Large Lobular Capillary Hemangioma Associated with Ingrown Toenail: Histopathological Features and Case Report
Abstract
:1. Introduction
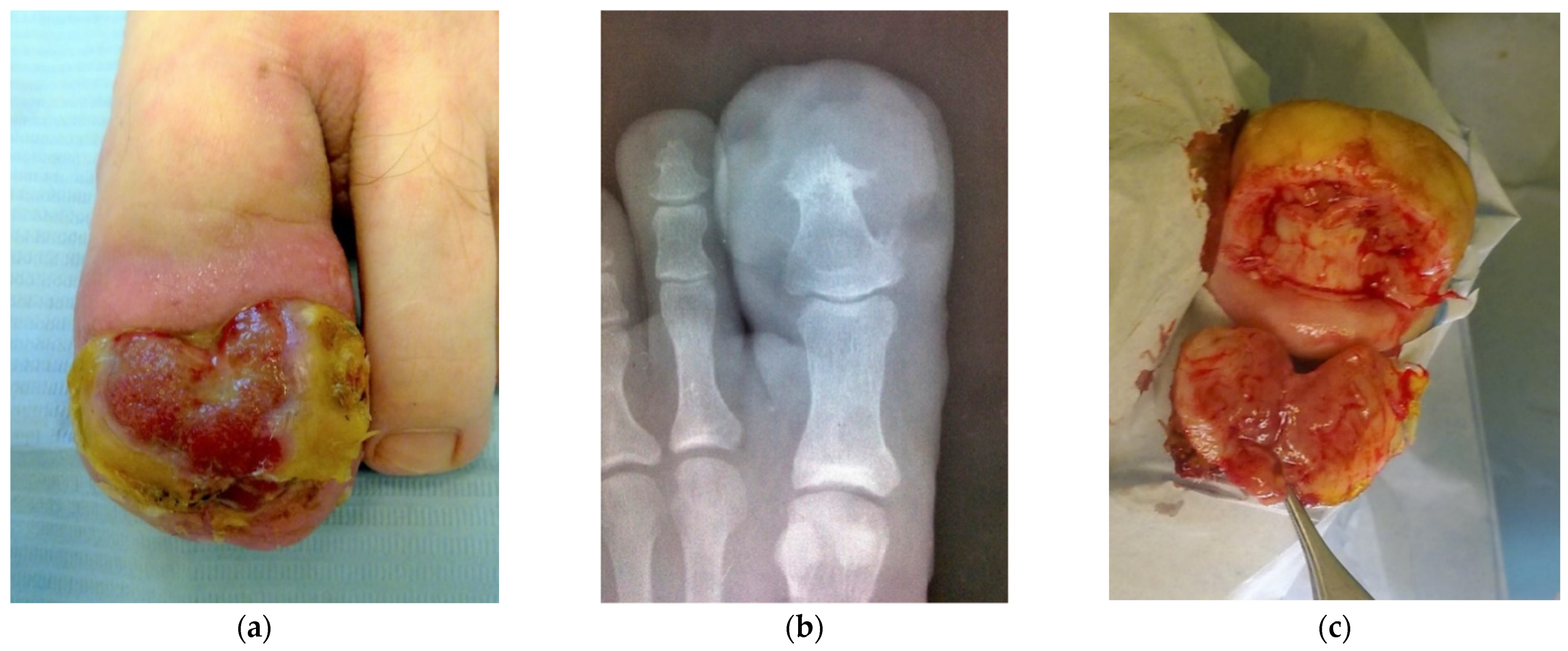
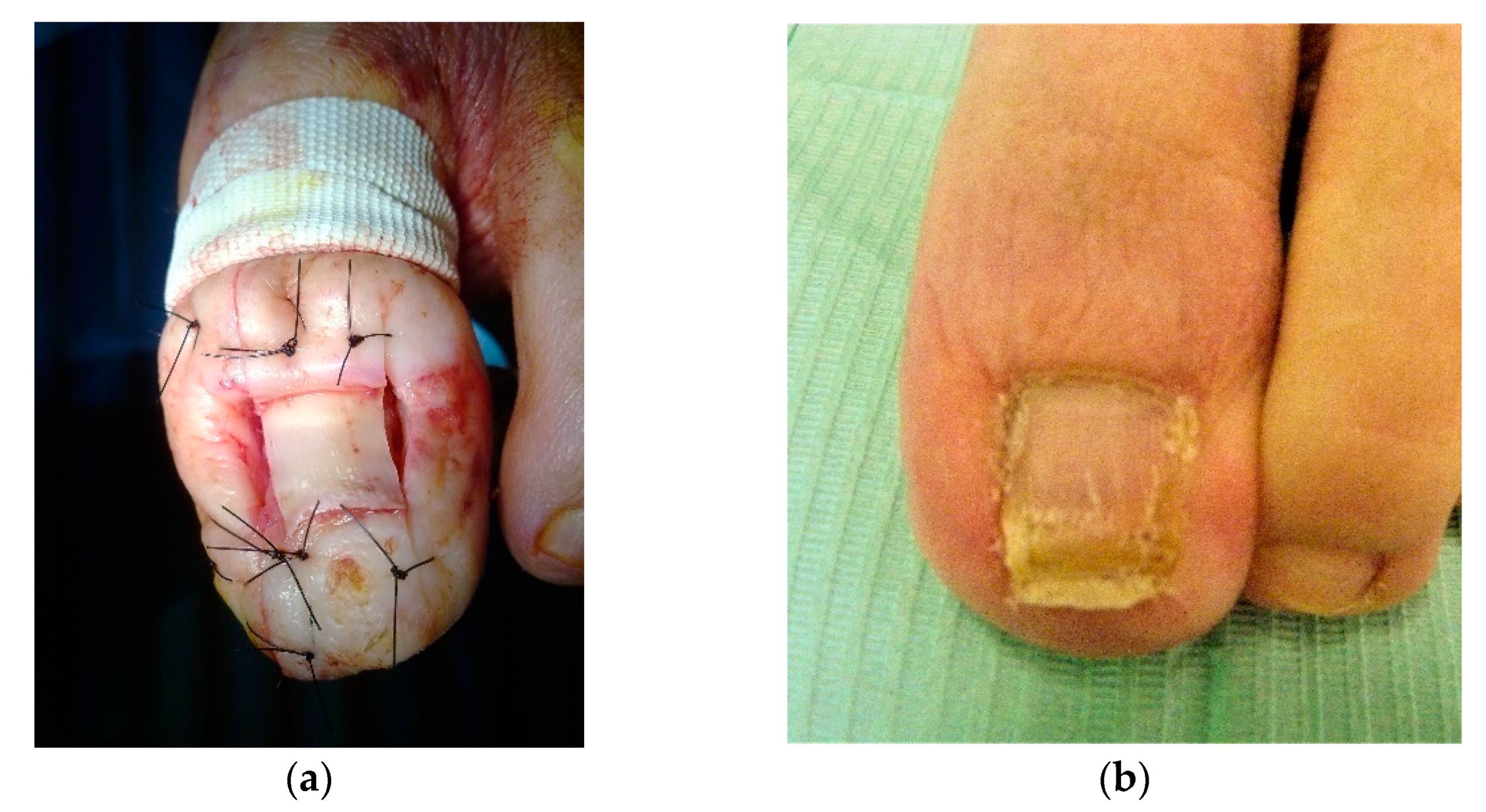
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Epivatianos, A.; Antoniades, D.; Zaraboukas, T.; Zairi, E.; Poulopoulos, A.; Kiziridou, A.; Iordanidis, S. Pyogenic granuloma of the oral cavity: Comparative study of its clinicopathological and immunohistochemical features. Pathol. Int. 2005, 55, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Kline, A. Onychocryptosis: A simple classification system. Foot Ankle J. 2008, 1, 6–13. [Google Scholar]
- Piraccini, B.M.; Bellavista, S.; Misciali, C.; Tosti, A.; de Berker, D.; Richert, B. Periungual and subungual pyogenic granuloma. Br. J. Dermatol. 2010, 163, 941–953. [Google Scholar] [CrossRef] [PubMed]
- Adnan, A.; Bajuri, M.Y.; Shukur, M.H.; Subanesh, S.; Das, S. Malignant melanoma masqueraded as ingrown toe nail. Clin. Ter. 2014, 165, 41–45. [Google Scholar] [PubMed]
- Abdul, W.; O’Neill, B.J.; Perera, A. Marjolin’s squamous cell carcinoma of the hallux following recurrent ingrown toenail infections. BMJ Case. Rep. 2017, 2017, bcr2017219715. [Google Scholar] [CrossRef] [PubMed]
- Fölster-Holst, R.; Rahmatpour Rokni, G.; Bagot, M.; Lallas, A.; Szepietowski, J.; Lotti, T.; Goldust, M. Uncommon presentation of pigmented paraungual basal cell carcinoma on the first toe treated with total excision. Dermatol. Ther. 2020, 33, e13289. [Google Scholar] [CrossRef] [PubMed]
- Korekawa, A.; Kaneko, T.; Nakano, H.; Sawamura, D. Pyogenic granuloma-like Kaposi’s sarcoma on the first toe. J. Dermatol. 2018, 45, e177–e178. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Flores, A.; Martínez-Nova, A.; Salgado-Fernandez, S. Ingrowntoenail: Histopathologic and immunohistochemical study. Am. J. Dermatol. 2009, 31, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Lemont, H.; Brady, J. Amelanotic melanoma masquerading as an ingrown toenail. J. Am. Podiatr. Med. Assoc. 2002, 92, 306–307. [Google Scholar] [CrossRef] [PubMed]
- Samaras, D.J.; Kingsford, A.C. Surgical management of extensive hypertrophic scarring of the halluces secondary to a decade of untreated onychocryptosis: An illustrative case report. SAGE Open Med. Case Rep. 2017, 5, 2050313X17740514. [Google Scholar] [CrossRef] [PubMed]
- Engel, E.; Butler, M.; Anain, J., Jr. Leiomyosarcoma of the foot: A case study. J. Am. Podiatr. Med. Assoc. 2007, 97, 475–479. [Google Scholar] [CrossRef] [PubMed]
- Mills, S.E.; Cooper, P.H.; Fechner, R.E. Lobular capillary hemangioma: The underlying lesion of pyogenic granuloma. A study of 73 cases from the oral and nasal mucous membranes. Am. J. Surg. Pathol. 1980, 4, 470–479. [Google Scholar] [CrossRef] [PubMed]
- Grosshans, E. Pyogenic granuloma:Who are you? J. Eur. Acad. Dermatol. Venereol. 2001, 15, 106–107. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, J.L.; Moraes, R.M.; Carvalho, B.F.C.; Nascimento, A.O.; Milhan, N.V.M.; Anbinder, A.L. Oral pyogenic granuloma: An 18-year retrospective clinicopathological and immunohistochemical study. J. Cutan. Pathol. 2021, 48, 863–869. [Google Scholar] [CrossRef] [PubMed]
- Shalin, S.C.; Ferriger, T.; Cassarino, D.S. PAS and GMS utility in derpathopatology. Review of the current medical literature. J. Cutan. Pathol. 2020, 47, 1096–1102. [Google Scholar] [CrossRef] [PubMed]
- Godfraind, C.; Calicchio, M.L.; Kozakewich, H. Pyogenic granuloma, an impaired wound healing process, linked to vascular growth driven by FLT4 and the nitric oxide pathway. Mod. Pathol. 2013, 26, 247–255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakamura, T. Apoptosis and expression of Bax/Bcl-2 proteins in pyogenic granuloma: A comparative study with granulation tissue and capillary hemangioma. J. Cutan. Pathol. 2000, 27, 400–405. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Córdoba-Fernández, A.; Jiménez-Cristino, M.D.; Córdoba-Jiménez, V.E. Large Lobular Capillary Hemangioma Associated with Ingrown Toenail: Histopathological Features and Case Report. Dermatopathology 2022, 9, 271-276. https://doi.org/10.3390/dermatopathology9030031
Córdoba-Fernández A, Jiménez-Cristino MD, Córdoba-Jiménez VE. Large Lobular Capillary Hemangioma Associated with Ingrown Toenail: Histopathological Features and Case Report. Dermatopathology. 2022; 9(3):271-276. https://doi.org/10.3390/dermatopathology9030031
Chicago/Turabian StyleCórdoba-Fernández, Antonio, María Dolores Jiménez-Cristino, and Victoria Eugenia Córdoba-Jiménez. 2022. "Large Lobular Capillary Hemangioma Associated with Ingrown Toenail: Histopathological Features and Case Report" Dermatopathology 9, no. 3: 271-276. https://doi.org/10.3390/dermatopathology9030031
APA StyleCórdoba-Fernández, A., Jiménez-Cristino, M. D., & Córdoba-Jiménez, V. E. (2022). Large Lobular Capillary Hemangioma Associated with Ingrown Toenail: Histopathological Features and Case Report. Dermatopathology, 9(3), 271-276. https://doi.org/10.3390/dermatopathology9030031





