Primary Localized Cutaneous Nodular Amyloidosis and Limited Cutaneous Systemic Sclerosis: Additional Cases with Dermatoscopic and Histopathological Correlation of Amyloid Deposition
Abstract
:1. Introduction
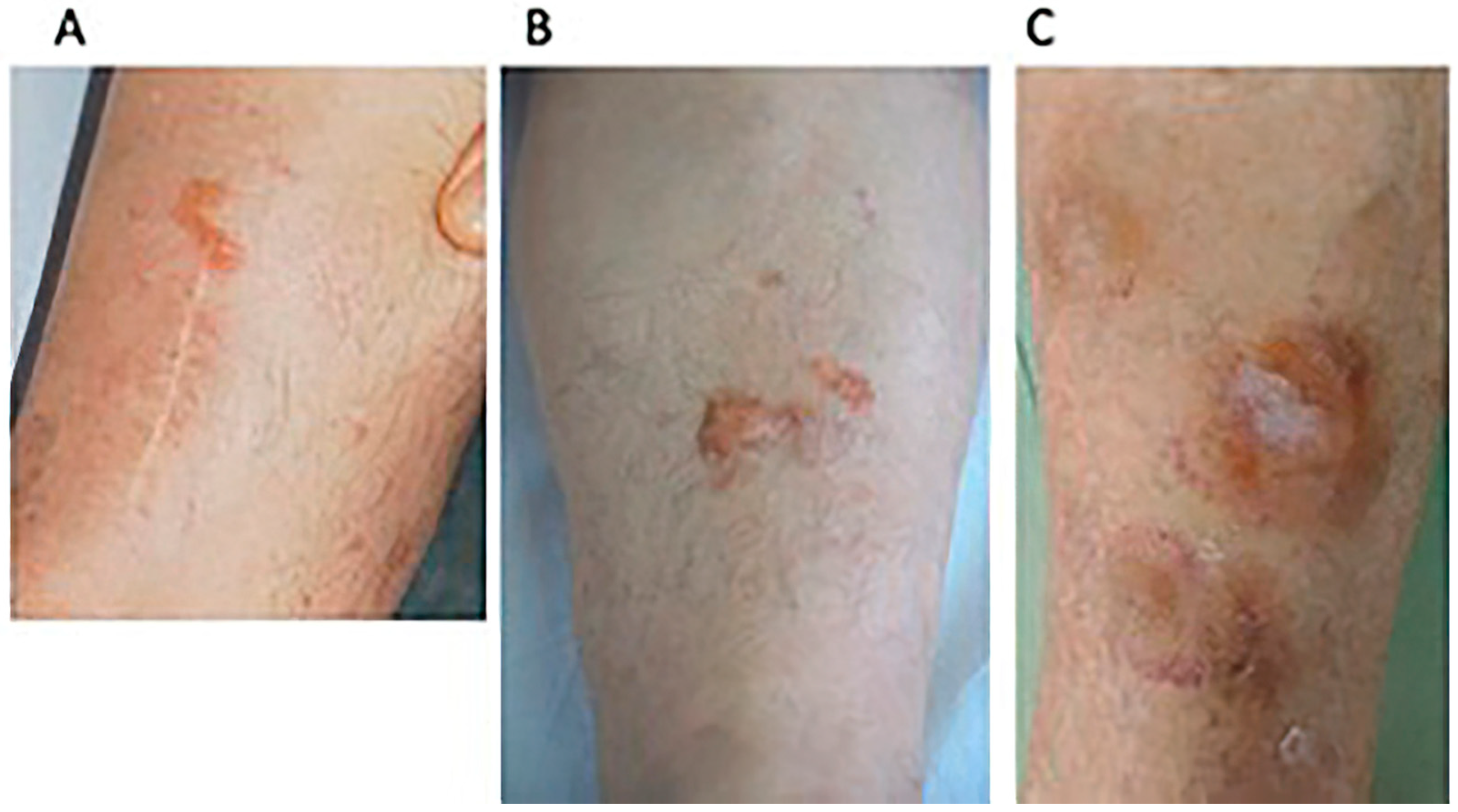
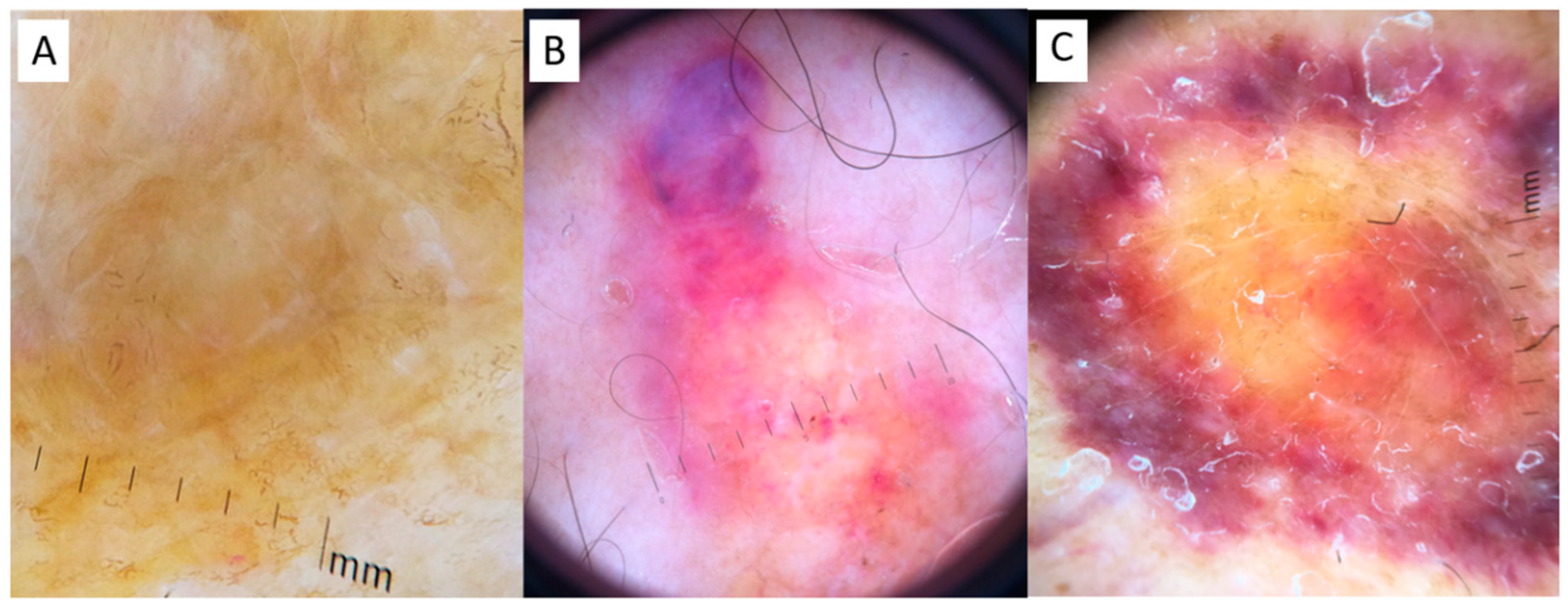
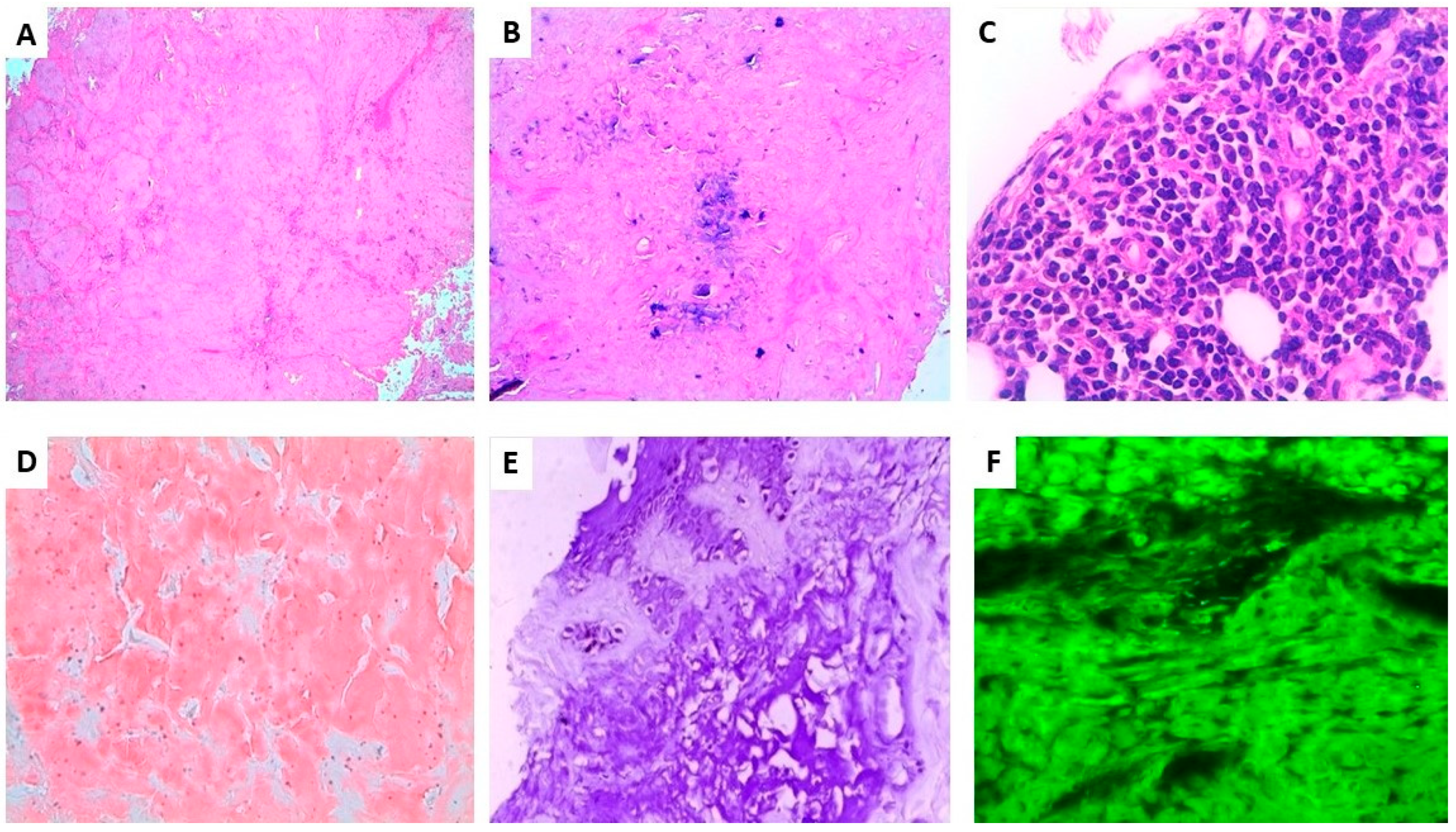
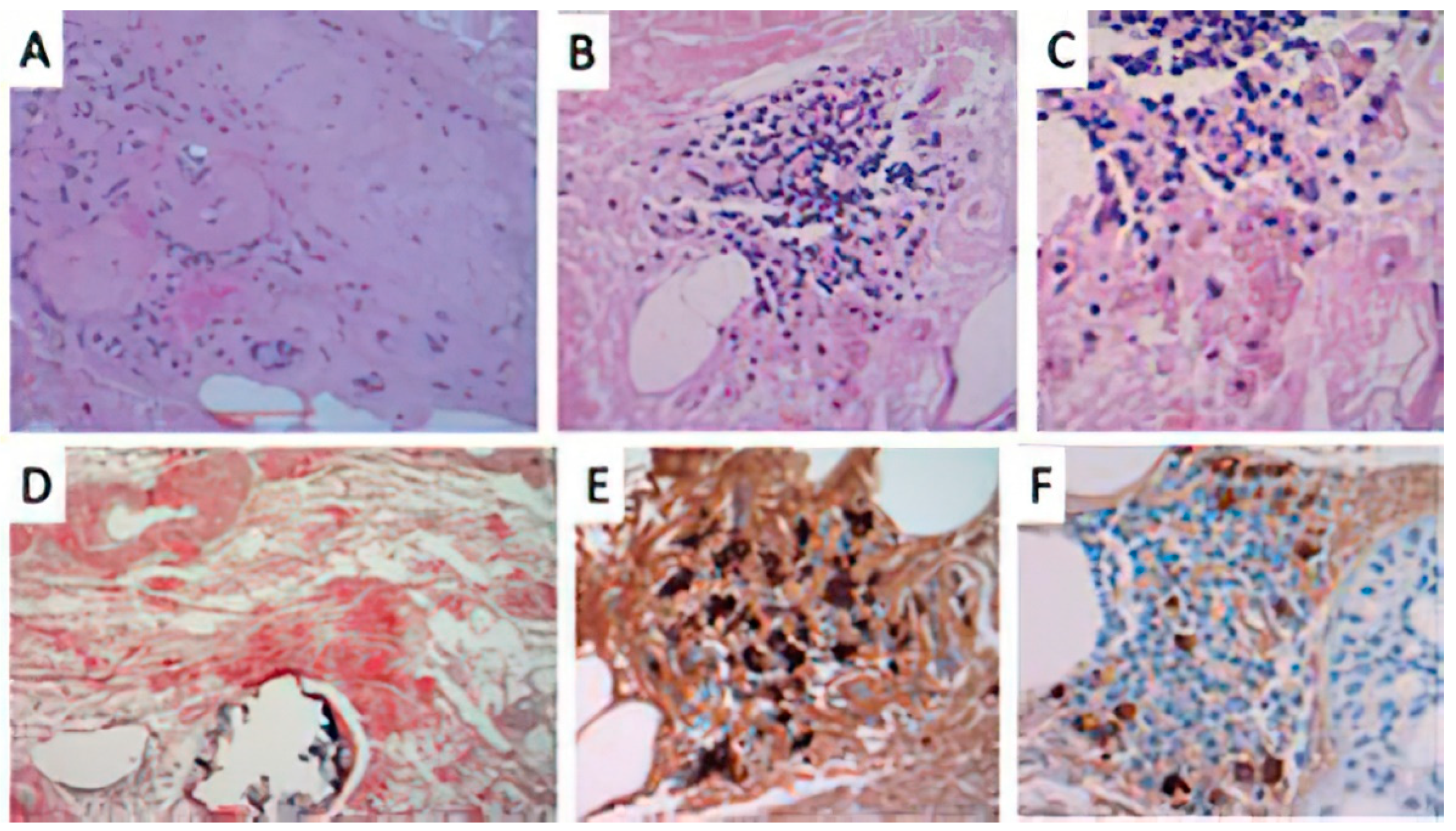
2. Presentation of Cases
2.1. Case 1
2.2. Case 2
2.3. Case 3
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Falk, R.H.; Comenzo, R.L.; Skinner, M. The Systemic Amyloidoses. N. Engl. J. Med. 1997, 337, 898–909. [Google Scholar] [CrossRef]
- Fernandez-Flores, A. Cutaneous Amyloidosis: A Concept Review. Am. J. Dermatopathol. 2012, 34, 1–17. [Google Scholar] [CrossRef]
- Evers, M.; Baron, E.; Zaim, M.T.; Han, A. Papules and Plaques on the Nose. Nodular Localized Primary Cutaneous Amyloidosis. Arch. Dermatol. 2007, 143, 535–540. [Google Scholar]
- Hagari, Y.; Mihara, M.; Hagari, S. Nodular Localized Cutaneous Amyloidosis: Detection of Monoclonality of Infiltrating Plasma Cells by Polymerase Chain Reaction. Br. J. Dermatol. 1996, 135, 630–633. [Google Scholar] [CrossRef]
- Cai, Y.X.; Li, S.J.; Zhou, Y.; Li, W.; Fan, Y.M. Immunohistochemical Study of Immunoglobulin Light Chains and Inflammatory Cells in a Patient with Localized Primary Cutaneous Nodular Amyloidosis. J. Eur. Acad. Dermatol. Venereol. 2016, 30, 469–470. [Google Scholar] [CrossRef]
- Moon, A.O.; Calamia, K.T.; Walsh, J.S. Nodular Amyloidosis: Review and Long-Term Follow-up of 16 Cases. Arch. Dermatol. 2003, 139, 1157–1159. [Google Scholar] [CrossRef] [Green Version]
- Woollons, A.; Black, M.M. Nodular Localized Primary Cutaneous Amyloidosis: A Long-Term Follow-up Study. Br. J. Dermatol. 2001, 145, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Yoneyama, K.; Tochigi, N.; Oikawa, A.; Shinkai, H.; Utani, A. Primary Localized Cutaneous Nodular Amyloidosis in a Patient with Sjögren’s Syndrome: A Review of the Literature. J. Dermatol. 2005, 32, 120–123. [Google Scholar] [CrossRef] [PubMed]
- Meijer, J.M.; Schönland, S.; Palladini, G.; Merlini, G.; Hegenbart, U.; Ciocca, O.; Perfetti, V.; Leijsma, M.K.; Bootsma, H.; Hazenberg, B. Sjögren’s syndrome and localized nodular cutaneous amyloidosis: Coincidence or a distinct clinical entity? Arthritis Rheum. 2008, 58, 1992–1999. [Google Scholar] [CrossRef] [PubMed]
- Brown, A.J.; Spicknall, K.E.; Mutasim, D.F. Multiple Lesions of Primary Cutaneous Nodular Amyloidosis in Sjögren Syndrome. Am. Acad. Dermatol. 2012, 67, e267–e268. [Google Scholar] [CrossRef]
- Kikuchi, N.; Sakai, E.; Nishibu, A.; Ohtsuka, M.; Yamamoto, T. Primary Localized Cutaneous Amyloidosis in Patients with Scleroderma. Acta Derm. Venereol. 2010, 90, 326–327. [Google Scholar] [CrossRef]
- Marano, A.L.; Selim, M.A.; Cardones, A.R.; Burton, C.S. Nodular amyloidosis in a patient with systemic scleroderma. Dermatol. Online J. 2018, 2, 9. [Google Scholar]
- Goettsche, L.S.; Moye, M.S.; Tschetter, A.J.; Stone, M.S.; Wanat, K.A. Three Cases of Localized Cutaneous Nodular Amyloidosis in Patients with Limited Systemic Sclerosis and a Brief Literature Review. Int. J. Womens Dermatol. 2017, 3, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Tong, P.L.; Walker, W.A.; Glancy, R.J.; Cooney, J.P.; Gebauer, K. Primary localized cutaneous nodular amyloidosis successfully treated with cyclophosphamide. Australas. J. Dermatol. 2011, 54, e12–e15. [Google Scholar] [CrossRef] [PubMed]
- Damian, D.L.; Bertouch, J.V. Images in dermatology. A plethora of protein. Primary localized cutaneous nodular amyloidosis. Am. J. Med. 2010, 123, 904–906. [Google Scholar] [CrossRef]
- Shiman, M.; Ricotti, C.; Miteva, M.; Kerdel, F.; Romanelli, P. Primary localized cutaneous nodular amyloidosis associated with CREST (calcinosis, Raynaud’s phenomenon, esophageal motility disorders, sclerodactyly, and telangiectasia) syndrome. Int. J. Dermatol. 2010, 49, 229–230. [Google Scholar] [CrossRef] [PubMed]
- Summers, E.M.; Kendrick, C.G. Primary Localized Cutaneous Nodular Amyloidosis and CREST Syndrome: A Case Report and Review of the Literature. Cutis 2008, 82, 55–59. [Google Scholar] [PubMed]
- Sgouros, D.; Apalla, Z.; Ioannides, D.; Katoulis, A.; Rigopoulos, D.; Sotiriou, E.; Stratigos, A.; Vakirlis, E.; Lallas, A. Dermoscopy of Common Inflammatory Disorders. Dermatol. Clin. 2018, 36, 359–368. [Google Scholar] [CrossRef]
- Chuang, Y.Y.; Lee, D.D.; Lin, C.S.; Chang, Y.J.; Tanaka, M.; Chang, Y.T.; Liu, H.N. Characteristic Dermoscopic Features of Primary Cutaneous Amyloidosis: A Study of 35 Cases. Br. J. Dermatol. 2012, 167, 548–554. [Google Scholar] [CrossRef]
- Rongioletti, F.; Atzori, L.; Ferreli, C.; Pinna, A.; Aste, N.; Pau, M. A Unique Dermoscopy Pattern of Primary Cutaneous Nodular Amyloidosis Mimicking a Granulomatous Disease. J. Am. Acad. Dermatol. 2016, 74, e9–e10. [Google Scholar] [CrossRef]
- Di Meo, N.; Noal, C.; Fadel, M.; Trevisan, G. Yellow teardrop-like structures in primary nodular skin amyloidosis. G. Ital. Dermatol. Venereol. 2018, 153, 118–119. [Google Scholar] [PubMed]
- Balestri, R.; LA Placa, M.; Bardazzi, F.; Rech, G. Dermoscopic subpatterns of granulomatous skin diseases. J. Am. Acad. Dermatol. 2013, 69, e217–e218. [Google Scholar] [CrossRef] [PubMed]
- Weidner, T.; Illing, T.; Elsner, P. Primary Localized Cutaneous Amyloidosis: A Systematic Treatment Review. Am. J. Clin. Dermatol. 2017, 18, 629–642. [Google Scholar] [CrossRef] [PubMed]
| Age | Sex | Site of PLCNA | PLCNA Duration | Scleroderma Duration before PLCNA | Histopathological Findings | Congo Red | Ref. |
|---|---|---|---|---|---|---|---|
| 61 | f | Left lower leg | 3 years | 1 year | Amyloid extending from the superficial derma to the subcutis | + | [17] |
| 83 | f | Bilateral lower legs | 25 years | Not reported | Diffuse eosinophilic aggregates of amorphous material in the superficial portion of the dermis, around vascular channels and adnexal structures with prominent plasmacells infiltrate. Deposits positive for k and lambda chains | + | [16] |
| 61 | m | Bilateral lower legs, ears | 18 months | 10 years | amorphous, eosinophilic periodic acid-Schiff-positive material in the papillary dermis and subcutis | + | [15] |
| 56 | f | Feet and lower legs | 18 months | Not reported | Diffuse amorphous eosinophilic material surrounding adipocytes and involving vascular walls | + | [14] |
| 71 | f | Left lower leg | 12 months | 4 years | Scattered plasma cells and amorphous pink material in the dermis and subcutis | + | [13] |
| 58 | f | Bilateral lower legs | 18 months | 4 years | Amorphous pink material with perivascular accentuation and scattered plasma cells | thioflavin T + | [13] |
| 70 | f | Left lower leg | 4-5 years | 22 years | Amorphous pink material with admixed sparse chronic inflammation | + | [13] |
| 60 | f | Left lower leg | 5 years | 15 years | Dermal amorphous eosinophilic material and a background of chronic inflammation with lymphocytes and plasma cells and neovascularization. immunoglobulin light chain amyloid protein deposition | + | [12] |
| 70 | f | Upper back | Not specified | 12 months | Amorphous deposits in the papillary dermis | + | [11] |
| 62 | m | Forearms | Not specified | 12 months | Irregular hyperkeratosis in the epidermis and dermal sclerosis with thickened and homogeneous collagen bundles in the thickened dermis. | + | [11] |
| 59 | f | Left lower leg | 3 years | 10 years | See text_Case 1 | + | Present report |
| 53 | f | Left lower leg | 8 years | 15 years | See text_Case2 | + | Present report |
| 74 | f | Left lower leg | 14 months | 5 years | See text_Case3 | + | Present report |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Atzori, L.; Ferreli, C.; Matucci-Cerinic, C.; Pilloni, L.; Rongioletti, F. Primary Localized Cutaneous Nodular Amyloidosis and Limited Cutaneous Systemic Sclerosis: Additional Cases with Dermatoscopic and Histopathological Correlation of Amyloid Deposition. Dermatopathology 2021, 8, 229-235. https://doi.org/10.3390/dermatopathology8030028
Atzori L, Ferreli C, Matucci-Cerinic C, Pilloni L, Rongioletti F. Primary Localized Cutaneous Nodular Amyloidosis and Limited Cutaneous Systemic Sclerosis: Additional Cases with Dermatoscopic and Histopathological Correlation of Amyloid Deposition. Dermatopathology. 2021; 8(3):229-235. https://doi.org/10.3390/dermatopathology8030028
Chicago/Turabian StyleAtzori, Laura, Caterina Ferreli, Caterina Matucci-Cerinic, Luca Pilloni, and Franco Rongioletti. 2021. "Primary Localized Cutaneous Nodular Amyloidosis and Limited Cutaneous Systemic Sclerosis: Additional Cases with Dermatoscopic and Histopathological Correlation of Amyloid Deposition" Dermatopathology 8, no. 3: 229-235. https://doi.org/10.3390/dermatopathology8030028
APA StyleAtzori, L., Ferreli, C., Matucci-Cerinic, C., Pilloni, L., & Rongioletti, F. (2021). Primary Localized Cutaneous Nodular Amyloidosis and Limited Cutaneous Systemic Sclerosis: Additional Cases with Dermatoscopic and Histopathological Correlation of Amyloid Deposition. Dermatopathology, 8(3), 229-235. https://doi.org/10.3390/dermatopathology8030028








