Abstract
(1) Background: Mental health significantly impacts personal relationships and societal integration. Portugal faces a high prevalence of psychiatric illnesses and psychological distress, which the COVID-19 pandemic might have exacerbated. Therefore, this study aims to study risk factors that lead to psychological problems, using data available in the primary health care centers of the region of Aveiro. (2) Methods: This observational and retrospective study analyzes data from 2009 to 2022 on psychological consultations in the Aveiro municipalities. Variables considered are municipality, International Classification of Primary Care problem, sex, and comorbidities (cancer, obesity, and diabetes). Summary statistics and graphs were employed for data understanding, with R software used for analysis. Regression models, odds ratios, and association tests were calculated. Also, cluster analysis was performed on municipalities. (3) Results: A new, significant increase in the appointment growth rate was observed in 2021 and 2022. Anxiety and depressive disorders contribute to the identified growth. Women reported more problems than men. Cancer was the most present comorbidity. (4) Conclusions: The study reveals increased mental health problems, with primary health care users in Aveiro experiencing worsened psychosocial health, resulting in more medical consultations for psychological reasons. Risk factors included being female and having chronic conditions such as cancer. The findings provide insights into the burden of mental health issues in the region, highlighting the need for effective mental health interventions and resources to address health inequalities and support at-risk groups.
1. Introduction
Mental health has been a topic of constant concern. In recent years, mental health’s important role in achieving global development goals has been recognized. This recognition is illustrated, for example, by the inclusion of mental health in the World Health Organization’s (WHO) Sustainable Development Goals: “By 2030, reduce premature mortality from non-communicable diseases by one-third through prevention and treatment, and promote mental health and well-being” [1,2].
However, in recent years, mental health and substance use disorders have increased by around 13%. The two most common mental health problems are depressive disorders and anxiety disorder [2]. According to information from the National Coordination for Mental Health, epidemiological studies have revealed that psychiatric disorders and mental health problems have become the leading cause of disability and morbidity in our societies. Of the ten leading causes of disability, five are psychiatric [3]. People with severe mental health problems tend to die prematurely due to preventable physical conditions. Globally, it is estimated that about 20% of children and adolescents have a mental health problem, and suicide is highlighted as the second leading cause of death among people aged 15–29 years [2]. Despite this information, the average global government spending on mental health is less than 2%. Many of these problems can even be treated efficiently at a relatively low cost; however, adequate treatment coverage remains extremely low, and, in addition, there is still a significant difference between people who need care and those who have access to it [2].
According to the Portuguese Society of Psychiatry and Mental Health, Portugal has Europe’s second-highest prevalence rate of psychiatric illnesses (22.9%). Other studies show that 57% of the Portuguese population has psychological distress [2,3]. According to the “Health at a Glance 2019” report of the Organization for Economic Cooperation and Development (OECD), Portugal is the second OECD country with the highest consumption of N04A antidepressants (1505 doses per thousand habitants) [4].
Since the COVID-19 pandemic emerged, an increased annual prevalence of mental health problems in the adult population has been reported, with the most frequent being depression, anxiety, mood disorders, post-traumatic stress, and obsessive-compulsive disorders [5]. Although the pandemic arose from the viral disease COVID-19, it turned out to be a crisis that affected the population at various levels: physical, mental, social, and economic. Therefore, it had a widespread impact, inducing, among other things, considerable levels of fear, restlessness, and concern. Some have referred to the growing burden on mental health as the “second” or “silent” pandemic [6].
Even though the negative consequences for mental health affect everyone, young people have been among populations with a higher risk of developing poor mental health, together with health professionals and females. The risk of poor mental health is also generally higher in individuals with pre-existing mental health problems [6].
The 2021 World Happiness Report indicates that the pandemic has been associated with a substantial increase in symptoms of mental illness, further noting that this period has contributed to the rise in inequalities in mental health, both within the population and among social groups [7]. In addition, four main types of mechanisms were identified with the various stressors associated with the pandemic. The four mechanisms that may affect mental health can be presumed as: (1) health-related anxieties directly resulting from COVID-19, such as the probability of being infected, the possibility of being hospitalized or dying, the probability of infecting others, and the possibility of loved ones becoming infected or dying; (2) the mental health consequences of concerns resulting from how the pandemic may affect a person’s financial situation, both in the short and long term; (3) complications resulting from domestic family arrangements during quarantine periods; and (4) the direct mental health effects of the loss or restriction of activities caused by the pandemic and the various quarantine policies [7].
The International Classification of Primary Care (ICPC) opened new horizons when it was published in 1987 by WONCA (World Organization of Colleges, Academies, and Academic Associations of General Practitioners/Family Physicians), now better known as the World Organization of Family Physicians. For the first time, health professionals had the means to classify, using only one classification, three essential elements of an appointment: reasons that led to the appointment, diagnoses or problems, and procedures. The link between these elements allows categorization from the beginning of the appointment to its conclusion [8].
The ICPC is a document with a simple structure based on two parts. One part comprises seventeen chapters, each with an alpha code. The other part contains seven identical components numbered with two-digit codes. This structure allows for specific categorization of the three elements of an appointment, facilitating manual classification systems. The rational and comprehensive structure of the ICPC makes it a classification model for present and future international classifications [8]. Since its publication, the ICPC has progressively received worldwide recognition as an appropriate classification for general and family medicine and primary care. It has been used intensively in some parts of the world, notably in Europe and Australia [8].
The reasons that lead patients to seek primary health care are found within the scope of general and family medicine. These reasons can present several natures, including symptoms, administrative procedures, diseases, established medical diagnoses, or even psychosocial problems. The latter can influence the course of a consultation, especially regarding correct medical diagnoses or managing the patient’s disease [9,10]. General and family medicine appointments are based on a “patient-centered” approach, which attends not only to the clinical response to the signs and symptoms presented but also to the expectations and fears of the user [10,11].
The Baixo Vouga Health Centre Group (Aveiro region), for general and family medicine, comprises eleven municipalities: Águeda, Albergaria-a-Velha, Anadia, Aveiro, Estarreja, Ílhavo, Murtosa, Oliveira do Bairro, Ovar, Sever do Vouga, and Vagos. There is a total of 74 parishes where, approximately estimated, three hundred and thirty thousand people live [12,13]. Its mission is to provide primary health care to the population in its geographical area with efficiency and quality, seeking to maintain the principles of equity and accessibility in a multidisciplinary manner and coordination with other national health services to enhance health gains. The mission also includes epidemiological surveillance, participation in teaching and training health professionals, and developing projects and programs in health and health services [13].
The present study was based on the ICPC classification of general and family medicine appointments between 2009 and 2022, with the goal of characterizing the population and identifying risk factors concerning mental health. Moreover, this study aimed to obtain more information on where municipalities stand regarding the impact of the pandemic on the mental health of their populations and, hence, adequate future mental health strategies and action plans in the area. In the analyzed dataset, each patient may have simultaneous diagnostic ICPC problems. Therefore, different rows can have information about the same patient.
According to the prioritization made in the Local Health Plan of the Region of Aveiro, the Public Health Unit chose to study three comorbidities (cancer, diabetes, and obesity) to better allocate resources to the population groups that will most benefit from its interventions.
2. Materials and Methods
The present epidemiological study is observational, analytical, and has a retrospective nature. The data under analysis refers to the collected data during medical consultations in which the codifications of the chapter “P—Psychological” of the International Classification of Primary Care (ICPC-2) were used. Data was collected between 2009 and 2022 in the municipalities that belong to the ACeS Baixo Vouga. Variables “Year”, “Municipality”, “ICPC-2 Code”, “ICPC-2 Title”, “Sex”, “N_Total”, and “Comorbidities” were considered.
Data regarding comorbidities were extracted separately by filtering the database to obtain the above mentioned variables, crossed with “P—Psychological” code and also with each comorbidity (T89 and T90 for diabetes, T82 for obesity, and B74, B75, D74, D75, D76, D77, D78, F74, H75, K72, L71, L97, N74, N75, N76, R84, R85, R86, R92, S77, S79, T71, T72, T73, U75, U76, U77, U78, U79, W72, W73, X75, X76, X77, X79, X80, X81, Y77, Y78, and Y79 for cancer). To obtain the final data for analysis, the different datasets were crossed through the variables “Year”, “Municipality”, “ICPC-2 Code”, “ICPC-2 Title”, and “Sex” to match the number of people who also had comorbidities. Variables for “Total_Diabetes”, “Total_Cancer”, and “Total_Obesity” were created.
The present study uses aggregated data considering the “ICPC-2 Title” and the “ICPC-2 Code” variables. All datasets were filtered according to ICPC-2 codification (variable ICPC-2 Code) regarding the diseases in question; only codes beginning with seven or higher were kept, as they refer to the diagnoses and diseases component.
Several statistical analyses were performed, including growth rate for the total number of problems, the individual analysis of each problem, and the number of problems with comorbidities.
The number of problems per year was analyzed by municipality, gender, and comorbidity. To visualize the data, scatterplots with fitted lines, dendograms, and geospatial graphs (maps) were constructed. Geospatial graphs illustrate the district of Aveiro and its municipalities, colored through a coded gradient in parallel with the number of problems registered; standardization was performed according to the number of residents [14].
Pearson correlation, and, after that, a linear regression model, was used to study the relationship between the annual number of problems and the registration year. Association measures, e.g., odds ratio (OR), between binary variables were calculated, namely for measuring the association between sex and psychological problems and between comorbidities and psychological problems. For the association between each psychological problem and its occurrence in the municipalities, and the strength of that association, Cramér’s V coefficient was calculated [15]. When required, assumptions were validated for all performed tests and analyses. Finally, a cluster analysis was performed with the goal of checking differences between municipalities.
All analyses were performed using the R software (version 4.0.2) through the RStudio interface. In addition, the analyses were conducted with a 5% significance level as a reference.
3. Results
3.1. Frequency Tables
Table A1 (Appendix A) reveals the number of psychological problems ICPC2 registered each year between 2009 and 2022. In 14 years, more than 1 million problems involving the chapter P—Psychological (all codes considered) of ICPC-2 were registered in the health centers of the ACeS Baixo Vouga, with an annual increase in reported problems since 2009. It should be noted that these results are not cumulative but refer to the number of problems registered every 12 months. The column “Growth in Percentage (%)” shows a general trend of decreasing growth rate, as revealed by the values of the percentages that decrease from year to year. However, in 2021 and 2022, this decrease did not occur, and a new increase in this percentage was observed (highlighted). The column “Number of patients of the ACeS” [16] presents data publicly accessible since 2016. Unfortunately, information before 2016 was unavailable. Here, an increase in the number of enrolled users from 2017 is verified.
When seeking to understand the nature of reported problems, the numbers of each ICPC-2 psychological problem recorded in each year and the respective growth rates were registered in Table A2 and Table A3 (Appendix A). These results helped to find which ICPC-2 psychological problems contributed most to the increase in percentage growth recorded in the last two years. Thus, anxiety disorder/anxiety state, phobia and compulsive disorder, hyperkinetic disorder, depressive disorder, post-traumatic stress, and nervous anorexia/bulimia showed considerable increases. Depressive and anxious/anxiety disorders were the most common diagnoses. The growth of hyperkinetic disorders has become more prominent over the years.
The percentage of all three comorbidities (cancer, diabetes, and obesity) present in the data was also recorded. For the last year (2022), 10.7% of the individuals with psychological problems had diabetes, 21.2% of the individuals had obesity, and 25.1% of the individuals had cancer. Therefore, cancer emerged as the more common comorbidity in 2022.
3.2. Results by Sex
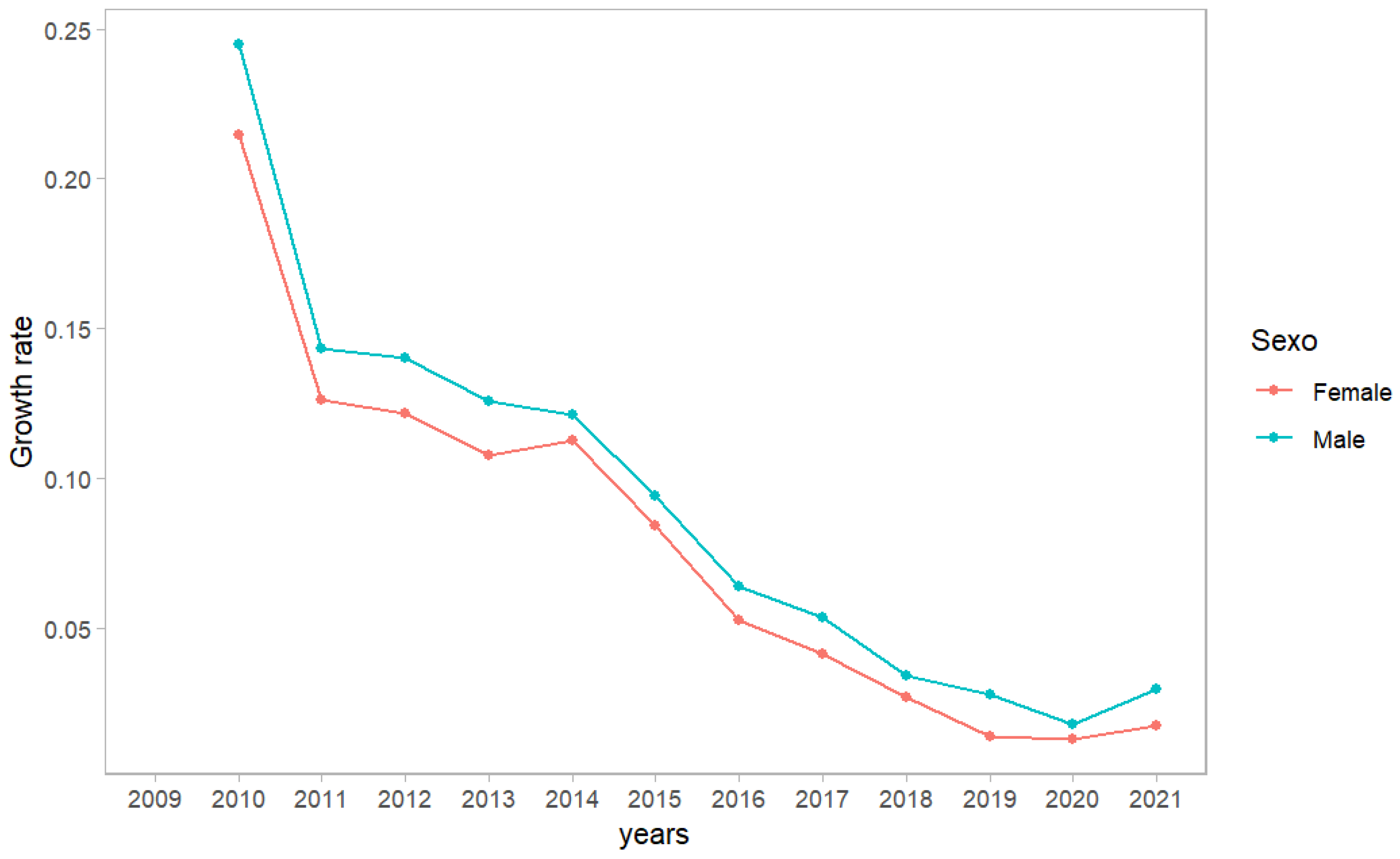
Women report more than double men’s psychological problems in primary health care consultations in the Aveiro region. The growth rate by sex is similar, with men’s growth rate always slightly bigger than women’s growth rate, but almost equal in recent years (Figure 1). Both results are not contradictory since the total number of psychological problems is much bigger for women; even with a higher growth rate, the total number of reported problems for men is growing far apart from the total number of reported problems for women.

Figure 1.
Growth rate of total number of problems registered per year in the ACeS BV according to gender.
The association with each ICPC-2 psychological problem was also verified, and the results are shown in Table 1, which presents ORs for different psychological problems according to sex. The female gender was used as the reference group. Therefore, an OR above 1 indicates that men have a higher possibility of developing a particular psychological problem. On the other hand, an OR below indicates the reverse situation. When the confidence interval for OR includes 1, the differences are not statistically significant [17]. In our analysis, all the reported problems had significant ORs. Nervous anorexia and bulimia (0.26), depressive disorders (0.49), and somatization (0.95) are the only ones that are more associated with the female gender since the OR is lower than 1. This does not contradict Figure 1 because depressive and anxiety disorders are clearly the most common problems (see Table A2 and Table A3). On the contrary, hyperkinetic disorders (9.07), schizophrenia (5.26), and post-traumatic stress (4.47) are problems that are more associated with males, but they are much more uncommon problems than depressive and anxiety disorders.

Table 1.
Calculated Odds Ratio (OR) for each psychological disorder and sex from August 2009 to August 2022.
3.3. Results by Comorbidities
In this subsection, we present the results concerning the OR calculated to test the association between comorbidities (diabetes, cancer, and obesity) and reported psychological disorders. Note that authors present unadjusted odds ratios, as confounders were not measured, implying caution in interpretations. More accurate results would be obtained for odds ratios adjusted by age and gender. The reference category represents the absence of the comorbidity. Thence, an OR above 1 yields a direct relation between the comorbidity and the psychological disorder, as an OR below 1 stands for the inverse situation. For example, for the more common problem (depressive disorders), all the OR are significant and above 1, indicating that patients with comorbidities are more likely to have depressive disorders than patients without comorbidities. Table 2 contains the results for the aforementioned comorbidities and psychological problems. The results with greater strength of association with diabetes are dementia (3.29), nervous anorexia and bulimia (0.10), and hyperkinetic disorder (0.07). The association between diabetes and dementia is well-known from the literature since blood sugar control can lead to hypoglycemia and damage the hippocampus [18]. The results with greater strength of association with cancer are nervous anorexia and bulimia (0.15), mental retardation (0.28), and hyperkinetic disorder (0.05). Finally, the results obtained regarding obesity present more non-significant ORs and values closer to 1.

Table 2.
Calculated Odds Ratio (OR) for each psychological disorder and comorbidity from August 2009 to August 2022.
3.4. Results by Municipalities
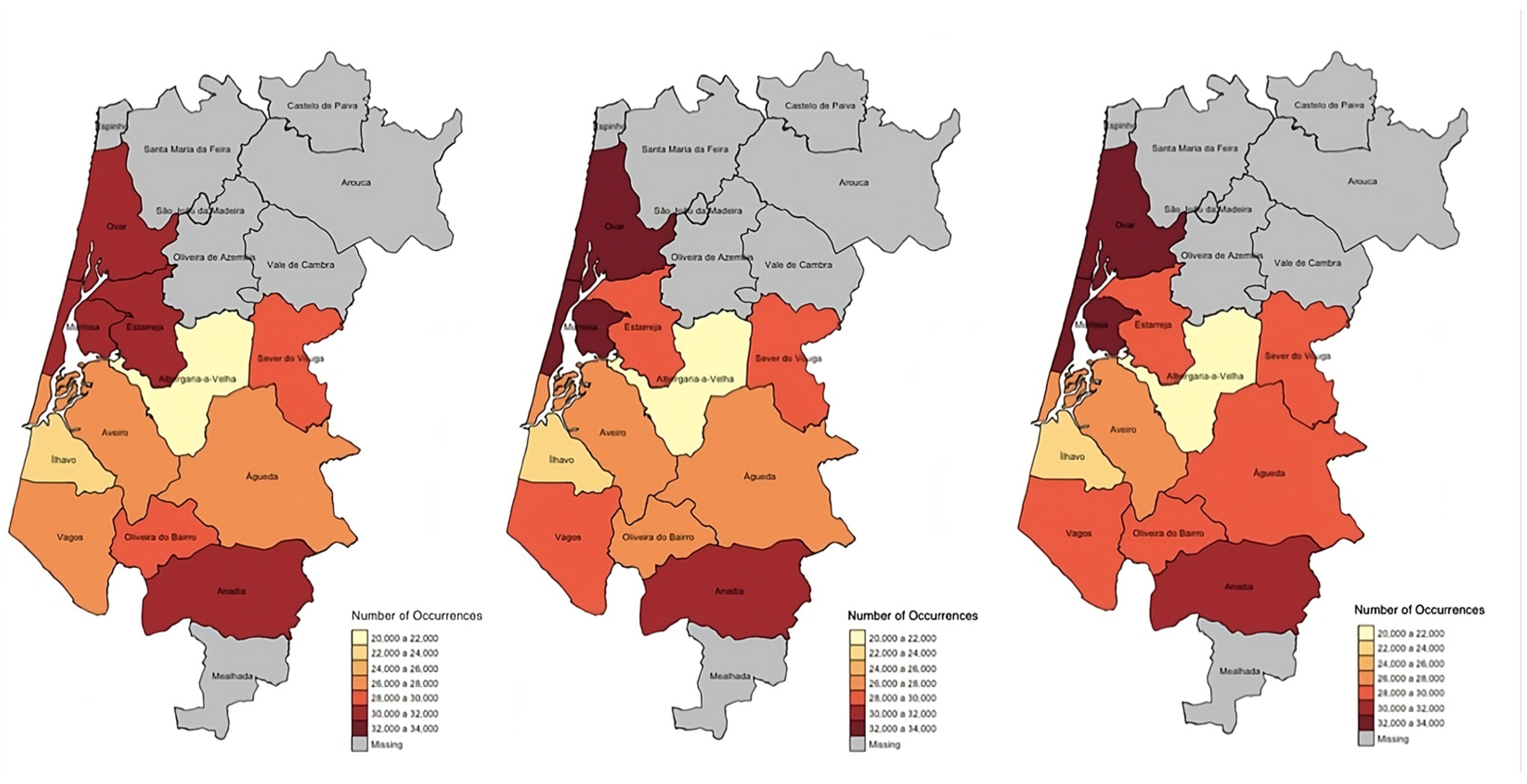
To visually compare the number of problems registered, maps of the district of Aveiro were built where the municipalities belonging to the ACeS Baixo Vouga were colored through a coded gradient in parallel with the number of problems registered each year. The darker the color, the more problems were registered; however, the municipalities colored in lighter colors registered fewer problems. A rate was also obtained (standardized according to the resident population) to make it possible to directly compare the number of problems recorded between municipalities without the number of residents being a source of bias. These results are illustrated in Figure 2. The municipality with more psychological problems registered in 2022 was Ovar. On the other hand, Albergaria-a-Velha was the municipality with the fewest registered psychological problems per 100,000 inhabitants.
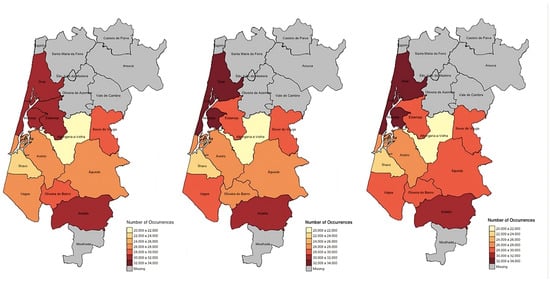
Figure 2.
Maps for 2020, 2021, and 2022, from left to right, respectively, with the municipalities belonging to the ACeS Baixo Vouga colored by a gradient representing the number of problems registered (from lighter to darker); results per 100,000 residents.
When testing independence between municipalities and mental illness, all Chi-square tests proved to be significant (p < 0.05), but Cramer’s V pointed to weak associations. Thus, no ICPC-2 psychological illness is strongly associated with its specific occurrence in the municipalities, despite the statistical relevance of this weak association.
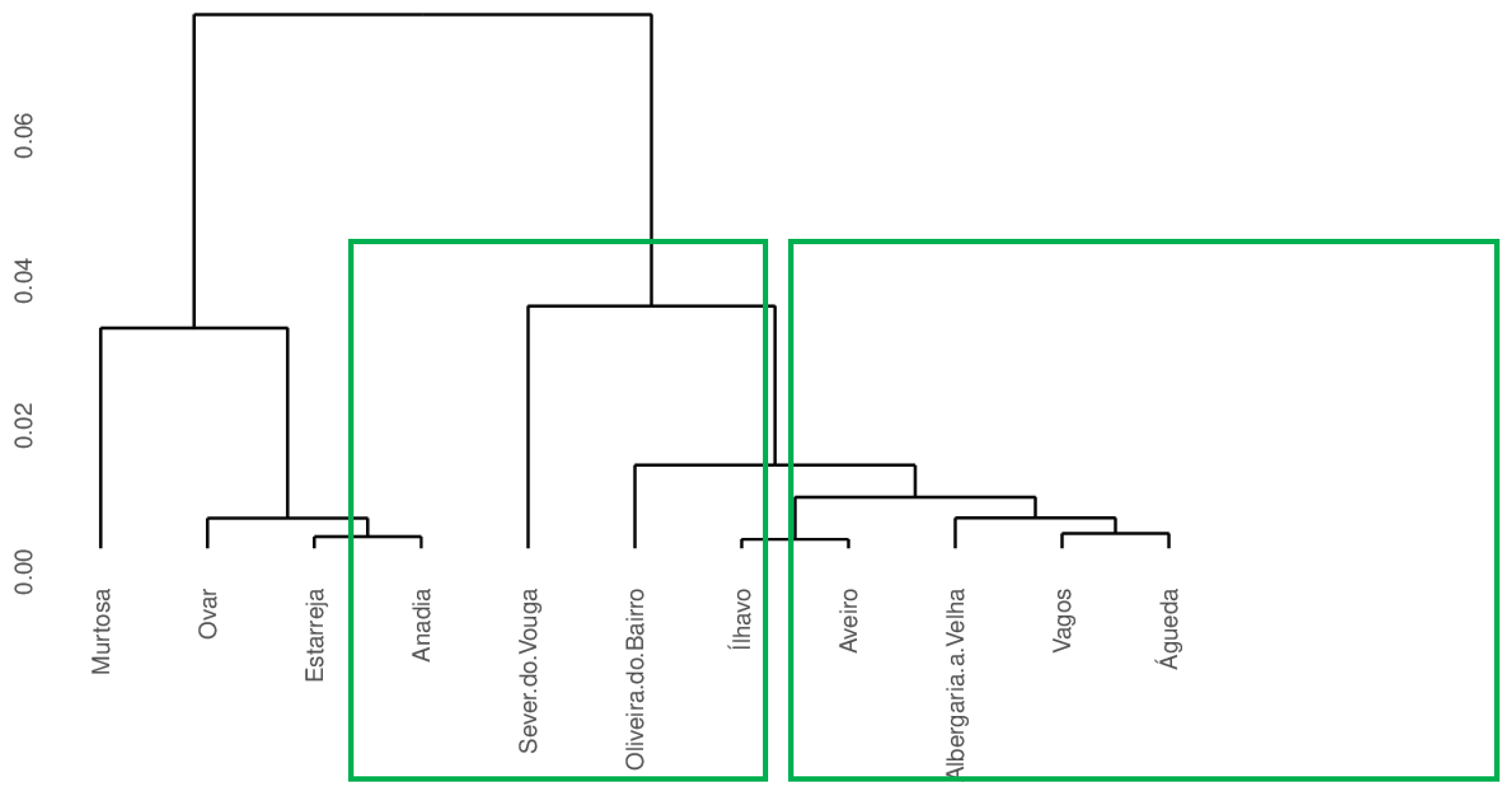
A cluster analysis was also conducted to determine if the occurrence profiles of psychological problems reported in each municipality were similar over the years. Ward’s method for clustering [19] was used since it is a general agglomerative hierarchical clustering procedure already implemented in R software. The results illustrated in Figure 3 reveal two clusters, with the first one consisting of Murtosa, Ovar, Estarreja, and Anadia, and the second one consisting of Sever do Vouga, Oliveira do Bairro, Ílhavo, Aveiro, Albergaria-a-Velha, Vagos, and Águeda. The results show that some municipalities have a similar behavior when considering the number of psychological problems over the years. The cluster analysis results are supported by grouping the municipalities with the most psychological problems recorded consistently over the years (Group 1).
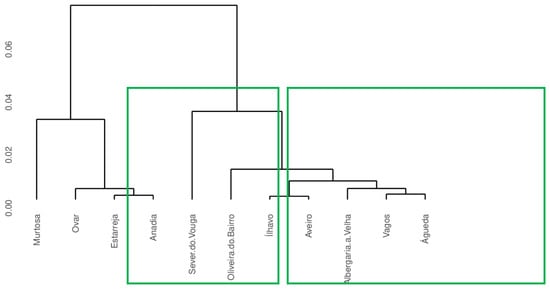
Figure 3.
Dendrogram for cluster analysis of occurrence profiles of psychological problems reported in each municipality.
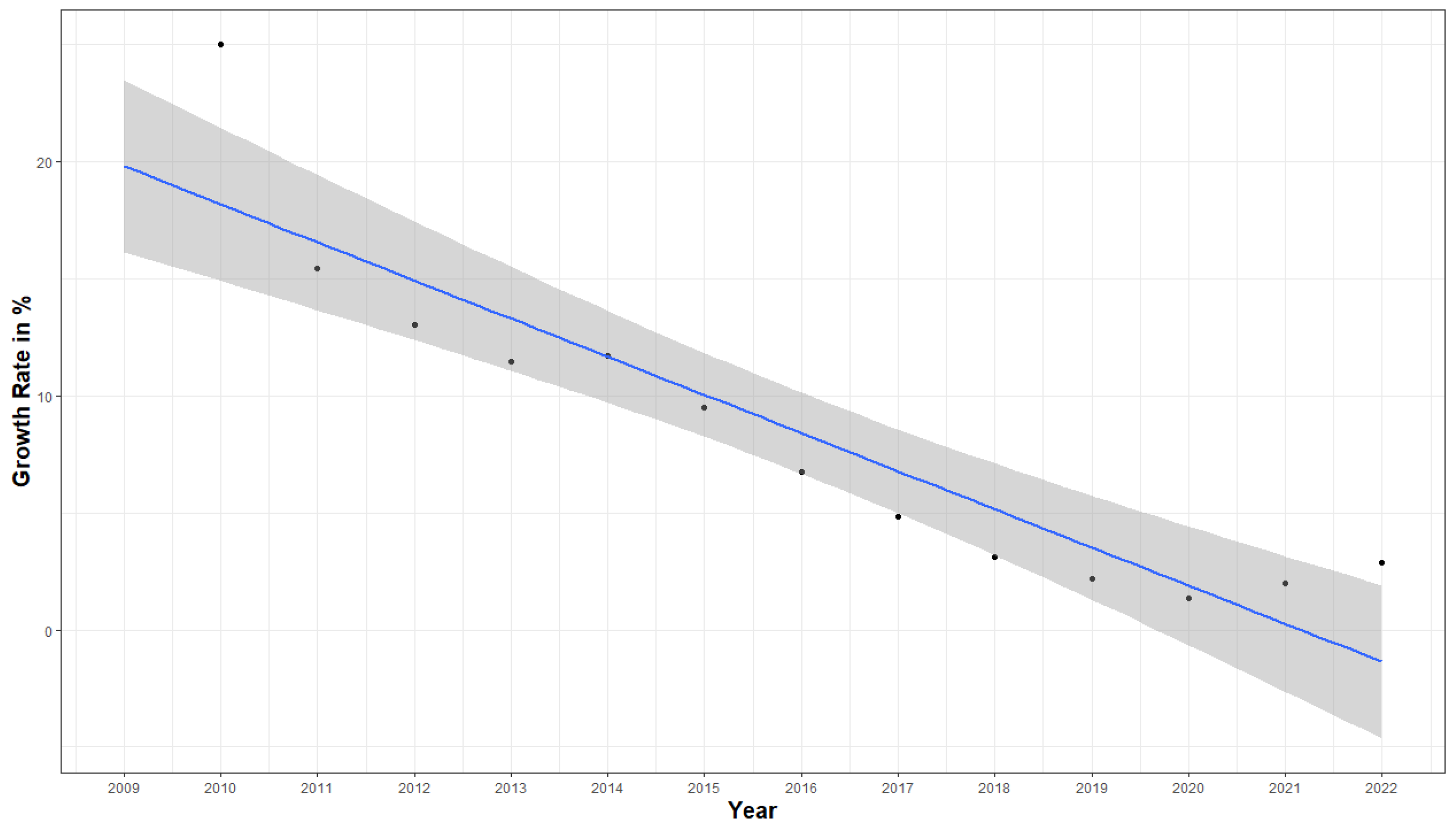
3.5. Results by Year
A significant correlation of −0.92 (p < 0.01) between the variables’ growth rate and year was verified. Figure 4 illustrates the growth in percentage by year. The obtained linear regression line, plotted in blue, considers the percentage growth values between 2010 and 2021 because the objective was to understand if the increase in the number of problems recorded in consultations in 2022 would be significantly higher to the point of reversing this downward trend that was being observed. It must be highlighted that the percentage growth in the number of problems, compared to the previous year, has decreased until 2020, despite an increase in the total number of reported problems (see Table A1). From this year onwards, the percentage growth was higher than in the previous year.
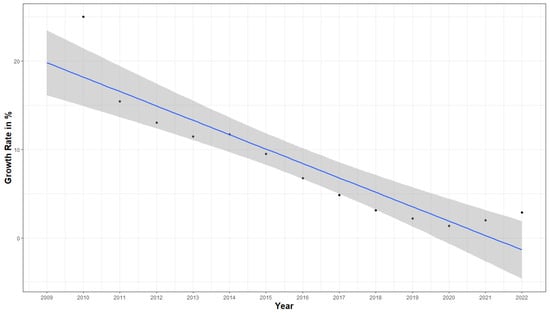
Figure 4.
Scatter plot for percentage growth of the number of problems per year with fit line and 95% CI.
By analyzing the obtained graph, the number of problems registered in 2022 is higher than predicted since the point is outside and above the calculated confidence interval (shown in gray); therefore, this growth is significant. The model estimated an increase in percentage for the year 2022 of −1.37% (−4.64%, 1.91%), while the actual value recorded was 2.86%. Therefore, there will likely be an increase in mental health problems due to the pandemic from 2020 onwards.
4. Discussion
Some limitations are present in this study, as only aggregated data was studied. The inherent limitations of aggregated data can impact the depth and accuracy of the conclusions that were drawn. This can be particularly problematic when studying mental health dynamics, where individual experiences and circumstances vary widely. Additionally, important variables such as age, socioeconomic status, and educational background were not available as they are not routinely collected in the National Health Service. While health care access is free and primary care units are distributed according to population needs, factors such as referral patterns and sociocultural influences could not be controlled. Therefore, this study offers a broad overview and facilitates high-level comparisons, but it is essential to analyze the obtained results with caution, recognizing the study’s potential to oversimplify complex realities and overlook critical nuances. Despite that, we believe that the results are useful as they can highlight several characteristics of mental health in the Aveiro region (major problems, gender differences, comorbidities influence, geographical patterns, and general tendency over the years).
Our work shows that primary health care users in the Aveiro region (Baixo Vouga Health Centre Group) have worsened their psychosocial health by increasing the number of medical consultations with a “P—Psychological” reason. Over the years, more psychological problems have been recorded in primary health care appointments. These results are general and do not consider if more than one psychological problem was mentioned per consultation or how many times a single patient visited the primary health care centers each year. However, as already stated, family doctors tend to send their patients to specialized appointments, leading to a small number of appointments with the same combination of patient and psychological problem in primary health care. It should also be noted that, in 2008, there was a reorganization of the national health service (SNS), which led to the digitalization of data, leading to greater awareness on the part of health professionals for improving clinical records [20,21].
Among the psychological problems recorded under the ‘P—Psychological’ chapter of the ICPC-2 classification in Aveiro, depressive disorders and anxiety disorders were the most frequently reported. These results are consistent with both the country’s and the world’s results regarding the prevalence of psychological problems [22]. Being female and having chronic conditions such as cancer seem to be risk factors associated with a higher likelihood of having more common psychological problems, especially for depressive disorders that represent about half of the reported problems.
The results reveal (Section 3.2) that women report more than twice as many psychological problems as men. The reported ORs are usually higher for men, but they concern more uncommon problems. Depressive disorders represent most of the reported problems each year, and, for that problem, women have an OR more than two times higher than men. We should point out that, in Portugal, there is some stigma and discrimination in mental health [23] affecting males, which may explain the lack of data concerning that gender. However, although this may be a plausible explanation, women represent a slightly higher proportion of primary health care center users. The higher prevalence of mental health disorders, psychological distress, and psychiatric drug use among women compared to men has been largely attributed to sex and gender differences [24,25]. Our results did not consider this difference due to the lack of available information.
To study psychological problems associated with comorbidities, diabetes, cancer, and obesity were chosen. The results revealed that 25% of individuals with at least one psychological problem have cancer. This percentage may be related to the fact that a cancer patient rarely closes the process regarding this disease, as it is chronic and usually always associated with active problems, and we may be facing a bias in the results. Cancer is a known significant stressor that can lead to increased psychological distress, such as anxiety and depressive disorders [26,27]. On the other hand, ageing may also be a plausible explanation since older people are more likely to develop psychological problems and cancer. For all the comorbidities, an association with depressive disorders has been shown since confidence intervals for OR are always above 1.
Regarding the low OR values of the association of each ICPC-2 psychological problem with cancer, these results may be due to greater difficulty in the clinical follow-up of patients with schizophrenia and mental retardation. Another noteworthy result is the hyperkinetic disorder, which is very much associated with children, hence the low OR value observed. Depressive and anxiety disorders are diseases that will hardly be considered surpassed, i.e., an “end” date is not attributed to the problem. Being relatively frequent pathologies, they will eventually lead to an accumulation of “active problems” without necessarily corresponding to the true prevalence of the problem.
A result highlighted with the diabetes comorbidity was the OR obtained for dementia (OR = 3.29). This is a high result indicating a strong association. However, it is most likely due to the age of the patients and the increased prevalence of type 2 diabetes in older people, as they are also more likely to develop psychological problems.
Concerning obesity, several results with a reduced effect may indicate a negligible association. Regarding this comorbidity, it should be noted that some drugs used in this group of diseases are associated with weight gain. For these reasons, it could be an interesting analysis, and it may be an alternative to study the overweight category instead of obesity.
Our study revealed that some municipalities behave similarly, considering the number of psychological problems reported over the years. The cluster analysis results are supported by grouping the municipalities with more reported psychological problems, which a greater presence of the elderly population, local social dynamics, or better primary care services can explain. No high association values were found using Cramer’s V coefficient for measuring the association between mental problems and municipalities, although independence was rejected (p < 0.05).
From Section 3.5, we can conclude that the percentage growth in the number of problems, compared to the previous year, has decreased until 2020. From this year onwards, the percentage growth was higher than in the previous year. Many reasons may explain this result, namely, the pandemic crisis. Also, the use of electronic medical records was not a standard from 2009 to 2022. Electronic records were increasingly adopted in the following decade, with many contributing factors: the expansion of family health units, the retirement of older physicians and their replacement with a younger generation, improvements in the electronic health record, and increased familiarity with ICPC-2. It was also expected that the registrations in 2022 were higher since there was an effort on the part of primary health care at the national level to again improve the access of users to the National Health Service with extraordinary work to catch up on the backlog of consultations that were suspended and postponed during the pandemic period. The number of patients enrolled in the ACeS Baixo Vouga has been increasing since 2017; however, there was only an increase in the growth rate in 2021.
The number of problems recorded in 2022 is higher than expected when applying the regression model to the percentage growth values between 2010 and 2021, as it is outside the confidence interval, and it can be concluded that this growth is significant. This behavior has been commonly identified as a striking feature of the COVID-19 pandemic, as a correlation between confinement, COVID-19, and mental problems is already well known [28,29,30,31].
5. Conclusions and Future Work
Major mental health strategies and action plans highlight the importance of mental health. However, interventions in the area are punctual and are not sustained over time [32]. Over 14 years of study, a notable surge in consultations has been observed in the Aveiro region, with particular evidence in the years 2021 and 2022, where unexpected increases in growth percentages were recorded. Depressive and anxiety disorders emerge as primary concerns. Gender disparities reveal that women seek psychological support more than twice as often as men, with certain disorders showing significant associations with gender. Geospatial analysis reveals variations in psychological burdens across municipalities, with Ovar notably reporting the highest number of cases. Additionally, cluster analysis elucidates distinct behavioral patterns among municipalities, paving the way for tailored strategies. Overall, these findings provide a nuanced understanding of psychological health dynamics in the Aveiro region, crucial for informed resource allocation in primary health care services. The results reinforce the importance of implementing community intervention programs and projects in mental health.
Future research should aim to incorporate individual-level data in order to account for confounding factors such as socioeconomic status, educational background, health care access, and age distribution. Additionally, longitudinal studies assessing post-pandemic trends and exploring specific mechanisms linking chronic diseases and mental health outcomes are suggested.
Author Contributions
Conceptualization, F.R., C.J.S., S.J.P., V.A., M.F. and R.P.L.; methodology, F.R., C.J.S., S.J.P., V.A., M.F. and R.P.L.; validation, F.R., C.J.S., S.J.P., V.A., M.F. and R.P.L.; formal analysis, F.R., C.J.S., S.J.P., V.A., M.F. and R.P.L.; investigation, F.R., C.J.S., S.J.P., V.A., M.F. and R.P.L.; data curation, R.P.L.; writing—original draft preparation, F.R., C.J.S., S.J.P., V.A., M.F. and R.P.L.; writing—review and editing, F.R., V.A. and M.F. All authors have read and agreed to the published version of the manuscript.
Funding
This work is supported by CIDMA under the FCT (Portuguese Foundation for Science and Technology) Multi-Annual Financing Program for R&D Units. Filipa Rocha was supported by a Research Grant of the Thematic Line Biomathematics of CIDMA. This work is partially financed by national funds through FCT—Fundação para a Ciência e a Tecnologia under the projects UID/00006/2025 and UIDB/00006/2020. https://doi.org/10.54499/UIDB/00006/2020. C.J.S. was also supported by the project “Mathematical Modelling of Multi-scale Control Systems: applications to human diseases (CoSysM3)”, 2022.03091.PTDC (https://doi.org/10.54499/2022.03091.PTDC), financially supported by national funds (OE), through FCT/MCTES.
Data Availability Statement
The original contributions presented in this study are included in the article. Despite being a secondary anonymized dataset extracted from the local database of the Public Health Unit of ACES BV, the dataset that supports the findings of this study is not publicly available because it may contain information that could compromise the normal operations of the data owner institution, but is available upon reasonable request to the coordination of Public Health Unit of ACES Baixo Vouga (usp.bv@arscentro.min-saude.pt).
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A

Table A1.
Representative table of the number of problems registered each year, the percentage growth rate related to the previous year, and the number of patients registered in the ACeS Baixo Vouga.
Table A1.
Representative table of the number of problems registered each year, the percentage growth rate related to the previous year, and the number of patients registered in the ACeS Baixo Vouga.
| Year (September to August) | Number of Problems | Growth Percentage (%) | Number of Patients of the ACeS |
|---|---|---|---|
| 2009 | 39,800 | ||
| 2010 | 49,755 | 25.0% | — |
| 2011 | 57,436 | 15.4% | — |
| 2012 | 64,932 | 13.1% | — |
| 2013 | 72,379 | 11.5% | — |
| 2014 | 80,869 | 11.7% | — |
| 2015 | 88,543 | 9.5% | — |
| 2016 | 94,537 | 6.8% | 384,303 |
| 2017 | 99,096 | 4.8% | 380,145 |
| 2018 | 102,191 | 3.1% | 384,967 |
| 2019 | 104,433 | 2.2% | 391,411 |
| 2020 | 105,870 | 1.4% | 393,881 |
| 2021 | 107,967 | 1.9% | 396,232 |
| 2022 | 111,063 | 2.8% | 402,526 |
| Total | 1,178,871 | — | — |

Table A2.
Number of problems registered each year by disease, and the respective percentage growth rate regarding the previous year (part I).
Table A2.
Number of problems registered each year by disease, and the respective percentage growth rate regarding the previous year (part I).
| Year | Personality Changes | Nervous Anorexia & Bulimia | Mental Retardation | Dementia | Anxiety Disorder/Anxiety State | Schizophrenia | Phobia, Compulsive Disorder | Neurasthenia, Surmenage | Other Psychological Disorders | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | |
| 2009 | 328 | 125 | 644 | 937 | 11,891 | 630 | 240 | 652 | 1605 | |||||||||
| 2010 | 436 | 32.9 | 157 | 25.6 | 770 | 19.6 | 1209 | 29.0 | 14,742 | 24.0 | 742 | 17.8 | 322 | 34.2 | 887 | 36.0 | 1989 | 23.9 |
| 2011 | 491 | 12.6 | 182 | 15.9 | 873 | 13.4 | 1492 | 23.4 | 16,894 | 14.6 | 817 | 10.1 | 381 | 18.3 | 1021 | 15.1 | 2271 | 14.2 |
| 2012 | 593 | 20.8 | 201 | 10.4 | 997 | 14.2 | 1634 | 9.5 | 18,906 | 11.9 | 899 | 10.0 | 424 | 11.3 | 1181 | 15.7 | 2510 | 10.5 |
| 2013 | 649 | 9.4 | 223 | 10.9 | 1073 | 7.6 | 1861 | 13.9 | 20,774 | 9.9 | 941 | 4.7 | 479 | 13.0 | 1318 | 11.6 | 2685 | 7.0 |
| 2014 | 737 | 13.6 | 246 | 10.3 | 1162 | 8.3 | 2082 | 11.9 | 23,060 | 11.0 | 1021 | 8.5 | 513 | 7.1 | 1438 | 9.1 | 2923 | 8.9 |
| 2015 | 791 | 7.3 | 268 | 8.9 | 1268 | 9.1 | 2354 | 13.1 | 25,134 | 9.0 | 1066 | 4.4 | 565 | 10.1 | 1517 | 5.5 | 3034 | 3.8 |
| 2016 | 842 | 6.4 | 276 | 3.0 | 1378 | 8.7 | 2607 | 10.7 | 26,866 | 6.9 | 1115 | 4.6 | 610 | 8.0 | 1599 | 5.4 | 3032 | −0.1 |
| 2017 | 871 | 3.4 | 294 | 6.5 | 1464 | 6.2 | 2786 | 6.9 | 28,550 | 6.3 | 1179 | 5.7 | 647 | 6.1 | 1687 | 5.5 | 3052 | 0.7 |
| 2018 | 914 | 4.9 | 300 | 2.0 | 1546 | 5.6 | 2898 | 4.0 | 29,921 | 4.8 | 1207 | 2.4 | 678 | 4.8 | 1805 | 7.0 | 3073 | 0.7 |
| 2019 | 945 | 3.4 | 299 | −0.3 | 1614 | 4.4 | 3043 | 5.0 | 30,968 | 3.5 | 1240 | 2.7 | 700 | 3.2 | 1829 | 1.3 | 3035 | −1.2 |
| 2020 | 978 | 3.5 | 299 | 0.0 | 1628 | 0.9 | 2994 | −1.6 | 31,851 | 2.9 | 1239 | −0.1 | 712 | 1.7 | 1810 | −1.0 | 2987 | −1.6 |
| 2021 | 1014 | 3.7 | 316 | 5.7 | 1647 | 1.2 | 3093 | 3.3 | 33,087 | 3.9 | 1255 | 1.3 | 738 | 3.7 | 1715 | −5.2 | 2929 | −1.9 |
| 2022 | 1039 | 2.5 | 330 | 4.4 | 1689 | 2.6 | 3183 | 2.9 | 34,583 | 4.5 | 1256 | 0.1 | 774 | 4.9 | 1687 | −1.6 | 2923 | −0.2 |

Table A3.
Number of problems registered each year by disease and the respective percentage growth rate regarding the previous year (part II).
Table A3.
Number of problems registered each year by disease and the respective percentage growth rate regarding the previous year (part II).
| Year | Other Organic Psychosis | Other Psychosis | Hyperkinetic Disorder | Depressive Disorders | Affective Psychosis | Somatization | Post-Traumatic Stress | Suicide/Attempted Suicide | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | |
| 2009 | 328 | 270 | 304 | 19,205 | 435 | 1846 | 153 | 207 | ||||||||
| 2010 | 393 | 19.8 | 316 | 17.0 | 461 | 51.6 | 24,072 | 25.3 | 545 | 25.3 | 2251 | 21.9 | 190 | 24.2 | 273 | 31.9 |
| 2011 | 431 | 9.7 | 344 | 8.9 | 599 | 29.9 | 27,987 | 16.3 | 627 | 15.0 | 2503 | 11.2 | 199 | 4.7 | 324 | 18.7 |
| 2012 | 460 | 6.7 | 366 | 6.4 | 778 | 29.9 | 31,970 | 14.2 | 741 | 18.2 | 2665 | 6.5 | 225 | 13.1 | 382 | 17.9 |
| 2013 | 491 | 6.7 | 405 | 10.7 | 961 | 23.5 | 36,005 | 12.6 | 850 | 14.7 | 2946 | 10.5 | 281 | 24.9 | 437 | 14.4 |
| 2014 | 533 | 8.6 | 446 | 10.1 | 1163 | 21.0 | 40,526 | 12.6 | 974 | 14.6 | 3244 | 10.1 | 305 | 8.5 | 496 | 13.5 |
| 2015 | 577 | 8.3 | 478 | 7.2 | 1389 | 19.4 | 44,635 | 10.1 | 1086 | 11.5 | 3497 | 7.8 | 325 | 6.6 | 559 | 12.7 |
| 2016 | 590 | 2.3 | 496 | 3.8 | 1535 | 10.5 | 47,796 | 7.1 | 1178 | 8.5 | 3676 | 5.1 | 345 | 6.2 | 596 | 6.6 |
| 2017 | 622 | 5.4 | 513 | 3.4 | 1666 | 8.5 | 49,707 | 4.0 | 1253 | 6.4 | 3799 | 3.3 | 369 | 7.0 | 637 | 6.9 |
| 2018 | 626 | 0.6 | 534 | 4.1 | 1782 | 7.0 | 50,587 | 1.8 | 1315 | 4.9 | 3963 | 4.3 | 388 | 5.1 | 654 | 2.7 |
| 2019 | 630 | 0.6 | 550 | 3.0 | 1889 | 6.0 | 51,250 | 1.3 | 1368 | 4.0 | 3999 | 0.9 | 404 | 4.1 | 670 | 2.4 |
| 2020 | 623 | −1.1 | 555 | 0.9 | 1959 | 3.7 | 51,747 | 1.0 | 1385 | 1.2 | 4007 | 0.2 | 411 | 1.7 | 685 | 2.2 |
| 2021 | 626 | 0.5 | 544 | −2.0 | 2046 | 4.4 | 52,642 | 1.7 | 1404 | 1.4 | 3826 | −4.5 | 409 | −0.5 | 676 | −1.3 |
| 2022 | 609 | −2.7 | 560 | 2.9 | 2191 | 7.1 | 54,042 | 2.7 | 1443 | 2.8 | 3624 | −5.3 | 432 | 5.6 | 698 | 3.3 |
References
- United Nations. The Sustainable Development Goals Report 2022. Available online: https://unstats.un.org/sdgs/report/2022/ (accessed on 30 December 2024).
- World Health Organization. Mental Health. Available online: https://www.who.int/health-topics/mental-health#tab=tab_1 (accessed on 30 December 2024).
- Relatório de Atividades UCC “Nós”. Available online: https://bicsp.min-saude.pt/pt/biufs/3/833/30019/3152671/O%20QUE%20FAZEMOS/Relato%CC%81rio%20de%20Atividades%20USF%20QM%202022.pdf (accessed on 30 December 2024).
- OECD Pharmaceutical Market: Pharmaceutical Consumption. 2022. Available online: https://stats.oecd.org/ (accessed on 30 December 2024).
- Baltazar, C. Mental Healthcare in Portugal: Support, Options, and More. Available online: https://www.expatica.com/pt/healthcare/healthcare-services/mental-health-portugal-104327/ (accessed on 30 December 2024).
- Scholz, N. Mental Health and the Pandemic. 2021. Available online: https://www.europarl.europa.eu/thinktank/en/document/EPRS_BRI(2021)696164 (accessed on 30 December 2024).
- Helliwell, J.; Layard, R.; Sachs, J.; Neve, J.E.; Aknin, L.; Wang, S. World Happiness Report. 2021. Available online: https://happiness-report.s3.amazonaws.com/2021/WHR+21.pdf (accessed on 30 December 2024).
- World Organization of Family Doctors. International Classification of Primary Care: ICPC-2; Oxford University Press: Oxford, UK, 2003. [Google Scholar]
- Rodrigues, J. Porque consultam os utentes o seu médico de família. Rev. Port. Med. Geral Fam. 2000, 16, 442–452. [Google Scholar]
- Gulbrandsen, P.; Fugelli, P.; Sandvik, L.; Hjortdahl, P. Influence of social problems on management in general practice: Multipractice questionnaire survey. BMJ 1998, 317, 28. [Google Scholar] [CrossRef] [PubMed]
- Rebelo, L.P. O médico de família do futuro: Três modelos de actuação, cinco atributos e cinco aptidões essenciais-parte II. Rev. Port. Med. Geral Fam. 2001, 17, 159–162. [Google Scholar]
- População Residente: Total. Available online: https://www.pordata.pt/municipios/populacao+residente+total-359 (accessed on 30 December 2024).
- Relatório Atividades ACES Baixo Vouga. 2022. Available online: https://bicsp.min-saude.pt/pt/biufs/2/20019/Pages/default.aspx (accessed on 30 December 2024).
- População Residente. Available online: https://www.ine.pt/xportal/xmain?xpid=INE&xpgid=ine_indicadores&contecto=pi&indOcorrCod=0011628&selTab=tab0 (accessed on 30 December 2024).
- Liebetrau, A.M. Measures of Association; Sage Publications Newbury Park: Thousand Oaks, CA, USA, 1983. [Google Scholar]
- Utentes Inscritos em Cuidados de Saúde Primários. Available online: https://transparencia.sns.gov.pt/explore/dataset/utentes-inscritos-em-cuidados-de-saude-primarios/table/?flg=pt&disjunctive.ars&disjunctive.aces&sort=periodo (accessed on 30 December 2024).
- Morris, J.A.; Gardner, M.J. Calculating confidence intervals for relative risks (odds ratios) and standardised ratios and rates. Br. Med. J. Clin. Res. Ed. 1988, 296, 1313–1316. [Google Scholar] [CrossRef] [PubMed]
- Cao, F.; Yang, F.; Li, J.; Guo, W.; Zhang, C.; Gao, F.; Sun, X.; Zhou, Y.; Zhang, W. The relationship between diabetes and the dementia risk: A meta-analysis. Diabetol. Metab. Syndr. 2024, 16, 101. [Google Scholar] [CrossRef] [PubMed]
- Ward, J.H. Hierarchical Grouping to Optimize an Objective Function. JASA 1963, 58, 236–244. [Google Scholar] [CrossRef]
- Diário da República Portugal. Decreto-Lei n.o 28/2008, de 22 de Fevereiro. 2008. Available online: https://diariodarepublica.pt/dr/detalhe/decreto-lei/28-2008-247675 (accessed on 30 December 2024).
- Diário da República Portugal. Decreto-Lei n.o 19/2010, de 22 de Março. 2010. Available online: https://diariodarepublica.pt/dr/detalhe/decreto-lei/19-2010-611341 (accessed on 30 December 2024).
- Institute of Health Metrics and Evaluation. Global Health Data Exchange. Available online: https://ghdx.healthdata.org/ (accessed on 30 December 2024).
- Di Fazio, N.; Morena, D.; Delogu, G.; Volonnino, G.; Manetti, F.; Padovano, M.; Fineschi, V. Mental Health Consequences of COVID-19 Pandemic Period in the European Population: An Institutional Challenge. Int. J. Environ. Res. Public Health 2022, 19, 9347. [Google Scholar] [CrossRef] [PubMed]
- Maestre-Miquel, C.; López-de-Andrés, A.; Ji, Z.; de Miguel-Diez, J.; Brocate, A.; Sanz-Rojo, S.; Zamorano-León, J.J. Gender differences in the prevalence of mental health, psychological distress and psychotropic medication consumption in Spain: A nationwide population-based study. Int. J. Environ. Res. Public Health 2021, 18, 6350. [Google Scholar] [CrossRef] [PubMed]
- Otten, D.; Tibubos, A.N.; Schomerus, G.; Brähler, E.; Binder, H.; Kruse, J.; Beutel, M.E. Similarities and differences of mental health in women and men: A systematic review of findings in three large German cohorts. Front. Public Health 2021, 9, 553071. [Google Scholar] [CrossRef] [PubMed]
- Forbes, H.; Carreira, H.; Funston, G.; Andresen, K.; Bhatia, U.; Strongman, H.; Bhaskaran, K. Early, medium and long-term mental health in cancer survivors compared with cancer-free comparators: Matched cohort study using linked UK electronic health records. EClinicalMedicine 2024, 76, 102826. [Google Scholar] [CrossRef] [PubMed]
- Pitman, A.; Suleman, S.; Hyde, N.; Hodgkiss, A. Depression and anxiety in patients with cancer. BMJ 2018, 361, k1415. [Google Scholar] [CrossRef] [PubMed]
- Larson, P.; Bergmans, R. Impact of the COVID-19 pandemic on temporal patterns of mental health and substance abuse related mortality in Michigan: An interrupted time series analysis. Lancet Reg. Health–Am. 2022, 10, 100218. [Google Scholar] [CrossRef] [PubMed]
- Lopes, S.; Soares, P.; Sousa, J.; Rocha, J.; Boto, P.; Santana, R. Effect of the COVID-19 pandemic on the frequency of emergency department visits in Portugal: An interrupted time series analysis until July 2021. J. Am. Coll. Emerg. Phys. 2023, 4, e12864. [Google Scholar] [CrossRef] [PubMed]
- Silva-Valencia, J. Effect of the COVID-19 pandemic on mental health visits in primary care: An interrupted time series analysis from nine INTRePID countries. EClinicalMedicine 2024, 70, 102533. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Hu, J.; Hu, W. Interrupted time series analysis using the ARIMA model of the impact of COVID-19 on the incidence rate of notifiable communicable diseases in China. BMC Infect. Dis. 2023, 23, 375. [Google Scholar] [CrossRef] [PubMed]
- Center for Disease Control and Prevention. About Mental Health. Available online: https://www.cdc.gov/mental-health/about/index.html (accessed on 30 December 2024).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).