Abstract
Objectives: To compare the objective refraction of young hyperopes obtained by two wavefront autorefractors with identical measurement principles but different optical designs: a monocular closed-field (VX 120) and a binocular open-field (Eye Refract), both developed by the same manufacturer (Visionix; Pont-de-l’Arche, France). Methods: A randomized, cross-sectional study was carried out with 37 hyperopic participants (18.2 ± 7.8 years; range 8 to 31 years). Each participant underwent two measurement sessions (one with and one without cycloplegia), during which three measurements were taken per autorefractor (monocular and binocular). Refractive variables (M, J0, and J45) were analyzed in one randomly selected eye. Results: The spherical equivalent (M) showed significant differences between autorefractors under noncycloplegic and cycloplegic conditions (p < 0.001). Without cycloplegia, the binocular autorefractor measured +0.45 (+1.49, −0.58) D more hyperopia than the monocular device. Under cycloplegia, this difference decreased to +0.26 D (+0.99, −0.48) D. Both autorefractors provided higher hyperopia with cycloplegia, with differences inversely correlated with age (r = −0.4; p < 0.05). Conclusions: Whenever possible, refraction in young hyperopes should be measured under cycloplegic conditions using a binocular open-field autorefractor to promote greater accommodative relaxation and ensure more reliable hyperopia measurements in both clinical practice and research.
1. Introduction
Autorefraction enables the objective measurement of ocular refraction and serves as an initial point for the subsequent subjective refraction performed by the optometrist [1]. Since the introduction of the first autorefractors in the 1980s, these devices have undergone significant development, resulting in a wide variety of instruments that differ in measurement principles and fixation target types.
Based on the measurement principle, autorefractors can be classified as traditional, relying on the Scheiner or retinoscopy principles [2,3], or as wavefront devices, which are aberrometers [4,5]. The distinction between monocular and binocular devices refers to whether measurements are performed under binocular viewing conditions or not. Similarly, a closed- or open-field design refers to if the fixation target is integrated into the device or positioned externally, respectively [2,3,4,5].
A key limitation of autorefractors in determining objective refraction is the tendency to overestimate myopia or underestimate hyperopia due to accommodative response during measurement, which primarily affects devices with a monocular closed-field design [6,7,8]. To a lesser extent, this limitation also affected binocular open-field autorefractors, even though they were developed to minimize these errors in objective refraction measurement caused by accommodation [9,10,11].
In individuals where accommodation may interfere with the accurate measurement of refraction, particularly in pediatric populations and young hyperopes, the use of cycloplegia is often indicated. Hyperopes, notably when their hyperopia is uncorrected or undercorrected [12], require greater accommodative effort for both distance and near tasks, which increases accommodative convergence, particularly in cases of high hyperopia [13]. This sustained accommodative demand can also trigger ciliary muscle fluctuations and spasms, contributing to latent hyperopia and, consequently, to an underestimation of the true refractive error [14].
Despite several studies suggesting that objective refraction under cycloplegia can be effective in estimating refractive error without the need for subjective refinement [2,3,4,15], little attention has been paid to the influence of autorefractor design on this efficacy. In this regard, the current study aimed to compare the objective refraction of young hyperopes obtained by two wavefront autorefractors with identical measurement principles but different optical designs: one with a monocular closed-field design (VX 120) and the other with a binocular open-field design (Eye Refract), both developed by the same manufacturer (Visionix; Pont-de-l’Arche, France).
These autorefractors had previously been compared in a general population of 99 individuals aged 8 to 69 years, but without cycloplegia. In that study, conducted by our research group, the monocular closed-field device showed spherical equivalent values that were 0.20 D more myopic than those obtained with the binocular open-field autorefractor, highlighting a greater influence of accommodation in the monocular design [5]. Based on this, the present study hypothesized that, even under cycloplegia, the binocular open-field autorefractor would provide more hyperopic measurements than the monocular closed-field device.
2. Materials and Methods
2.1. Study Design
An experimental, cross-sectional, and randomized study was carried out in which each participant underwent two measurement sessions on different days within the same week: one in a physiological state without cycloplegia and another with cycloplegia. The order of these two sessions was randomly assigned.
During each session, three measurements were taken using the monocular autorefractometer VX 120 (Visionix; Pont-de-l’Arche, France), and three more using the binocular autorefractometer Eye Refract (Visionix). The mean of each set of three measurements was used for statistical analysis. The order of the two autorefractometers was also randomized. The same optometrist carried out all measurements.
Two drops of 1% cyclopentolate hydrochloride (Alcon Cusí; Barcelona, Spain) were topically instilled to induce cycloplegia, with a 15 min interval between them. Measurements with both autorefractometers were taken 15 min after the final instillation. A 1% concentration of cyclopentolate was selected, with a dosage of two instillations, as this is the most commonly used regimen in the scientific literature [12]. No topical anesthesia was used prior to the instillation of cyclopentolate.
All measurement sessions were conducted at the University Clinic of Optometry of the Complutense University of Madrid (Madrid, Spain). Participation was voluntary, and all subjects signed a written informed consent form (signed by the legal guardians when participants were minors), which detailed all procedures performed. The study was approved by the Research Ethics Committee of Hospital Clínico San Carlos (code 18/459-R_P; Madrid, Spain) and was conducted in accordance with Good Clinical Practice guidelines, institutional Spanish and European regulations, and the principles of the Declaration of Helsinki.
2.2. Participants
Out of 48 participants initially assessed, 37 were ultimately included in the study (mean age: 18.2 ± 7.8 years; range: 8 to 31 years; 28 female and 9 male). The results from the participants’ right eyes were selected for statistical analysis.
The study included individuals who met the following conditions: age between 6 and 35 years (to avoid participants with presbyopic symptoms, as their accommodative function might be compromised), a spherical equivalent between +0.75 D and +6.00 D under cycloplegia with at least one of the two autorefractometers, and the ability to understand the testing procedures.
Participants were excluded if they had a clinical history of amblyopia, strabismus, or other binocular vision disorders, as well as in cases of ocular disease, previous eye surgery or trauma, or the use of systemic or ocular medications that could affect accommodation.
All participants were registered in the database of the University Clinic of Optometry and were previously evaluated by different staff optometrists, who confirmed the absence of any accommodative and/or vergence dysfunction prior to their inclusion in the study.
2.3. Wavefront Autorefraction
The VX 120 system (monocular autorefractometer) is a multi-diagnostic instrument that includes a monocular closed-field aberrometer. This aberrometer is equipped with a Hartmann–Shack sensor that performs refraction measurements individually for each eye in a sequential manner. The Hartmann–Shack sensor uses near-infrared light with a wavelength of 800 nm and analyzes up to 1500 refractive points when the pupil diameter is 7 mm. Measurements were performed according to the manufacturer’s instructions, with participants instructed to place their chin and forehead on the support and to fixate on a virtual image (a hot air balloon at the end of a long straight road) located at optical infinity.
On the other hand, the Eye Refract system (binocular autorefractometer) is a binocular open-field aberrometer integrated with a phoropter. It incorporates two Hartmann–Shack sensors that simultaneously perform objective refraction in both eyes. These sensors also use near-infrared light with a wavelength of 800 nm, and the microlens array has a pitch of 0.1 mm. Measurements were also performed following the manufacturer’s guidelines, instructing participants to position their chin and forehead on the appropriate support and to fixate on a digital target (a hot air balloon at the end of a long straight road) placed at a distance of 4 m. To compensate for the accommodative demand of 0.25 D that the Eye Refract may induce by placing the fixation target at 4 m, the instrument performs the measurement under fogging conditions using plus lenses.
Because the Eye Refract combines an aberrometer with a phoropter, it can provide both objective and subjective refraction. In this regard, a previous study conducted by our research group evaluated the system’s effectiveness in performing automated subjective refraction, comparing its outcomes with those obtained by conventional subjective refraction performed by an optometrist [16]. Therefore, only the results related to objective refraction are reported in the present study.
Objective refraction with both autorefractometers is determined by the manufacturer through wavefront analysis using the equivalent quadratic method, based on the paraxial curvature matching approach proposed by Thibos et al. [17]. This analysis is limited in both instruments to higher-order aberrations up to the fourth order, using Zernike coefficients C20 (defocus) and C40 (spherical aberration) to calculate the spherical equivalent (M), C22 (vertical astigmatism) and C42 (vertical secondary astigmatism) for the vertical astigmatism component (J0), and C2−2 (oblique astigmatism) and C4−2 (oblique secondary astigmatism) for the oblique astigmatism component (J45). Measurements were taken under physiological pupil conditions, but both systems automatically recalculated the refractive values for a standardized pupil diameter of 3 mm. None of the participants had a pupil diameter smaller than 3 mm.
Refraction data from both wavefront autorefractometers were obtained in terms of sphere and cylinder and were subsequently analyzed using the vectorial representation standardized by Thibos et al. [18], which considers the refractive variables M, J0, and J45. The formulas used for the calculations were as follows:
M = sphere + (cylinder/2),
J0 = −(cylinder/2) × cos(2 × axis),
J45 = −(cylinder/2) × sin(2 × axis).
2.4. Statistical Analysis
Statistical analyses were performed with SPSS Statistics software version 23 (IBM, Chicago, IL, USA). The normal distribution of each variable was evaluated using the Shapiro–Wilk test. Upon confirmation of normality, a one-way repeated-measures ANOVA with Bonferroni correction was applied to compare the different autorefraction methods (noncycloplegic monocular, noncycloplegic binocular, cycloplegic monocular, and cycloplegic binocular).
The agreement between the different autorefraction methods was assessed by means of Bland–Altman plots [19], which examined the mean difference along with the 95% limits of agreement (LoA), calculated as ±1.96 times the standard deviation of the differences. Furthermore, the Pearson correlation coefficient (r) was computed to explore the association between participants’ age and the mean differences observed between methods.
The variables analyzed included M, J0, and J45. Results are presented as mean ± standard deviation. Statistical significance was set at p < 0.05 for all analyses.
3. Results
The mean values of the refractive variables obtained with the two wavefront autorefractometers, both with and without cycloplegia, along with the statistical comparisons between the different measurements, are presented in Table 1 and Table 2.

Table 1.
Mean values and standard deviations of the spherical equivalent (M) and cylindrical components (J0 and J45) obtained using the different autorefraction methods.

Table 2.
Statistical comparisons between the different autorefraction methods for the spherical equivalent (M) and cylindrical components (J0 and J45).
The spherical equivalent (M) was the only variable that showed statistically significant differences between the different autorefraction methods (p < 0.05). Accordingly, Figure 1 presents the Bland–Altman plots for M, detailing the mean differences observed between these methods, as well as the 95% LoA (upper, lower). Without cycloplegia, the binocular autorefractometer yielded hyperopia values that were +0.45 (95% LoA: +1.49, −0.58) D higher than those obtained with the monocular device (p < 0.001). However, under cycloplegia, the binocular autorefractometer continued to produce more positive values than the monocular autorefractometer (p = 0.001), although the difference was reduced to +0.26 (95% LoA: +0.99, −0.48) D.
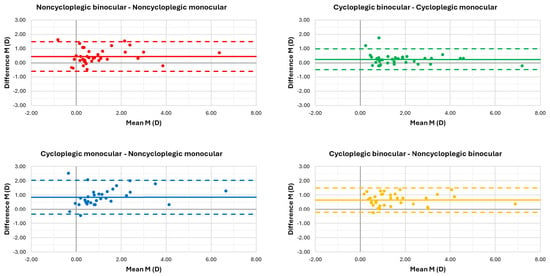
Figure 1.
Bland–Altman plots of the spherical equivalent (M) illustrating the agreement between the different autorefraction methods. The solid central line represents the mean difference, and the dashed lines indicate the 95% limits of agreement.
On the other hand, when comparing the M values with and without cycloplegia obtained using the monocular autorefractometer, hyperopia was found to be +0.85 (95% LoA: +2.06, −0.35) D higher under cycloplegic conditions (p < 0.001). When the same comparison was made using the binocular autorefractometer, measurements with cycloplegia also showed more positive hyperopia values compared to those without cycloplegia (p < 0.001). However, this difference was reduced to +0.65 (95% LoA: +1.51, −0.20) D.
It is important to note that, under cycloplegic conditions, the binocular autorefractometer demonstrated the highest hyperopia values compared to all other autorefraction methods (p < 0.001).
Figure 2 and Figure 3 show the Bland–Altman plots for the cylindrical components J0 and J45, respectively. Notably, no statistically significant differences were reported between the monocular and binocular autorefractometers, regardless of the use of cycloplegia (p ≥ 0.05). Similarly, for both autorefractometers, the results obtained under cycloplegia were comparable to those obtained without cycloplegia (p > 0.05). Despite no statistically significant differences being found, it should be noted that both J0 and J45 values were higher with the monocular autorefractor under cycloplegia.
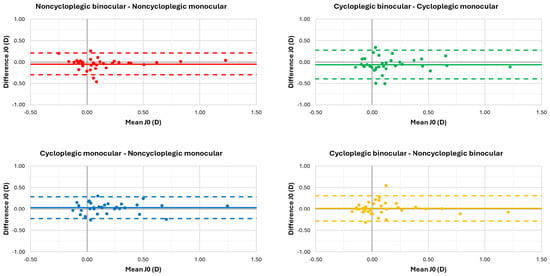
Figure 2.
Bland–Altman plots of the vertical cylindrical component (J0) illustrating the agreement between the different autorefraction methods. The solid central line represents the mean difference, and the dashed lines indicate the 95% limits of agreement.
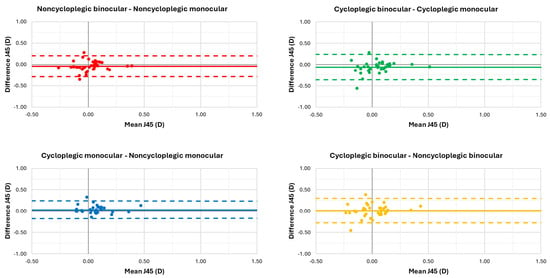
Figure 3.
Bland–Altman plots of the oblique cylindrical component (J45) illustrating the agreement between the different autorefraction methods. The solid central line represents the mean difference, and the dashed lines indicate the 95% limits of agreement.
Finally, the scatter plots and linear correlation analyses between participants’ age and the mean differences among the different autorefraction methods are shown in Figure 4. M was the only variable that exhibited statistically significant correlations. For both the monocular and binocular autorefractometers, the differences in M between cycloplegic and noncycloplegic conditions showed a low but significant inverse correlation with participants’ age. The Pearson correlation coefficients (r) were −0.42 for the monocular autorefractometer (p = 0.009) and −0.38 for the binocular autorefractometer (p = 0.019).
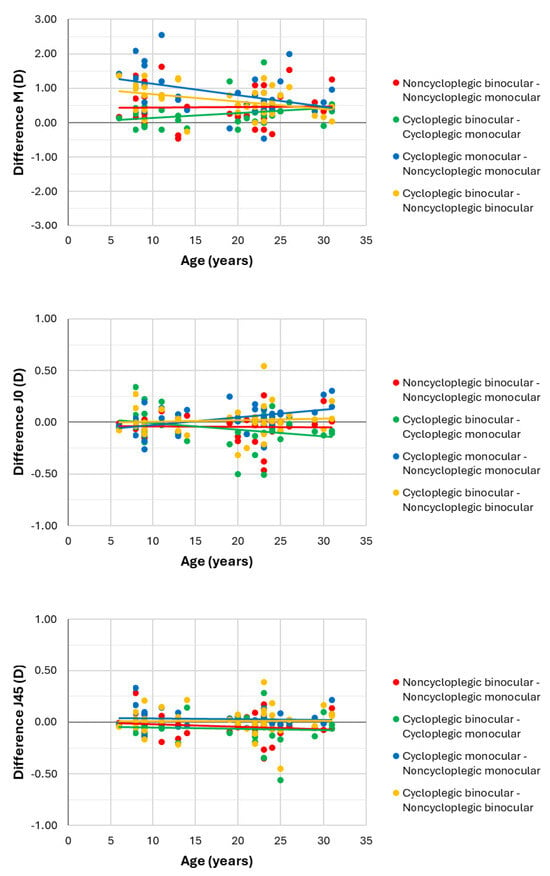
Figure 4.
Scatter plots and linear correlation analyses between participants’ age and the mean differences among the different autorefraction methods for the spherical equivalent (M) and cylindrical components (J0 and J45). In terms of M, the Pearson correlation coefficients (r) were −0.42 for the monocular autorefractometer (p = 0.009; blue line) and −0.38 for the binocular autorefractometer (p = 0.019; yellow line).
4. Discussion
The present study is, as far as we know, the first to investigate the isolated effect of the optical design of autorefractors (monocular closed-field vs. binocular open-field) on the cycloplegic refraction of young hyperopes. Unlike many recent studies that already compared refractive outcomes among autorefractors with different optical designs and measurement principles [20,21,22,23,24], the present study used two wavefront autorefractors developed by the same manufacturer. This implies that both the measurement principle (aberrometry) and the subsequent analysis metric, based on the paraxial curvature matching approach [17], were the same in both devices. In this way, the optical design effect of the two autorefractors on objective refraction could be isolated, minimizing the comparative bias that arises between instruments that, despite having a similar design, use different measurement principles or analysis metrics [25,26,27].
The monocular and binocular autorefractors used in the present study to assess young hyperopes under cycloplegia had already been compared in a previous study by our research group, conducted in a general population aged 8 to 69 years but without cycloplegia [5]. That earlier study found that the monocular autorefractor provided mean M values that were 0.20 D more myopic than those obtained with the binocular autorefractor. This suggests that the monocular design may induce greater accommodative stimulation, likely because the binocular cues that help relax accommodation (such as vergence and binocular disparity) are absent, potentially leading to increased accommodation during the refraction measurement. It also ruled out that these differences were due to factors such as the wavelength of the wavefront sensors or accommodative convergence [5]. Regarding the young hyperopes in the present study, this effect was magnified, as the monocular autorefractor underestimated the participants’ hyperopia under noncycloplegic conditions by 0.45 D compared to the binocular autorefractor (see Figure 1). The greater accommodative stimulation observed in hyperopes during the measurement process may be associated with a higher sustained accommodative demand over time, potentially leading to ciliary muscle spasms and fluctuations, and ultimately causing an underestimation of hyperopia [12,14]. In line with these findings, several studies conducted in children under noncycloplegic conditions demonstrated that monocular closed-field autorefractors stimulated accommodation more than binocular open-field designs, leading to an overestimation of myopia or underestimation of hyperopia by 0.13 D to 0.63 D, depending on the instruments compared [20,22,23].
While the use of cycloplegia for measuring objective refraction has been proposed in various studies as an effective alternative to subjective refinement performed by the optometrist [2,3,4,15], it remains unclear whether this procedure is valid for all autorefractors, regardless of their design. In this regard, the present study found that, even under cycloplegia, the monocular autorefractor produced mean hyperopia values that were 0.26 D lower compared to the binocular design, a clinically relevant difference, as it exceeds the 0.25 D threshold typically considered the minimum significant change in spherical power. This suggests that, despite cycloplegia, young hyperopes may preserve some accommodative response stimulated by the monocular closed-field design, which is minimized in a binocular open-field environment. Several recent studies conducted in children confirmed that binocular open-field autorefractors seem to achieve greater accommodation relaxation even under cycloplegia [20,21,22,23,24]. This is based on the fact that, under these conditions, some monocular closed-field autorefractor models also overestimated myopia or underestimated hyperopia by between 0.08 D and 0.32 D compared to binocular open-field designs [20,21,22,23,24]. The only exception to this was reported in a study by Rosenfield and Ciuffreda [20], in which a handheld wavefront autorefractor measured 0.17 D less myopic refraction compared to a binocular open-field device and subjective refraction, and no hypothesis was offered to explain this finding.
Given that subjective refraction performed by an optometrist is the reference standard for measuring refractive error [1], it is also relevant to question the efficacy of the two wavefront autorefractors evaluated in the present work in comparison to this standard. In a recent study performed by our research group, the results of the subjective refraction, based on an initial retinoscopy, carried out on the present sample were partially reported [16]. In these young hyperopes, the mean value of M for noncycloplegic subjective refraction was 1.05 ± 0.86 D, which was higher than the values obtained with the monocular autorefractor but lower than those measured by the binocular device (see Table 1), but these differences were not statistically significant (p ≥ 0.05). Under cycloplegia, however, the binocular autorefractor showed significantly higher hyperopia values (p = 0.039) compared to the subjective refraction, which had a mean M value of 1.74 ± 1.40 D. These findings indicate that the binocular open-field autorefractor under cycloplegia provided the highest hyperopia values, suggesting that this type of design may promote greater accommodative relaxation during refractive error measurement.
Regarding the influence of age on the measurement of M, it is worth noting that the differences observed between noncycloplegic and cycloplegic refractions with both autorefractors were inversely correlated with participants’ age (see Figure 4). This would indicate that younger hyperopes are more likely to experience accommodative stimulation when their refractive error is measured without cycloplegia, resulting in an underestimation of their hyperopia. However, the strength of these correlations was low for both autorefractors (r ≈ 0.40), so this finding cannot be generalized to all cases. Nonetheless, it remains a clinically relevant consideration. In line with this, a previous study by our research group comparing both autorefractors in a general population under noncycloplegic conditions also showed that accommodative stimulation may occur in isolated cases of myopic children, particularly when using the monocular autorefractor [5].
Thus far, this discussion has focused on the results for M, since neither of the vector components of astigmatism (J0 and J45) showed significant differences between the autorefractors, either with or without cycloplegia (see Table 2). The fact that both devices exhibited differences in M but not in astigmatism suggests that accommodative stimulation induced by these instruments does not affect cylinder measurements, as previously confirmed in our comparison of these two autorefractors in a general population [5]. Overall, most studies in the scientific literature agree that autorefractors are quite reliable for measuring astigmatism, regardless of the type of refractive error, the subject’s age, or the device’s design and measurement principle [3,7,8,20,21,22,23,24,28,29,30,31].
The main limitation of this study, which is shared with other investigations evaluating different refraction methods under cycloplegia, is the use of a single cycloplegic agent (1% cyclopentolate hydrochloride) administered using a single dosing protocol (two drops instilled 15 min apart). The use of alternative agents or dosing regimens could provide further insight into the optimal combination for assessing objective refraction, particularly considering that many of these studies, including the present one, consistently showed some degree of accommodative stimulation under cycloplegic conditions, which primarily affects measurements obtained with monocular closed-field autorefractors [20,21,22,23,24]. Moreover, the use of only two wavefront autorefractors in this study, although it allowed for the isolated assessment of the effect of optical design on refractive error measurement, highlights that the findings cannot be extrapolated to all commercially available autorefractors, particularly given the wide variety of designs and measurement principles they exhibit. Finally, it should be noted that this study did not take the gender dimension into account, as it included 28 female and 9 male participants.
5. Conclusions
In addition to both wavefront autorefractors providing higher hyperopia values under cycloplegia, the binocular open-field autorefractor provided greater hyperopia measurements than the monocular closed-field device both with and without cycloplegia. These findings suggest that, whenever possible, refraction in young hyperopes should be measured under cycloplegic conditions using a binocular open-field autorefractor to promote greater accommodative relaxation and ensure more reliable hyperopia measurements in both clinical practice and research.
Author Contributions
Conceptualization, G.C. and C.C.-T.; methodology, G.C. and C.C.-T.; investigation, C.C.-T., C.P. and M.R.-L.; resources, A.P.-A., M.S. and L.B.; writing—original draft preparation, C.C.-T.; writing—review and editing, G.C., C.P., M.R.-L., A.P.-A., M.S. and L.B.; supervision, G.C.; project administration, G.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was approved by the Research Ethics Committee of Hospital Clínico San Carlos (code 18/459-R_P; date of approval: 16 November 2018) and was conducted in accordance with Good Clinical Practice guidelines, institutional Spanish and European regulations, and the principles of the Declaration of Helsinki.
Informed Consent Statement
Participation was voluntary, and all subjects signed a written informed consent form (signed by legal guardians in the case of minors), which detailed all procedures performed.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on reasonable request.
Conflicts of Interest
Gonzalo Carracedo received a personal grant from Visionix (Pont-de-l’Arche, France) for the performance of the study. The authors declare no conflicts of interest.
References
- Elliott, D.B. What is the appropriate gold standard test for refractive error? Ophthalmic Physiol. Opt. 2017, 37, 115–117. [Google Scholar] [CrossRef]
- Cleary, G.; Spalton, D.J.; Patel, P.M.; Lin, P.F.; Marshall, J. Diagnostic accuracy and variability of autorefraction by the Tracey Visual Function Analyzer and the Shin-Nippon NVision-K 5001 in relation to subjective refraction. Ophthalmic Physiol. Opt. 2009, 29, 173–181. [Google Scholar] [CrossRef]
- McGinnigle, S.; Naroo, S.A.; Eperjesi, F. Evaluation of the auto-refraction function of the Nidek OPD-Scan III. Clin. Exp. Optom. 2014, 97, 160–163. [Google Scholar] [CrossRef] [PubMed]
- Gordon-Shaag, A.; Pinero, D.P.; Kahloun, C.; Markov, D.; Parnes, T.; Gantz, L.; Shneor, E. Validation of refraction and anterior segment parameters by a new multi-diagnostic platform (VX120). J. Optom. 2018, 11, 242–251. [Google Scholar] [CrossRef] [PubMed]
- Carracedo, G.; Carpena-Torres, C.; Batres, L.; Serramito, M.; Gonzalez-Bergaz, A. Comparison of Two Wavefront Autorefractors: Binocular Open-Field versus Monocular Closed-Field. J. Ophthalmol. 2020, 2020, 8580471. [Google Scholar] [CrossRef] [PubMed]
- Nissman, S.A.; Tractenberg, R.E.; Saba, C.M.; Douglas, J.C.; Lustbader, J.M. Accuracy, repeatability, and clinical application of spherocylindrical automated refraction using time-based wavefront aberrometry measurements. Ophthalmology 2006, 113, 577.e571–577.e572. [Google Scholar] [CrossRef]
- Reinstein, D.Z.; Archer, T.J.; Couch, D. Accuracy of the WASCA aberrometer refraction compared to manifest refraction in myopia. J. Refract. Surg. 2006, 22, 268–274. [Google Scholar] [CrossRef]
- Zhu, X.; Dai, J.; Chu, R.; Lu, Y.; Zhou, X.; Wang, L. Accuracy of WASCA aberrometer refraction compared to manifest refraction in Chinese adult myopes. J. Refract. Surg. 2009, 25, 1026–1033. [Google Scholar] [CrossRef]
- Choong, Y.F.; Chen, A.H.; Goh, P.P. A comparison of autorefraction and subjective refraction with and without cycloplegia in primary school children. Am. J. Ophthalmol. 2006, 142, 68–74. [Google Scholar] [CrossRef]
- Queiros, A.; Gonzalez-Meijome, J.; Jorge, J. Influence of fogging lenses and cycloplegia on open-field automatic refraction. Ophthalmic Physiol. Opt. 2008, 28, 387–392. [Google Scholar] [CrossRef]
- Mallen, E.A.; Gilmartin, B.; Wolffsohn, J.S.; Tsujimura, S. Clinical evaluation of the Shin-Nippon SRW-5000 autorefractor in adults: An update. Ophthalmic Physiol. Opt. 2015, 35, 622–627. [Google Scholar] [CrossRef]
- Yazdani, N.; Sadeghi, R.; Momeni-Moghaddam, H.; Zarifmahmoudi, L.; Ehsaei, A. Comparison of cyclopentolate versus tropicamide cycloplegia: A systematic review and meta-analysis. J. Optom. 2018, 11, 135–143. [Google Scholar] [CrossRef]
- Babinsky, E.; Candy, T.R. Why do only some hyperopes become strabismic? Investig. Ophthalmol. Vis. Sci. 2013, 54, 4941–4955. [Google Scholar] [CrossRef]
- Wilson, S.; Ctori, I.; Shah, R.; Suttle, C.; Conway, M.L. Systematic review and meta-analysis on the agreement of non-cycloplegic and cycloplegic refraction in children. Ophthalmic Physiol. Opt. 2022, 42, 1276–1288. [Google Scholar] [CrossRef]
- Sheppard, A.L.; Davies, L.N. Clinical evaluation of the Grand Seiko Auto Ref/Keratometer WAM-5500. Ophthalmic Physiol. Opt. 2010, 30, 143–151. [Google Scholar] [CrossRef]
- Carracedo, G.; Carpena-Torres, C.; Pastrana, C.; Rodríguez-Lafora, M.; Serramito, M.; Privado-Aroco, A.; Espinosa-Vidal, T.M. Accuracy and precision of automated subjective refraction in young hyperopes under cycloplegia. J. Optom. 2023, 16, 252–260. [Google Scholar] [CrossRef]
- Thibos, L.N.; Hong, X.; Bradley, A.; Applegate, R.A. Accuracy and precision of objective refraction from wavefront aberrations. J. Vis. 2004, 4, 329–351. [Google Scholar] [CrossRef]
- Thibos, L.N.; Wheeler, W.; Horner, D. Power vectors: An application of Fourier analysis to the description and statistical analysis of refractive error. Optom. Vis. Sci. 1997, 74, 367–375. [Google Scholar] [CrossRef] [PubMed]
- Bland, J.M.; Altman, D.G. Measuring agreement in method comparison studies. Stat. Methods Med. Res. 1999, 8, 135–160. [Google Scholar] [CrossRef] [PubMed]
- Rosenfield, M.; Ciuffreda, K.J. Evaluation of the SVOne Handheld Autorefractor in a Pediatric Population. Optom. Vis. Sci. 2017, 94, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Ying, G.S.; Maguire, M.G.; Kulp, M.T.; Ciner, E.; Moore, B.; Pistilli, M.; Candy, R. Comparison of cycloplegic refraction between Grand Seiko autorefractor and Retinomax autorefractor in the Vision in Preschoolers-Hyperopia in Preschoolers (VIP-HIP) Study. J. AAPOS 2017, 21, 219–223.e213. [Google Scholar] [CrossRef]
- Kuo, Y.C.; Wang, J.H.; Chiu, C.J. Comparison of open-field autorefraction, closed-field autorefraction, and retinoscopy for refractive measurements of children and adolescents in Taiwan. J. Formos. Med. Assoc. 2020, 119, 1251–1258. [Google Scholar] [CrossRef]
- Guo, R.; Shi, L.; Xu, K.; Hong, D. Clinical evaluation of autorefraction and subjective refraction with and without cycloplegia in Chinese school-aged children: A cross-sectional study. Transl. Pediatr. 2022, 11, 933–946. [Google Scholar] [CrossRef]
- Lei, Y.; Chen, X.; Cheng, M.; Li, B.; Jiang, Y.; Xu, Y.; Wang, X. Comparisons of objective and subjective refraction with and without cycloplegia using binocular wavefront optometer with autorefraction and retinoscopy in school-age children. Graefes Arch. Clin. Exp. Ophthalmol. 2023, 261, 1465–1472. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, H.R.; Svarverud, E.; Hagen, L.A.; Gilson, S.J.; Baraas, R.C. Comparing ocular biometry and autorefraction measurements from the Myopia Master with the IOLMaster 700 and the Huvitz HRK-8000A autorefractor. Ophthalmic Physiol. Opt. 2023, 43, 410–417. [Google Scholar] [CrossRef] [PubMed]
- de Castro Neto, F.C.; Louzada, R.N.; Dantas, D.O.; Amaral, D.C.; Chaves Filho, C.D.C.; Alves, M.R. Evaluation of Portable, Low-Cost Autorefractor in School Students with Limited Eye Care Access in Northeastern Brazil. Vision 2025, 9, 17. [Google Scholar] [CrossRef]
- Calvo-Maroto, A.M.; Llorente-González, S.; Bezunartea-Bezunartea, J.; Hurtado-Ceña, F.J.; Berrozpe-Villabona, C.; Bilbao-Malavé, V.; Piñero, D.P.; Barrio-Barrio, J.; Recalde-Maestre, S. Comparative Study of Refraction between Wave Front-Based Refraction and Autorefraction without and with Cycloplegia in Children and Adolescents. Children 2022, 9, 88. [Google Scholar] [CrossRef]
- Salmon, T.O.; West, R.W.; Gasser, W.; Kenmore, T. Measurement of refractive errors in young myopes using the COAS Shack-Hartmann aberrometer. Optom. Vis. Sci. 2003, 80, 6–14. [Google Scholar] [CrossRef]
- Cooper, J.; Citek, K.; Feldman, J.M. Comparison of refractive error measurements in adults with Z-View aberrometer, Humphrey autorefractor, and subjective refraction. Optometry 2011, 82, 231–240. [Google Scholar] [CrossRef]
- Shneor, E.; Millodot, M.; Avraham, O.; Amar, S.; Gordon-Shaag, A. Clinical evaluation of the L80 autorefractometer. Clin. Exp. Optom. 2012, 95, 66–71. [Google Scholar] [CrossRef] [PubMed]
- Lebow, K.A.; Campbell, C.E. A comparison of a traditional and wavefront autorefraction. Optom. Vis. Sci. 2014, 91, 1191–1198. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).