Diet, Nutrition, and Oral Health in Older Adults: A Review of the Literature
Abstract
:1. Introduction
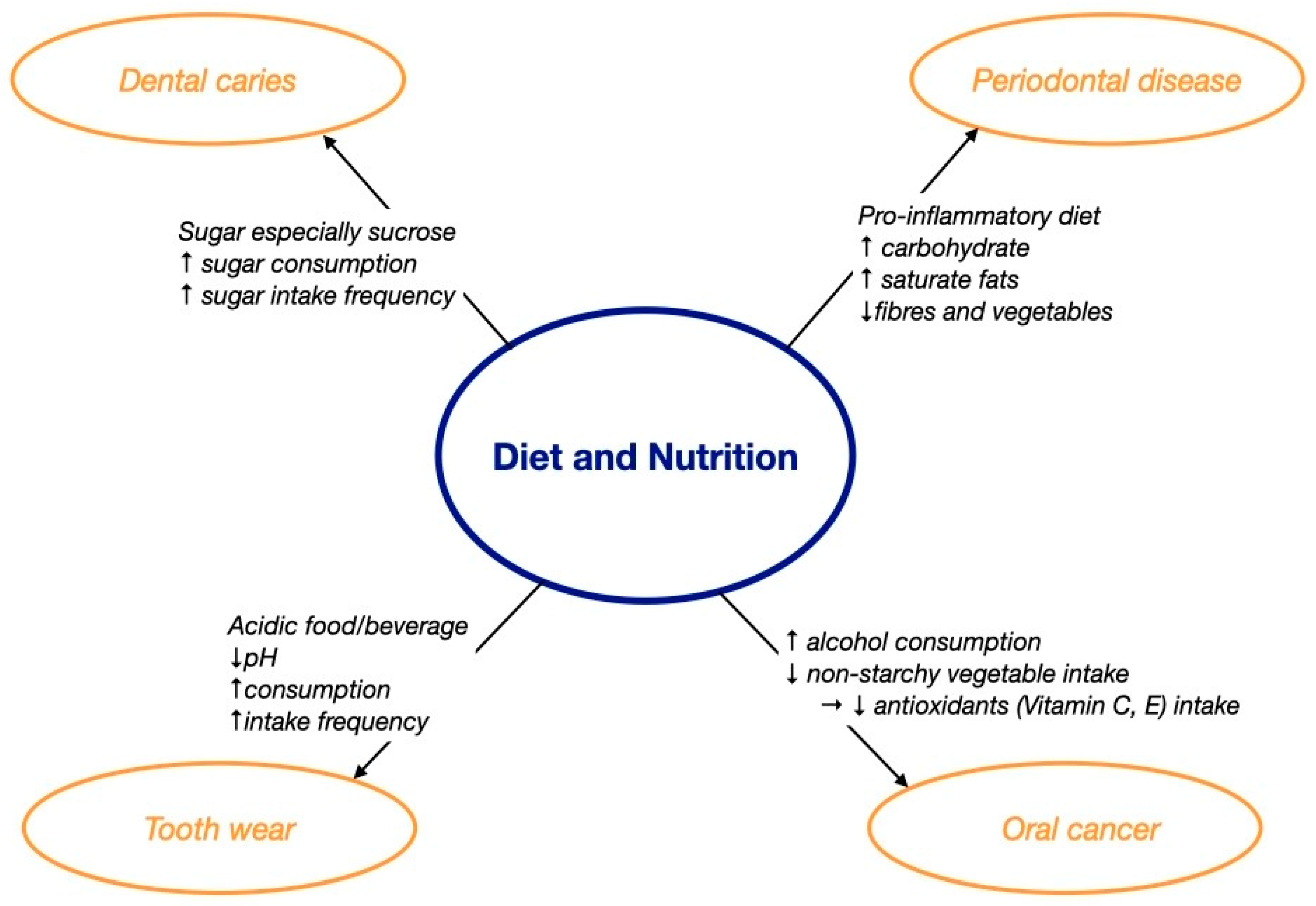
2. The Impact of Diet and Nutrition on Oral Health
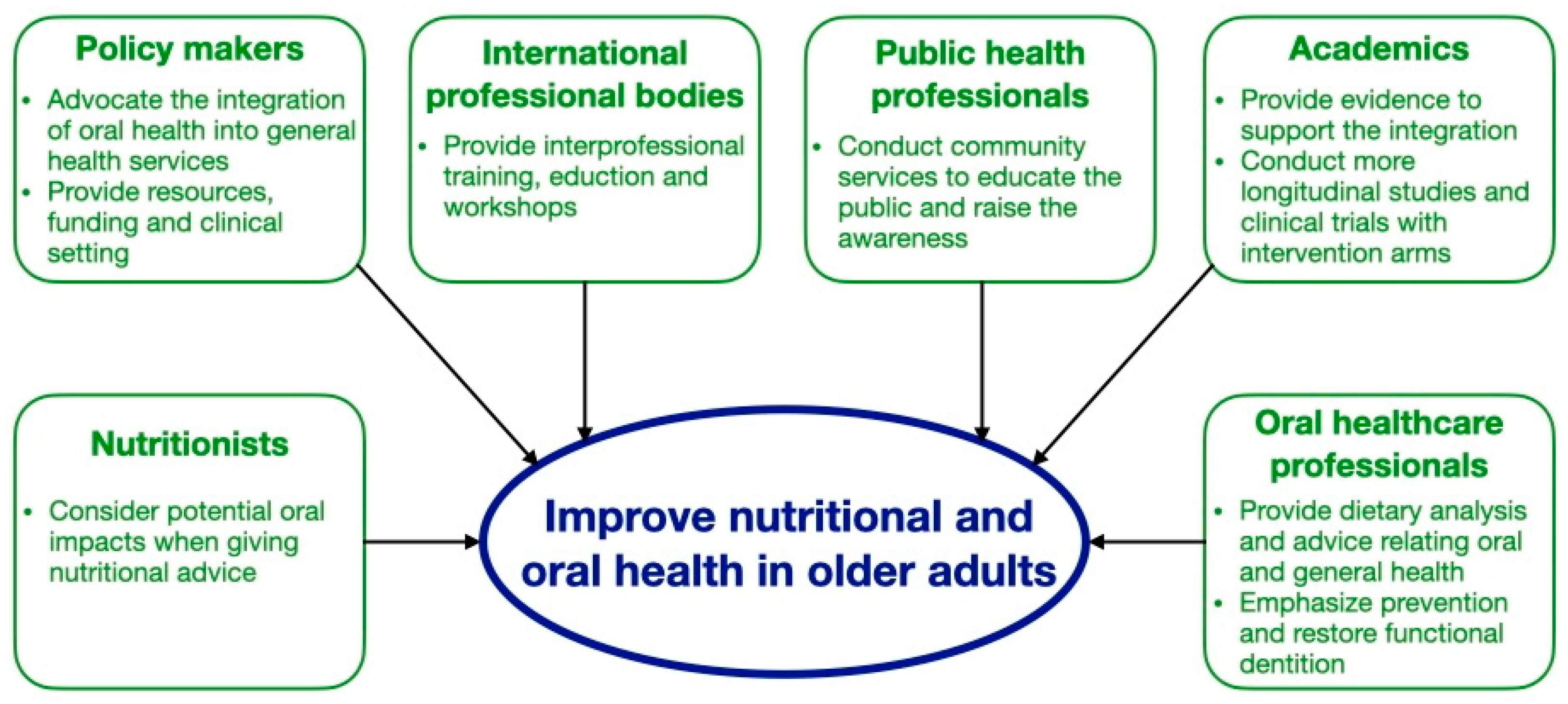
2.1. Dental Caries
2.2. Periodontal Disease
2.3. Tooth Wear
2.4. Oral Cancer
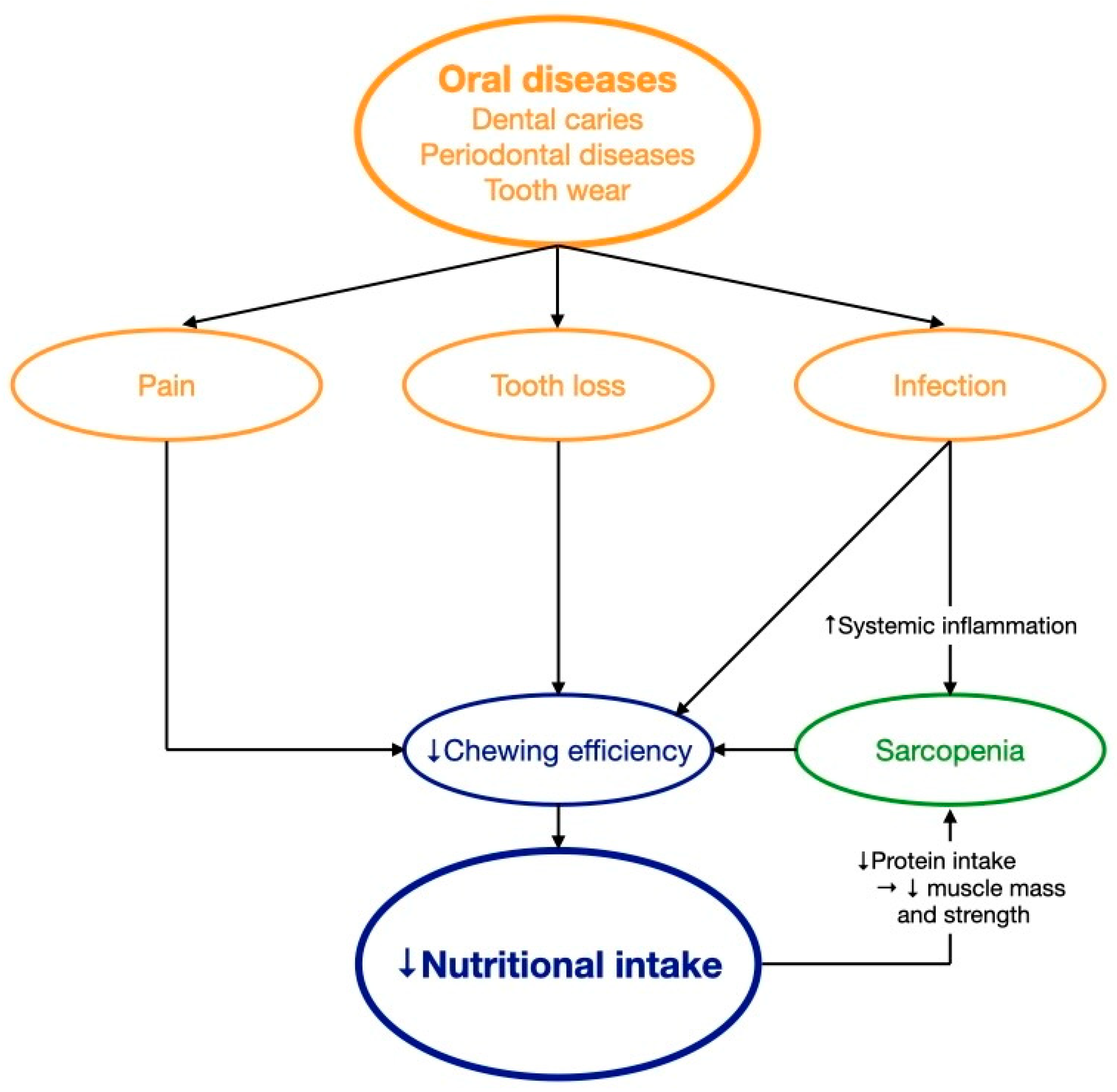
3. The Impact of Oral Health on Diet and Nutrition
3.1. Pain
3.2. Infection
3.3. Tooth Loss
3.4. Hyposalivation
4. Implications for Improving Nutritional and Oral Health in Older Adults
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Keep Fit for Life: Meeting the Nutritional Needs of Older Persons. 2002. Available online: https://apps.who.int/iris/handle/10665/42515 (accessed on 30 May 2023).
- Petersen, P.E.; Kandelman, D.; Arpin, S.; Ogawa, H. Global oral health of older people—Call for public health action. Community Dent. Health 2010, 27 (Suppl. S2), 257–267. [Google Scholar] [PubMed]
- World Report on Ageing and Health. 2015. Available online: https://apps.who.int/iris/handle/10665/186463 (accessed on 30 May 2023).
- Glick, M.; Williams, D.M.; Kleinman, D.V.; Vujicic, M.; Watt, R.G.; Weyant, R.J. A new definition for oral health developed by the FDI World Dental Federation opens the door to a universal definition of oral health. Int. Dent. J. 2016, 66, 322–324. [Google Scholar] [CrossRef] [PubMed]
- Dent, E.; Wright, O.R.L.; Woo, J.; Hoogendijk, E.O. Malnutrition in older adults. Lancet 2023, 401, 951–966. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.K.Y.; Tamrakar, M.; Leung, K.C.M.; Jiang, C.M.; Lo, E.C.M.; Chu, C.H. Oral Health Care of Older Adults in Hong Kong. Geriatrics 2021, 6, 97. [Google Scholar] [CrossRef]
- Peres, M.A.; Macpherson, L.M.; Weyant, R.J.; Daly, B.; Venturelli, R.; Mathur, M.R.; Listl, S.; Celeste, R.K.; Guarnizo-Herreño, C.C.; Kearns, C.; et al. Oral diseases: A global public health challenge. Lancet 2019, 394, 249–260. [Google Scholar] [CrossRef]
- Halpern, L.R. The Geriatric Syndrome and Oral Health: Navigating Oral Disease Treatment Strategies in the Elderly. Dent. Clin. N. Am. 2020, 64, 209–228. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.K.Y.; Tamrakar, M.; Jiang, C.M.; Lo, E.C.M.; Leung, K.C.M.; Chu, C.H. Common Medical and Dental Problems of Older Adults: A Narrative Review. Geriatrics 2021, 6, 76. [Google Scholar] [CrossRef]
- Ogawa, T.; Annear, M.J.; Ikebe, K.; Maeda, Y. Taste-related sensations in old age. J. Oral Rehabil. 2017, 44, 626–635. [Google Scholar] [CrossRef]
- Moynihan, P.J. The relationship between nutrition and systemic and oral well-being in older people. J. Am. Dent. Assoc. 2007, 138, 493–497. [Google Scholar] [CrossRef]
- Nutrition and Oral Health. 2021. Available online: https://www.ada.org/resources/research/science-and-research-institute/oral-health-topics/nutrition-and-oral-health (accessed on 30 May 2023).
- Kiesswetter, E.; Hengeveld, L.M.; Keijser, B.J.; Volkert, D.; Visser, M. Oral health determinants of incident malnutrition in community-dwelling older adults. J. Dent. 2019, 85, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Petersen, P.E. The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century—The approach of the WHO Global Oral Health Programme. Community Dent. Oral Epidemiol. 2003, 31 (Suppl. S1), 3–23. [Google Scholar] [CrossRef] [PubMed]
- de Sire, A.; Ferrillo, M.; Lippi, L.; Agostini, F.; de Sire, R.; Ferrara, P.E.; Raguso, G.; Riso, S.; Roccuzzo, A.; Ronconi, G.; et al. Sarcopenic Dysphagia, Malnutrition, and Oral Frailty in Elderly: A Comprehensive Review. Nutrients 2022, 14, 982. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.K.Y.; Tsang, Y.C.; Jiang, C.M.; Leung, K.C.M.; Lo, E.C.M.; Chu, C.H. Integration of Oral Health into General Health Services for Older Adults. Geriatrics 2023, 8, 20. [Google Scholar] [CrossRef]
- Chapple, I.L.; Bouchard, P.; Cagetti, M.G.; Campus, G.; Carra, M.C.; Cocco, F.; Nibali, L.; Hujoel, P.; Laine, M.L.; Lingström, P.; et al. Interaction of lifestyle, behaviour or systemic diseases with dental caries and periodontal diseases: Consensus report of group 2 of the joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J. Clin. Periodontol. 2017, 44 (Suppl. S18), S39–S51. [Google Scholar] [CrossRef]
- Algra, Y.; Haverkort, E.; Kok, W.; Etten-Jamaludin, F.V.; Schoot, L.V.; Hollaar, V.; Naumann, E.; Schueren, M.D.; Jerković-Ćosić, K. The Association between Malnutrition and Oral Health in Older People: A Systematic Review. Nutrients 2021, 13, 3584. [Google Scholar] [CrossRef] [PubMed]
- Selwitz, R.H.; Ismail, A.I.; Pitts, N.B. Dental caries. Lancet 2007, 369, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.K.Y.; Tamrakar, M.; Jiang, C.M.; Lo, E.C.M.; Leung, K.C.M.; Chu, C.H. A Systematic Review on Caries Status of Older Adults. Int. J. Environ. Res. Public. Health 2021, 18, 10662. [Google Scholar] [CrossRef]
- Sugars and Dental Caries. 2017. Available online: https://www.who.int/news-room/fact-sheets/detail/sugars-and-dental-caries (accessed on 30 May 2023).
- Sheiham, A.; James, W.P. Diet and Dental Caries: The Pivotal Role of Free Sugars Reemphasized. J. Dent. Res. 2015, 94, 1341–1347. [Google Scholar] [CrossRef]
- Moynihan, P.J.; Kelly, S.A. Effect on caries of restricting sugars intake: Systematic review to inform WHO guidelines. J. Dent. Res. 2014, 93, 8–18. [Google Scholar] [CrossRef]
- Guideline: Sugars Intake for Adults and Children. Available online: https://www.who.int/publications/i/item/9789241549028 (accessed on 30 May 2023).
- Sergi, G.; Bano, G.; Pizzato, S.; Veronese, N.; Manzato, E. Taste loss in the elderly: Possible implications for dietary habits. Crit. Rev. Food Sci. Nutr. 2017, 57, 3684–3689. [Google Scholar] [CrossRef]
- Yoshihara, A.; Suwama, K.; Miyamoto, A.; Watanabe, R.; Ogawa, H. Diet and root surface caries in a cohort of older Japanese. Community Dent. Oral Epidemiol. 2021, 49, 301–308. [Google Scholar] [CrossRef] [PubMed]
- van Loveren, C. Sugar Restriction for Caries Prevention: Amount and Frequency. Which Is More Important? Caries Res. 2019, 53, 168–175. [Google Scholar] [CrossRef]
- Wysokiński, A.; Sobów, T.; Kłoszewska, I.; Kostka, T. Mechanisms of the anorexia of aging—A review. Age 2015, 37, 9821. [Google Scholar] [CrossRef] [PubMed]
- Zizza, C.A.; Tayie, F.A.; Lino, M. Benefits of snacking in older Americans. J. Am. Diet. Assoc. 2007, 107, 800–806. [Google Scholar] [CrossRef]
- Cekici, A.; Kantarci, A.; Hasturk, H.; Van Dyke, T.E. Inflammatory and immune pathways in the pathogenesis of periodontal disease. Periodontol. 2000 2014, 64, 57–80. [Google Scholar] [CrossRef] [PubMed]
- Tsang, Y.; Corbet, E.; Jin, L. Subgingival glycine powder air-polishing as an additional approach to nonsurgical periodontal therapy in subjects with untreated chronic periodontitis. J. Periodontal Res. 2018, 53, 440–445. [Google Scholar] [CrossRef]
- Genco, R.J.; Sanz, M. Clinical and public health implications of periodontal and systemic diseases: An overview. Periodontol. 2000 2020, 83, 7–13. [Google Scholar] [CrossRef]
- O’Connor, J.P.; Milledge, K.L.; O’Leary, F.; Cumming, R.; Eberhard, J.; Hirani, V. Poor dietary intake of nutrients and food groups are associated with increased risk of periodontal disease among community-dwelling older adults: A systematic literature review. Nutr. Rev. 2020, 78, 175–188. [Google Scholar] [CrossRef]
- Iwasaki, M.; Taylor, G.W.; Moynihan, P.; Yoshihara, A.; Muramatsu, K.; Watanabe, R.; Miyazaki, H. Dietary ratio of n-6 to n-3 polyunsaturated fatty acids and periodontal disease in community-based older Japanese: A 3-year follow-up study. Prostaglandins Leukot. Essent. Fatty Acids 2011, 85, 107–112. [Google Scholar] [CrossRef]
- Iwasaki, M.; Moynihan, P.; Manz, M.C.; Taylor, G.W.; Yoshihara, A.; Muramatsu, K.; Watanabe, R.; Miyazaki, H. Dietary antioxidants and periodontal disease in community-based older Japanese: A 2-year follow-up study. Public Health Nutr. 2013, 16, 330–338. [Google Scholar] [CrossRef]
- Adegboye, A.R.; Christensen, L.B.; Holm-Pedersen, P.; Avlund, K.; Boucher, B.J.; Heitmann, B.L. Intake of dairy products in relation to periodontitis in older Danish adults. Nutrients 2012, 4, 1219–1229. [Google Scholar] [CrossRef] [PubMed]
- Dental Erosion. 2021. Available online: https://www.ada.org/resources/research/science-and-research-institute/oral-health-topics/dental-erosion (accessed on 30 May 2023).
- Reddy, A.; Norris, D.F.; Momeni, S.S.; Waldo, B.; Ruby, J.D. The pH of beverages in the United States. J. Am. Dent. Assoc. 2016, 147, 255–263. [Google Scholar] [CrossRef]
- Liska, D.; Kelley, M.; Mah, E. 100% Fruit Juice and Dental Health: A Systematic Review of the Literature. Front. Public Health 2019, 7, 190. [Google Scholar] [CrossRef]
- Saads Carvalho, T.; Lussi, A. Chapter 9: Acidic Beverages and Foods Associated with Dental Erosion and Erosive Tooth Wear. Monogr. Oral Sci. 2020, 28, 91–98. [Google Scholar] [PubMed]
- Dominguez, L.J.; Veronese, N.; Baiamonte, E.; Guarrera, M.; Parisi, A.; Ruffolo, C.; Tagliaferri, F.; Barbagallo, M. Healthy Aging and Dietary Patterns. Nutrients 2022, 14, 889. [Google Scholar] [CrossRef] [PubMed]
- Siddarth, P.; Li, Z.; Miller, K.J.; Ercoli, L.M.; Merril, D.A.; Henning, S.M.; Heber, D.; Small, G.W. Randomized placebo-controlled study of the memory effects of pomegranate juice in middle-aged and older adults. Am. J. Clin. Nutr. 2020, 111, 170–177. [Google Scholar] [CrossRef]
- Chai, S.C.; Davis, K.; Zhang, Z.; Zha, L.; Kirschner, K.F. Effects of Tart Cherry Juice on Biomarkers of Inflammation and Oxidative Stress in Older Adults. Nutrients 2019, 11, 228. [Google Scholar] [CrossRef]
- Pontefract, H.A. Erosive toothwear in the elderly population. Gerodontology 2002, 19, 5–16. [Google Scholar] [CrossRef]
- O’Toole, S.; Bernabé, E.; Moazzez, R.; Bartlett, D. Timing of dietary acid intake and erosive tooth wear: A case-control study. J. Dent. 2017, 56, 99–104. [Google Scholar] [CrossRef]
- Li, H.; Zou, Y.; Ding, G. Dietary factors associated with dental erosion: A meta-analysis. PLoS ONE 2012, 7, e42626. [Google Scholar] [CrossRef]
- Oral Health. 2023. Available online: https://www.who.int/news-room/fact-sheets/detail/oral-health (accessed on 30 May 2023).
- Diet, Nutrition, Physical Activity and Cancers of the Mouth, Pharynx and Larynx. 2018. Available online: https://www.wcrf.org/wp-content/uploads/2021/02/mouth-pharynx-larynx-cancer-report.pdf (accessed on 30 May 2023).
- Hashibe, M.; Brennan, P.; Benhamou, S.; Castellsague, X.; Chen, C.; Curado, M.P.; Maso, L.D.; Daudt, A.W.; Fabianova, E.; Wünsch-Filho, V.; et al. Alcohol drinking in never users of tobacco, cigarette smoking in never drinkers, and the risk of head and neck cancer: Pooled analysis in the International Head and Neck Cancer Epidemiology Consortium. J. Natl. Cancer Inst. 2007, 99, 777–789. [Google Scholar] [CrossRef] [PubMed]
- Budtz-Jørgensen, E.; Chung, J.P.; Mojon, P. Successful aging—The case for prosthetic therapy. J. Public Health Dent. 2000, 60, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Salmi, A.; Komulainen, K.; Nihtilä, A.; Tiihonen, M.; Nykänen, I.; Hartikainen, S.; Suominen, A.L. Eating problems among old home care clients. Clin. Exp. Dent. Res. 2022, 8, 959–968. [Google Scholar] [CrossRef] [PubMed]
- Altenhoevel, A.; Norman, K.; Smoliner, C.; Peroz, I. The impact of self-perceived masticatory function on nutrition and gastrointestinal complaints in the elderly. J. Nutr. Health Aging 2012, 16, 175–178. [Google Scholar] [CrossRef]
- Cederholm, T.; Jensen, G.L.; Correia, M.I.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; Baptista, G.; Barazzoni, R.; Blaauw, R.; Coats, A.J.; et al. GLIM criteria for the diagnosis of malnutrition—A consensus report from the global clinical nutrition community. Clin. Nutr. 2019, 38, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Landi, F.; Calvani, R.; Tosato, M.; Martone, A.M.; Ortolani, E.; Savera, G.; Sisto, A.; Marzetti, E. Anorexia of Aging: Risk Factors, Consequences, and Potential Treatments. Nutrients 2016, 8, 69. [Google Scholar] [CrossRef]
- Azzolino, D.; Passarelli, P.C.; De Angelis, P.; Piccirillo, G.B.; D’Addona, A.; Cesari, M. Poor Oral Health as a Determinant of Malnutrition and Sarcopenia. Nutrients 2019, 11, 2898. [Google Scholar] [CrossRef]
- Yan, G.L.K.; Tan, M.N.; Wong, M.L.; Tay, C.M.; Allen, P.F. Functional Dentition, Chronic Periodontal Disease and Frailty in Older Adults—A Narrative Review. Int. J. Environ. Res. Public Health 2022, 20, 502. [Google Scholar] [CrossRef]
- WHO Expert Committee. Recent Advances in Oral Health. Report of a WHO Expert Committee. World Health Organ. Tech. Rep. Ser. 1992, 826, 1–37. [Google Scholar]
- Gotfredsen, K.; Walls, A.W. What dentition assures oral function? Clin. Oral Implants Res. 2007, 18 (Suppl. S3), 34–45. [Google Scholar] [CrossRef]
- Kassebaum, N.J.; Bernabé, E.; Dahiya, M.; Bhandari, B.; Murray, C.J.; Marcenes, W. Global Burden of Severe Tooth Loss: A Systematic Review and Meta-analysis. J. Dent. Res. 2014, 93 (Suppl. S7), 20S–28S. [Google Scholar] [CrossRef] [PubMed]
- Fleming, E.; Afful, J.; Griffin, S.O. Prevalence of Tooth Loss among Older Adults: United States, 2015–2018; NCHS Data Brief No. 368; National Center for Health Statistics: Hyattsville, MD, USA, 2020; pp. 1–8. [Google Scholar]
- Friedman, P.K.; Kaufman, L.B.; Karpas, S.L. Oral health disparity in older adults: Dental decay and tooth loss. Dent. Clin. N. Am. 2014, 58, 757–770. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.A.; Brennan, D.S. Chewing disability in older adults attributable to tooth loss and other oral conditions. Gerodontology 2012, 29, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Mishellany, A.; Woda, A.; Labas, R.; Peyron, M.A. The challenge of mastication: Preparing a bolus suitable for deglutition. Dysphagia 2006, 21, 87–94. [Google Scholar] [CrossRef]
- Zelig, R.; Goldstein, S.; Touger-Decker, R.; Firestone, E.; Golden, A.; Johnson, Z.; Kaseta, A.; Sackey, J.; Tomesko, J.; Parrott, J.S. Tooth Loss and Nutritional Status in Older Adults: A Systematic Review and Meta-analysis. JDR Clin. Trans. Res. 2022, 7, 4–15. [Google Scholar] [CrossRef]
- Pina, G.M.S.; Mota Carvalho, R.; Silva, B.S.F.; Almeida, F.T. Prevalence of hyposalivation in older people: A systematic review and meta-analysis. Gerodontology 2020, 37, 317–331. [Google Scholar] [CrossRef]
- Iwasaki, M.; Yoshihara, A.; Ito, K.; Sato, M.; Minagawa, K.; Muramatsu, K.; Watanabe, R.; Manz, M.C.; Ansai, T.; Miyazaki, H. Hyposalivation and dietary nutrient intake among community-based older Japanese. Geriatr. Gerontol. Int. 2016, 16, 500–507. [Google Scholar] [CrossRef]
- Norman, K.; Haß, U.; Pirlich, M. Malnutrition in Older Adults-Recent Advances and Remaining Challenges. Nutrients 2021, 13, 2764. [Google Scholar] [CrossRef]
- McKenna, G.; Allen, P.F.; Flynn, A.; O’Mahony, D.; DaMata, C.; Cronin, M.; Woods, N. Impact of tooth replacement strategies on the nutritional status of partially-dentate elders. Gerodontology 2012, 29, e883–e890. [Google Scholar] [CrossRef]
- Integrated Care for Older People. 2018. Available online: https://www.who.int/publications/i/item/WHO-HIS-SDS-2018.44 (accessed on 30 May 2023).
- Harnagea, H.; Couturier, Y.; Shrivastava, R.; Girard, F.; Lamothe, L.; Bedos, C.P.; Emami, E. Barriers and facilitators in the integration of oral health into primary care: A scoping review. BMJ Open 2017, 7, e016078. [Google Scholar] [CrossRef]
- Moynihan, P. Foods and dietary factors that prevent dental caries. Quintessence Int. 2007, 38, 320–324. [Google Scholar] [PubMed]
- Chan, A.K.Y.; Tamrakar, M.; Jiang, C.M.; Tsang, Y.C.; Leung, K.C.M.; Chu, C.H. Clinical evidence for professionally applied fluoride therapy to prevent and arrest dental caries in older adults: A systematic review. J. Dent. 2022, 125, 104273. [Google Scholar] [CrossRef] [PubMed]
- McGowan, L.; McCrum, L.A.; Watson, S.; Cardwell, C.; McGuinness, B.; Rutherford, H.; Paice, V.; Moore, C.; Brocklehurst, P.R.; Woodside, J.V.; et al. The impact of oral rehabilitation coupled with healthy dietary advice on the nutritional status of adults: A systematic review and meta-analysis. Crit. Rev. Food Sci. Nutr. 2020, 60, 2127–2147. [Google Scholar] [CrossRef] [PubMed]
| Study Type (Authors, Year) | Title | Main Findings |
|---|---|---|
| Dental caries | ||
| Systematic review (Chan et al., 2021) [20] | “A systematic review on caries status of older adults” | Diet was a risk factor for caries in older adults. |
| Cross-sectional study (Yoshihara et al., 2021) [26] | “Diet and root surface caries in a cohort of older Japanese” | High intake of sucrose in coffee or tea and low milk intake were associated with the increment of root surface caries. |
| Periodontal diseases | ||
| Systematic review (O’Connor et al., 2020) [33] | “Poor dietary intake of nutrients and food groups are associated with increased risk of periodontal disease among community-dwelling older adults: a systematic literature review” | High intakes of fatty acids, vitamin C, vitamin E, beta-carotene, fiber, calcium, dairy, fruits, and vegetables were inversely associated with the risk of periodontal disease. |
| Longitudinal study (Iwasaki et al., 2011) [34] | “Dietary ratio of n-6 to n-3 polyunsaturated fatty acids and periodontal disease in community- based older Japanese: a 3-year follow-up study” | High dietary n-6 to n-3 polyunsaturated fatty acids ratio was associated with greater number of periodontal disease events. |
| Longitudinal study (Iwasaki et al., 2013) [35] | “Dietary antioxidants and periodontal disease in community-based older Japanese: a 2-year follow-up study” | A high intake of antioxidants (vitamin C, vitamin E, α-carotene, and β-carotene) was inversely associated with periodontal disease progression. |
| Cross-sectional study (Adegboye et al., 2012) [36] | “Intake of dairy products in relation to periodontitis in older Danish adults” | Total dairy foods, milk, and fermented food intakes were associated with reduced risk of periodontitis. |
| Tooth wear | ||
| Systematic review # (Liska et al., 2019) [39] | “100% fruit juice and dental health: a systematic review of the literature” | Intake of 100% fruit juice could contribute to tooth erosion in adults. |
| Case-control study # (O’Toole et al., 2017) [45] | “Timing of dietary acid intake and erosive tooth wear: A case-control study” | Acid consumption between meals increased risk of erosive tooth wear in adults (odds ratio: 11.84). |
| Systematic review # (Li et al., 2012) [46] | “Dietary factors associated with dental erosion: a meta-analysis” | Intake of soft drinks (odds ratio: 2.41) and vitamin C (odds ratio: 1.16) was associated with dental erosion in adults. |
| Oral cancer | ||
| Systematic review # (Hashibe et al., 2007) [49] | “Alcohol drinking in never users of tobacco, cigarette smoking in never drinkers, and the risk of head and neck cancer: pooled analysis in the International Head and Neck Cancer Epidemiology Consortium” | Alcohol consumption of more than two drinks daily increased risk of head and neck cancer (odds ratio: 2) |
| Study Type (Authors, Year) | Title | Main Findings |
|---|---|---|
| Poor oral health | ||
| Systematic review (Algra et al., 2021) [18] | “The association between malnutrition and oral health in older people: A systematic review” | In older adults, malnutrition was associated with self-perceived poor oral health, hard tissue problems such as few functional teeth, and soft tissue problems such as cracked lips. |
| Pain on chewing | ||
| Longitudinal study (Kiesswetter et al., 2019) [13] | “Oral health determinants of incident malnutrition in community-dwelling older adults” | Toothache while chewing increased risk of malnutrition of older adults (odds ratio: 2.14). |
| Cross-sectional study (Salmi et al., 2022) [51] | “Eating problems among old home care clients” | Edentulous older adults (odds ratio: 3.5) and older adults with toothache or denture problems (odds ratio: 10.3) had a higher risk for oral health-related eating problems. |
| Cross-sectional study (Altenhoevel et al., 2012) [52] | “The impact of self-perceived masticatory function on nutrition and gastrointestinal complaints in the elderly” | Denture retention affected nutritional status. Chewing problems, denture discomfort, or ill-fitting dentures increased incidence of food avoidance and digestive complaints of older adults. |
| Tooth loss | ||
| Cross-sectional study (Singh et al., 2012) [62] | “Chewing disability in older adults attributable to tooth loss and other oral conditions” | In older adults, chewing ability was associated with loss of functional teeth (odds ratio: 4.2), dental pain (odds ratio: 4.88), and hypermobile teeth (odds ratio: 4.7). |
| Systematic review (Zelig et al., 2022) [64] | “Tooth loss and nutritional status in older adults: A systematic review and meta-analysis” | Malnutrition was associated with loss of functional teeth (odds ratio: 1.21) in older adults. |
| Randomized clinical trial (McKenna et al., 2012) [68] | “Impact of tooth replacement strategies on the nutritional status of partially-dentate elders” | Prosthodontic rehabilitation improved nutritional status of older adults. |
| Hyposalivation | ||
| Cross-sectional study (Iwasaki et al., 2016) [66] | “Hyposalivation and dietary nutrient intake among community-based older Japanese” | Low intake of n-3 polyunsaturated fatty acid, potassium, vitamin D, vitamin E, vitamin B6, and folate increased risk of hyposalivation of older Japanese. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chan, A.K.Y.; Tsang, Y.C.; Jiang, C.M.; Leung, K.C.M.; Lo, E.C.M.; Chu, C.H. Diet, Nutrition, and Oral Health in Older Adults: A Review of the Literature. Dent. J. 2023, 11, 222. https://doi.org/10.3390/dj11090222
Chan AKY, Tsang YC, Jiang CM, Leung KCM, Lo ECM, Chu CH. Diet, Nutrition, and Oral Health in Older Adults: A Review of the Literature. Dentistry Journal. 2023; 11(9):222. https://doi.org/10.3390/dj11090222
Chicago/Turabian StyleChan, Alice Kit Ying, Yiu Cheung Tsang, Chloe Meng Jiang, Katherine Chiu Man Leung, Edward Chin Man Lo, and Chun Hung Chu. 2023. "Diet, Nutrition, and Oral Health in Older Adults: A Review of the Literature" Dentistry Journal 11, no. 9: 222. https://doi.org/10.3390/dj11090222
APA StyleChan, A. K. Y., Tsang, Y. C., Jiang, C. M., Leung, K. C. M., Lo, E. C. M., & Chu, C. H. (2023). Diet, Nutrition, and Oral Health in Older Adults: A Review of the Literature. Dentistry Journal, 11(9), 222. https://doi.org/10.3390/dj11090222