A Rapid and Convenient Procedure to Evaluate Optical Performance of Intraocular Lenses
Abstract
:1. Introduction
2. Methods
2.1. Lenses
| Lens name, manufacturer | ACRI.TEC 44S, Surgicon Healthcare | TECNIS ASPHERIS ZCB00, Abbott Medical Optics | CT SPHERIS 204, Zeiss Meditec | CT ASPHERIS 509M, Zeiss Meditec | CT ASPHINA 509M, Zeiss Meditec | SN60WF, Alcon Pharma | DOMICRYL 677AB, Polytech-Domilens GmbH |
|---|---|---|---|---|---|---|---|
| Base power | +21.0D | +21.0D | +21.0D | +21.0D | +21.0D | +21.0D | +21.0D |
| Near add | none | none | none | none | none | none | None |
| Short name used in Figures | ACRITEC | TECNIS ASPH | SPHERIS | ASPHERIS | ASPHINA | ALCON +21 | DOMILENS |
| Lens name, manufacturer | AT LISA 809M, Zeiss Meditec | TECNIS ZMB00, Abbott Medical Optics | SN6AD3, Alcon Pharma | SN6AD1, Alcon Pharma |
|---|---|---|---|---|
| Base power | +21.0D | +21.0D | +21.0D | +21.0D |
| Near add | +3.75D | +4.00D | +4.0D | +3.0D |
| Short name used in Figures | LISA | TECNIS MULT | ALCON +21 +4 | ALCON +21 +3 |
2.2. Hardware of the Lens Scanner
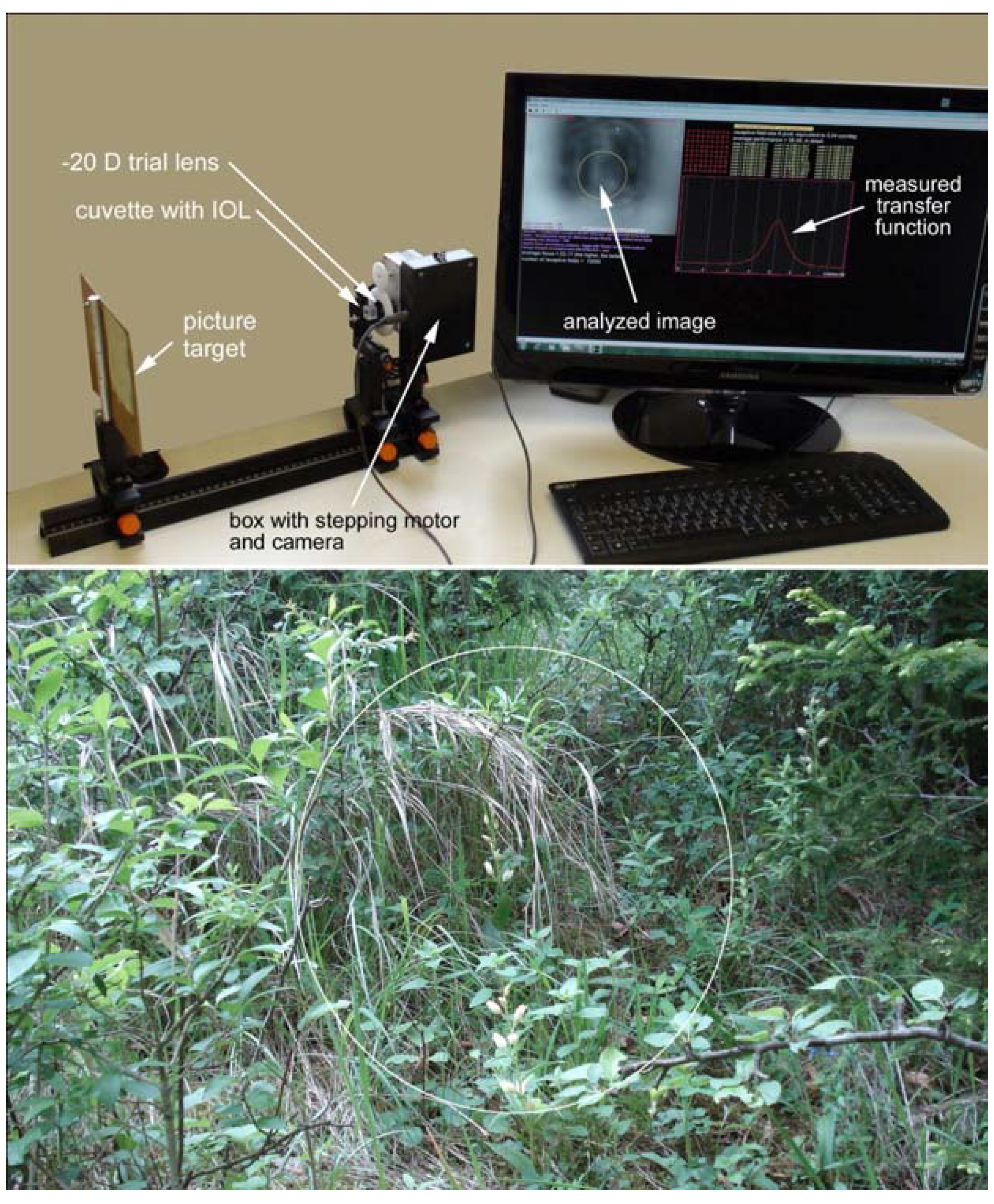
2.3. Image Processing and Software

2.4. Calibration of the System

3. Results
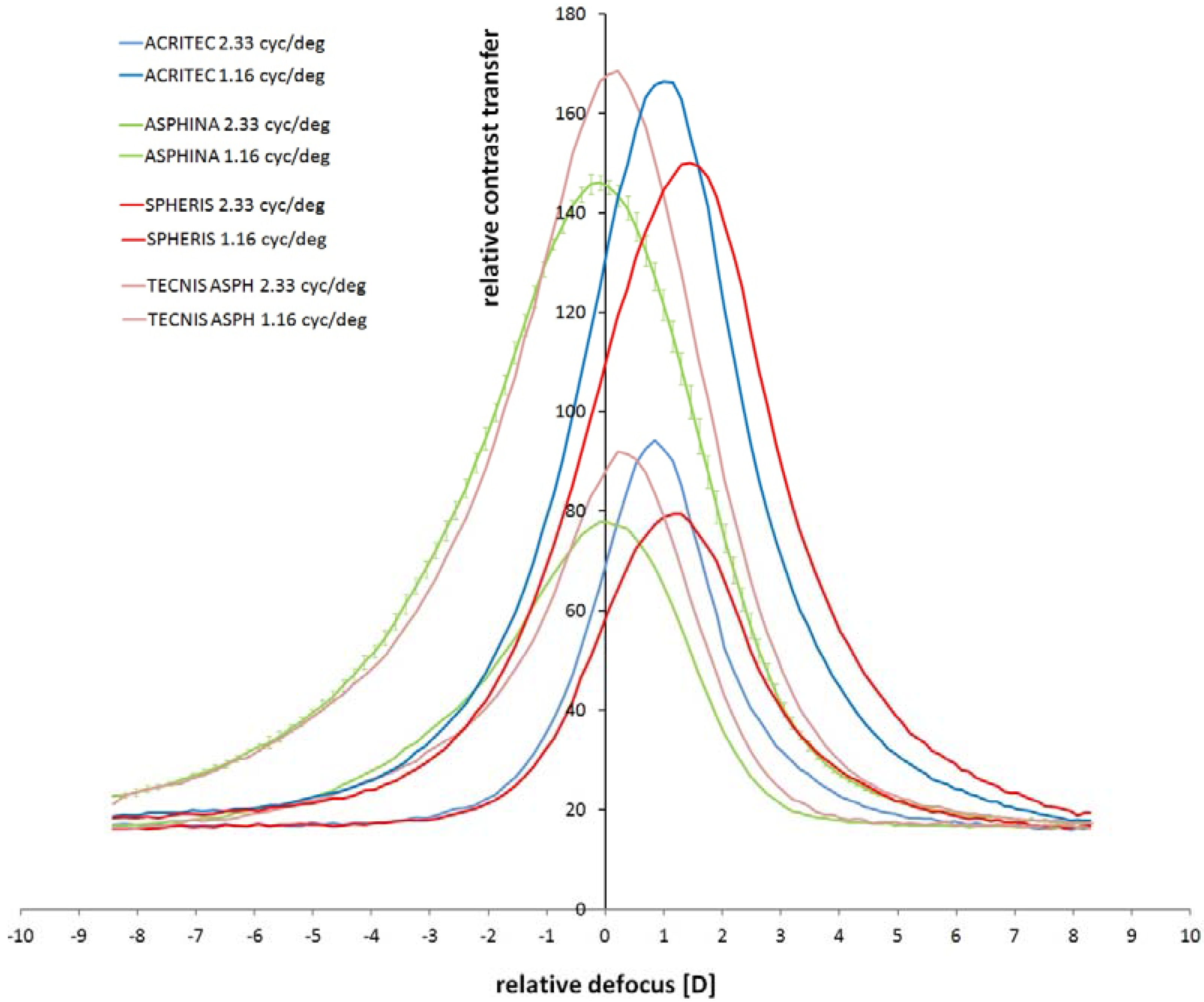
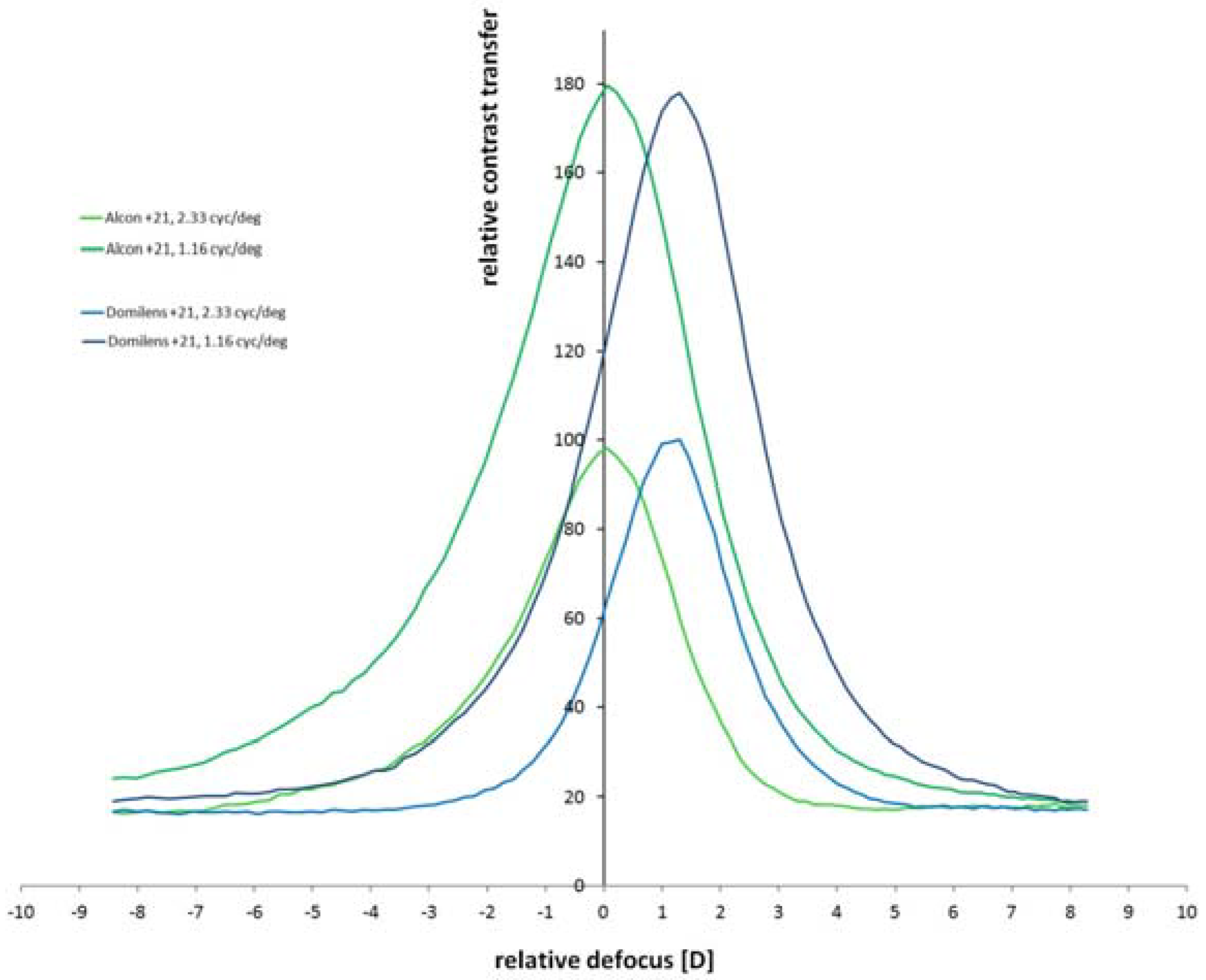
3.1. Measurement of Monofocal Lenses
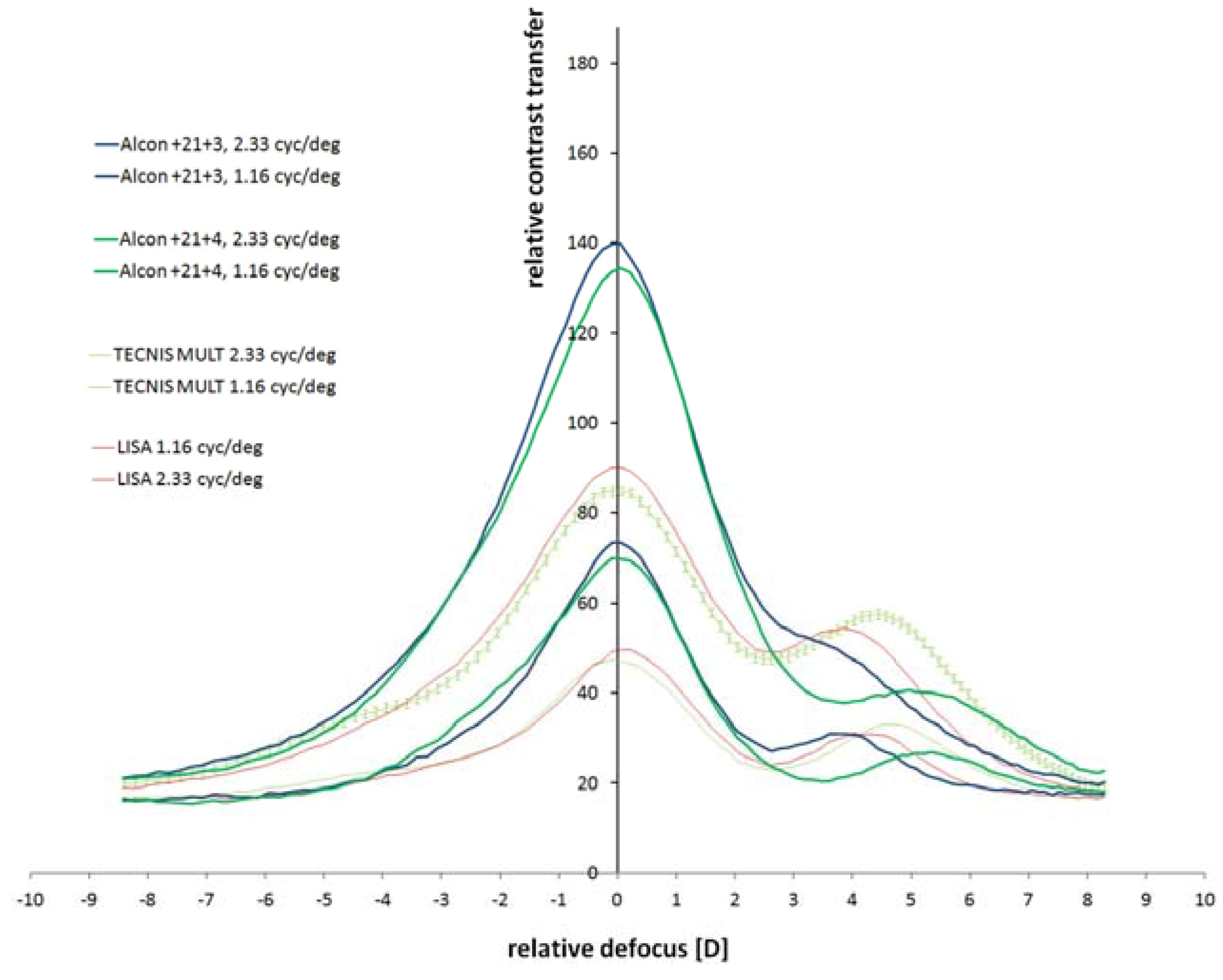
3.2. Measurement of Multifocal Lenses
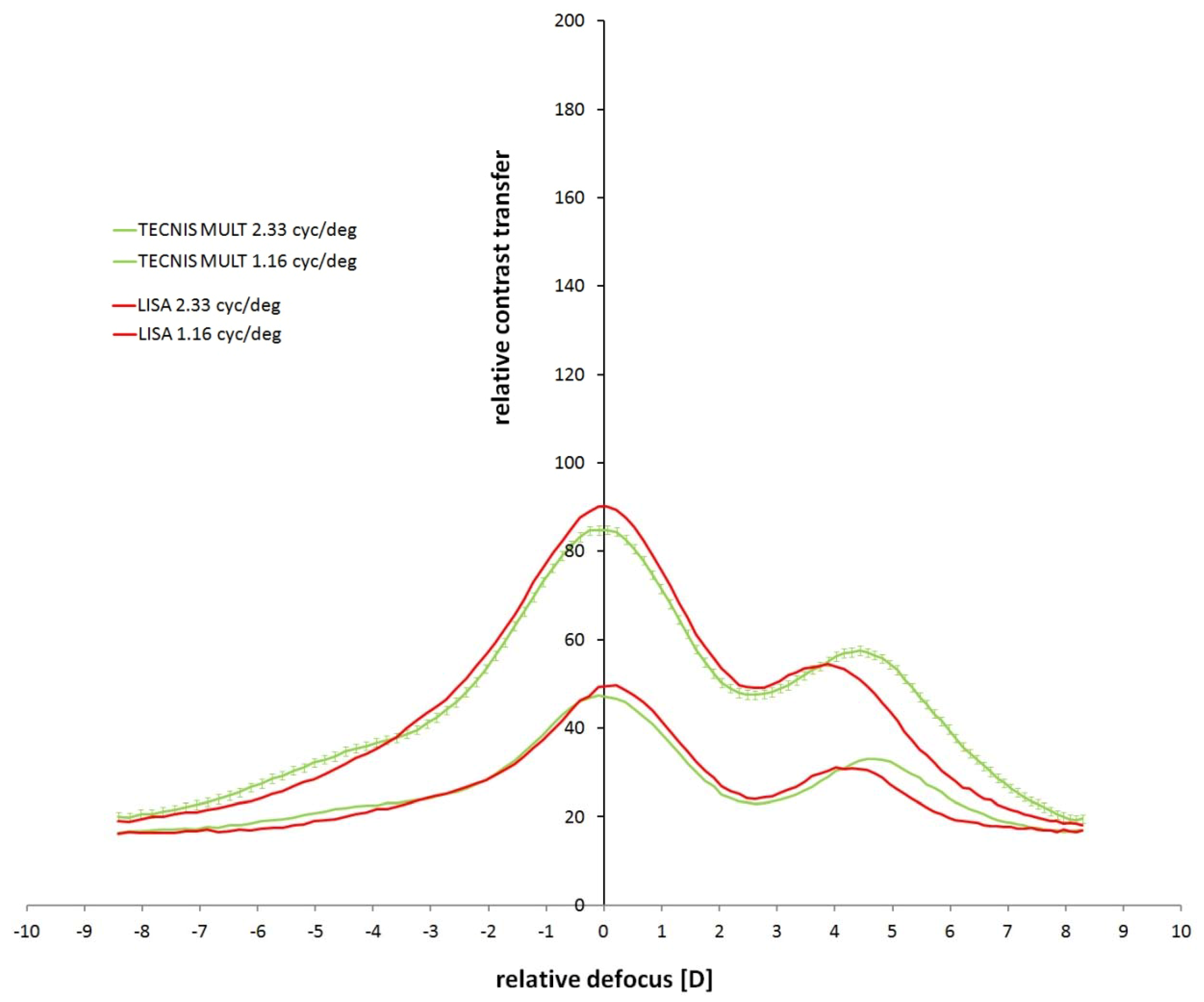
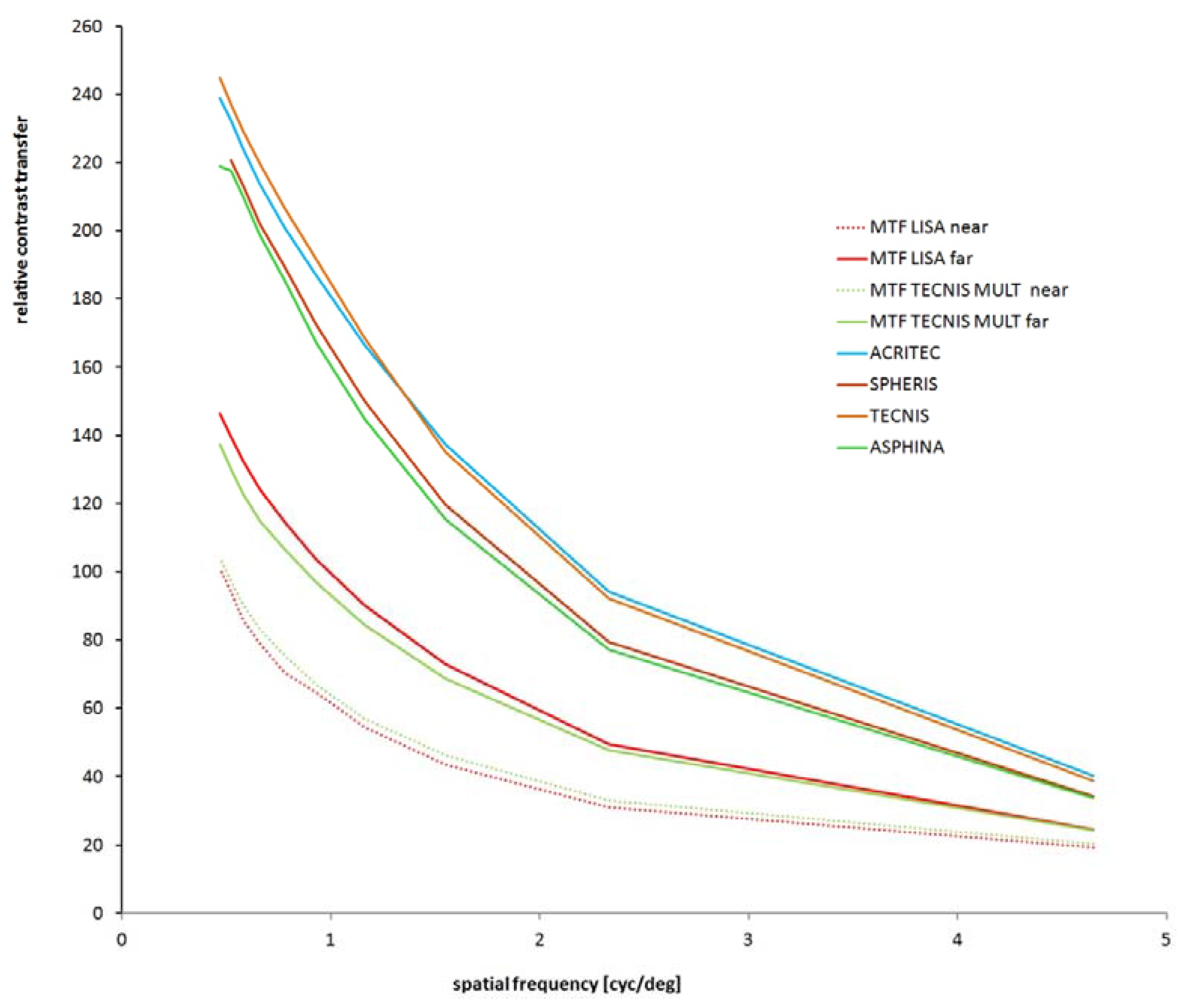
3.3. Relative Contrast Transfer at Different Spatial Frequencies
3.4. Measurements of Further Monofocal and Multifocal IOLs
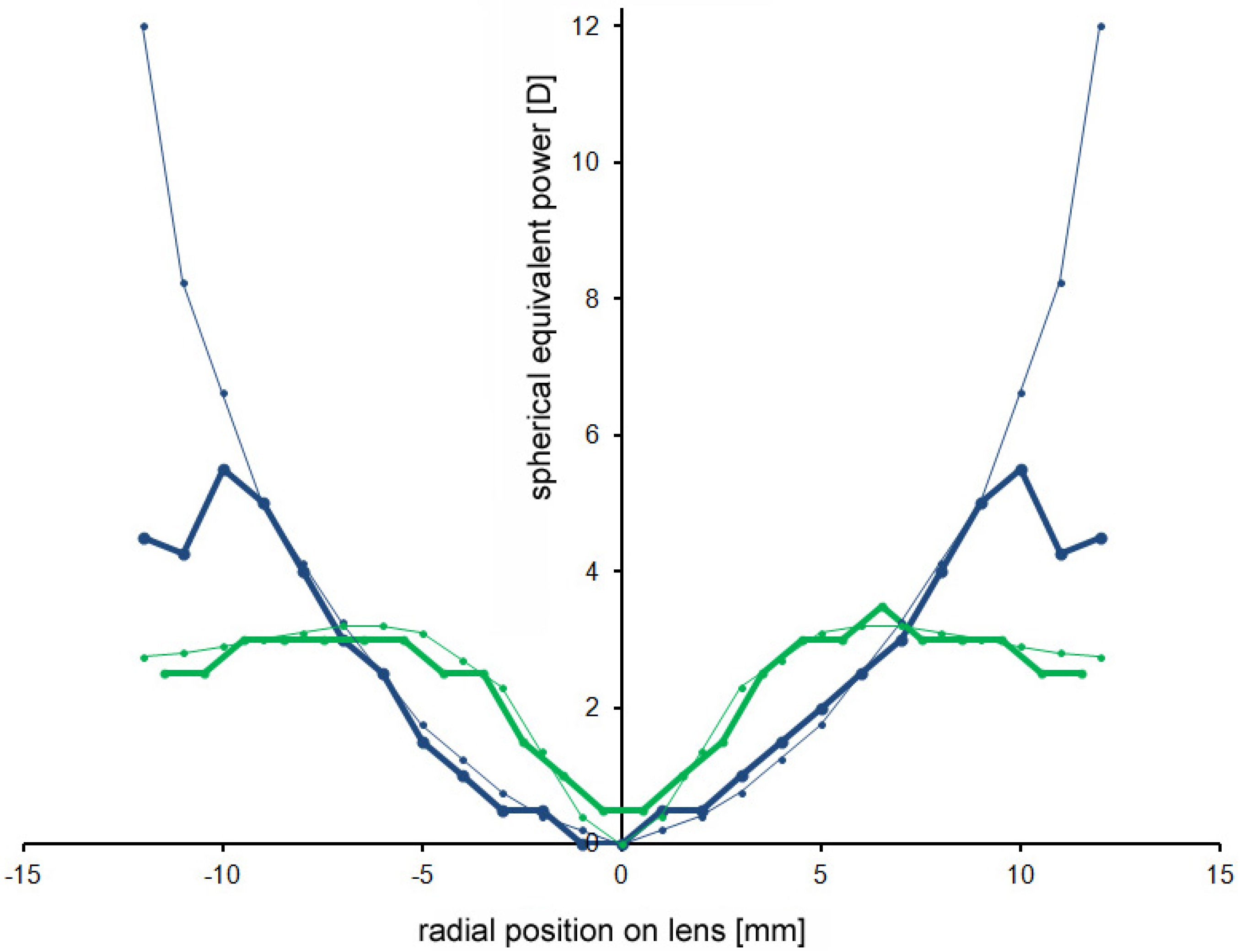
3.5. Measurement of Radial Refractive Gradient Lenses
4. Conclusions
4.1. Possible limitations of the Lens Scanner
- (1)
- The positioning and centration of the IOL in the cuvette. The custom-made lens holder does not allow for perfect centration of the IOL in the camera axis since this was done manually with a pair of tweezers. In addition, it was found that even minor mechanical forces acting on the soft lenses caused a rapid decay of their optical performance.
- (2)
- Since both the “neutralizing” trial lens and IOL had high power, small differences in the axial positions of the lenses had severe effects on the measurements of their absolute optical power: 1 mm displacement was equivalent to about 0.6 D.
- (3)
- The linearity of the video camera. It is assumed that luminance differences between the receptive field center and periphery were converted into pixel differences, no matter what the absolute local brightness of the picture was. It is known that video systems show a more log-linear response which means brightness differences are not linearly encoded in pixel values. Related to this problem, saturation is not fully controlled. However, since the average contrast in the image is determined from the sum of the absolute outputs of 10,000 receptive fields at different places, these variations may partially average out. In the current set-up, the gain control of the video system was set on automatic, resulting in an average pixel brightness of the video image of about 130 in all cases.
- (4)
- The ISO standard 11979-2 requests that IOLs should have a modulation transfer at a pupil size of 3 mm of at least 0.43 at 100 cyc/mm, corresponding to about 34.5 cyc/deg on the retina (image magnification in the human eye: 290 µm/deg). The current set-up can only measure the modulation transfer at spatial frequencies up to 4.65 cyc/deg. To measure at 34.5 cyc/deg, as requested by ISO 11979-2, either a video camera needs to be used with much smaller pixels of the CCD chip, or the imaging lens needs to have a longer focal length.
- (5)
- The ISO standard 11979-2 requests IOL performance to be measured in monochromatic light of 550 nm. While it is clear that a defined wavelength has its merits, we believe that the broadband white light that was used in the current study matches the typical experience of the subjects. We expect that the refractive power differences that might be measured with our procedure in green light to be negligible. Moreover, it would be easy to illuminate the target (Figure 1) with monochromatic light by use of an interference filter.
- (6)
- The optical aberrations potentially introduced by the cuvette wall and the neutralizing lens were not studied. Potentially, both could introduce spherical aberration. However, a water or saline-filled cuvette was also used in previous studies to measure IOLs and other authors should have faced the same problem (i.e., [4]).
4.2. Comparison to Other Procedures to Measure the Performance of Artificial Intraocular Lenses
4.3. Outlook: Measurements of Absolute Contrast Transfer, Astigmatism, and at Higher Spatial Frequencies
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Zalevsky, Z. Extended depth of focus imaging: A review. SPIE Rev. 2010, 1, 018001. [Google Scholar]
- Kusel, R.; Rassow, B. Preoperative assessment of intraocular lens corrected vision. Klin. Monbl. Augenheilkd. 1999, 215, 127–131. (In German) [Google Scholar] [CrossRef]
- Terwee, T.; Weeber, H.; van der Mooren, M.; Piers, P. Visualization of the retinal image in an eye model with spherical and aspheric, diffractive, and refractive multifocal intraocular lenses. J. Refract. Surg. 2008, 24, 223–232. [Google Scholar]
- Maxwell, W.A.; Lane, S.S.; Zhou, F. Performance of presbyopia-correcting intraocular lenses in distance optical bench tests. J. Cataract Refract. Surg. 2009, 35, 166–171. [Google Scholar] [CrossRef]
- Norrby, S. ISO eye model not valid for assessing aspherical lenses. J. Cataract Refract. Surg. 2008, 34, 1056–1057. [Google Scholar] [CrossRef]
- Tepelus, T.C.; Vazquez, D.; Seidemann, A.; Uttenweiler, D.; Schaeffel, F. Effects of lenses with different power profiles on eye shape in chickens. Vision Res. 2012, 54, 12–19. [Google Scholar] [CrossRef]
- Kim, M.J.; Zheleznyak, L.; MacRae, S.; Tchah, H.; Yoon, G. Optical evaluation of through-focus optical performance of presbyopia-correcting intraocular lenses using an optical bench system. J. Cataract Refract. Surg. 2011, 37, 1305–1312. [Google Scholar] [CrossRef]
- Marcos, S.; Barbero, S.; Jiménez-Alfaro, I. Optical quality and depth-of-field of eyes implanted with spherical and aspheric intraocular lenses. J. Refract. Surg. 2005, 21, 223–235. [Google Scholar]
- Piers, P.A.; Weeber, H.A.; Artal, P.; Norrby, S. Theoretical comparison of aberration-correcting customized and aspheric intraocular lenses. J. Refract. Surg. 2007, 23, 374–384. [Google Scholar]
- Bellucci, R.; Morselli, S.; Piers, P. Comparison of wavefront aberrations and optical quality of eyes implanted with five different intraocular lenses. J. Refract. Surg. 2004, 20, 297–306. [Google Scholar]
- Navarro, R.; Ferro, M.; Artal, P.; Miranda, I. Modulation transfer functions of eyes implanted with intraocular lenses. Appl. Opt. 1993, 32, 6359–6367. [Google Scholar] [CrossRef]
- Hütz, W.W.; Eckhardt, H.B.; Röhrig, B.; Grolmus, R. Reading ability with 3 multifocal intraocular lens models. J. Cataract Refract. Surg. 2006, 32, 2015–2021. [Google Scholar]
- Richter-Mueksch, S.; Weghaupt, H.; Skorpik, C.; Velikay-Parel, M.; Radner, W. Reading performance with a refractive multifocal and a diffractive bifocal intraocular lens. J. Cataract Refract. Surg. 2002, 28, 1957–1963. [Google Scholar] [CrossRef]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Schaeffel, F.; Kaymak, H. A Rapid and Convenient Procedure to Evaluate Optical Performance of Intraocular Lenses. Photonics 2014, 1, 267-282. https://doi.org/10.3390/photonics1030267
Schaeffel F, Kaymak H. A Rapid and Convenient Procedure to Evaluate Optical Performance of Intraocular Lenses. Photonics. 2014; 1(3):267-282. https://doi.org/10.3390/photonics1030267
Chicago/Turabian StyleSchaeffel, Frank, and Hakan Kaymak. 2014. "A Rapid and Convenient Procedure to Evaluate Optical Performance of Intraocular Lenses" Photonics 1, no. 3: 267-282. https://doi.org/10.3390/photonics1030267
APA StyleSchaeffel, F., & Kaymak, H. (2014). A Rapid and Convenient Procedure to Evaluate Optical Performance of Intraocular Lenses. Photonics, 1(3), 267-282. https://doi.org/10.3390/photonics1030267




