Predictability of Invisalign® Clear Aligners Using OrthoPulse®: A Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mester, A.; Mester, A. The History of Photobiomodulation: Endre Mester (1903–1984). Photomed. Laser Surg. 2017, 35, 393–394. [Google Scholar] [CrossRef]
- Posten, W.; Wrone, D.A.; Dover, J.S.; Arndt, K.A.; Silapunt, S.; Alam, M. Low-level laser therapy for wound healing: Mechanism and efficacy. Derm. Surg. 2005, 31, 334–340. [Google Scholar] [CrossRef]
- Kim, W.S.; Calderhead, R.G. Is light-emitting diode phototherapy (LED-LLLT) really effective? Laser 2011, 20, 205–215. [Google Scholar] [CrossRef]
- Chung, H.; Dai, T.; Sharma, S.K.; Huang, Y.Y.; Carroll, J.D.; Hamblin, M.R. The nuts and bolts of low-level laser (light) therapy. Ann. Biomed. Eng. 2012, 40, 516–533. [Google Scholar] [CrossRef] [PubMed]
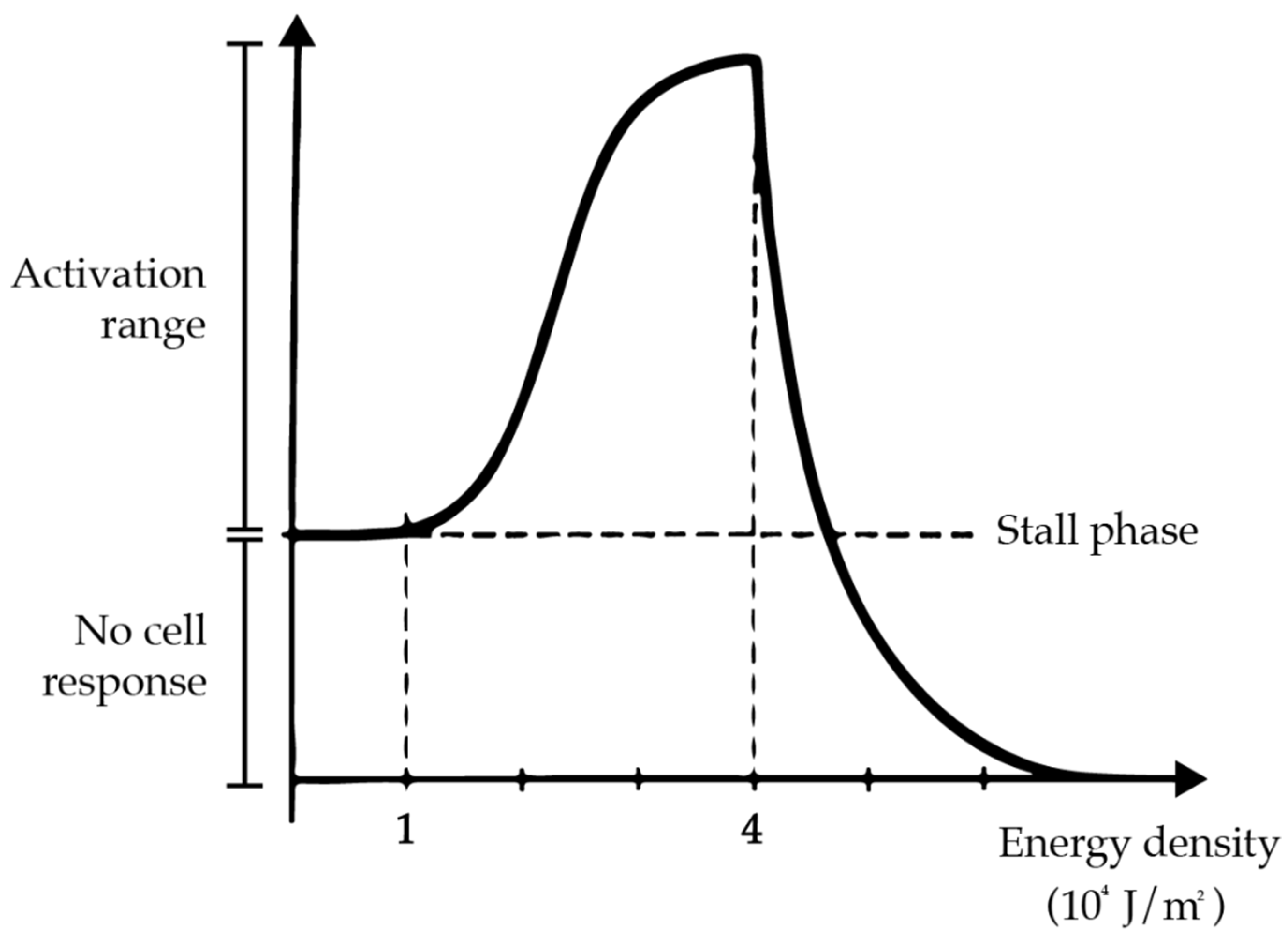
- Sommer, A.P.; Pinheiro, A.L.; Mester, A.R.; Franke, R.P.; Whelan, H.T. Biostimulatory windows in low-intensity laser activation: Lasers, scanners, and NASA’s light-emitting diode array system. J. Clin. Laser Med. Surg. 2001, 19, 29–33. [Google Scholar] [CrossRef] [PubMed]
- AlShahrani, I.; Togoo, R.A.; Hosmani, J.; Alhaizaey, A. Photobiomodulation in acceleration of orthodontic tooth movement: A systematic review and meta analysis. Complement. Med. 2019, 47, 102220. [Google Scholar] [CrossRef]
- Kamal, A.; Salman, B.; Ar, N.H.; Samsudin, A.R. Management of dry socket with low-level laser therapy. Clin. Oral Investig. 2021, 25, 1029–1033. [Google Scholar] [CrossRef] [PubMed]
- Pandeshwar, P.; Roa, M.D.; Das, R.; Shastry, S.P.; Kaul, R.; Srinivasreddy, M.B. Photobiomodulation in oral medicine: A review. J. Investig. Clin. Dent. 2016, 7, 114–126. [Google Scholar] [CrossRef]
- Jiang, Q.; Li, J.; Mei, L.; Du, J.; Levrini, L.; Abbate, G.M.; Li, H. Periodontal health during orthodontic treatment with clear aligners and fixed appliances: A meta-analysis. J. Am. Dent. Assoc. 2018, 149, 712–720.e12. [Google Scholar] [CrossRef]
- Levrini, L.; Carganico, A.; Abbate, L. Maxillary expansion with clear aligners in the mixed dentition: A preliminary study with Invisalign(R) First system. Eur. J. Paediatr. Dent. 2021, 22, 125–128. [Google Scholar] [CrossRef]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Efficacy of clear aligners in controlling orthodontic tooth movement: A systematic review. Angle Orthod. 2015, 85, 881–889. [Google Scholar] [CrossRef] [PubMed]
- Robertson, L.; Kaur, H.; Fagundes, N.C.F.; Romanyk, D.; Major, P.; Flores Mir, C. Effectiveness of clear aligner therapy for orthodontic treatment: A systematic review. Orthod. Craniofac. Res. 2020, 23, 133–142. [Google Scholar] [CrossRef]
- Kravitz, N.D.; Kusnoto, B.; BeGole, E.; Obrez, A.; Agran, B. How well does Invisalign work? A prospective clinical study evaluating the efficacy of tooth movement with Invisalign. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Houle, J.P.; Piedade, L.; Todescan, R., Jr.; Pinheiro, F.H. The predictability of transverse changes with Invisalign. Angle Orthod. 2017, 87, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Sambevski, J.; Papadopoulou, A.K.; Foley, M.; Dalci, K.; Petocz, P.; Darendeliler, M.A.; Dalci, O. Physical properties of root cementum: Part 29. The effects of LED-mediated photobiomodulation on orthodontically induced root resorption and pain: A pilot split-mouth randomized controlled trial. Eur. J. Orthod. 2022, 44, 650–658. [Google Scholar] [CrossRef] [PubMed]
- Almpani, K.; Kantarci, A. Surgical Methods for the Acceleration of the Orthodontic Tooth Movement. Front. Oral. Biol. 2016, 18, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Kacprzak, A.; Strzecki, A. Methods of accelerating orthodontic tooth movement: A review of contemporary literature. Dent. Med. Probl. 2018, 55, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Baek, W.Y.; Byun, I.H.; Yun, I.S.; Kim, J.Y.; Roh, T.S.; Lew, D.H.; Kim, Y.S. The effect of light-emitting diode (590/830 nm)-based low-level laser therapy on posttraumatic edema of facial bone fracture patients. J. Craniomaxillofac. Surg. 2017, 45, 1875–1877. [Google Scholar] [CrossRef] [PubMed]
- Bjordal, J.M.; Johnson, M.I.; Iversen, V.; Aimbire, F.; Lopes-Martins, R.A. Low-level laser therapy in acute pain: A systematic review of possible mechanisms of action and clinical effects in randomized placebo-controlled trials. Photomed. Laser Surg. 2006, 24, 158–168. [Google Scholar] [CrossRef]
- Christie, A.; Jamtvedt, G.; Dahm, K.T.; Moe, R.H.; Haavardsholm, E.A.; Hagen, K.B. Effectiveness of nonpharmacological and nonsurgical interventions for patients with rheumatoid arthritis: An overview of systematic reviews. Phys. Ther. 2007, 87, 1697–1715. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Li, L.; Lin, Z.; Wang, L.; Lin, L.; Li, M.; Zhang, Y.; Yin, Q.; Li, Q.; Xia, H. A New Treatment Modality for Rheumatoid Arthritis: Combined Photothermal and Photodynamic Therapy Using Cu7.2 S4 Nanoparticles. Adv. Heal. Mater. 2018, 7, e1800013. [Google Scholar] [CrossRef]
- Ordahan, B.; Karahan, A.Y. Role of low-level laser therapy added to facial expression exercises in patients with idiopathic facial (Bell’s) palsy. Lasers Med. Sci. 2017, 32, 931–936. [Google Scholar] [CrossRef]
- Genc, G.; Kocadereli, I.; Tasar, F.; Kilinc, K.; El, S.; Sarkarati, B. Effect of low-level laser therapy (LLLT) on orthodontic tooth movement. Lasers Med. Sci. 2013, 28, 41–47. [Google Scholar] [CrossRef]
- Gkantidis, N.; Mistakidis, I.; Kouskoura, T.; Pandis, N. Effectiveness of non-conventional methods for accelerated orthodontic tooth movement: A systematic review and meta-analysis. J. Dent. 2014, 42, 1300–1319. [Google Scholar] [CrossRef]
- Hamblin, M.; Demidova, T. Mechanisms of Low Level Light Therapy; SPIE: San Jose, CA, USA, 2006; Volume 6140. [Google Scholar]
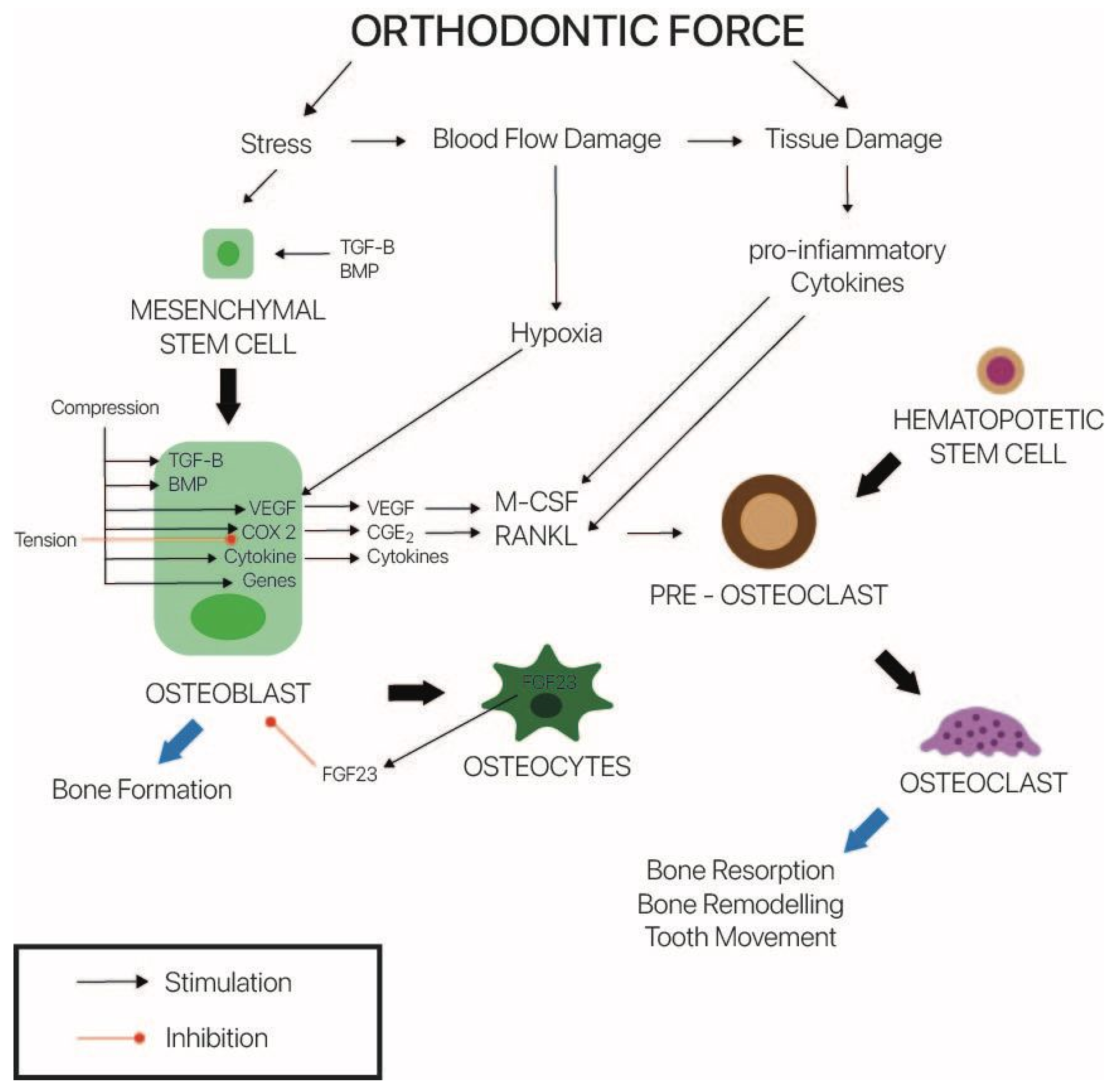
- Nimeri, G.; Kau, C.H.; Abou-Kheir, N.S.; Corona, R. Acceleration of tooth movement during orthodontic treatment--a frontier in orthodontics. Prog. Orthod. 2013, 14, 42. [Google Scholar] [CrossRef]
- Sousa, M.V.; Pinzan, A.; Consolaro, A.; Henriques, J.F.; de Freitas, M.R. Systematic literature review: Influence of low-level laser on orthodontic movement and pain control in humans. Photomed. Laser Surg. 2014, 32, 592–599. [Google Scholar] [CrossRef]
- Vescovi, P.; Meleti, M.; Merigo, E.; Manfredi, M.; Fornaini, C.; Guidotti, R.; Nammour, S. Case series of 589 tooth extractions in patients under bisphosphonates therapy. Proposal of a clinical protocol supported by Nd:YAG low-level laser therapy. Med. Oral Patol. Oral Cir. Bucal. 2013, 18, e680–e685. [Google Scholar] [CrossRef]
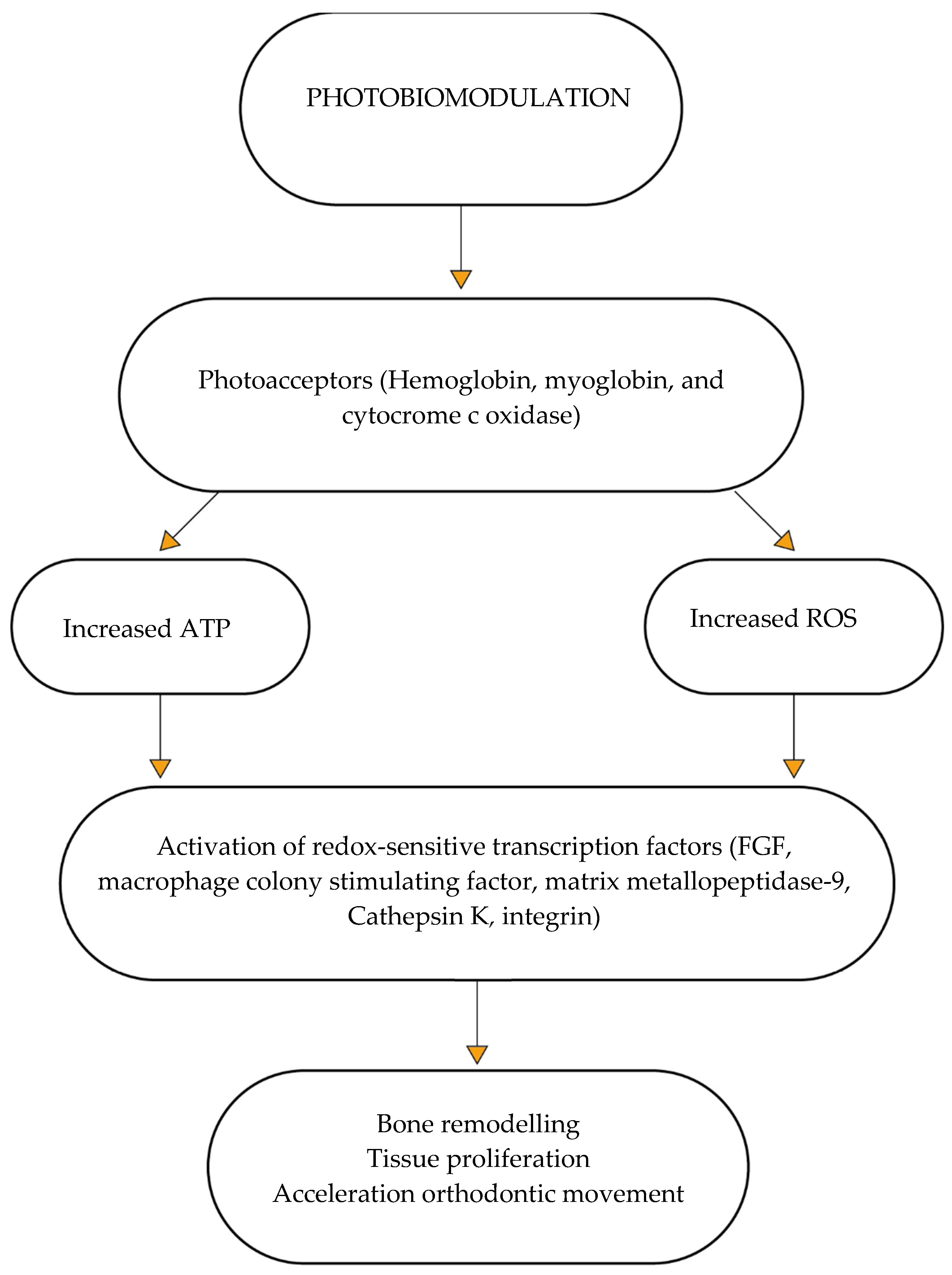
- Na, S.; TruongVo, T.; Jiang, F.; Joll, J.E.; Guo, Y.; Utreja, A.; Chen, J. Dose analysis of photobiomodulation therapy on osteoblast, osteoclast, and osteocyte. J. Biomed. Opt. 2018, 23, 1–8. [Google Scholar] [CrossRef]
- Yamaguchi, M.; Hayashi, M.; Fujita, S.; Yoshida, T.; Utsunomiya, T.; Yamamoto, H.; Kasai, K. Low-energy laser irradiation facilitates the velocity of tooth movement and the expressions of matrix metalloproteinase-9, cathepsin K, and alpha(v) beta(3) integrin in rats. Eur. J. Orthod. 2010, 32, 131–139. [Google Scholar] [CrossRef]
- Cruz, D.R.; Kohara, E.K.; Ribeiro, M.S.; Wetter, N.U. Effects of low-intensity laser therapy on the orthodontic movement velocity of human teeth: A preliminary study. Lasers Surg. Med. 2004, 35, 117–120. [Google Scholar] [CrossRef]
- Ge, M.K.; He, W.L.; Chen, J.; Wen, C.; Yin, X.; Hu, Z.A.; Liu, Z.P.; Zou, S.J. Efficacy of low-level laser therapy for accelerating tooth movement during orthodontic treatment: A systematic review and meta-analysis. Lasers Med. Sci. 2015, 30, 1609–1618. [Google Scholar] [CrossRef]
- Goulart, C.S.; Nouer, P.R.; Mouramartins, L.; Garbin, I.U.; de Fatima Zanirato Lizarelli, R. Photoradiation and orthodontic movement: Experimental study with canines. Photomed. Laser Surg. 2006, 24, 192–196. [Google Scholar] [CrossRef] [PubMed]
- Kau, C.H.; Kantarci, A.; Shaughnessy, T.; Vachiramon, A.; Santiwong, P.; de la Fuente, A.; Skrenes, D.; Ma, D.; Brawn, P. Photobiomodulation accelerates orthodontic alignment in the early phase of treatment. Prog. Orthod. 2013, 14, 30. [Google Scholar] [CrossRef]
- Nimeri, G.; Kau, C.H.; Corona, R.; Shelly, J. The effect of photobiomodulation on root resorption during orthodontic treatment. Clin. Cosmet. Investig. Dent. 2014, 6, 1–8. [Google Scholar] [CrossRef][Green Version]
- Guray, Y.; Yuksel, A.S. Effect of light-emitting photobiomodulation therapy on the rate of orthodontic tooth movement: A randomized controlled clinical trial. J. Orofac. Orthop. 2022. [Google Scholar] [CrossRef]
- Al-Dboush, R.; Esfahani, A.N.; El-Bialy, T. Impact of photobiomodulation and low-intensity pulsed ultrasound adjunctive interventions on orthodontic treatment duration during clear aligner therapy. Angle Orthod. 2021, 91, 619–625. [Google Scholar] [CrossRef]
- Saccomanno, S.; Saran, S.; Lagana, D.; Mastrapasqua, R.F.; Grippaudo, C. Motivation, Perception, and Behavior of the Adult Orthodontic Patient: A Survey Analysis. Biomed. Res. Int. 2022, 2022, 2754051. [Google Scholar] [CrossRef]
- White, D.W.; Julien, K.C.; Jacob, H.; Campbell, P.M.; Buschang, P.H. Discomfort associated with Invisalign and traditional brackets: A randomized, prospective trial. Angle Orthod. 2017, 87, 801–808. [Google Scholar] [CrossRef]
- Levrini, L.; Tieghi, G.; Bini, V. Invisalign ClinCheck and the Aesthetic Digital Smile Design Protocol. J. Clin. Orthod. 2015, 49, 518–524. [Google Scholar]
- Haouili, N.; Kravitz, N.D.; Vaid, N.R.; Ferguson, D.J.; Makki, L. Has Invisalign improved? A prospective follow-up study on the efficacy of tooth movement with Invisalign. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 420–425. [Google Scholar] [CrossRef]
- Simon, M.; Keilig, L.; Schwarze, J.; Jung, B.A.; Bourauel, C. Treatment outcome and efficacy of an aligner technique--regarding incisor torque, premolar derotation and molar distalization. BMC Oral. Health 2014, 14, 68. [Google Scholar] [CrossRef]
- Scribante, A.; Gallo, S.; Bertino, K.; Meles, S.; Gandini, P.; Sfondrini, M.F. The Effect of Chairside Verbal Instructions Matched with Instagram Social Media on Oral Hygiene of Young Orthodontic Patients: A Randomized Clinical Trial. Appl. Sci. 2021, 11, 706. [Google Scholar] [CrossRef]
- Imani, M.M.; Golshah, A.; Safari-Faramani, R.; Sadeghi, M. Effect of Low-level Laser Therapy on Orthodontic Movement of Human Canine: A Systematic Review and Meta-analysis of Randomized Clinical Trials. Acta Inf. Med. 2018, 26, 139–143. [Google Scholar] [CrossRef]
- Torri, S.; Weber, J.B. Influence of low-level laser therapy on the rate of orthodontic movement: A literature review. Photomed. Laser Surg. 2013, 31, 411–421. [Google Scholar] [CrossRef]
- Carroll, J.D.; Milward, M.R.; Cooper, P.R.; Hadis, M.; Palin, W.M. Developments in low level light therapy (LLLT) for dentistry. Dent. Mater. 2014, 30, 465–475. [Google Scholar] [CrossRef]
- Seifi, M.; Shafeei, H.A.; Daneshdoost, S.; Mir, M. Effects of two types of low-level laser wave lengths (850 and 630 nm) on the orthodontic tooth movements in rabbits. Lasers Med. Sci. 2007, 22, 261–264. [Google Scholar] [CrossRef]
- Yang, H.; Liu, J.; Yang, K. Comparative Study of 660 and 830 nm Photobiomodulation in Promoting Orthodontic Tooth Movement. Photobiomodul. Photomed. Laser Surg. 2019, 37, 349–355. [Google Scholar] [CrossRef]
- Al-Shafi, S.; Pandis, N.; Darendeliler, M.A.; Papadopoulou, A.K. Effect of light-emitting diode-mediated photobiomodulation on extraction space closure in adolescents and young adults: A split-mouth, randomized controlled trial. Am. J. Orthod. Dentofac. Orthop. 2021, 160, 19–28. [Google Scholar] [CrossRef] [PubMed]

| Compliance | Planned Aligners | Finishing Aligners | Total Aligners | % Variation | |
|---|---|---|---|---|---|
| Group 1 | 79.75% ± 0.20 | 29.52 ± 12.06 | 19.65 ± 18.00 | 49.17 ± 20.75 | 66.55% |
| Group 2 | N.A. | 26.57 ± 12.32 | 27.48 ± 20.32 | 54.05 ± 26.93 | 103.42% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Levrini, L.; Carganico, A.; Deppieri, A.; Saran, S.; Bocchieri, S.; Zecca, P.A.; Bertini, S.; D’Apote, A.; Segù, M. Predictability of Invisalign® Clear Aligners Using OrthoPulse®: A Retrospective Study. Dent. J. 2022, 10, 229. https://doi.org/10.3390/dj10120229
Levrini L, Carganico A, Deppieri A, Saran S, Bocchieri S, Zecca PA, Bertini S, D’Apote A, Segù M. Predictability of Invisalign® Clear Aligners Using OrthoPulse®: A Retrospective Study. Dentistry Journal. 2022; 10(12):229. https://doi.org/10.3390/dj10120229
Chicago/Turabian StyleLevrini, Luca, Andrea Carganico, Alessandro Deppieri, Stefano Saran, Salvatore Bocchieri, Piero Antonio Zecca, Sara Bertini, Anna D’Apote, and Marzia Segù. 2022. "Predictability of Invisalign® Clear Aligners Using OrthoPulse®: A Retrospective Study" Dentistry Journal 10, no. 12: 229. https://doi.org/10.3390/dj10120229
APA StyleLevrini, L., Carganico, A., Deppieri, A., Saran, S., Bocchieri, S., Zecca, P. A., Bertini, S., D’Apote, A., & Segù, M. (2022). Predictability of Invisalign® Clear Aligners Using OrthoPulse®: A Retrospective Study. Dentistry Journal, 10(12), 229. https://doi.org/10.3390/dj10120229









