Influence of Framework Material and Posterior Implant Angulation in Full-Arch All-on-4 Implant-Supported Prosthesis Stress Concentration
Abstract
:1. Introduction
2. Materials and Methods
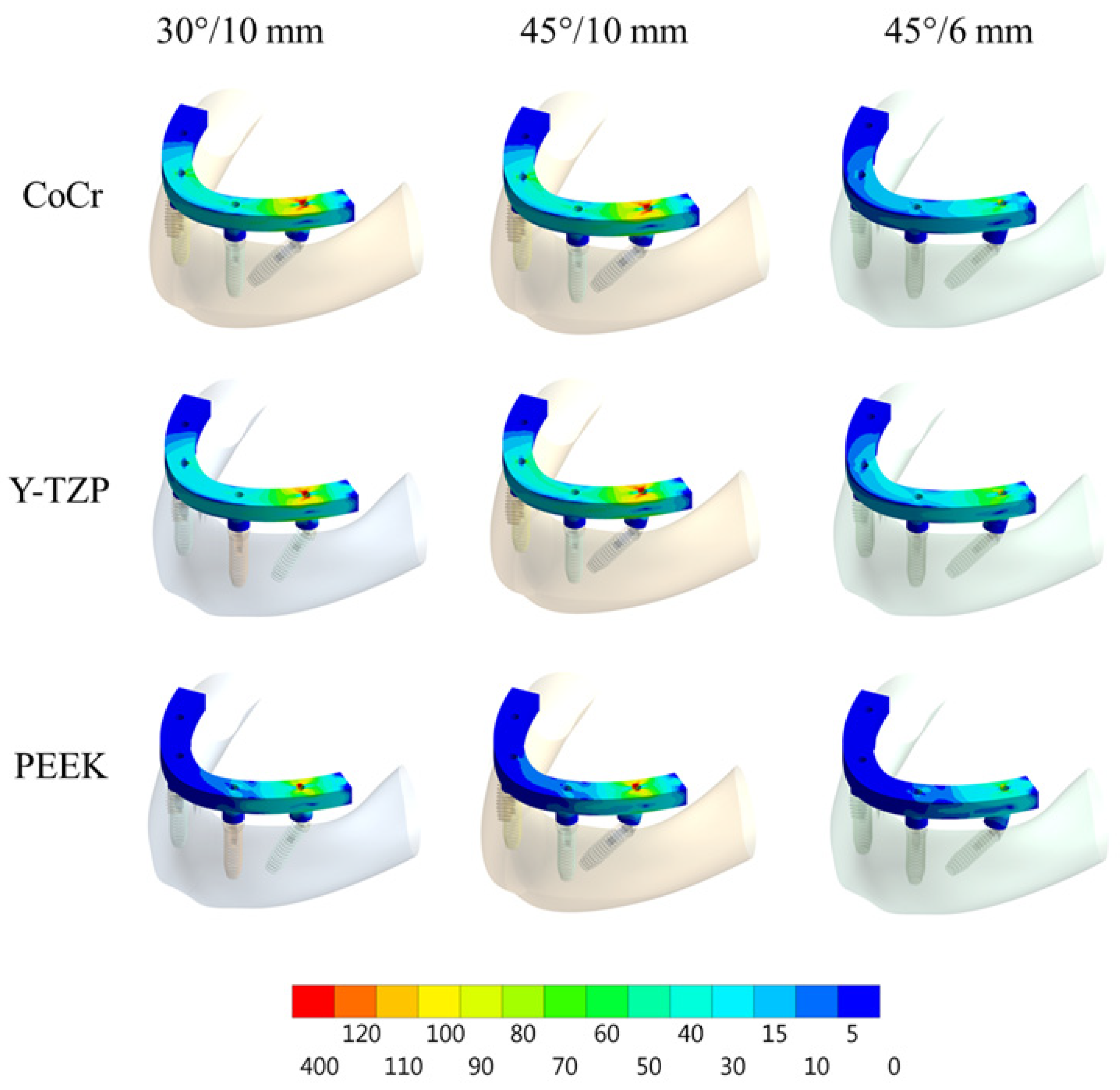
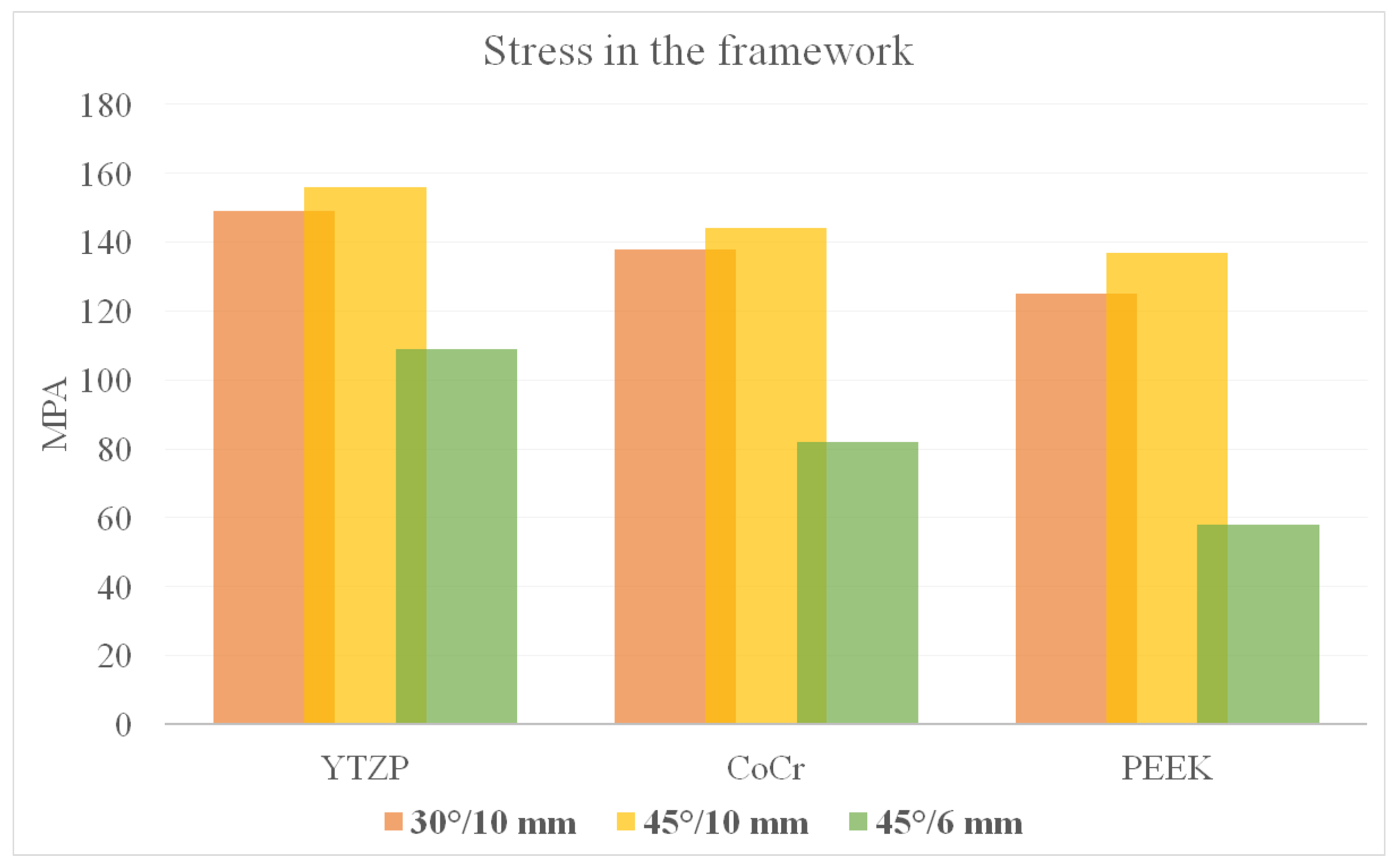
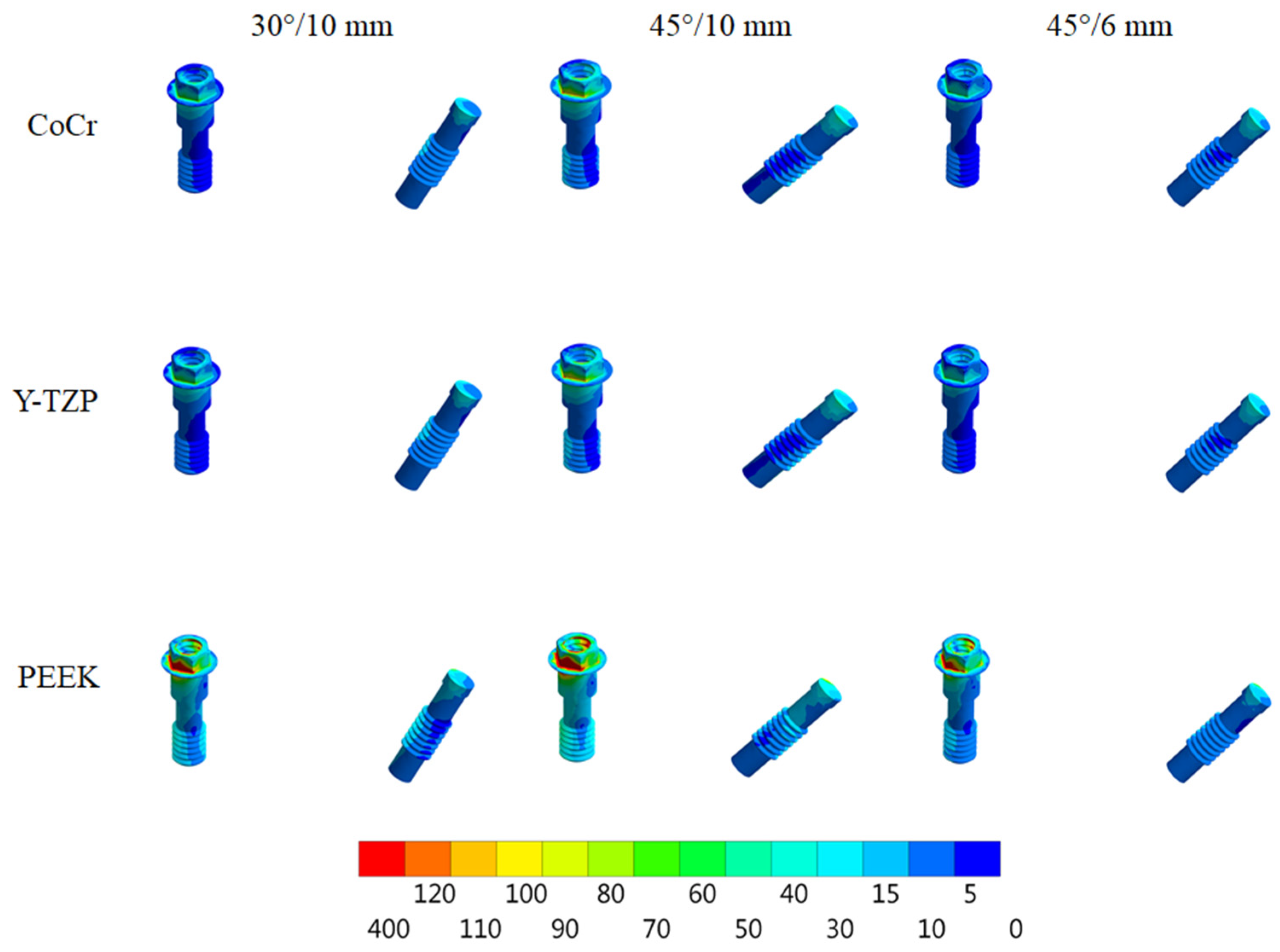
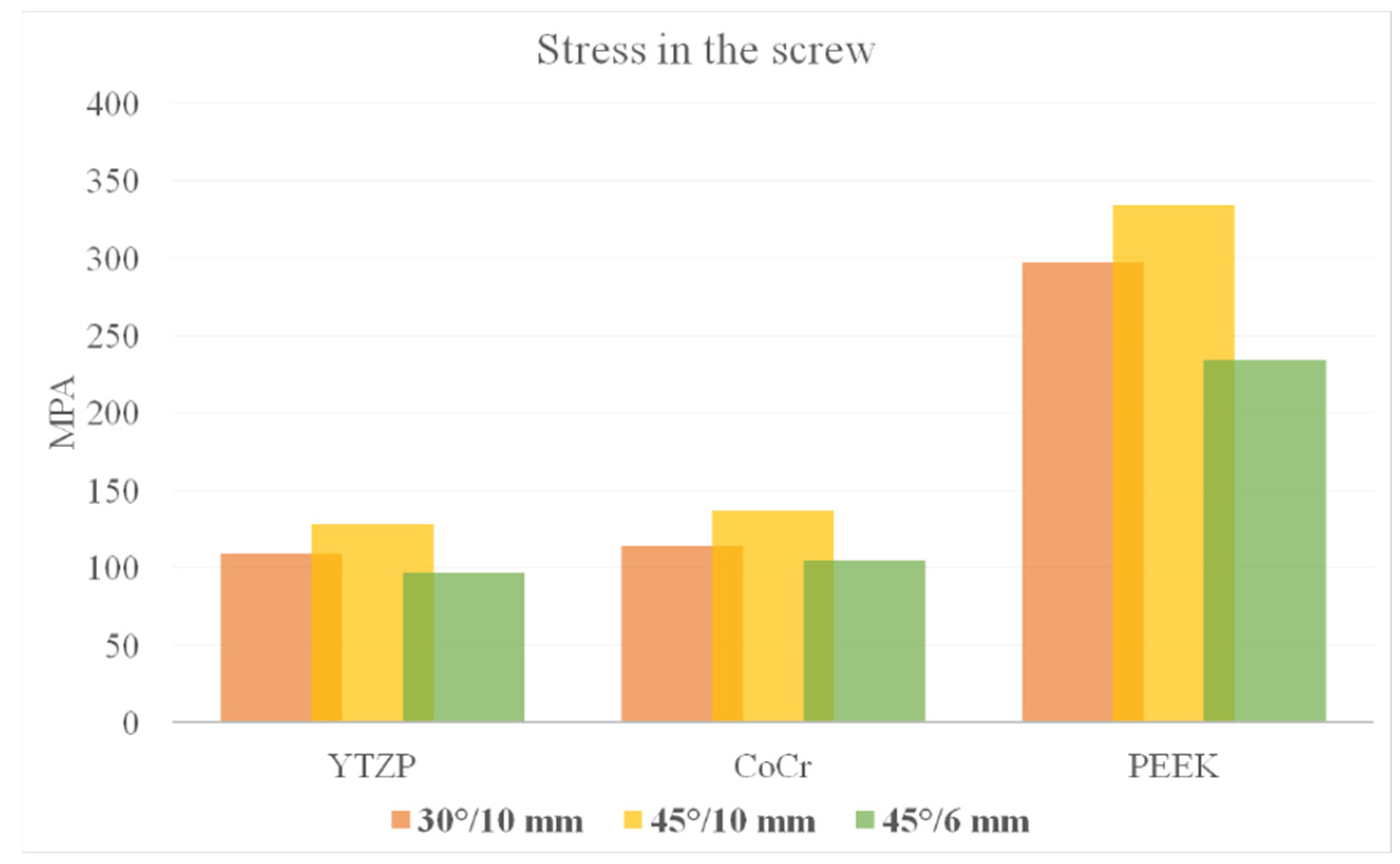
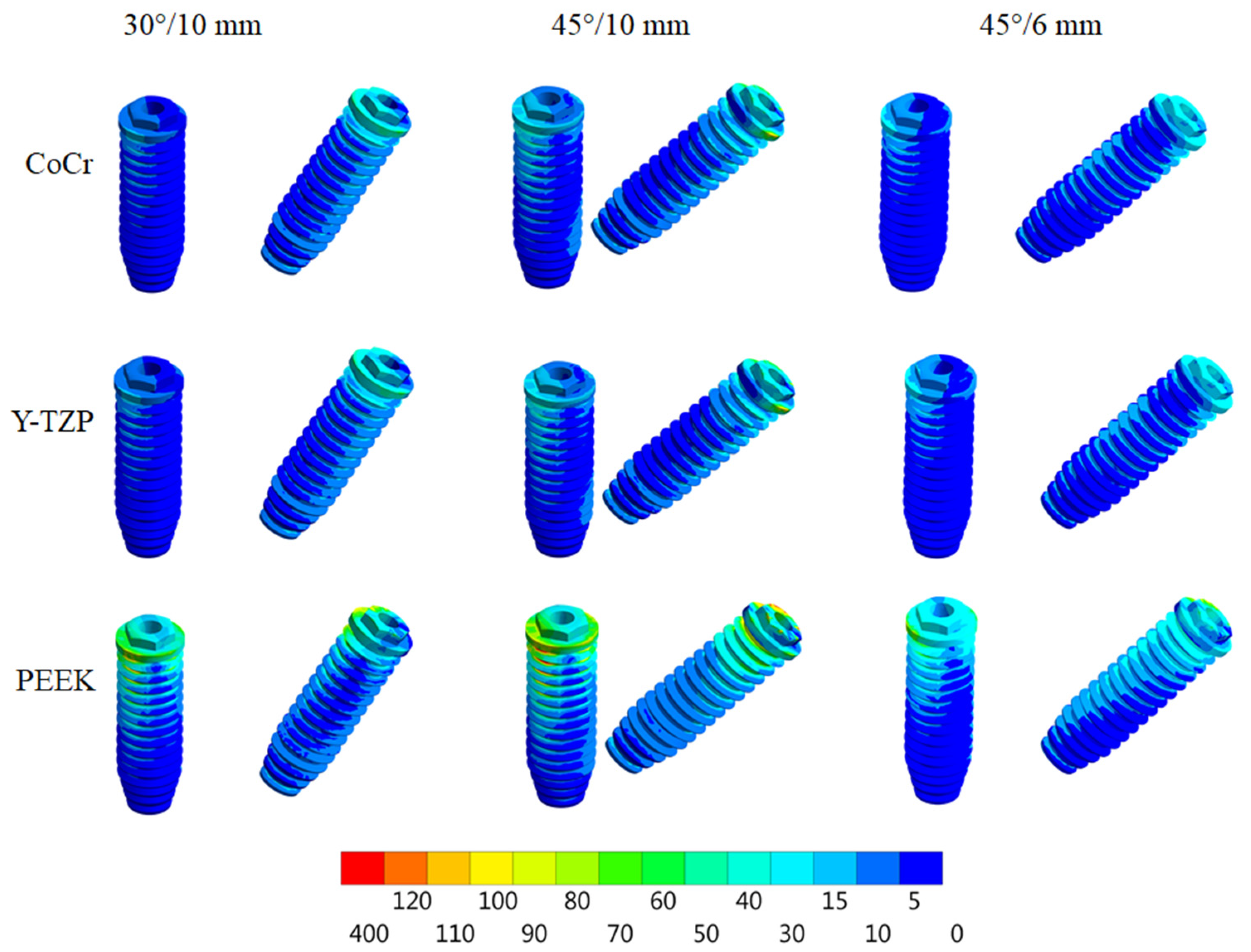
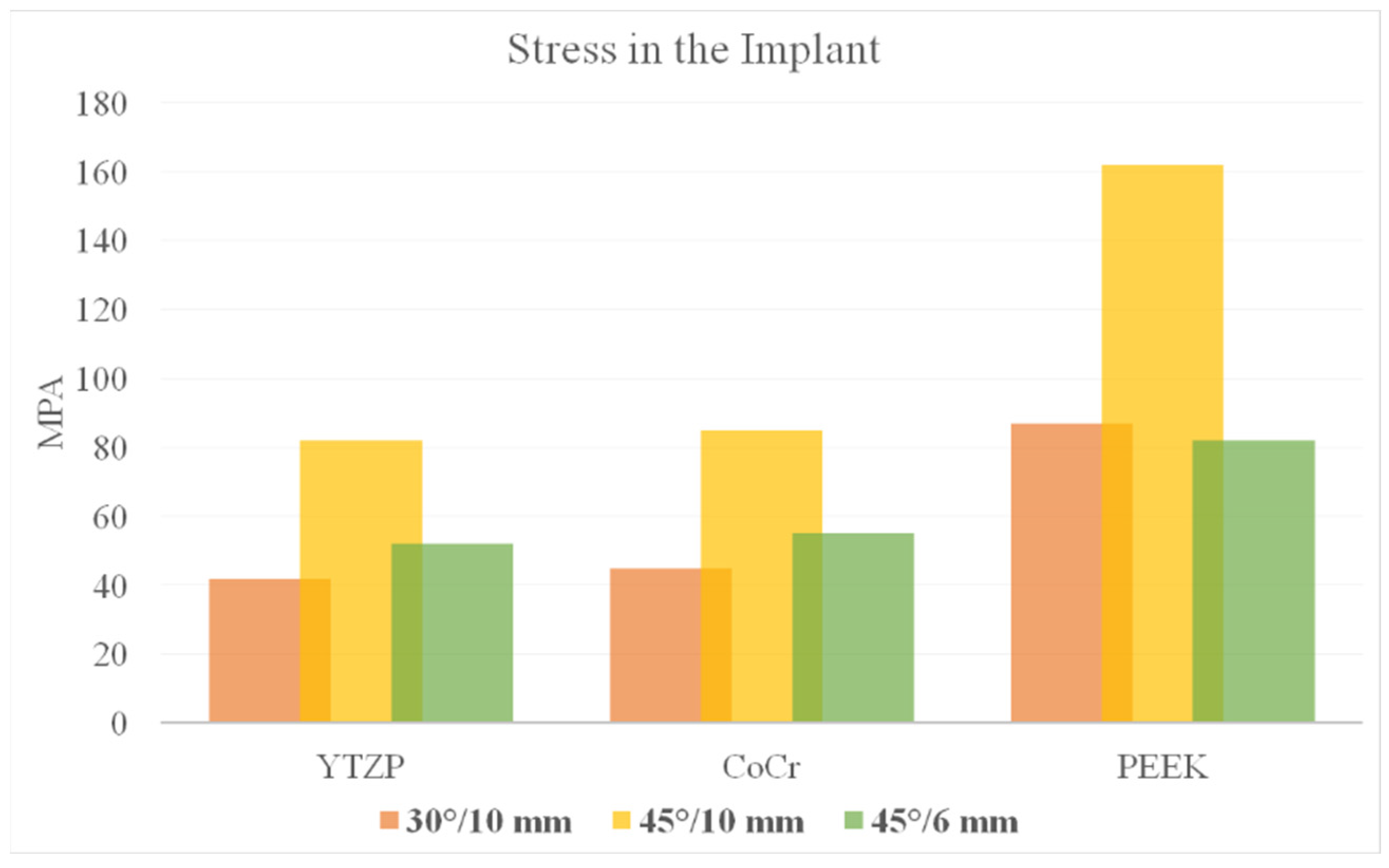
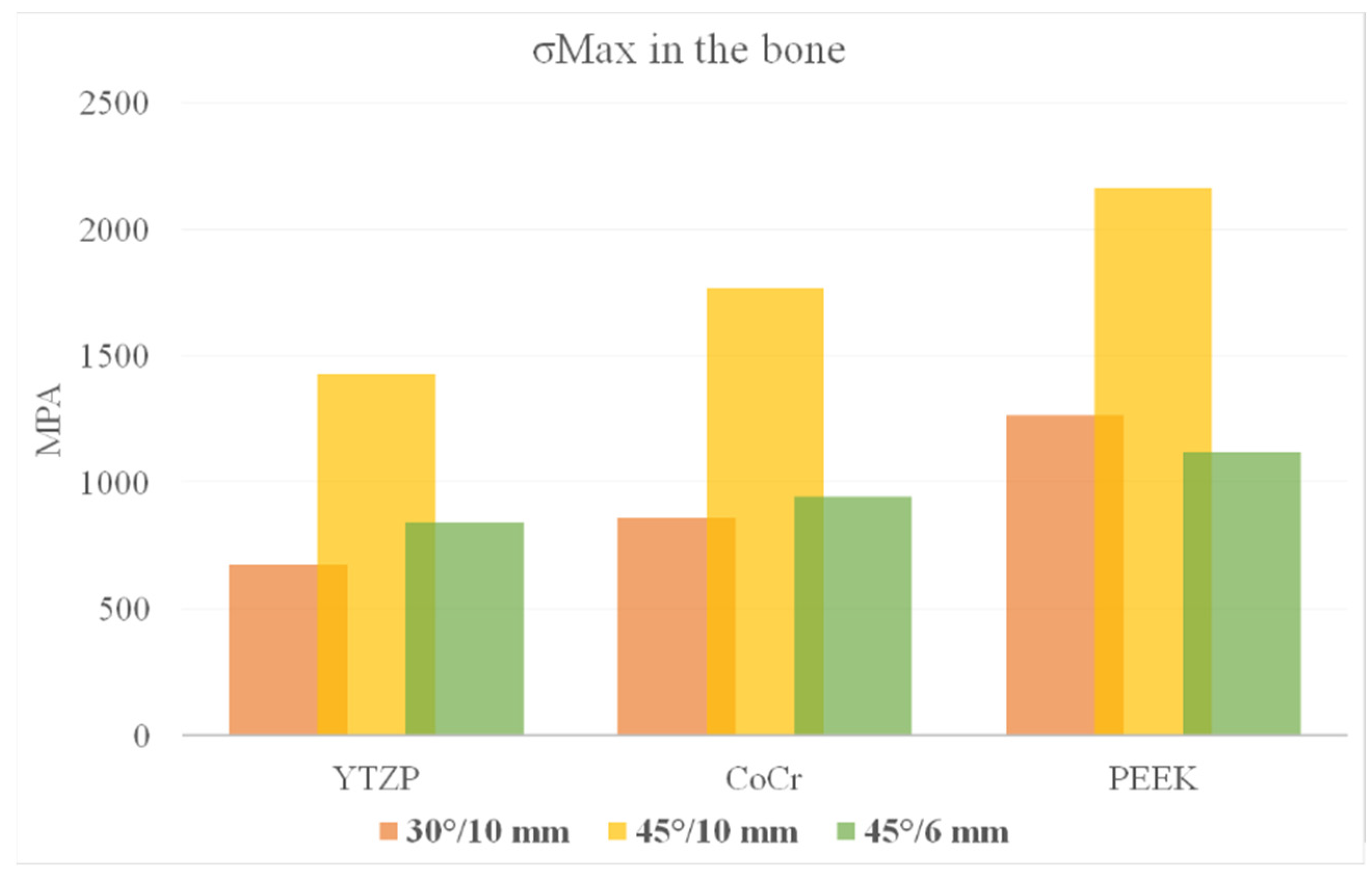
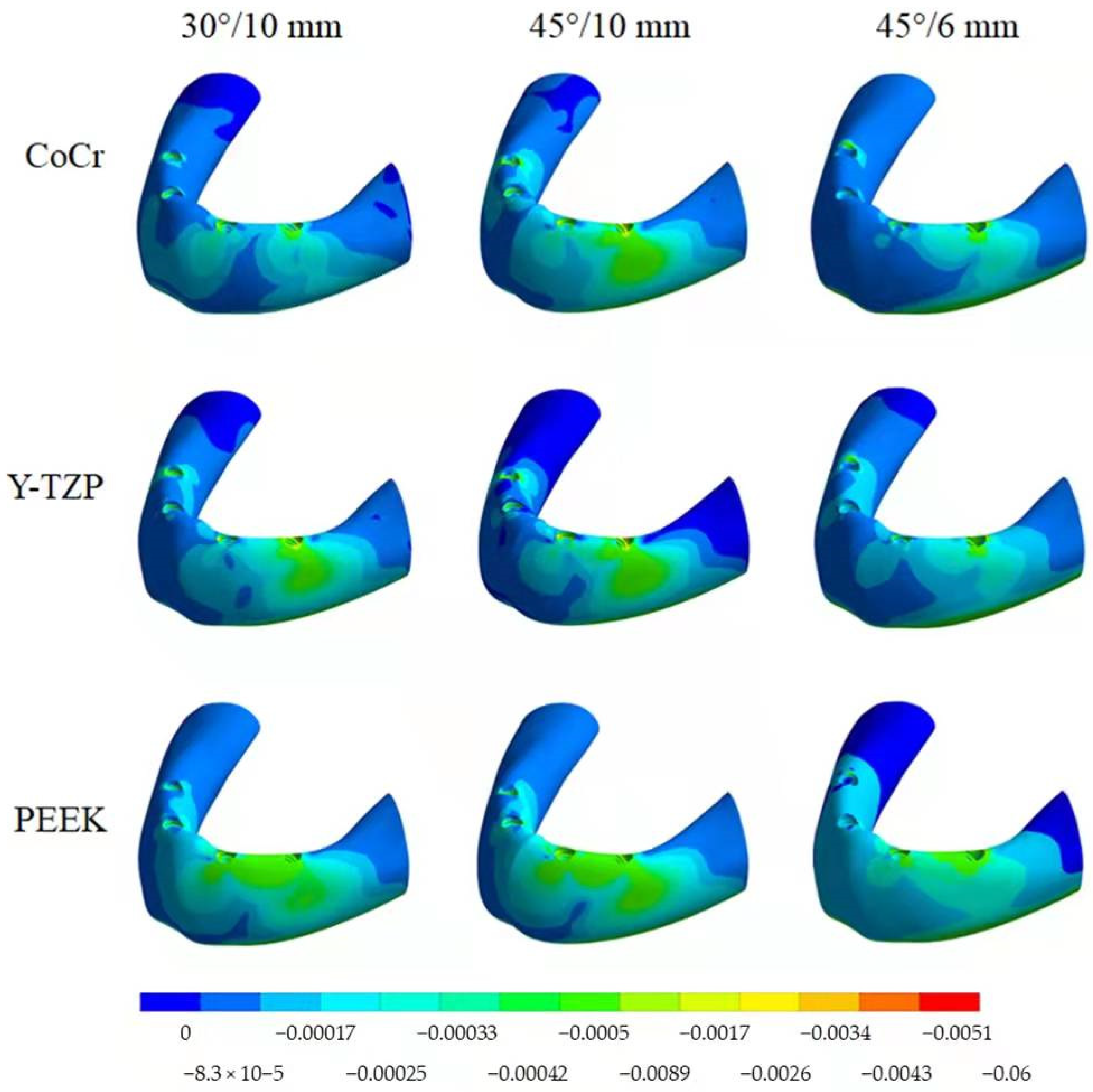
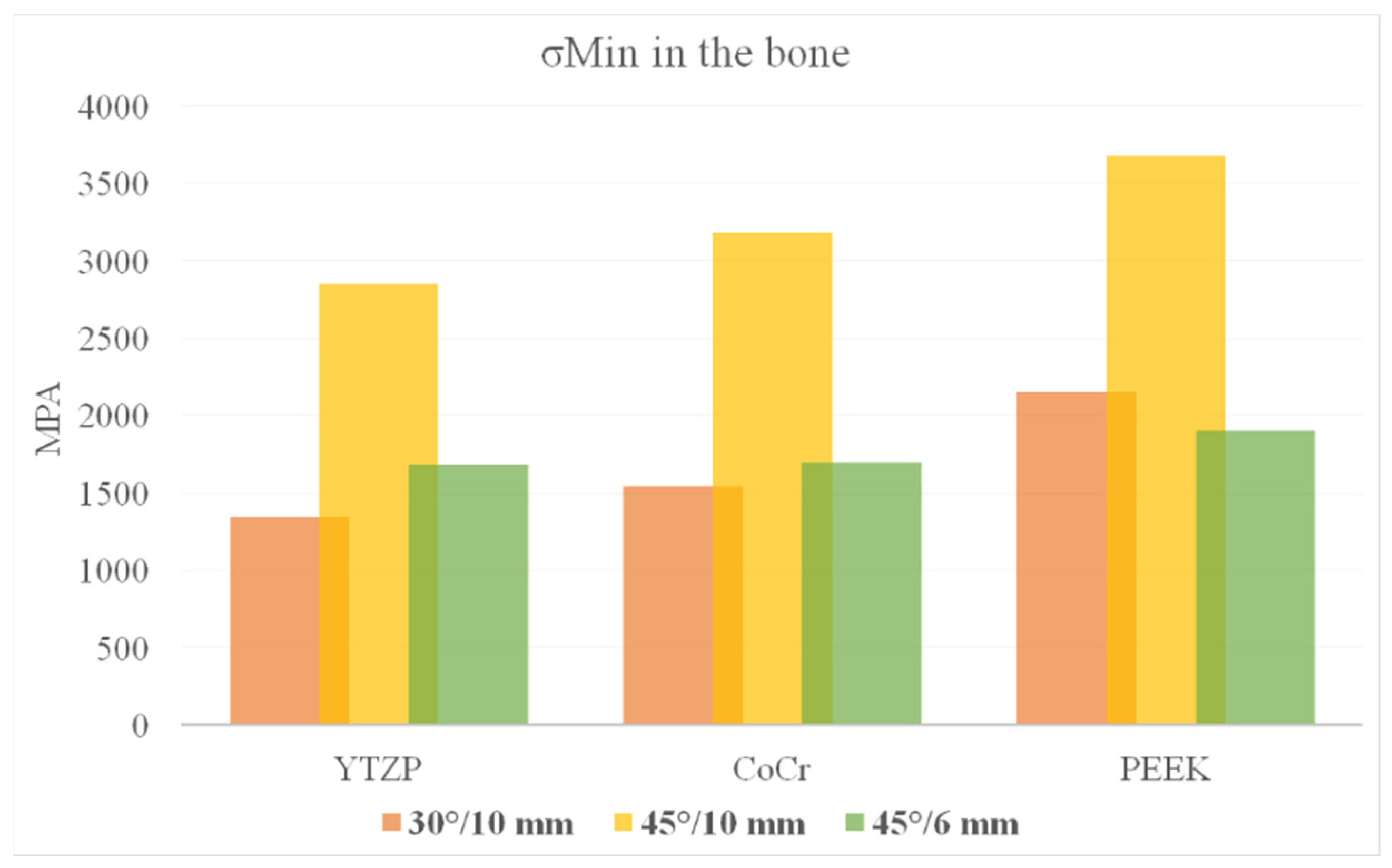
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Astrand, P.; Ahlqvist, J.; Gunne, J.; Nilson, H. Implant treatment of patients with edentulous jaws: A 20-year follow-up. Clin. Implant Dent. Relat. Res. 2008, 10, 207–217. [Google Scholar] [CrossRef]
- Jemt, T.; Johansson, J. Implant treatment in the edentulous maxillae: A 15-year follow-up study on 76 consecutive patients provided with fixed prostheses. Clin. Implant Dent. Relat. Res. 2006, 8, 61–69. [Google Scholar] [CrossRef]
- Irandoust, S.; Müftü, S. The interplay between bone healing and remodeling around dental implants. Sci. Rep. 2020, 10, 4335. [Google Scholar] [CrossRef] [Green Version]
- Gomes, L.C.L.; Pierre, F.Z.; Tribst, J.P.M.; Ramos, N.D.C.; Bresciani, E.; de Araújo, R.M.; Júnior, L.N.; Bottino, M.A. Occlusal scheme effect on the biomechanical response of full-arch dental prosthesis supported by titanium implants: A systematic review. Metals 2021, 11, 1574. [Google Scholar] [CrossRef]
- Jivraj, S.; Chee, W. Treatment planning of implants in posterior quadrants. Br. Dent. J. 2006, 201, 13–23. [Google Scholar] [CrossRef] [Green Version]
- Maló, P.; de Araújo Nobre, M.; Lopes, A.; Ferro, A.; Gravito, I. All-on-4® treatment concept for the rehabilitation of the completely edentulous mandible: A 7-year clinical and 5-year radiographic retrospective case series with risk assessment for implant failure and marginal bone level: Complete edentulous mandible rehabilitation. Clin. Implant Dent. Relat. Res. 2015, 17, e531–e541. [Google Scholar]
- Bevilacqua, M.; Tealdo, T.; Menini, M.; Pera, F.; Mossolov, A.; Drago, C.; Pera, P. The influence of cantilever length and implant inclination on stress distribution in maxillary implant-supported fixed dentures. J. Prosthet. Dent. 2011, 105, 5–13. [Google Scholar] [CrossRef]
- Capparé, P.; Teté, G.; Romanos, G.E.; Nagni, M.; Sannino, G.; Gherlone, E.F. The “All-on-four” protocol in HIV-positive patients: A prospective, longitudinal 7-year clinical study. Int. J. Oral Implantol. 2019, 12, 501–510. [Google Scholar]
- Durkan, R.; Oyar, P.; Deste, G. Maxillary and mandibular all-on-four implant designs: A review. Niger. J. Clin. Pract. 2019, 22, 1033–1040. [Google Scholar] [PubMed]
- Rubo, J.H.; Souza, E.A.C. Finite element analysis of stress in bone adjacent to dental implants. J. Oral Implantol. 2008, 34, 248–255. [Google Scholar]
- Türker, N.; Büyükkaplan, U.S.; Sadowsky, S.J.; Özarslan, M.M. Finite element stress analysis of applied forces to implants and supporting tissues using the “all-on-Four” concept with different occlusal schemes. J. Prosthodont. 2019, 28, 185–194. [Google Scholar] [CrossRef]
- Agliardi, E.; Clericò, M.; Ciancio, P.; Massironi, D. Immediate loading of full-arch fixed prostheses supported by axial and tilted implants for the treatment of edentulous atrophic mandibles. Quintessence Int. 2010, 41, 285–293. [Google Scholar]
- Agliardi, E.; Panigatti, S.; Clericò, M.; Villa, C.; Malò, P. Immediate rehabilitation of the edentulous jaws with full fixed prostheses supported by four implants: Interim results of a single cohort prospective study. Clin. Oral Implants Res. 2010, 21, 459–465. [Google Scholar] [CrossRef] [PubMed]
- Francetti, L.; Agliardi, E.; Testori, T.; Romeo, D.; Taschieri, S.; Del Fabbro, M. Immediate rehabilitation of the mandible with fixed full prosthesis supported by axial and tilted implants: Interim results of a single cohort prospective study. Clin. Implant Dent. Relat. Res. 2008, 10, 255–263. [Google Scholar] [CrossRef]
- Crespi, R.; Vinci, R.; Capparé, P.; Romanos, G.E.; Gherlone, E. A clinical study of edentulous patients rehabilitated according to the “all on four” immediate function protocol. Int. J. Oral Maxillofac. Implant. 2012, 27, 428–434. [Google Scholar]
- Liu, T.; Mu, Z.; Yu, T.; Wang, C.; Huang, Y. Biomechanical comparison of implant inclinations and load times with the all-on-4 treatment concept: A three-dimensional finite element analysis. Comput. Methods Biomech. Biomed. Eng. 2019, 22, 585–594. [Google Scholar] [CrossRef]
- Wu, A.Y.-J.; Hsu, J.-T.; Fuh, L.-J.; Huang, H.-L. Effects of positions and angulations of titanium dental implants in biomechanical performances in the all-on-four treatment: 3D numerical and strain gauge methods. Metals 2020, 10, 280. [Google Scholar] [CrossRef] [Green Version]
- Tribst, J.P.M.; Dal Piva, A.M.D.O.; Lo Giudice, R.; Borges, A.L.S.; Bottino, M.A.; Epifania, E.; Ausiello, P. The influence of custom-milled framework design for an implant-supported full-arch fixed dental prosthesis: 3D-FEA sudy. Int. J. Environ. Res. Public Health 2020, 17, 4040. [Google Scholar] [CrossRef]
- Gonzalez, J. The evolution of dental materials for hybrid prosthesis. Open Dent. J. 2014, 8, 85–94. [Google Scholar] [CrossRef] [Green Version]
- Tribst, J.P.M.; Dal Piva, A.M.D.O.; Borges, A.L.S.; Rodrigues, V.A.; Bottino, M.A.; Kleverlaan, C.J. Does the prosthesis weight matter? 3D finite element analysis of a fixed implant-supported prosthesis at different weights and implant numbers. J. Adv. Prosthodont. 2020, 12, 67–74. [Google Scholar] [CrossRef] [Green Version]
- Ashkanani, H.M.; Raigrodski, A.J.; Flinn, B.D.; Heindl, H.; Mancl, L.A. Flexural and shear strengths of ZrO2 and a high-noble alloy bonded to their corresponding porcelains. J. Prosthet. Dent. 2008, 100, 274–284. [Google Scholar] [CrossRef]
- Sailer, I.; Gottnerb, J.; Kanelb, S.; Hammerle, C.H.F. Randomized controlled clinical trial of zirconia-ceramic and metal-ceramic posterior fixed dental prostheses: A 3-year follow-up. Int. J. Prosthodont. 2009, 22, 553–560. [Google Scholar]
- Takaba, M.; Tanaka, S.; Ishiura, Y.; Baba, K. Implant-supported fixed dental prostheses with CAD/CAM-fabricated porcelain crown and zirconia-based framework: CAD/CAM porcelain crowns and Zirconia framework. J. Prosthodont. 2013, 22, 402–407. [Google Scholar] [CrossRef]
- Pokorný, D.; Fulín, P.; Slouf, M.; Jahoda, D.; Landor, I.; Sosna, A. Polyetheretherketone (PEEK). Part II: Application in clinical practice. Acta Chir. Orthop. Traumatol. Cech. 2010, 77, 470–478. [Google Scholar]
- Papathanasiou, I.; Kamposiora, P.; Papavasiliou, G.; Ferrari, M. The use of PEEK in digital prosthodontics: A narrative review. BMC Oral Health 2020, 20, 217. [Google Scholar] [CrossRef]
- Dal Piva, A.M.D.O.; Tribst, J.P.M.; Borges, A.L.S.; Souza, R.O.d.A.e.; Bottino, M.A. CAD-FEA modeling and analysis of different full crown monolithic restorations. Dent. Mater. 2018, 34, 1342–1350. [Google Scholar] [CrossRef] [Green Version]
- Tribst, J.P.M.; Dal Piva, A.M.D.O.; Bottino, M.A.; Kleverlaan, C.J.; Koolstra, J.H. Mouthguard use and TMJ injury prevention with different occlusions: A three-dimensional finite element analysis. Dent. Traumatol. 2020, 36, 662–669. [Google Scholar] [CrossRef]
- Idogava, H.T.; Noritomi, P.Y.; Daniel, G.B. Numerical model proposed for a temporomandibular joint prosthesis based on the recovery of the healthy movement. Comput. Methods Biomech. Biomed. Eng. 2018, 21, 503–511. [Google Scholar] [CrossRef]
- Dal Piva, A.M.D.O.; Tribst, J.M.; de Morais, D.; Alonso, A.; Borges, A.S. Comparative three-dimensional finite element analysis of implant-supported fixed complete arch mandibular prostheses in two materials. J. Indian Prosthodont. Soc. 2017, 17, 255. [Google Scholar] [CrossRef]
- Penteado, M.M.; Tribst, J.P.M.; Dal Piva, A.M.; Ausiello, P.; Zarone, F.; Garcia-Godoy, F.; Borges, A.L. Mechanical behavior of conceptual posterior dental crowns with functional elasticity gradient. Am. J. Dent. 2019, 32, 165–168. [Google Scholar]
- Ausiello, P.; Ciaramella, S.; Di Rienzo, A.; Lanzotti, A.; Ventre, M.; Watts, D.C. Adhesive class I restorations in sound molar teeth incorporating combined resin-composite and glass ionomer materials: CAD-FE modeling and analysis. Dent. Mater. 2019, 35, 1514–1522. [Google Scholar] [CrossRef]
- Martorelli, M.; Ausiello, P. A novel approach for a complete 3D tooth reconstruction using only 3D crown data. Int. J. Interact. Des. Manuf. (IJIDeM) 2013, 7, 125–133. [Google Scholar] [CrossRef]
- Bonfante, E.A.; Coelho, P.G. A critical perspective on mechanical testing of implants and prostheses. Adv. Dent. Res. 2016, 28, 18–27. [Google Scholar] [CrossRef]
- DeLong, R.; Douglas, W.H. Development of an artificial oral environment for the testing of dental restoratives: Bi-axial force and movement control. J. Dent. Res. 1983, 62, 32–36. [Google Scholar] [CrossRef]
- Ausiello, P.; Tribst, J.P.M.; Ventre, M.; Salvati, E.; di Lauro, A.E.; Martorelli, M.; Lanzotti, A.; Watts, D.C. The role of cortical zone level and prosthetic platform angle in dental implant mechanical response: A 3D finite element analysis. Dent. Mater. 2021, 37, 1688–1697. [Google Scholar] [CrossRef]
- Mericske-Stern, R.; Assal, P.; Mericske, E.; Ing, W.B. Occlusal force and oral tactile sensibility measured in partially edentulous patients with ITI implants. Implant Dent. 1996, 5, 59. [Google Scholar] [CrossRef]
- Horita, S.; Sugiura, T.; Yamamoto, K.; Murakami, K.; Kirita, T. Biomechanical analysis of immediately loaded implants according to the all-on-four concept. Int. J. Oral Maxillofac. Surg. 2017, 46, 268. [Google Scholar] [CrossRef] [Green Version]
- Villefort, R.F.; Tribst, J.P.M.; Dal Piva, A.M.D.O.; Borges, A.L.; Binda, N.C.; Ferreira, C.E.d.A.; Bottino, M.A.; von Zeidler, S.L.V. Stress distribution on different bar materials in implant-retained palatal obturator. PLoS ONE 2020, 15, e0241589. [Google Scholar] [CrossRef]
- Maló, P.; de Araújo Nobre, M.; Moura Guedes, C.; Almeida, R.; Silva, A.; Sereno, N.; Legatheaux, J. Short-term report of an ongoing prospective cohort study evaluating the outcome of full-arch implant-supported fixed hybrid polyetheretherketone-acrylic resin prostheses and the All-on-Four concept. Clin. Implant Dent. Relat. Res. 2018, 20, 692–702. [Google Scholar] [CrossRef]
- De Araújo Nobre, M.; Moura Guedes, C.; Almeida, R.; Silva, A.; Sereno, N. Hybrid polyetheretherketone (PEEK)-acrylic resin prostheses and the all-on-4 concept: A full-arch implant-supported fixed solution with 3 years of follow-up. J. Clin. Med. 2020, 9, 2187. [Google Scholar] [CrossRef]
- Çalışkan, A.; Yöndem, İ. Stress Analysis Of Fixed Dental Prostheses Produced With Different Materials According To The All-On-Four Concept. J. Biotechnol. Strateg. Health Res. 2019, 3, 183–191. [Google Scholar] [CrossRef]
- Bankoğlu Güngör, M.; Yılmaz, H. Evaluation of stress distributions occurring on zirconia and titanium implant-supported prostheses: A three-dimensional finite element analysis. J. Prosthet. Dent. 2016, 116, 346–355. [Google Scholar] [CrossRef]
- Bellini, C.M.; Romeo, D.; Galbusera, F.; Taschieri, S.; Raimondi, M.T.; Zampelis, A.; Francetti, L. Comparison of tilted versus nontilted implant-supported prosthetic designs for the restoration of the edentuous mandible: A biomechanical study. Int. J. Oral Maxillofac. Implant. 2009, 24, 511–517. [Google Scholar]
- Bhering, C.L.B.; Mesquita, M.F.; Kemmoku, D.T.; Noritomi, P.Y.; Consani, R.L.X.; Barão, V.A.R. Comparison between all-on-four and all-on-six treatment concepts and framework material on stress distribution in atrophic maxilla: A prototyping guided 3D-FEA study. Mater. Sci. Eng. C Mater. Biol. Appl. 2016, 69, 715–725. [Google Scholar] [CrossRef]
- Tashkandi, E.A.; Lang, B.R.; Edge, M.J. Analysis of strain at selected bone sites of a cantilevered implant-supported prosthesis. J. Prosthet. Dent. 1996, 76, 158–164. [Google Scholar] [CrossRef]
- Takahashi, T.; Shimamura, I.; Sakurai, K. Influence of number and inclination angle of implants on stress distribution in mandibular cortical bone with All-on-4 Concept. J. Prosthodont. Res. 2010, 54, 179–184. [Google Scholar] [CrossRef]
- Campaner, L.M.; Silveira, M.P.M.; de Andrade, G.S.; Borges, A.L.S.; Bottino, M.A.; Dal Piva, A.M.D.O.; Lo Giudice, R.; Ausiello, P.; Tribst, J.P.M. Influence of polymeric restorative materials on the stress distribution in posterior fixed partial dentures: 3D finite element analysis. Polymers 2021, 13, 758. [Google Scholar] [CrossRef] [PubMed]
- Tribst, J.P.M.; Dal Piva, A.M.D.O.; Borges, A.L.S.; Araújo, R.M.; da Silva, J.M.F.; Bottino, M.A.; Kleverlaan, C.J.; de Jager, N. Effect of different materials and undercut on the removal force and stress distribution in circumferential clasps during direct retainer action in removable partial dentures. Dent. Mater. 2020, 36, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Villefort, R.F.; Diamantino, P.J.S.; von Zeidler, S.L.V.; Borges, A.L.S.; Silva-Concílio, L.R.; Saavedra, G.D.S.F.A.; Tribst, J.P.M. Mechanical response of PEKK and PEEK as frameworks for implant-supported full-arch fixed dental prosthesis: 3D finite element analysis. Eur. J. Dent. 2021. [Google Scholar] [CrossRef] [PubMed]
- Treglia, A.S.; Turco, S.; Ulianich, L.; Ausiello, P.; Lofrumento, D.D.; Nicolardi, G.; Miele, C.; Garbi, C.; Beguinot, F.; Di Jeso, B. Cell fate following ER stress: Just a matter of “quo ante” recovery or death? Histol. Histopathol. 2012, 27, 1–12. [Google Scholar]
- Apicella, A.; Di Palma, L.; Aversa, R.; Ausiello, P. DSC kinetic characterization of dental composites using different light sources. J. Adv. Mater. 2002, 34, 22–25. [Google Scholar]
- Kelkar, K.C.; Bhat, V.; Hegde, C. Finite element analysis of the effect of framework materials at the bone-implant interface in the all-on-four implant system. Dent. Res. J. 2021, 18, 1. [Google Scholar]
- Saleh Saber, F.; Ghasemi, S.; Koodaryan, R.; Babaloo, A.; Abolfazli, N. The comparison of stress distribution with different implant numbers and inclination angles in all-on-four and conventional methods in maxilla: A finite element analysis. J. Dent. Res. Dent. Clin. Dent. Prospects 2015, 9, 246–253. [Google Scholar] [CrossRef]
- Haroun, F.; Ozan, O. Evaluation of stresses on implant, bone, and restorative materials caused by different opposing arch materials in hybrid prosthetic restorations using the All-on-4 technique. Materials 2021, 14, 4308. [Google Scholar] [CrossRef]
- Shetty, R.; Singh, I.; Sumayli, H.A.; Jafer, M.A.; Abdul Feroz, S.M.; Bhandi, S.; Raj, A.T.; Patil, S.; Ferrari, M. Effect of prosthetic framework material, cantilever length and opposing arch on peri-implant strain in an all-on-four implant prostheses. Niger. J. Clin. Pract. 2021, 24, 866–873. [Google Scholar]
- Ebadian, B.; Farzin, M.; Talebi, S.; Khodaeian, N. Evaluation of stress distribution of implant-retained mandibular overdenture with different vertical restorative spaces: A finite element analysis. Dent. Res. J. 2012, 9, 741–747. [Google Scholar]
- Malhotra, A.O.; Padmanabhan, T.V.; Mohamed, K.; Natarajan, S.; Elavia, U. Load transfer in tilted implants with varying cantilever lengths in an all-on-four situation: Load transfer in an all-on-four situation. Aust. Dent. J. 2012, 57, 440–445. [Google Scholar] [CrossRef]
- Refaie, A.; Zohdy, M.; Aboelfadl, A.; Wahsh, M. Effect of different immediate implant loading protocols on Peri-implant soft tissue health. Braz. Dent. Sci. 2020, 23, 7. [Google Scholar] [CrossRef]
- Tribst, J.P.M.; Dal Piva, A.M.D.O.; Rodrigues, V.A.; Borges, A.L.S.; Nishioka, R.S. Stress and strain distributions on short implants with two different prosthetic connections—An in vitro and in silico analysis. Braz. Dent. Sci. 2017, 20, 101–109. [Google Scholar] [CrossRef] [Green Version]
- Ceruso, F.M.; Ieria, I.; Martelli, M.; Lumbau, A.I.; Xhanari, E.; Gargari, M. New generation of fixture-abutment connection combining soft tissue design and vertical screw-retained restoration: 1-year clinical, aesthetics and radiographic preliminary evaluation. Dent. J. 2021, 9, 35. [Google Scholar] [CrossRef]
- Barreiros, P.; Neves, L.; Aroso, C.; Mendes, J.M.; Silva, A.S. Comparison in four different implant systems of mechanical resistance to maximal stress in prosthetic screws-an in vitro study. Dent. J. 2020, 8, 116. [Google Scholar] [CrossRef] [PubMed]


| Inclination of Distal Implants (°) | Distal Cantilever (mm) | Nodes | Elements |
|---|---|---|---|
| 30 | 10 | 1.133.298 | 645.591 |
| 45 | 10 | 1.037.324 | 625.014 |
| 45 | 6 | 1.084.148 | 597.018 |
| Structure | Elastic Modulus (GPa) | Poisson Ratio |
|---|---|---|
| Cancellous bone | 1.37 | 0.3 |
| Cortical bone | 13.7 | 0.3 |
| CoCr | 210 | 0.3 |
| Y-TZP | 200 | 0.3 |
| PEEK | 4 | 0.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tribst, J.P.M.; Campanelli de Morais, D.; Melo de Matos, J.D.; Lopes, G.d.R.S.; Dal Piva, A.M.d.O.; Souto Borges, A.L.; Bottino, M.A.; Lanzotti, A.; Martorelli, M.; Ausiello, P. Influence of Framework Material and Posterior Implant Angulation in Full-Arch All-on-4 Implant-Supported Prosthesis Stress Concentration. Dent. J. 2022, 10, 12. https://doi.org/10.3390/dj10010012
Tribst JPM, Campanelli de Morais D, Melo de Matos JD, Lopes GdRS, Dal Piva AMdO, Souto Borges AL, Bottino MA, Lanzotti A, Martorelli M, Ausiello P. Influence of Framework Material and Posterior Implant Angulation in Full-Arch All-on-4 Implant-Supported Prosthesis Stress Concentration. Dentistry Journal. 2022; 10(1):12. https://doi.org/10.3390/dj10010012
Chicago/Turabian StyleTribst, João Paulo Mendes, Dayana Campanelli de Morais, Jefferson David Melo de Matos, Guilherme da Rocha Scalzer Lopes, Amanda Maria de Oliveira Dal Piva, Alexandre Luiz Souto Borges, Marco Antonio Bottino, Antonio Lanzotti, Massimo Martorelli, and Pietro Ausiello. 2022. "Influence of Framework Material and Posterior Implant Angulation in Full-Arch All-on-4 Implant-Supported Prosthesis Stress Concentration" Dentistry Journal 10, no. 1: 12. https://doi.org/10.3390/dj10010012
APA StyleTribst, J. P. M., Campanelli de Morais, D., Melo de Matos, J. D., Lopes, G. d. R. S., Dal Piva, A. M. d. O., Souto Borges, A. L., Bottino, M. A., Lanzotti, A., Martorelli, M., & Ausiello, P. (2022). Influence of Framework Material and Posterior Implant Angulation in Full-Arch All-on-4 Implant-Supported Prosthesis Stress Concentration. Dentistry Journal, 10(1), 12. https://doi.org/10.3390/dj10010012












