Abstract
The objective of this study was to evaluate the power output of two dental devices. The study examined two semiconductor lasers, namely, SIROLaser Blue (445 nm, 970 nm) and Picasso (810 nm). The power output performance was studied at the maximum output power of the devices. The study compared the preset power output measured by a power meter in a continuous-wave mode and in pulsed mode at 50% duty cycles. Ten 60 s measurements were performed for each setting. The largest difference between the stipulated and the actual output power at continuous-wave (D-cw) and pulsed (D-p) modes was calculated. Moreover, the percentage variations in the mean output power at continuous-wave (%D-cw) and pulsed (%D-p) modes were calculated. The D-cw values for 445 nm, 970 nm, and 810 nm lasers were 0.7 W, 0.5 W, and −0.3 W, respectively, and %D-cw values were 21%, 23%, and −8%, respectively. The D-p values for 445 nm, 970 nm, and 810 nm lasers were 1.1 W, 0.5 W, and −0.1 W, respectively, whereas the %D-p values were 37%, 26%, and −3%, respectively. This study found that the actual power is not necessarily lower but can be higher than the displayed power output. Clinicians are recommended to calibrate the laser output by using a power meter before use.
1. Introduction
Lasers have emerged as a safe, minimally invasive, and convenient tool in dentistry in the past few decades. Compared to the conventional dental scalpel, lasers can minimize bleeding and swelling, reduce pain and anxiety, and preserve more healthy tooth material in dental treatment []. Various types of lasers are available, such as carbon dioxide (CO2) laser, Neodymium Yttrium Aluminum Garnet (Nd:YAG) laser, Erbium-doped Yttrium Aluminium Garnet (Er:YAG) laser, Erbium, Chromium:yttrium-scandium-gallium-garnet (Er,Cr:YSGG) laser, and semiconductor lasers []. Compared to other laser systems, semiconductor lasers take up little space and are quite portable due to their low weight. Moreover, their affordable price makes them accessible to a wide range of dental professionals []. Because of their compact size, relatively affordable pricing, and versatility, semiconductor lasers are gaining popularity in the treatment of dental diseases [].
Energy from near-infrared semiconductor lasers is mainly absorbed by pigmented tissues. Melanin, hemoglobin, and protein are the primary chromophores. Semiconductor lasers are mainly used for soft tissue procedures []. It offers better patient satisfaction and comfort than traditional scalpels in soft tissue management [,], because it offers intraoperative and postoperative clinical advantages, such as hemostasis, reduced post-operative edema, effective wound healing, and decreased scar formation []. Semiconductor lasers can also be used for applications involving dental hard tissue, such as root canal disinfection [,], cervical dentinal hypersensitivity treatment [], laser-assisted tooth whitening [], and caries prevention [].
Conventionally, the available dental semiconductor lasers emit wavelengths ranging from 635 nm to 1064 nm. Recently, the 445 nm semiconductor laser, which emits blue light in the visible spectrum, has become commercially available in the dental market. Modern dental semiconductor lasers can operate in continuous-wave and pulsed modes []. Continuous-wave mode means that the laser continuously emits light and is generally the fastest way to ablate tissue, but heat can build up and cause collateral damage to the target and adjacent tissues []. In order to decrease thermal damage and carbonization as well as allow for thermal recovery of the tissue, modern laser instruments are equipped with pulsed mode, and their energy is emitted in pulses. There are two basic forms of pulsed laser modes: free-running pulsed and gated-pulsed []. Free-running pulse emission occurs with very short bursts of laser energy due to a very rapid on–off pumping mechanism []. Nd:YAG, Er:YAG, and Er,Cr:YSGG and some carbon dioxide devices are the typical free-running emission lasers []. Gated-pulsed mode is usually made with a shutter that hinders the laser beam from reaching the fiber tip at a certain rate []. The laser is constantly switched on, but the shutter device blocks the light from transmitting. Potassium-titanyl-phosphate (KTP) laser and semiconductor lasers are the typical gated-pulsed emission lasers [].
Often, the power indicated on that panel does not correspond to the power at the exit of the handpiece or fiber []. The common components of nearly all types of laser devices involve an active medium, a pumping mechanism, a resonator, a cooling system, controls, and a delivery system. Each element may influence the entire schematic []. Current semiconductor lasers are electronically pumped. Individual diode chip generates relatively low energy output, so current surgical semiconductor lasers employ groups of individual diode chips concurrently to achieve the desired power output []. The output power of a semiconductor laser is measured by the optical power output as a function of the drive current’s input characteristic. However, in the actual situation, useful power levels can be impacted by other factors including kinks, power rollover with increasing current, and catastrophic optical damage []. In addition, the operation of a semiconductor laser at constant drive current and temperature over a long period of time usually leads to a reduction in optical output power. This drop-off depends on the laser structure, including materials, fabrication technology, and how well thermal dissipation is managed [].
A laser’s output power is one of the most critical parameters for determining its interaction with the target tissue. Insufficient power will be inadequate to create a desired clinical outcome. A high output power generates substantial heat, which may damage the tissue. Clinicians need to check the power output of the lasers by using a power meter or energy meter. Blue (Dentsply Sirona, Bensheim, Germany) and Picasso (AMD Lasers, West Jordan, UT, USA) are commonly used dental semiconductor lasers on the market. The 445 nm, 970 nm, and 810 nm diode lasers can all be used for various clinical treatments, such as soft tissue surgery, periodontal therapy, endodontic treatment, and tooth whitening [,,,,]. The 445 nm diode laser has a higher cutting than other near-infrared diode lasers because it has higher absorption for melanin and hemoglobin [,]. We intended to check whether the common semiconductor lasers’ accuracy is the same as the manufacturer indicated. Therefore, we conducted this study. The study aimed to evaluate the power output of two common dental semiconductor lasers.
2. Materials and Methods
This was an observational study conducted at the Prince Philip Dental Hospital, Hong Kong. We used SIROLaser Blue (wavelengths at 445 nm and 970 nm) with a fiber tip 320 µm in diameter and Picasso (wavelength of 810 nm) with a fiber tip 300 µm in diameter. The two laser devices were new and provided by two local dealers. The tip is uninitiated and brand new. For every ten usages, the tip was changed to a new one. The ambient room temperature is 25 °C. We operated both laser devices in continuous-wave and pulsed modes, and the output power was adjustable. The 810 nm semiconductor laser has a fixed pulse rate and duration, and for the SIROLaser Blue semiconductor laser, the pulse duration can be controlled, and the interval between each pulse is adjustable. We fixed the handpiece with a universal laboratory clamp to avoid any slight movement, and we ensured that the fiber was perpendicular to the sensor. We used a wireless foot pedal to control the laser device so that the handpiece remained steady on the clamp. We positioned the fiber tip 1 cm away from the power meter’s base. We evaluated the lasers’ performance of power output in their continuous-wave mode and pulsed mode separately and at their maximum output power. Table 1 and Table 2 present the laser settings for SIROLaser Blue and Picasso. We measured the laser’s power output with a PowerMax Pro 150F HD-50 mW-150 W fan-cooled sensor and LabMax-Pro SSIM Laser Power Meter (Coherent Inc., Santa Clara, CA, USA). The power meter has the function of temperature compensation and wavelength correction on every measurement sample. We performed the power measurement in high-speed mode. The calibration of the power meter was performed by the manufacturer prior to conducting the experiment.

Table 1.
Parameters stipulated and actual power of laser devices in continuous-wave mode.

Table 2.
Parameters stipulated and actual power of laser devices in pulsed mode.
2.1. Power Delivered in Continuous-Wave Mode
In continuous-wave mode, the manufacturer claimed a maximum output power of 3 W, 2 W, and 2.5 W for the 445 nm, 970 nm, and 810 nm semiconductor lasers, respectively. We observed the power output with the power meter for 60 s. The average, minimum, and maximum powers were displayed on the software for each measurement. We recorded the power output each time. We repeated the procedure ten times. We identified the highest and lowest power output and calculated the mean output power.
2.2. Power Delivered in Pulsed Mode
In pulsed mode, the manufacturer claimed an output power of 3 W, 2 W, and 2.5 W for the 445 nm, 970 nm, and 810 nm semiconductor lasers, respectively. Therefore, the average power at 50% duty cycle should be 1.5 W, 1 W, and 1.2 W. We observed the power output with the power meter for 5 s. The average power and output power were displayed on the software for each measurement. We recorded the average power and output power each time. We repeated the procedure ten times. We identified the highest and lowest output and calculated the mean of the average power.
After completing the measurements, we conducted statistical analyses of the collected data using the SPSS Statistics—V25.0 software (IBM Corporation, Armonk, NY, USA). We obtained the mean value for each measurement. According to the highest power output we identified and the mean power we calculated, we computed the percentage change in the average power in continuous-wave and pulsed modes and the percentage change in the maximum output power in the pulsed mode test. Then, we calculated the range in output power.
3. Results
3.1. Test in Continuous-Wave Mode
The actual power output of the SIROLaser Blue (445 nm) laser in continuous-wave mode was not steady in the first 30 s. It became steady after 30 s (Figure 1). The actual output power of the SIROLaser Blue (445 nm) was always higher than the preset output power by 0.5–0.7 W. Similarly, the power output of the SIROLaser Blue (970 nm) was unstable at the beginning in the continuous-wave mode. Unlike the 445 nm semiconductor laser, which showed an upward fluctuation initially, the power output of Picasso (810 nm) started at its highest and gradually decreased to a stable level (Figure 2). The actual output power of Picasso in continuous-wave mode was always lower than the preset output power by 0.4–0.5 W. Picasso performed differently in the continuous-wave mode from SIROLaser Blue. The actual output power of Picasso was not always higher than the preset output power, and it fluctuated from −0.3 W to 0.1 W, compared to the preset output power. Figure 3 shows the representative power output of Picasso in continuous-wave modes. The percentage change in the mean output power of the 445 nm, 970 nm, and 810 nm lasers was 21%, 23%, and −8%, respectively.
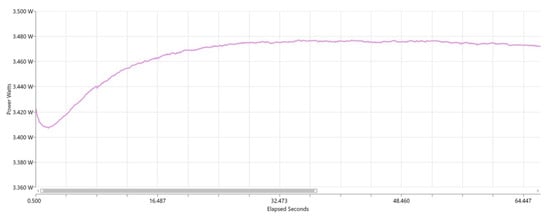
Figure 1.
Representative power output of the SIROLaser Blue (445 nm) in continuous-wave mode over 60 s.
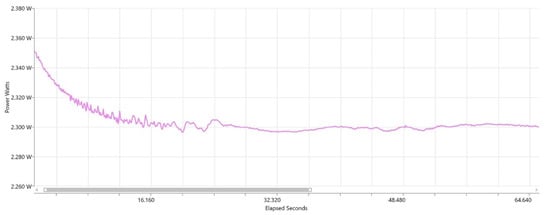
Figure 2.
Representative power output of the SIROLaser Blue (970 nm) in continuous-wave mode over 60 s.
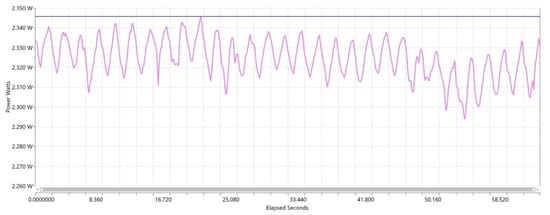
Figure 3.
Representative power output of the Picasso (810 nm) in continuous-wave mode over 60 s.
3.2. Test in Pulsed Mode
The actual power output of the SIROLaser Blue (445 nm) semiconductor laser spiked, whereas the shape of the power output of SIROLaser Blue (970 nm) and Picasso was closer to a rectangular shape, as Figure 4, Figure 5 and Figure 6 show. The pulses of SIROLaser Blue and Picasso were all evenly distributed. The actual output power of SIROLaser Blue (445 nm) in pulsed mode was always higher than the preset output power by 1.0–1.1 W. The output power of SIROLaser Blue (970 nm) was also approximately 0.5 W higher than the preset output power. Nevertheless, the actual output power of Picasso in pulsed mode was always lower than the preset output power by approximately 0.1 W. The percentage change in the mean output power of the SIROLaser Blue (445 nm), SIROLaser Blue (970 nm), and Picasso (810 nm) semiconductor lasers was 37%, 26% and −3%, respectively. The mean average power of SIROLaser Blue (445 nm) and SIROLaser Blue (970 nm) was 0.9 W and 0.5 W higher than its preset average power, respectively, and the mean power of Picasso (810 nm) was 0.1 W lower than its pre-set average power. The percentage changes in the mean power of SIROLaser Blue (445 nm), SIROLaser Blue (970 nm), and Picasso (810 nm) were 29%, 24%, and −5%, respectively. Table 1 and Table 2 show the percentage change in the mean power and output power as well as the range in variation between actual power and preset power in continuous-wave and pulsed modes.
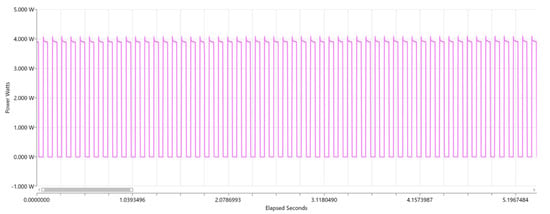
Figure 4.
Representative power output of SIROLaser Blue (445 nm) in pulsed mode over 5 s.
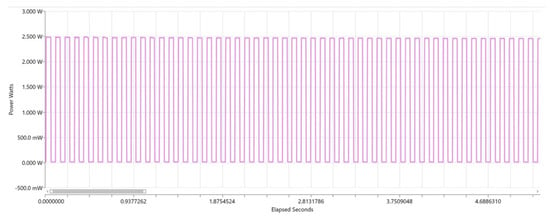
Figure 5.
Representative power output of SIROLaser Blue (970 nm) in pulsed mode over 5 s.
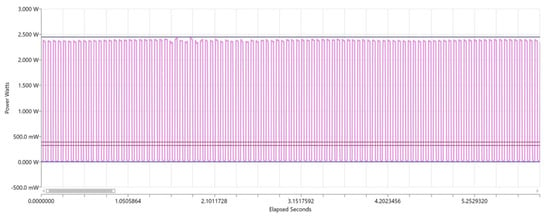
Figure 6.
Representative power output of Picasso (810 nm) in pulsed mode over 5 s.
4. Discussion
The power output of the laser directly determined the effectiveness and safety of laser treatment. This is the first observational study to investigate the power output of the two common semiconductor lasers. This study used one machine for each laser evaluation. Laser machines are medical devices for clinical use. It is reasonable to assume that every laser machine must pass stringent quality control. We did not assess several machines of the same manufacturers because it is not the objective of this study to evaluate quality control or to compare machines of the same series and type. In this study, we use LabMax-Pro SSIM Laser Power Meter (Coherent Inc., Santa Clara, CA, USA). Coherent is a registered ISO 9001:2000 company, and this product is NMI (National Metrology Institute)-traceable and CE (Conformitè Europëenne)-marked. This power meter can deliver precise measurements and high accuracy with calibration uncertainty within 1%.
Semiconductor lasers (diode lasers) use solid material (some combination of gallium, arsenide, and other elements such as aluminum and indium) as active media to convert electrical energy into light energy, and each diode “chip” generates a relatively low-energy output []. At milliwatt power level, the low-power semiconductor laser is generally used for low-level laser therapy. However, individual diode chips can be employed in parallel to increase the power output. Variations in each laser diode can affect the overall power output. We did not measure the power output of the 660 nm low-level laser from SIROLaser Blue. The laser at 660 nm is recommended for photobiomodulation with small power within the mW range []. In addition, the fiber tip used at 660 nm is comparatively large at 4 mm and 8 mm. In addition, the power output for photobiomodulation is very small and within the mW range.
It is generally accepted that the actual power at the exit of the fiber tip will be lower than the power indicated on that panel due to energy loss during energy transport and degradation phenomena. However, our study found that this point of view is not always true. The actual power output for SIROLaser Blue (445 nm and 970 nm) was higher than the preset power. The results showed that the largest difference in power output was in SIROLaser Blue (445 nm), which is probably due to a compromise in reliability at high optical power. However, factors such as optical power density at the output facet, heat dissipation, and current density in the semiconductor also affect the power output of the laser [].
Laser tissue interaction depends on many factors, such as the operator-dependent factors (modality of use, application time and speed, and distance from the tissue) and the operator-independent factors related to the wavelength and preset parameters. However, the power output of dental lasers should be precise, which is determined by their application in clinical treatment. This study found considerable deviations in the power output of semiconductor lasers. The deviation in the power of the 455 nm laser was up to an increase of 21% (0.7 W) in continuous mode and 29% (1.1 W) in pulsed mode. A study investigated cut efficiency as well as the thermal effects of the 455 nm laser []. The investigators conducted incisions on porcine gingiva in continuous mode using a 320 μm fiber tip at a cut speed of 2 mm s−1. They found that irradiation with 3.5 W had a significantly larger zone of collateral thermal damage in gingiva than that with 3.0 W []. Reducing collateral thermal damage from laser incisions is important to promote wound healing and to minimize the postoperative discomfort of patients [].
In addition, excessive heat caused by excessive power may damage the pulp, even leading to pulpitis or pulp necrosis. A study compared irradiation on tooth root surfaces with an 808 nm diode laser at 417 mW and 207 mW in continuous mode for 30 s. The 417 mW irradiation increased pulpal temperature of thin-walled teeth above the threshold (5.5 °C), whereas 207 mW irradiation did not []. Excessive heat due to excessive power also could damage the periodontal tissues. Another study evaluated the temperature changes on the root surfaces of incisors with 810 nm laser irradiation. The root canals of the incisors were irradiated in continuous mode at 3.0 W and 3.5W. The study reported that 3.0 W irradiation did not create thermal damage. However, 3.5 W irradiation increased the temperature of the outer root surface by 7 °C, which could damage periodontal tissues [].
We observed the lasers’ output power for 60 s in continuous-wave mode and 5 s in pulsed mode. We found that the power output of lasers in pulsed mode remained stable over time, whereas the power output of lasers in continuous-wave mode fluctuated for a while, and it took some time for the power output to stay constant. Many dentists do not irradiate lasers on the tissue for a long time. They normally activate the laser device by stepping on the foot paddle for a few seconds and stopping for a while before they continue. We found the output power to be unstable in the first few seconds. Therefore, a significant variation in output power can occur in clinical practice.
Keeping the incident laser beam perpendicular to the tissue can achieve maximum control of laser-tissue interaction. To mimic this position in the laboratory, we used a clamp to make sure the fiber was perpendicular to the sensor of the power meter. In clinical practice, dentists can bend the tip to a proper angle to ensure that the fiber tip is perpendicular to oral tissue during irradiation. A light ray travels in a straight line when it is perpendicular to the surface between two mediums, while the ray refracts when applied at an angle relative to the surface. Moreover, there may be unnecessary damage to adjacent tissues []. Note that the fiber angle is compromised at an angle when comes to fibrous tissue ablation and the laser tip is in light contact with the tissue. It is because the movement of fiber will be smoother without being stuck at a fixed point which would cause more thermal damage. Also, visual field is improved.
In this study, we observed a steady pulse distribution and frequency in the two semiconductor laser devices. The mode of pulse emission will affect the evenness of pulse distribution. Some laser users consider that the laser pulses are evenly distributed because the emission mode for dental semiconductor lasers only included continuous-wave mode and gated-pulsed mode []. The pulse distribution is largely dependent on the construction of the mechanical shutter. For devices that use individual shutters for each semiconductor to control the frequency and duration of the pulses, they can have unevenly distributed pulses.
5. Conclusions
We found a discrepancy between the preset power output and that measured by the power meter of the two dental devices for semiconductor lasers, and the actual power is not necessarily lower but can be higher than the displayed power output. For clinicians, we recommend checking the power output of their laser devices with a power meter for the safe and effective use of laser. We also suggest that manufacturers equip a calibration function on the laser device as part of the setup procedure.
Author Contributions
Conceptualization, K.L., E.C.M.L. and C.H.C.; Data curation, V.W.X. and J.Y.N.; Formal analysis, V.W.X.; Funding acquisition, C.H.C.; Investigation, V.W.X. and I.X.Y.; Methodology, K.L.; Resources, K.L.; Software, J.Y.N. and K.L.; Supervision, E.C.M.L. and C.H.C.; Validation, I.X.Y.; Writing—original draft, V.W.X.; Writing—review & editing, C.H.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research is funded by the National Natural Science Foundation of China (Project Number: 81870812).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Verma, S.K.; Maheshwari, S.; Singh, R.K.; Chaudhari, P.K. Laser in dentistry: An innovative tool in modern dental practice. Natl. J. Maxillofac. Surg. 2012, 3, 124–132. [Google Scholar] [CrossRef] [Green Version]
- Karic, V.; Melman, G.; Mulder, R. Introduction to Dental Lasers. S. Afr. Dent. J. 2016, 71, 178. [Google Scholar]
- Rios, F.G.; Viana, E.R.; Ribeiro, G.M.; González, J.C.; Abelenda, A.; Peruzzo, D.C. Temperature evaluation of dental implant surface irradiated with high-power diode laser. Lasers Med. Sci. 2016, 31, 1309–1316. [Google Scholar] [CrossRef] [PubMed]
- Derikvand, N.; Chinipardaz, Z.; Ghasemi, S.; Chiniforush, N. The versatility of 980 nm diode laser in dentistry: A case series. J. Lasers Med. Sci. 2016, 7, 205. [Google Scholar] [CrossRef] [PubMed]
- Ortega-Concepción, D.; Cano-Durán, J.A.; Peña-Cardelles, J.F.; Paredes-Rodríguez, V.M.; González-Serrano, J.; López-Quiles, J. The application of diode laser in the treatment of oral soft tissues lesions. A literature review. J. Clin. Exp. Dent. 2017, 9, e925–e928. [Google Scholar] [CrossRef] [Green Version]
- Kumar, R.; Jain, G.; Dhodapkar, S.V.; Kumathalli, K.I.; Jaiswal, G. The Comparative Evaluation of Patient’s Satisfaction and Comfort Level by Diode Laser and Scalpel in the Management of Mucogingival Anomalies. J. Clin. Diagn Res. 2015, 9, ZC56–ZC58. [Google Scholar] [CrossRef] [PubMed]
- Michalik, M.; Szymańczyk, J.; Stajnke, M.; Ochrymiuk, T.; Cenian, A. Medical Applications of Diode Lasers: Pulsed versus Continuous Wave (cw) Regime. Micromachines 2021, 12, 710. [Google Scholar] [CrossRef] [PubMed]
- Azma, E.; Safavi, N. Diode laser application in soft tissue oral surgery. J. Lasers Med. Sci. 2013, 4, 206–211. [Google Scholar] [PubMed]
- Bago, I.; Plečko, V.; Gabrić Pandurić, D.; Schauperl, Z.; Baraba, A.; Anić, I. Antimicrobial efficacy of a high-power diode laser, photo-activated disinfection, conventional and sonic activated irrigation during root canal treatment. Int. Endod. J. 2013, 46, 339–347. [Google Scholar] [CrossRef] [Green Version]
- Beer, F.; Farmakis, E.T.; Kopic, J.; Kurzmann, C.; Moritz, A. Temperature Development on the External Root Surface During Laser-Assisted Endodontic Treatment Applying a Microchopped Mode of a 980 nm Diode Laser. Photomed. Laser Surg. 2017, 35, 206–212. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, H.G.; Kurtulmus-Yilmaz, S.; Cengiz, E. Long-term effect of diode laser irradiation compared to sodium fluoride varnish in the treatment of dentine hypersensitivity in periodontal maintenance patients: A randomized controlled clinical study. Photomed. Laser Surg. 2011, 29, 721–725. [Google Scholar] [CrossRef] [PubMed]
- De Moor, R.J.; Verheyen, J.; Verheyen, P.; Diachuk, A.; Meire, M.A.; De Coster, P.J.; De Bruyne, M.; Keulemans, F. Laser teeth bleaching: Evaluation of eventual side effects on enamel and the pulp and the efficiency in vitro and in vivo. Sci. World J. 2015, 2015, 835405. [Google Scholar] [CrossRef]
- Al-Maliky, M.A.; Frentzen, M.; Meister, J. Artificial Caries Resistance in Enamel after Topical Fluoride Treatment and 445 nm Laser Irradiation. Biomed. Res. Int. 2019, 2019, 9101642. [Google Scholar] [CrossRef] [PubMed]
- Lagdive, S.; Doshi, Y.; Marawar, P. Management of Gingival Hyperpigmentation Using Surgical Blade and Diode Laser Therapy: A Comparative Study. J. Oral Laser Appl. 2009, 9, 208–210. [Google Scholar]
- Pogrel, M.; Muff, D.; Marshall, G. Structural changes in dental enamel induced by high energy continuous wave carbon dioxide laser. Lasers Surg. Med. 1993, 13, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Miglani, S.; Patro, S. Lasers in Implant Dentistry. In Advances in Dental Implantology using Nanomaterials and Allied Technology Applications; Chaughule, R.S., Dashaputra, R., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 225–245. [Google Scholar] [CrossRef]
- George, R. Laser in dentistry-Review. Int. J. Dent. Clin. 2009, 1, 13–19. [Google Scholar]
- Coluzzi, D.; Parker, S. Lasers in Dentistry—Current Concepts; Springer International Publishing: Berlin/Heidelberg, Germany, 2017. [Google Scholar] [CrossRef]
- Belikov, A.V.; Skrypnik, A.V.; Shatilova, K.V. Comparison of diode laser in soft tissue surgery using continuous wave and pulsed modes in vitro. Front. Optoelectron. 2015, 8, 212–219. [Google Scholar] [CrossRef]
- Coluzzi, D.J.; Robert, A. Laser fundamentals. In Principles and Practice of Laser Dentistry; Elsevier: Amsterdam, The Netherlands, 2015; pp. 12–26. [Google Scholar]
- Parker, S. Verifiable CPD paper: Introduction, history of lasers and laser light production. Br. Dent. J. 2007, 202, 21–31. [Google Scholar] [CrossRef] [PubMed]
- Epperlein, P.W. Semiconductor Laser Engineering, Reliability and Diagnostics: A Practical Approach to High Power and Single Mode Devices; John Wiley & Sons: Hoboken, NJ, USA, 2013. [Google Scholar]
- Jiménez, J. Laser diode reliability: Crystal defects and degradation modes. Comptes Rendus Phys. 2003, 4, 663–673. [Google Scholar] [CrossRef]
- Pirnat, S. Versatility of an 810 nm diode laser in dentistry: An overview. J. Laser Health Acad. 2007, 4, 1–9. [Google Scholar]
- Frentzen, M.; Kraus, D.; Reichelt, J.; Engelbach, C.; Dehn, C.; Meister, J. A novel blue light diode laser (445 nm) for dental application Biomedical testing and clinical aspects. Laser Int. Mag. Laser Dent. 2016, 8, 6–13. [Google Scholar]
- Katalinić, I.; Budimir, A.; Bošnjak, Z.; Jakovljević, S.; Anić, I. The photo-activated and photo-thermal effect of the 445/970 nm diode laser on the mixed biofilm inside root canals of human teeth in vitro: A pilot study. Photodiagnosis Photodyn. Ther. 2019, 26, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Klim, J.D.; Fox, D.B.; Coluzzi, D.J.; Neckel, C.P.; Swick, M.D. The diode laser in dentistry. Rev. Wavel. 2000, 8, 13–16. [Google Scholar]
- Dostalova, T.; Jelinkova, H.; Housova, D.; Sulc, J.; Nemec, M.; Miyagi, M.; Junior, A.B.; Zanin, F. Diode laser-activated bleaching. Braz. Dent. J. 2004, 15, SI-3. [Google Scholar]
- Braun, A.; Braun, A.; Kettner, M.; Berthold, M.; Wenzler, J.-S.; Heymann, P.G.B.; Frankenberger, R. Efficiency of soft tissue incision with a novel 445-nm semiconductor laser. Lasers Med. Sci. 2018, 33, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Ibacache, M.C.T.; Arcos, P.; Sanchez, S.; Weinstein, G. Use of diode lasers in dentistry. Clin. Dent. Rev. 2020, 4, 6. [Google Scholar] [CrossRef]
- Ren, C.; McGrath, C.; Jin, L.; Zhang, C.; Yang, Y. The effectiveness of low-level laser therapy as an adjunct to non-surgical periodontal treatment: A meta-analysis. J. Periodontal Res. 2017, 52, 8–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mehuys, D.G. Chapter 4-High-Power Semiconductor Lasers. In Semiconductor Lasers II; Kapon, E., Ed.; Academic Press: San Diego, CA, USA, 1999; pp. 259–321. [Google Scholar]
- Hanke, A.; Fimmers, R.; Frentzen, M.; Meister, J. Quantitative determination of cut efficiency during soft tissue surgery using diode lasers in the wavelength range between 400 and 1500 nm. Lasers Med. Sci. 2021, 36, 1633–1647. [Google Scholar] [CrossRef] [PubMed]
- Beer, F.; Körpert, W.; Passow, H.; Steidler, A.; Meinl, A.; Buchmair, A.G.; Moritz, A. Reduction of collateral thermal impact of diode laser irradiation on soft tissue due to modified application parameters. Lasers Med. Sci. 2012, 27, 917–921. [Google Scholar] [CrossRef]
- de Alencar Mollo, M.; Frigo, L.; Favero, G.M.; Lopes-Martins, R.Á.B.; Junior, A.B. In vitro analysis of human tooth pulp chamber temperature after low-intensity laser therapy at different power outputs. Lasers Med. Sci. 2011, 26, 143–147. [Google Scholar] [CrossRef] [PubMed]
- da Fonseca Alvarez, A.; Davidowicz, H.; Moura-Netto, C.; Frugoli, A.D.; Fernando, C.; Aranha, A.C.C. Temperature changes on the root surfaces of mandibular incisors after an 810-nm high-intensity intracanal diode laser irradiation. J. Biomed. Opt. 2012, 17, 015006. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).