/ |
| 34 | exp dentist/ |
| 35 | (oral adj3 (health* or hygiene or care)).ab,kw,ti. |
| 36 | dental.ab,kw,ti. |
| 37 | ((tooth adj3 (health* or hygiene or care or brush* or floss*)) or toothbrush*).ab,kw,ti. |
| 38 | (teeth adj3 (health* or hygiene or care or brush* or floss*)).ab,kw,ti. |
| 39 | dentist*.ab,kw,ti. |
| 40 | or/31–39 |
| 41 | (1 or 2 or 3) and 30 and 40 |
References
- Better Care Network. The Continuum of Care. 2022. Available online: https://bettercarenetwork.org/library/the-continuum-of-care (accessed on 27 February 2022).
- Delap, E.; Melville, L. Fostering Better Care: Improving Foster Care Provision Around the World, Every Child. 2011. Available online: https://bettercarenetwork.org/sites/default/files/Fostering%20Better%20Care%20-%20Improving%20Foster%20Care%20Provision%20Around%20the%20World.pdf (accessed on 27 February 2022).
- United Nations General Assembly, Guidelines for the Alternative Care of Children: Resolution Adopted by the General Assembly, UN, New York. 2010. Available online: https://resourcecentre.savethechildren.net/pdf/5416.pdf/ (accessed on 27 February 2022).
- UNICEF Data: Monitoring the Situation of Children and Women, Children in Alternative Care. 2022. Available online: https://data.unicef.org/topic/child-protection/children-alternative-care/ (accessed on 27 September 2022).
- Murray, E.T.; Lacey, R.; Maughan, B.; Sacker, A. Non-parental care in childhood and health up to 30 years later: ONS Longitudinal Study 1971–2011. Eur. J. Public Health 2020, 30, 1121–1127. [Google Scholar] [CrossRef]
- UK Parliament, Mental Health and Well-Being of Looked-After Children. 2016. Available online: https://publications.parliament.uk/pa/cm201516/cmselect/cmeduc/481/48102.htm (accessed on 27 May 2022).
- Ford, T.; Vostanis, P.; Meltzer, H.; Goodman, R. Psychiatric disorder among British children looked after by local authorities: Comparison with children living in private households. Br. J. Psychiatry 2007, 190, 319–325. [Google Scholar] [CrossRef] [PubMed]
- McAuley, C.; Davis, T. Emotional well-being and mental health of looked after children in England. Child. Fam. Soc. Work 2009, 14, 147–155. [Google Scholar] [CrossRef]
- Oftsed, ‘Ready or Not’: Care Leavers’ Views of Preparing to Leave Care. 2022. Available online: https://www.gov.uk/government/publications/ready-or-not-care-leavers-views-of-preparing-to-leave-care/ready-or-not-care-leavers-views-of-preparing-to-leave-care (accessed on 27 May 2023).
- Reeve, K. The Hidden Truth about Homelessness: Experiences of Single Homelessness in England; Crisis, 2011. Available online: https://www.crisis.org.uk/media/236816/the_hidden_truth_about_homelessness_es.pdf (accessed on 27 February 2022).
- Berman, G. Prison Population Statistics. 2013. Available online: http://www.antoniocasella.eu/nume/Berman_2013.pdf (accessed on 27 May 2023).
- Office for National Statistics, Who Are the Children Entering Care in England? 2022. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/socialcare/articles/whoarethechildrenenteringcareinengland/2022-11-04 (accessed on 27 May 2023).
- Erwin, J.; Horrell, J.; Wheat, H.; Axford, N.; Burns, L.; Booth, J.; Witton, R.; Shawe, J.; Doughty, J.; Kaddour, S.; et al. Access to Dental Care for Children and Young People in Care and Care Leavers: A Global Scoping Review. Dent. J. 2024, 12, 37. [Google Scholar] [CrossRef]
- Ridsdale, L.; Johnston, L.; James, N.; Balmer, R. Looked after children: An overview for the dental team. Br. Dent. J. 2023, 234, 34–38. [Google Scholar] [CrossRef] [PubMed]
- Local Government Association, Tackling Poor Oral Health in Children. 2016. Available online: https://www.local.gov.uk/sites/default/files/documents/tackling-poor-oral-health-d84.pdf (accessed on 27 May 2023).
- Hurry, K.J.; Ridsdale, L.; Davies, J.; Muirhead, V.E. The Dental Health of Looked After Children in the UK and Dental Care Pathways: A Scoping Review. Community Dent. Health 2023, 40, 154–161. [Google Scholar] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- World Population Review, Human Development Index (HDI) by Country 2023. 2023. Available online: https://worldpopulationreview.com/country-rankings/hdi-by-country (accessed on 27 May 2023).
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Pollock, A.; Campbell, P.; Struthers, C.; Synnot, A.; Nunn, J.; Hill, S.; Goodare, H.; Morris, J.; Watts, C.; Morley, R. Development of the ACTIVE framework to describe stakeholder involvement in systematic reviews. J. Health Serv. Res. Policy 2019, 24, 245–255. [Google Scholar] [CrossRef]
- Jenner, A.; Ramseier, C.A. Impact of a single information session with oral hygiene instructions on unaccompanied minor asylum seekers living in Switzerland. Swiss Dent. J. 2022, 132, 404–413. [Google Scholar]
- Sarvas, E.W.; Eckerle, J.K.; Gustafson, K.L.; Freese, R.L.; Shlafer, R.J. Oral health needs among youth with a history of foster care: A population-based study. J. Am. Dent. Assoc. 2021, 152, 589–595. [Google Scholar] [CrossRef]
- Al-Maweri, S.A.; Al-Soneidar, W.A.; Halboub, E.S. Oral lesions and dental status among institutionalized orphans in Yemen: A matched case-control study. Contemp. Clin. Dent. 2021, 5, 81–84. [Google Scholar] [CrossRef]
- Meshki, R.; Basir, L.; Motaghi, S.; Kazempour, M. Oral health status among orphan and non-orphan children in Mashhad: A case-control study. J. Med. Life 2022, 15, 1198–1201. [Google Scholar] [CrossRef]
- Kamyabi, H.; Darijani, M.A.; Amanpour, S.; Yazdi-Feyzabadi, V.; Fereidooni, R.; Fardisi, S. Oral health-related quality of life among children aged 11-14 years old with and without parental care in south-east of Iran. Pesqui 2023, 23, e220103. [Google Scholar] [CrossRef]
- Khattab, N.M.; Abd-Elsabour, M.A. Assessment of dental caries among a group of institutionalized orphan children compared to parented school children: Case–control study. BMC Oral. Health 2023, 23, 202. [Google Scholar] [CrossRef]
- Chambers, M.F.; Saunders, A.M.; New, B.D.; Williams, C.L.; Stachurska, A. Assessment of children coming into care: Processes, pitfalls and partnerships. Clin. Child. Psychol. Psychiatry 2010, 15, 511–527. [Google Scholar] [CrossRef]
- Khedekar, M.; Suresh, K.V.; Parkar, M.I.; Malik, N.; Patil, S.; Taur, S.; Pradhan, D. Implementation of oral health education to orphan children. J. Coll. Physicians Surg. Pak. 2015, 25, 856–859. [Google Scholar] [PubMed]
- Valpreda, L.; Carcieri, P.; Cabras, M.; Vecchiati, G.; Arduino, P.G.; Bassi, F. Frequency and severity of dental caries in foster care children of Turin, Italy: A retrospective cohort study. Eur. J. Paediatr. Dent. 2020, 21, 299–302. [Google Scholar] [PubMed]
- Chernoff, R.; Combs-Orme, T.; Risley-Curtiss, C.; Heisler, A. Assessing the health status of children entering foster care. Pediatrics 1994, 93, 594–601. [Google Scholar] [CrossRef] [PubMed]
- Randsalu, L.S.; Laurell, L. Children in out-of-home care are at high risk of somatic, dental and mental ill health. Acta Paediatr. 2018, 107, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.; Cassar, C.; Siggers, G.; Taylor, S. Medical and social issues of child refugees in Europe. Arch. Dis. Child. 2016, 101, 839–842. [Google Scholar] [CrossRef]
- Moeller-Saxone, M.; McCutcheon, L.; Halperin, S.; Herrman, H.; Chanen, A. Meeting the primary care needs of young people in residential care. Aust. Fam. Physician. 2016, 45, 706–711. [Google Scholar]
- Supporting and Promoting the Health Needs of Looked After Children; Local Government Association, Healthy Futures: London, UK, 2016.
- Mooney, Promoting the Health of Looked after Children: A Study to Inform Revision of the 2002 Guidance. 2009. Available online: https://dera.ioe.ac.uk/id/eprint/11156/1/DCSF-RR125.pdf (accessed on 27 May 2023).
- McSherry, D.; Fargas Malet, M.; McLaughlin, K.; Adams, C.; O’Neill, N.; Cole, J.; Walsh, C. Mind your Health: The Physical and Mental Health of Looked after Children and Young People in Northern Ireland. 2016. Available online: https://pureadmin.qub.ac.uk/ws/portalfiles/portal/17213677/mind_your_health_report_october_2015.pdf (accessed on 27 May 2023).
- Vinnerljung, B.; Hjern, A. Health and health care for children in out–of–home care. Int. J. Soc. Welf. 2018, 27, 321–324. [Google Scholar] [CrossRef]
- Williams, J.; Jackson, S.; Maddocks, A.; Cheung, W.Y.; Love, A.; Hutchings, H. Case–control study of the health of those looked after by local authorities. Arch. Dis. Child. 2001, 85, 280–285. [Google Scholar] [CrossRef]
- Shmerling, E.; Creati, M.; Belfrage, M.; Hedges, S. The health needs of Aboriginal and Torres Strait Islander children in out-of-home care. J. Paediatr. Child. Health 2020, 56, 384–388. [Google Scholar] [CrossRef]
- Raman, S.; Sahu, S. Health, Developmental and Support Needs of Vulnerable Children—Comparing Children in Foster Care and Children in Need. Child. Abus. Rev. 2014, 23, 415–425. [Google Scholar] [CrossRef]
- Raman, S.; Reynolds, S.; Khan, R. Addressing the well-being of Aboriginal children in out-of-home care: Are we there yet? J. Paediatr. Child. Health 2011, 47, 806–811. [Google Scholar] [CrossRef] [PubMed]
- Espeleta, H.C.; Schelbe, L.; Ruggiero, K.J.; Klika, J.B. Initial health outcomes of a community-based collaboration for children in Foster Care. Health Soc. Work. 2023, hlad038. [Google Scholar] [CrossRef] [PubMed]
- Christian, B.; Ummer-Christian, R.; Blinkhorn, A.; Hegde, V.; Nandakumar, K.; Marino, R.; Chattopadhyay, A. An epidemiological study of dental caries and associated factors among children residing in orphanages in Kerala, India: Health in Orphanages Project (HOPe). Int. Dent. J. 2019, 69, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Solis-Riggioni, A.; Gallardo-Barquero, C.; Chavarria-Bolanos, D. Prevalence and Severity of Dental Caries in Foster-Care Children and Adolescents. J. Clin. Pediatr. Dent. 2018, 42, 269–272. [Google Scholar] [CrossRef] [PubMed]
- Alsaif, A.A.; Alkhadra, T.A.; AlJameel, A.H. Impact of DMFT, PUFA, DAI, and TDIs on Oral Health-Related Quality of Life (OHRQoL) Among Foundling, Delinquent, and Mainstream School Children: A Preliminary Study. Front. Public Health 2022, 10, 894638. [Google Scholar] [CrossRef]
- Kamran, R.; Farooq, W.; Faisal, M.R.; Jahangir, F. Clinical consequences of untreated dental caries assessed using PUFA index and its covariates in children residing in orphanages of Pakistan. BMC Oral Health 2017, 17, 108. [Google Scholar] [CrossRef]
- Shanbhog, R.; Godhi, B.S.; Nandlal, B.; Kumar, S.S.; Raju, V.; Rashmi, S. Clinical consequences of untreated dental caries evaluated using PUFA index in orphanage children from India. J. Int. Oral. Health 2013, 5, 1–9. [Google Scholar]
- Rauter, M.; Jayakar, A.; Clemens, T.; Galanos, Z.; Newbery, L.; Whelan, A. Health of Southern Tasmanian 4- to 6-year-old children in out-of-home care compared to peers. J. Paediatr. Child. Health 2018, 54, 405–410. [Google Scholar] [CrossRef]
- Mohan, A.; Misra, N.; Umapathy, D.; Kumar, S.; Srivastav, D.; Mohan, U. Oral and Dental Health Status in Orphan Children of Lucknow. Indian. J. Community Health 2014, 26, 170–173. [Google Scholar]
- Olivan-Gonzalvo, G.; Parte-Serna, A.C. Prevalence of untreated dental caries in Latin American children in the Spanish child protection system. Iberoam. J. Med. 2020, 2, 261–267. [Google Scholar] [CrossRef]
- Khare, V.; Koshy, A.; Rani, P.J.; Srilatha, S.; Kapse, S.C.; Agrawal, A. Prevalence of dental caries and treatment needs among the orphan children and adolescents of Udaipur District, Rajasthan, India. J. Contemp. Dent. Pract. 2012, 13, 182–187. [Google Scholar]
- Dixit, S.; Chaudhary, M.; Singh, A. Molluscum contagiosum and dental caries: A pertinent combination. J. Indian Soc. Pedod. Prev. Dent. 2009, 27, 197–201. [Google Scholar] [CrossRef]
- Alsayeh, A.; Abdulbaseer, M.; Aljelaly, H.; Alshamrani, B.; Aldaijy, R.; Alshlash, K.; Odeh, T.; Alshiha, A. Dentition status and treatment needs among orphans in Riyadh city, Saudi Arabia: A cross-sectional descriptive study. Open Dent. J. 2020, 14, 203–210. [Google Scholar] [CrossRef]
- O’Sullivan, E.A.; Stephens, A.J. The oral and dental status of children residing in a Romanian orphanage. Int. J. Paediatr. Dent. 1997, 7, 41–42. [Google Scholar] [CrossRef]
- Virk, P.; Jain, R.L.; Pathak, A.; Sharma, U.; Rajput, J.S. Inter-relationship of intelligence-quotient and self-concept with dental caries amongst socially handicapped orphan children. J. Indian Soc. Pedod. Prev. Dent. 2012, 30, 127–132. [Google Scholar] [CrossRef]
- Shanbhog, R.; Raju, V.; Nandlal, B. Correlation of oral health status of socially handicapped children with their oral heath knowledge, attitude, and practices from India. J. Nat. Sci. Biol. Med. 2014, 5, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Thetakala, R.K.; Sunitha, S.; Chandrashekar, B.R.; Sharma, P.; Krupa, N.C.; Srilatha, Y. Periodontal and Dentition Status among Orphans and Children with Parents in Mysore City, India: A Comparative Study. J. Clin. Diagn. Res. 2017, 11, ZC115–ZC118. [Google Scholar] [CrossRef] [PubMed]
- Kling, S.; Vinnerljung, B.; Hjern, A. Somatic assessments of 120 Swedish children taken into care reveal large unmet health and dental care needs. Acta Paediatr. 2016, 105, 416–420. [Google Scholar] [CrossRef] [PubMed]
- Blignaut, E. Oral health needs of HIV/AIDS orphans in Gauteng, South Africa. AIDS Care 2007, 19, 532–538. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Zhu, Y.; Wang, C.; Wang, D. The Dental Health of Orphan and Non-orphan Children in Fuyang City, China. Oral. Health Prev. Dent. 2021, 19, 523–528. [Google Scholar] [PubMed]
- Morón, E.M.; Tomar, S.L.; Souza, R.; Balzer, J.; Savioli, C.; Shawkat, S. Dental Status and Treatment Needs of Children in Foster Care. Pediatr. Dent. 2019, 41, 206–210. [Google Scholar] [PubMed]
- Ehlers, V.; Callaway, A.; Wantzen, S.; Patyna, M.; Deschner, J.; Azrak, B. Oral health of children and adolescents with or without attention deficit hyperactivity disorder (ADHD) living in residential care in rural Rhineland-Palatinate, Germany. BMC Oral. Health 2019, 19, 258. [Google Scholar] [CrossRef]
- Pavithran, V.K.; Murali, R.; Krishna, M.; Shamala, A.; Yalamalli, M.; Kumar, A.V.; Raina, R. Impact of oral diseases on daily activities among 12- to 15-year-old institutionalized orphan and non-orphan children in Bengaluru city: A cross-sectional analytical study. Indian J. Dent. Res. 2020, 31, 396–402. [Google Scholar] [CrossRef]
- Kumari, A.; Marya, C.; Oberoi, S.S.; Nagpal, R.; Bidyasagar, S.C.; Taneja, P. Oral Hygiene Status and Gingival Status of the 12- to 15-year-old Orphanage Children Residing in Delhi State: A Cross-sectional Study. Int. J. Clin. Pediatr. Dent. 2021, 14, 482–487. [Google Scholar]
- Al-Jobair, A.M.; Al-Sadhan, S.A.; Al-Faifi, A.A.; Andijani, R.I.; Al-Motlag, S.K. Medical and dental health status of orphan children in central Saudi Arabia. Saudi Med. J. 2013, 34, 531–536. [Google Scholar]
- Oliván-Gonzalvo, G. Health status and infectious diseases in male unaccompanied immigrant minors from Africa in Spain. Enferm. Infecc. Microbiol. Clin. 2021, 39, 340–344. [Google Scholar] [CrossRef]
- Dumitrache, M.A.; Caramida, M.; Romanița Ilici, R. Oral health-related knowledge, behaviour and status in a group of institutionalized children in Valenii de Munte, Romania. Int. J. Med. Dent. 2020, 24, 197–201. [Google Scholar]
- Ojahanon, P.I.; Akionbare, O.; Umoh, A.O. The oral hygiene status of institution dwelling orphans in Benin City, Nigeria. Niger. J. Clin. Pract. 2013, 16, 41–44. [Google Scholar] [CrossRef]
- Rubin, P.F.; Winocur, E.; Erez, A.; Birenboim-Wilensky, R.; Peretz, B. Dental Treatment Needs among Children and Adolescents Residing in an Ugandan Orphanage. J. Clin. Pediatr. Dent. 2016, 40, 486–489. [Google Scholar] [CrossRef]
- Goswami, M.; Bhardwaj, S. Assessment of Traumatic Dental Injuries among Institutionalized Orphan Children: A Cross-sectional Study. Int. J. Clin. Pediatr. Dent. 2022, 15, 124–127. [Google Scholar]
- AlSadhan, S.A.; Al-Jobair, A.M. Oral habits, dental trauma, and occlusal characteristics among 4- to 12-year-old institutionalized orphan children in Riyadh, Saudi Arabia. Spec. Care Dentist. 2017, 37, 10–18. [Google Scholar] [CrossRef]
- Sarri, G.; Evans, P.; Stansfeld, S.; Marcenes, W. A school-based epidemiological study of dental neglect among adolescents in a deprived area of the UK. Br. Dent. J. 2017, 213, E17. [Google Scholar] [CrossRef]
- Ahammed, A.R.; Shetty, V.; Panda, A.K.; Gunda, S.; Pradhan, D.; Husain, N.; Gugwad, S. Prevalence of malocclusion among 12 to 15 years age group orphan children using dental aesthetic index. J. Contemp. Dent. Pract. 2013, 14, 111–114. [Google Scholar]
- Kumar, D.A.; Varghese, R.K.; Chaturvedi, S.S.; Agrawal, A.; Fating, C.; Makkad, R.S. Prevalence of malocclusion among children and adolescents residing in orphanages of Bilaspur, Chattishgarh, India. J. Adv. Oral. Res. 2012, 3, 21–28. [Google Scholar] [CrossRef]
- Sermet Elbay, U.; Demirturk Kocasarac, H.; Elbay, M.; Kaya, C.; Ugurluel, C.; Baydemir, C. Temporomandibular disorders and oral parafunction in children living with their parents and children living in institutional protective care: A comparative study. Int. Dent. J. 2017, 67, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Friedman Rubin, P.; Erez, A.; Peretz, B.; Birenboim-Wilensky, R.; Winocur, E. Prevalence of bruxism and temporomandibular disorders among orphans in southeast Uganda: A gender and age comparison. Cranio 2018, 36, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Rodolfo Tavares de Melo, J.; Brito Vasconcelos, G.; Kelly Barreira, A.; Colares, V. Assessment of self-injurious behavior and oral injuries among adolescents in Shelter Care: A cross-sectional study. Vulnerable Child. Youth Stud. 2023, 18, 431–444. [Google Scholar] [CrossRef]
- Hans, R.; Thomas, S.; Dagli, R.; Bhateja, G.A.; Sharma, A.; Singh, A. Oral health knowledge, Attitude and practices of children and adolescents of orphanages in jodhpur city rajasthan. India. J. Clin. Diagn. Res. 2014, 8, ZC22–ZC25. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Goyal, A.; Tadakamadla, J.; Tibdewal, H.; Duraiswamy, P.; Kulkarni, S. Oral health related quality of life among children with parents and those with no parents. Community Dent. Health 2011, 28, 227–231. [Google Scholar] [PubMed]
- Kelly, A.R. Factors Associated with the Ability of the Care System to Meet the Physical and Mental Health Needs of Young People Looked after in England: A Mixed-Methods Study. Ph.D. Thesis, Department of Education, University of Oxford, Oxford, UK, 2022. [Google Scholar]
- Shah, A.F.; Tangade, P.; Ravishankar, T.L.; Tirth, A.; Pal, S.; Batra, M. Dental Caries Status of Institutionalized Orphan Children from Jammu and Kashmir, India. Int. J. Clin. Pediatr. Dent. 2016, 9, 364–371. [Google Scholar]
- Sushanth, V.H.; Krishna, M.; Suresh Babu, A.M.; Prashant, G.M.; Chandu, G.N. A peer group approach model of oral health promotion among orphans at Puduchery, South India. J. Int. Soc. Prev. Community Dent. 2011, 1, 71–75. [Google Scholar] [CrossRef]
- Shanthi, M.; Goud, E.V.S.S.; Kumar, G.P.; Rajguru, J.P.; Ratnasothy, S.; Ealla, K.K. Risk Factors and Treatment Needs among Orphan School Children. J. Contemp. Dent. Pract. 2017, 18, 893–898. [Google Scholar] [CrossRef]
- Unnikrishnan, V.; Dhamali, D.; Balakrishna, M.S.; Kavya, M.J.; Saheer, A.; Chandran, T. Perception of oral health and practices among children residing in orphanages in Bengaluru. J. Pharm. Bioallied Sci. 2022, 14 (Suppl. 1), S420–S423. [Google Scholar] [PubMed]
- Markeviciute, G.; Narbutaite, J. Effectiveness of a Motivation and Practical Skills Development Methods on the Oral Hygiene of Orphans Children in Kaunas, Lithuania. J. Oral. Maxillofac. Res. 2015, 6, e2. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Saleem, J.; Ishaq, M.; Butt, M.S.; Zakar, R.; Malik, U.; Iqbal, M.; Fischer, F. Oral health perceptions and practices of caregivers at children’s religious schools and foster care centers: A qualitative exploratory study in Lahore, Pakistan. BMC Oral. Health 2022, 22, 641. [Google Scholar] [CrossRef] [PubMed]
- Burnett, D.; Aronson, J.; Asgary, R. Oral health status, knowledge, attitudes and behaviours among marginalized children in Addis Ababa, Ethiopia. J. Child. Health Care 2016, 20, 252–261. [Google Scholar] [CrossRef]
- Muralidharan, D.; Fareed, N.; Shanthi, M. Comprehensive dental health care program at an orphanage in Nellore district of Andhra Pradesh. Indian J. Dent. Res. 2012, 23, 171–175. [Google Scholar] [CrossRef]
- Muirhead, V.; Subramanian, S.K.; Wright, D.; Wong, F.S.L. How do foster carers manage the oral health of children in foster care? A qualitative study. Community Dent. Oral. Epidemiol. 2017, 45, 529–537. [Google Scholar] [CrossRef]
- Vijayasekaram, R.; Senerath, O.; Thevarasah, N.; Baig, M.H.; Raj, S.S. A tailored tooth brushing program to control plaque accumulation and gingivitis among orphan children: A randomized trial. J. Glob. Oral. Health 2020, 3, 118–123. [Google Scholar] [CrossRef]
- Shekhar, M.G.; Abraham, S.; Joy, S.; Mahabob, N. Comparative Evaluation of Powered and Manual Toothbrushes in Reducing Plaque and Gingivitis in Institutionalized Orphan Children. J. Int. Dent. Med. Res. 2022, 15, 735–740. [Google Scholar]
- Fadjeri, I.; Budiarti, R.; Purnama, T. Dental care interventions as efforts to reduce pufa index and improve nutritional status in children aged 9–12 years in orphanages. Med.-Leg. Update 2021, 21, 366–371. [Google Scholar]
- Public Health England, Improving Oral Health: Supervised Tooth Brushing Programme Toolkit. 2016. Available online: https://www.gov.uk/government/publications/improving-oral-health-supervised-tooth-brushing-programme-toolkit (accessed on 27 May 2023).
- da Silva, S.N.; Gimenez, T.; Souza, R.C.; Mello-Moura, A.C.V.; Raggio, D.P.; Morimoto, S.; Lara, J.S.; Soares, G.C.; Tedesco, T.K. Oral health status of children and young adults with autism spectrum disorders: Systematic review and meta-analysis. Int. J. Paediatr. Dent. 2017, 27, 388–398. [Google Scholar] [CrossRef]
- Erwin, J.; Paisi, M.; Neill, S.; Burns, L.; Vassallo, I.; Nelder, A.; Facenfield, J.; Devalia, U.; Vassallo, T.; Witton, R. Factors influencing oral health behaviours, access and delivery of dental care for autistic children and adolescents: A mixed-methods systematic review. Health Expect. 2022, 25, 1269–1318. [Google Scholar] [CrossRef]
- Department for Education, Looked-After Children: Improving Permanence. 2013. Available online: https://www.gov.uk/government/publications/improving-permanence-for-looked-after-children-data-pack (accessed on 27 May 2023).
- Barriers and Facilitators for Promoting Physical, Mental and Emotional Health and Wellbeing of Looked-After Children and Young People and Care Leavers; National Institute for Health and Care Excellence, 2021. Available online: https://www.nice.org.uk/guidance/ng205/evidence/g-barriers-and-facilitators-for-promoting-physical-mental-and-emotional-health-and-wellbeing-of-lookedafter-children-and-young-people-and-care-leavers-pdf-333471052729 (accessed on 5 February 2024).
- Ward, H.; Jones, H.; Lynch, M.; Skuse, T. Issues concerning the Health of Looked after Children. Adopt. Foster. 2002, 26, 8–18. [Google Scholar] [CrossRef]
- Murray, E.T.; Lacey, R.; Maughan, B.; Sacker, A. Association of childhood out-of-home care status with all-cause mortality up to 42-years later: Office of National Statistics Longitudinal Study. BMC Public. Health 2020, 20, 735. [Google Scholar] [CrossRef] [PubMed]
- Grant, M.J.; Booth, A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Inf. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef] [PubMed]
- Paez, A. Grey literature: An important resource in systematic reviews. J. Evid. Based Med. 2017, 10, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Sheiham, A.; James, W.P. Diet and Dental Caries: The Pivotal Role of Free Sugars Reemphasized. J. Dent. Res. 2015, 94, 1341–1347. [Google Scholar] [CrossRef]
- The Care Leavers’ Association, Caring for Better Health: An Investigation into the Health Needs of Care Leavers. 2017. Available online: https://www.careleavers.com/wp-content/uploads/2017/12/Caring-for-Better-Health-Final-Report.pdf (accessed on 27 May 2023).
- Paisi, M.; Kay, E.; Plessas, A.; Burns, L.; Quinn, C.; Brennan, N.; White, S. Barriers and enablers to accessing dental services for people experiencing homelessness: A systematic review. Community Dent. Oral. Epidemiol. 2019, 47, 103–111. [Google Scholar] [CrossRef]
- Booth, J.; O’Malley, L.; Meek, R.; Mc Goldrick, N.; Maycock, M.; Clarkson, J.; Wanyonyi-Kay, K. A scoping review of interventions to improve oral health in prison settings. Community Dent. Oral. Epidemiol. 2023, 51, 373–379. [Google Scholar] [CrossRef]
| Total Number of Studies | ||||
|---|---|---|---|---|
| Oral Health Outcomes (n = 59) | Low n = 5 | Medium n = 19 | High n = 4 | Very High n = 31 |
| Dental caries/PUFA | 6 | 14 | 3 | 18 |
| Periodontal disease | 1 | 5 | 1 | 7 |
| Oral hygiene | 2 | 4 | 2 | 8 |
| Dental trauma | 1 | 1 | 0 | 5 |
| Occlusion and orthodontic treatment need | 1 | 2 | 0 | 5 |
| Tooth surface loss | 2 | 0 | 0 | 1 |
| Temporomandibular disorders | 0 | 1 | 0 | 1 |
| Oral medicine conditions | 2 | 2 | 1 | 0 |
| Oral health related quality of life | 0 | 3 | 2 | 5 |
| General dental health | 0 | 0 | 0 | 10 |
| Oral Health Behaviours (n = 23) | Low n = 2 | Medium n = 9 | High n = 1 | Very High n = 11 |
| Oral health self-care | 2 | 7 | 1 | 6 |
| Oral health knowledge and perceptions | 0 | 5 | 0 | 5 |
| Oral Health Interventions (n = 8) | Low n = 0 | Medium n = 4 | High n = 1 | Very High n = 3 |
| Oral health education | 0 | 4 | 0 | 2 |
| Dental treatment or preventative care | 0 | 1 | 1 | 0 |
| Supervised toothbrushing | 0 | 2 | 0 | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Booth, J.; Erwin, J.; Burns, L.; Axford, N.; Horrell, J.; Wheat, H.; Witton, R.; Shawe, J.; Doughty, J.; Kaddour, S.; et al. A Scoping Review of the Oral Health Status, Oral Health Behaviours and Interventions to Improve the Oral Health of Children and Young People in Care and Care Leavers. Dent. J. 2024, 12, 38. https://doi.org/10.3390/dj12020038
Booth J, Erwin J, Burns L, Axford N, Horrell J, Wheat H, Witton R, Shawe J, Doughty J, Kaddour S, et al. A Scoping Review of the Oral Health Status, Oral Health Behaviours and Interventions to Improve the Oral Health of Children and Young People in Care and Care Leavers. Dentistry Journal. 2024; 12(2):38. https://doi.org/10.3390/dj12020038
Chicago/Turabian StyleBooth, Joelle, Jo Erwin, Lorna Burns, Nick Axford, Jane Horrell, Hannah Wheat, Robert Witton, Jill Shawe, Janine Doughty, Sarah Kaddour, and et al. 2024. "A Scoping Review of the Oral Health Status, Oral Health Behaviours and Interventions to Improve the Oral Health of Children and Young People in Care and Care Leavers" Dentistry Journal 12, no. 2: 38. https://doi.org/10.3390/dj12020038
APA StyleBooth, J., Erwin, J., Burns, L., Axford, N., Horrell, J., Wheat, H., Witton, R., Shawe, J., Doughty, J., Kaddour, S., Boswell, S., Devalia, U., Nelder, A., & Paisi, M. (2024). A Scoping Review of the Oral Health Status, Oral Health Behaviours and Interventions to Improve the Oral Health of Children and Young People in Care and Care Leavers. Dentistry Journal, 12(2), 38. https://doi.org/10.3390/dj12020038






