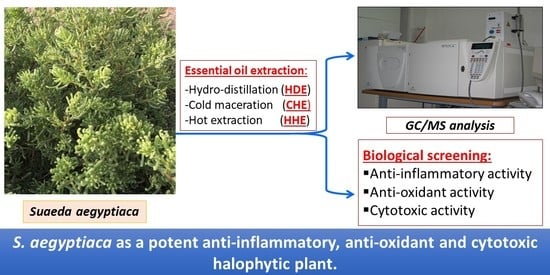
GC-MS Analysis and Bioactivities of the Essential Oil of Suaeda aegyptiaca
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Preparation
2.2. Extraction of Essential Oil
2.2.1. Cold n-Hexane Extraction (CHE)
2.2.2. Hot n-Hexane Extraction (HHE)
2.2.3. Hydro-distillation Extraction (HDE)
2.3. GC-MS Analysis of the Different Extracts
2.4. Biological Evaluation
2.4.1. Anti-Oxidant Activity
2.4.2. Anti-Inflammatory Activity
COX-1 and COX-2 Inhibition Assay
Measurement of TNF-α in an LPS-stimulated murine macrophage cell line (RAW264.7)
2.4.3. Cytotoxic Evaluation of the Different Extracts Using an MTT Assay
- Cell preparation
- MTT assay
3. Results
3.1. GC-MS Analysis of the Different Extracts of S. aegyptiaca
3.2. Biological Evaluation
3.2.1. Anti-Oxidant Activity
3.2.2. Cytotoxic Activity
3.2.3. Anti-Inflammatory Evaluation
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Boscaiu, M. Anatomical Adaptations of Halophytes. A Review of Classic Literature and Recent Findings. An. Stiintifice Ale Univ. Al. I. Cuza Din Iasi 2017, 63, 59–61. [Google Scholar]
- Abogadallah, G.M. Insights into the significance of antioxidative defense under salt stress. Plant Signal. Behav. 2010, 5, 369–374. [Google Scholar] [CrossRef] [PubMed]
- Saleh, I.A.; Usman, K.; Abu-Dieyeh, M.H. Halophytes as important sources of antioxidants and anti-cholinesterase compounds. In Handbook of Halophytes: From Molecules to Ecosystems towards Biosaline Agriculture; Springer: Berlin/Heidelberg, Germany, 2020; pp. 1–22. [Google Scholar] [CrossRef]
- Hussain, T.; Tan, B.; Yin, Y.; Blachier, F.; Tossou, M.C.; Rahu, N. Oxidative stress and inflammation: What polyphenols can do for us? Oxidative Med. Cell. Longev. 2016, 2016, 7432797. [Google Scholar] [CrossRef] [PubMed]
- Amin, E.; Abdel-Bakky, M.S.; Mohammed, H.A.; Chigrupati, S.; Qureshi, K.A.; Hassan, M.H. Phytochemical Analysis and Evaluation of the Antioxidant and Antimicrobial Activities of Five Halophytes from Qassim Flora. Pol. J. Environ. Stud. 2022, 31, 3005–3012. [Google Scholar] [CrossRef]
- Luo, M.; Zhou, L.; Huang, Z.; Li, B.; Nice, E.C.; Xu, J.; Huang, C. Antioxidant Therapy in Cancer: Rationale and Progress. Antioxidants 2022, 11, 1128. [Google Scholar] [CrossRef]
- Canli, Ö.; Nicolas, A.M.; Gupta, J.; Finkelmeier, F.; Goncharova, O.; Pesic, M.; Neumann, T.; Horst, D.; Löwer, M.; Sahin, U. Myeloid cell-derived reactive oxygen species induce epithelial mutagenesis. Cancer Cell 2017, 32, 869–883.e865. [Google Scholar] [CrossRef]
- Laksmitawati, D.R.; Prasanti, A.P.; Larasinta, N.; Syauta, G.A.; Hilda, R.; Ramadaniati, H.U.; Widyastuti, A.; Karami, N.; Afni, M.; Rihibiha, D.D. Anti-inflammatory potential of gandarusa (Gendarussa vulgaris Nees) and soursoup (Annona muricata L) extracts in LPS stimulated-macrophage cell (RAW264. 7). J. Nat. Remedies 2016, 16, 73–81. [Google Scholar] [CrossRef]
- Rassem, H.H.; Nour, A.H.; Yunus, R.M. Techniques for extraction of essential oils from plants: A review. Aust. J. Basic Appl. Sci. 2016, 10, 117–127. [Google Scholar]
- Charles, D.J.; Simon, J.E. Comparison of extraction methods for the rapid determination of essential oil content and composition of basil. J. Am. Soc. Hortic. Sci. 1990, 115, 458–462. [Google Scholar] [CrossRef]
- Okonkwo, C.; Ohaeri, O. Comparative study of steam distillation and soxhlet for the extraction of botanical oils. Asian J. Biol. Sci. 2020, 13, 62–69. Available online: https://scialert.net/abstract/?doi=ajbs.2020.62.69 (accessed on 13 November 2021). [CrossRef]
- Zhang, C.-Y.; Guo, M. Comparing three different extraction techniques on essential oil profiles of cultivated and wild lotus (Nelumbo nucifera) flower. Life 2020, 10, 209. [Google Scholar] [CrossRef] [PubMed]
- Oueslati, S.; Trabelsi, N.; Boulaaba, M.; Legault, J.; Abdelly, C.; Ksouri, R. Evaluation of antioxidant activities of the edible and medicinal Suaeda species and related phenolic compounds. Ind. Crops Prod. 2012, 36, 513–518. [Google Scholar] [CrossRef]
- Vizetto-Duarte, C.; Figueiredo, F.; Rodrigues, M.J.; Polo, C.; Rešek, E.; Custódio, L. Sustainable valorization of halophytes from the mediterranean area: A comprehensive evaluation of their fatty acid profile and implications for human and animal nutrition. Sustainability 2019, 11, 2197. [Google Scholar] [CrossRef]
- Mohammed, H.A.; Al-Omar, M.S.; El-Readi, M.Z.; Alhowail, A.H.; Aldubayan, M.A.; Abdellatif, A.A. Formulation of ethyl cellulose microparticles incorporated pheophytin a isolated from suaeda vermiculata for antioxidant and cytotoxic activities. Molecules 2019, 24, 1501. [Google Scholar] [CrossRef]
- Patra, J.; Dhal, N.; Thatoi, H. In vitro bioactivity and phytochemical screening of Suaeda maritima (Dumort): A mangrove associate from Bhitarkanika, India. Asian Pac. J. Trop. Med. 2011, 4, 727–734. [Google Scholar] [CrossRef]
- Panta, S.; Flowers, T.; Lane, P.; Doyle, R.; Haros, G.; Shabala, S. Halophyte agriculture: Success stories. Environ. Exp. Bot. 2014, 107, 71–83. [Google Scholar] [CrossRef]
- Park, J.M.; Kim, S.D.; Lee, W.M.; Cho, J.Y.; Park, H.J.; Kim, T.W.; Choe, N.-H.; Kim, S.K.; Rhee, M.H. In vitro anti-oxidative and anti-inflammatory effects of solvent-extracted fractions from Suaeda asparagoides. Die Pharm.-Int. J. Pharm. Sci. 2007, 62, 453–458. [Google Scholar] [CrossRef]
- Mzoughi, Z.; Abdelhamid, A.; Rihouey, C.; Le Cerf, D.; Bouraoui, A.; Majdoub, H. Optimized extraction of pectin-like polysaccharide from Suaeda fruticosa leaves: Characterization, antioxidant, anti-inflammatory and analgesic activities. Carbohydr. Polym. 2018, 185, 127–137. [Google Scholar] [CrossRef]
- Oueslati, S.; Ksouri, R.; Falleh, H.; Pichette, A.; Abdelly, C.; Legault, J. Phenolic content, antioxidant, anti-inflammatory and anticancer activities of the edible halophyte Suaeda fruticosa Forssk. Food Chem. 2012, 132, 943–947. [Google Scholar] [CrossRef]
- Abd El-Latif, R.R.; Mansour, R.M.; Sharaf, M.; Farag, A. Three new flavonol glycosides from Suaeda maritima. J. Asian Nat. Prod. Res. 2014, 16, 434–439. [Google Scholar] [CrossRef]
- Saleem, H.; Khurshid, U.; Sarfraz, M.; Tousif, M.I.; Alamri, A.; Anwar, S.; Alamri, A.; Ahmad, I.; Abdallah, H.H.; Mahomoodally, F.M. A comprehensive phytochemical, biological, toxicological and molecular docking evaluation of Suaeda fruticosa (L.) Forssk.: An edible halophyte medicinal plant. Food Chem. Toxicol. 2021, 154, 112348. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Shao, X.; Zhang, W.; Sun, T.; Ding, Y.; Lin, Z.; Li, Y. Genus Suaeda: Advances in Phytology, Chemistry, Pharmacology and Clinical Application (1895–2021). Pharmacol. Res. 2022, 179, 106203. [Google Scholar] [CrossRef] [PubMed]
- AL-Alamiry, A.A.N. Comparative study of antibacterial effect of ethanolic leaf extracts Suaeda aegyptiaca plant and some antibiotics in the growth of pathogenic bacteria. Univ. Thi-Qar J. Med. 2015, 9, 102–112. [Google Scholar]
- Ao, C.; Li, A.; Elzaawely, A.A.; Xuan, T.D.; Tawata, S. Evaluation of antioxidant and antibacterial activities of Ficus microcarpa L. fil. extract. Food Control 2008, 19, 940–948. [Google Scholar] [CrossRef]
- Ahmed, E.M.; Kassab, A.E.; El-Malah, A.A.; Hassan, M.S. Synthesis and biological evaluation of pyridazinone derivatives as selective COX-2 inhibitors and potential anti-inflammatory agents. Eur. J. Med. Chem. 2019, 171, 25–37. [Google Scholar] [CrossRef]
- Mosmann, T. Rapid colorimetric assay for cellular growth and survival: Application to proliferation and cytotoxicity assays. J. Immunol. Methods 1983, 65, 55–63. [Google Scholar] [CrossRef]
- Dewi, K.; Widyarto, B.; Erawijantari, P.P.; Widowati, W. In vitro study of Myristica fragrans seed (Nutmeg) ethanolic extract and quercetin compound as anti-inflammatory agent. Int. J. Res. Med Sci. 2015, 3, 2303–2310. [Google Scholar] [CrossRef]
- Mohammed, H.A.; Al-Omar, M.S.; Aly, M.S.; Hegazy, M.M. Essential oil constituents and biological activities of the halophytic plants, Suaeda vermiculata Forssk and Salsola cyclophylla Bakera growing in Saudi Arabia. J. Essent. Oil Bear. Plants 2019, 22, 82–93. [Google Scholar] [CrossRef]
- Saïdana, D.; Mahjoub, S.; Boussaada, O.; Chriaa, J.; Mahjoub, M.A.; Chéraif, I.; Daami, M.; Mighri, Z.; Helal, A.N. Antibacterial and antifungal activities of the essential oils of two Saltcedar species from Tunisia. l and antifungal activities of the essential oils of two Saltcedar species from Tunisia. J. Am. Oil Chem. Soc. 2008, 85, 817–826. [Google Scholar] [CrossRef]
- FADIPE, L.A.; Haruna, A.; Mohammed, I. Antibacterial activity of 1, 2-benzenedicarboxylic acid, dioctyl ester isolated from the ethyl acetate soluble sub-portion of the unripe fruits of Nauclea latifolia. Int. J. Pure Appl. Biosci. 2014, 2, 223–230. [Google Scholar]
- Joghee, S.; Kalarikkal, S.P.; Sundaram, G.M.; Kumar, T.D.A.; Chidambaram, S.B. Chemical profiling and in-vitro anti-inflammatory activity of bioactive fraction (s) from Trichodesma indicum (L.) R. Br. against LPS induced inflammation in RAW 264.7 murine macrophage cells. J. Ethnopharmacol. 2021, 279, 114235. [Google Scholar] [CrossRef]
- Youssif, K.A.; Elshamy, A.M.; Rabeh, M.A.; Gabr, N.; Afifi, W.M.; Salem, M.A.; Albohy, A.; Abdelmohsen, U.R.; Haggag, E.G. Cytotoxic potential of green synthesized silver nanoparticles of Lampranthus coccineus extracts, metabolic profiling and molecular docking study. ChemistrySelect 2020, 5, 12278–12286. [Google Scholar] [CrossRef]
- Nguyen, D.; Nguyen, D.H.; Hwa-La, L.; Lee, H.-B.; Shin, J.-H.; Kim, E.-K. Inhibition of melanogenesis by dioctyl phthalate isolated from Nigella glandulifera Freyn. J. Microbiol. Biotechnol. 2007, 17, 1585–1590. [Google Scholar] [PubMed]
- Pelo, S.P.; Adebo, O.A.; Green, E. Chemotaxonomic profiling of fungal endophytes of Solanum mauritianum (alien weed) using gas chromatography high resolution time-of-flight mass spectrometry (GC-HRTOF-MS). Metabolomics 2021, 17, 1–13. [Google Scholar] [CrossRef]
- Kebbi, S.; Noman, L.; Demirtas, I.; Bensouici, C.; Adem, S.; Benayache, S.; Benayache, F.; Seghiri, R.; Gok, M. In vitro Antioxidant and Anticholinesterase Activities of Senecio massaicus Essential Oil and Its Molecular Docking Studies as a Potential Inhibitor of COVID-19 and Alzheimer’s Diseases. J. Biol. Act. Prod. Nat. 2021, 11, 380–394. [Google Scholar] [CrossRef]
- Bhardwaj, M.; Sali, V.K.; Mani, S.; Vasanthi, H.R. Neophytadiene from Turbinaria ornata suppresses LPS-induced inflammatory response in RAW 264.7 macrophages and Sprague Dawley rats. Inflammation 2020, 43, 937–950. [Google Scholar] [CrossRef]
- Kim, S.J.; Chung, W.S.; Kim, S.S.; Ko, S.G.; Um, J.Y. Antiinflammatory effect of Oldenlandia diffusa and its constituent, hentriacontane, through suppression of caspase-1 activation in mouse peritoneal macrophages. Phytother. Res. 2011, 25, 1537–1546. [Google Scholar] [CrossRef]
- Khajuria, V.; Gupta, S.; Sharma, N.; Kumar, A.; Lone, N.A.; Khullar, M.; Dutt, P.; Sharma, P.R.; Bhagat, A.; Ahmed, Z. Anti-inflammatory potential of hentriacontane in LPS stimulated RAW 264.7 cells and mice model. Biomed. Pharmacother. 2017, 92, 175–186. [Google Scholar] [CrossRef]
- Avoseh, O.N.; Mtunzi, F.M.; Ogunwande, I.A.; Ascrizzi, R.; Guido, F. Albizia lebbeck and Albizia zygia volatile oils exhibit anti-nociceptive and anti-inflammatory properties in pain models. J. Ethnopharmacol. 2021, 268, 113676. [Google Scholar] [CrossRef]
- Wei, G.; Kong, L.; Zhang, J.; Ma, C.; Wu, X.; Li, X.; Jiang, H. Essential oil composition and antibacterial activity of Lindera nacusua (D. Don) Merr. Nat. Prod. Res. 2016, 30, 2704–2706. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, Y.H.; Ghaidaa, J.M.; Imad, H.H. Analysis of bioactive chemical compounds of Nigella sativa using gas chromatography-mass spectrometry. J. Pharmacogn. Phytother. 2016, 8, 8–24. [Google Scholar] [CrossRef]
- Ravikumar, S.; Gnanadesigan, M.; Inbaneson, S.J.; Kalaiarasi, A. Hepatoprotective and antioxidant properties of Suaeda maritima (L.) Dumort ethanolic extract on concanavalin—A induced hepatotoxicity in rats. Indian J. Pharmacol. Exp. Ther. 2011, 49, 455–460. [Google Scholar]
- Ali, I.; Bibi, S.; Hussain, H.; Bano, F.; Ali, S.; Khan, S.W.; Ahmad, V.U.; Al-Harrasi, A. Biological activities of Suaeda heterophylla and Bergenia stracheyi. Asian Pac. J. Trop. Dis. 2014, 4, S885–S889. [Google Scholar] [CrossRef]
- Saleh, K.A.; Albinhassan, T.H.; Al-Ghazzawi, A.M.; Mohaya, A.; Shati, A.A.; Ayoub, H.J.; Abdallah, Q.M. Anticancer property of hexane extract of Suaeda fruticose plant leaves against different cancer cell lines. Trop. J. Pharm. Res. 2020, 19, 129–136. [Google Scholar] [CrossRef]

| Compound Name | RT | Molecular Formula | % Area | |||
|---|---|---|---|---|---|---|
| Cold n-Hexane Extraction (CHE) | Hot n-Hexane Extraction (HHE) | Hydro-Distillation Extraction (HDE) | ||||
| 1. | 2-allyl-5-t-butylhydroquinone | 14.40 | C13H18O2 | 0.44 | ND | ND |
| 2. | 2(4H)-Benzofuranone, 5,6,7,7a-tetrahydro-4,4,7a-trimethyl-, (R) | 14.76 | C11H16O2 | ND | 0.57 | 0.48 |
| 3. | 9-eicosene, (e)- | 19.19 | C20H40 | 1.22 | 0.61 | ND |
| 4. | Neophytadiene | 19.93 | C20H38 | 3.43 | 5.70 | 3.40 |
| 5. | Hexahydrofarnesyl acetone | 20.00 | C18H36O | 1.76 | 1.14 | 0.42 |
| 6. | Cyclopropanenonanoic acid, 2-[(2-butylcyclopropyl) methyl]-, methyl ester | 20.32 | C21H38O2 | ND | 0.84 | 0.47 |
| 7. | Dibutyl phthalate | 20.33 | C16H22O4 | 0.88 | ND | ND |
| 8. | Phytol, acetate | 20.58 | C22H42O2 | 0.51 | 0.93 | 0.54 |
| 9. | 7,9-Di-tert-butyl-1-oxaspiro (4,5)deca-6,9-diene-2,8-dione | 21.13 | C17H24O3 | ND | 0.66 | ND |
| 10. | Cis-11-Eicosenoic acid | 21.17 | C20H38O2 | 0.83 | ND | ND |
| 11. | Heptacos-1-ene | 22.25 | C21H44O | 1.68 | 1.22 | ND |
| 12. | Phytol | 23.99 | C20H40O | 0.84 | 0.74 | ND |
| 13. | Nonacos-1-ene | 25.05 | C29H58 | 1.09 | ND | ND |
| 14. | E-8-Methyl-9-tetradecen-1-ol acetate | 25.61 | C17H32O2 | ND | 1.16 | ND |
| 15. | 4,8,12,16-Tetramethylheptadecan-4-olide | 27.12 | C21H40O2 | 0.93 | 0.70 | 0.26 |
| 16. | 1-nonadecene | 27.63 | C19H38 | 1.08 | 0.75 | ND |
| 17. | Stigmasterol | 28.50 | C29H48O | ND | 6.35 | 3.52 |
| 18. | 1-heptatriacotanol | 29.00 | C37H76O | ND | 4.34 | 2.22 |
| 19. | 1,2-benzenedicarboxylic acid diisooctyl ester | 29.50 | C24H38O4 | 19.28 | 13.12 | 57.87 |
| 20. | 9-octadecenoic acid (z) | 30.03 | C18H34O2 | 0.63 | ND | ND |
| 21. | Stigmast-5-en-3-ol, (3α) | 31.08 | C29H50O | ND | 3.58 | 2.01 |
| 22. | Hentriacontane | 31.23 | C31H64 | 3.40 | 3.40 | 1.62 |
| 23. | Cholestanol | 31.46 | C27H48O | ND | 1.15 | ND |
| 24. | Undec-10-ynoic acid, octadecyl ester | 31.56 | C29H54O2 | ND | 1.75 | 3.37 |
| 25. | Octacosanol | 31.74 | C28H58O | ND | 6.67 | 2.08 |
| 26. | Tert-Hexadecanethiol | 32.27 | C16H34S | 0.46 | ND | ND |
| 27. | Dotriacontane | 32.32 | C32H66 | 0.49 | ND | ND |
| 28. | 2,2-dideutero octadecanal | 32.72 | C18H34D2O | 1.65 | 1.37 | ND |
| 29. | Isochiapin b | 32.92 | C19H22O6 | 1.26 | 0.71 | 0.38 |
| 30. | 17-pentatriacontene | 33.05 | C35H70 | ND | 0.68 | ND |
| 31. | 3′,4′,7-trimethylquercetin | 33.16 | C18H16O7 | 1.09 | ND | 0.54 |
| 32. | Heptacosane | 33.25 | C27H56 | 0.44 | ND | ND |
| 33. | Docosane | 33.30 | C22H46 | 0.42 | ND | ND |
| 34. | 11-decyldocosane | 33.47 | C32H66 | ND | 29.20 | 13.38 |
| 35. | 2-methyloctacosane | 33.51 | C29H60 | 48.72 | ND | ND |
| 36. | E-10,13,13-Trimethyl-11-tetradecen-1-ol acetate | 33.90 | C19H36O2 | 0.58 | ND | ND |
| 37. | Hexadecenoic acid, phenylmethyl ester | 34.08 | C23H38O2 | ND | ND | 1.19 |
| 38. | Octadecane, 3-ethyl-5-(2-ethylbutyl) | 34.47 | C26H54 | 0.80 | 0.73 | 0.37 |
| 39. | Cis-1-Chloro-9-octadecene | 34.78 | C18H35Cl | ND | ND | 3.05 |
| 40. | Triacontyl acetate | 34.82 | C32H64O2 | ND | 7.05 | ND |
| 41. | Ethanol, 2-(9-octadecenyloxy)-, (Z) | 34.94 | C20H40O2 | 2.43 | 1.44 | ND |
| 42. | 6,7-Epoxypregn-4-ene-9,11,18-triol-3,20-dione, 11,18-diacetate | 35.12 | C25H32O8 | 0.60 | 0.79 | 1.03 |
| 43. | 9,12,15-octadecatrienoic acid, 2,3-bis[(trimethylsilyl)oxy]propyl ester, (z,z,z) | 35.37 | C27H52O4Si2 | 0.34 | ND | ND |
| Total percentage of identified components | 97.28% | 97.35% | 98.65% | |||
| Extracts | Cytotoxicity (IC50 µg/mL) | Antioxidant Activity | |
|---|---|---|---|
| HCT-116 | Caco2 | DPPH (IC50 mg/mL) | |
| HHE | 32.51 ± 1.8 | 12.42 ± 0.63 | 1.56 ± 0.57 |
| CHE | 11.18 ± 0.62 a | 8.11 ± 0.41a | 3.39 ± 0.44 a |
| HDE | 46.21 ± 2.57 a,b | 32.35 ± 1.65 a,b | 0.36 ± 0.17 a,b |
| Staurosporine | 5.25 ± 0.29 a,b,c | 3.69 ± 0.19 a,b,c | --- |
| Ascorbic acid | --- | --- | 0.26 ± 0.17 a,b |
| Extracts | COX-1 | COX-2 | TNF-α (LPS-Stimulated Raw264.7 Cells) |
|---|---|---|---|
| (IC50 µg/mL) | Pg/mL | ||
| HHE | 28.88 ± 1.46 | 15.62 ± 0.69 | 868.80 ± 3.0 |
| CHE | 24.41 ± 1.24 | 7.25 ± 0.32 a | 836.20 ± 25.1 |
| HDE | 5.50 ± 0.28 a,b | 2.59 ± 0.11 a,b | 572.20 ± 17.4 a,b |
| Indomethacin® | 0.14 ± 0.01 a,b,c | 0.71 ± 0.03 a,b,c | --- |
| Celecoxib® | 15.05 ± 0.76 a,b,c,d | 1.11 ± 0.05 a,b,c | 442.80 ± 14.6 a,b |
| Control | --- | --- | 1755 ± 117 a,b,c,e |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amin, E.; Elwekeel, A.; Alshariedh, N.F.; Abdel-Bakky, M.S.; Hassan, M.H.A. GC-MS Analysis and Bioactivities of the Essential Oil of Suaeda aegyptiaca. Separations 2022, 9, 439. https://doi.org/10.3390/separations9120439
Amin E, Elwekeel A, Alshariedh NF, Abdel-Bakky MS, Hassan MHA. GC-MS Analysis and Bioactivities of the Essential Oil of Suaeda aegyptiaca. Separations. 2022; 9(12):439. https://doi.org/10.3390/separations9120439
Chicago/Turabian StyleAmin, Elham, Ahlam Elwekeel, Nasrah F. Alshariedh, Mohamed Sadek Abdel-Bakky, and Marwa H. A. Hassan. 2022. "GC-MS Analysis and Bioactivities of the Essential Oil of Suaeda aegyptiaca" Separations 9, no. 12: 439. https://doi.org/10.3390/separations9120439
APA StyleAmin, E., Elwekeel, A., Alshariedh, N. F., Abdel-Bakky, M. S., & Hassan, M. H. A. (2022). GC-MS Analysis and Bioactivities of the Essential Oil of Suaeda aegyptiaca. Separations, 9(12), 439. https://doi.org/10.3390/separations9120439