The Burden of the Past: A Systematic Review of Childhood Trauma and Mental Health in Transgender and Gender Nonconforming Individuals
Abstract
1. Introduction
- (1)
- What is the prevalence and typology of adverse childhood experiences reported by TGNC individuals in recent empirical studies?
- (2)
- How are these experiences associated with mental health and physical health outcomes, and to what extent do resilience and protective factors (e.g., gender-affirming care, social support) moderate these associations?
- (3)
- Which conceptual and methodological gaps remain in the literature, and what directions are most promising for future research, including longitudinal and intersectional approaches?
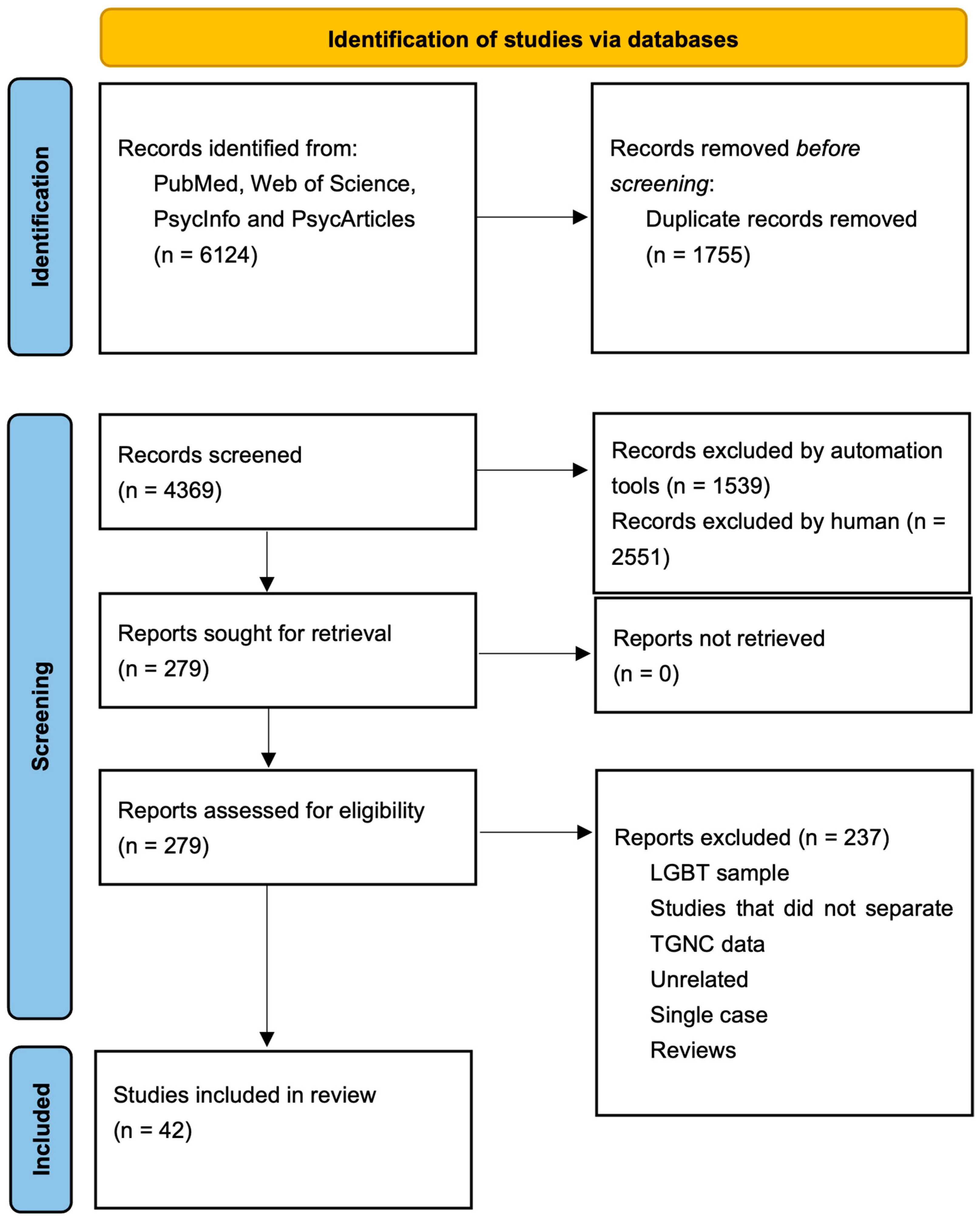
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria and Selection Process
2.3. Data Extraction and Synthesis
2.4. Quality Assessment
3. Results
3.1. Traditional ACEs
3.1.1. Prevalence of Traditional ACEs
3.1.2. Effects of Traditional ACEs on Mental and Physical Health
3.1.3. Protective and Mediating Factors
3.2. TGNC-Specific ACEs
3.2.1. Identity-Related Rejection in the Family and Among Peers
3.2.2. Systemic and Structural Discrimination
3.2.3. Trauma in the Context of Gender Nonconformity
3.2.4. Structural and Communal Trauma
3.2.5. Effects of TGNC-Specific ACEs on Mental Health
3.2.6. Intersectional Factors: Ethnicity, Socioeconomic Status, and Geography
4. Discussion
- -
- Types of ACEs experienced by TGNC individuals, such as childhood maltreatment, family rejection, and peer victimization.
- -
- Mental health consequences of ACEs, including increased risk for depression, anxiety, PTSD, suicidality, and substance use.
- -
- Protective factors and resilience mechanisms, such as social support, gender affirmation, and access to mental healthcare.
- -
- Implications for clinical interventions, including trauma-informed and gender-specific treatment strategies.
5. Clinical Implications
5.1. Trauma-Informed Care
5.2. Affirmative Practices
5.3. Intersectional Considerations
5.4. Early Screening and Intervention
5.5. Family Education Programs
5.6. Policy and Advocacy
5.7. Holistic Approaches to Care
5.8. Education and Training
5.9. Policy Implications
6. Limitations and Future Directions
Persistent Gaps in the Literature
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arayasirikul, S., Turner, C. M., Hernandez, C. J., Trujillo, D., Fisher, M. R., & Wilson, E. C. (2022). Transphobic adverse childhood experiences as a determinant of mental and sexual health for young trans women in the San Francisco bay area. Transgender Health, 7(6), 552–555. [Google Scholar] [CrossRef] [PubMed]
- Austin, A., Craig, S. L., D’Souza, S., & McInroy, L. B. (2022). Suicidality among transgender youth: Elucidating the role of interpersonal risk factors. Journal of Interpersonal Violence, 37(5–6), NP2696–NP2718. [Google Scholar] [CrossRef]
- Barboza-Salerno, G. E., & Meshelemiah, J. C. (2024). Associations between early child adversity and lifetime suicide attempts among gender diverse individuals: A moderated mediation. Child Abuse & Neglect, 149, 106705. [Google Scholar] [CrossRef]
- Belloir, J. A., Fabiano, F., Jackman, K. B., & Bockting, W. O. (2023). General self-efficacy as a mediator of the association between adverse childhood experiences and psychological distress in gender-minority individuals. Journal of Nursing Scholarship, 56(1), 9–17. [Google Scholar] [CrossRef] [PubMed]
- Bick, J., & Nelson, C. A. (2016). Early adverse experiences and the developing brain. Neuropsychopharmacology, 41(1), 177–196. [Google Scholar] [CrossRef] [PubMed]
- Biedermann, S. V., Asmuth, J., Schröder, J., Briken, P., Auer, M. K., & Fuss, J. (2021). Childhood adversities are common among trans people and associated with adult depression and suicidality. Journal of Psychiatric Research, 141, 318–324. [Google Scholar] [CrossRef]
- Brangwin, E., Zhao, Z., Shramko, M., Toomey, R. B., & Syvertsen, A. K. (2023). The association between family physical abuse and suicide attempts among gender minority adolescents: A comparison study. LGBT Health, 10(2), 99–108. [Google Scholar] [CrossRef]
- Cao, Q., Zhang, Q., Chen, Y., He, Z., Xiang, Z., Guan, H., Yan, N., Qiang, Y., & Li, M. (2023). The relationship between non-suicidal self-injury and childhood abuse in transgender people: A cross-sectional cohort study. Frontiers in Psychology, 14, 1062601. [Google Scholar] [CrossRef]
- Chakrapani, V., Scheim, A. I., Newman, P. A., Shunmugam, M., Rawat, S., Baruah, D., Bhatter, A., Nelson, R., Jaya, A., & Kaur, M. (2022). Affirming and negotiating gender in family and social spaces: Stigma, mental health and resilience among transmasculine people in India. Culture, Health and Sexuality, 24(7), 951–967. [Google Scholar] [CrossRef] [PubMed]
- Chan, R. C., Suen, Y. T., & Leung, J. S. Y. (2024). Gender identity differences in the experiences of family stressors and violence among transgender and non-binary individuals in China. Family Process, 63(2), 1046–1067. [Google Scholar]
- Coleman, E., Radix, A. E., Bouman, W. P., Brown, G. R., de Vries, A. L. C., Deutsch, M. B., Ettner, R., Fraser, L., Goodman, M., Green, J., & Hancock, A. B. (2022). Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health, 23(Suppl. S1), S1–S259. [Google Scholar] [CrossRef]
- Cussino, M., Crespi, C., Mineccia, V., Molo, M., Motta, G., & Veglia, F. (2021). State of mind of attachment and reflective function in an Italian transsexual sample. European Journal of Trauma & Dissociation, 5(4), 100108. [Google Scholar] [CrossRef]
- Danese, A., Moffitt, T. E., Harrington, H., Milne, B. J., Polanczyk, G., Pariante, C. M., Poulton, R., & Caspi, A. (2009). Adverse childhood experiences and adult risk factors for age-related disease: Depression, inflammation, and clustering of metabolic risk markers. Archives of Pediatrics & Adolescent Medicine, 163(12), 1135–1143. [Google Scholar]
- Domínguez-Martínez, T., Rebeca, R. G., Fresán, A., Cruz, J., Vega, H., & Reed, G. M. (2023). Risk factors for violence in transgender people: A retrospective study of experiences during adolescence. Psychology & Sexuality, 14(4), 659–675. [Google Scholar] [CrossRef]
- Eastwood, E. A., Nace, A. J., Hirshfield, S., & Birnbaum, J. M. (2021). Young transgender women of color: Homelessness, poverty, childhood sexual abuse and implications for HIV care. AIDS and Behavior, 25(Suppl. S1), 96–106. [Google Scholar] [CrossRef] [PubMed]
- Feil, K., Riedl, D., Böttcher, B., Fuchs, M., Kapelari, K., Gräßer, S., Toth, B., & Lampe, A. (2023). Higher prevalence of adverse childhood experiences in transgender than in cisgender individuals: Results from a single-center observational study. Journal of Clinical Medicine, 12(13), 4501. [Google Scholar] [CrossRef]
- Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., Koss, M. P., & Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse childhood experiences (ACE) study. American Journal of Preventive Medicine, 14(4), 245–258. [Google Scholar] [CrossRef]
- Ford-Gilboe, M., Wathen, C. N., Varcoe, C., MacMillan, H. L., Scott-Storey, K., Mantler, T., Hegarty, K., & Perrin, N. (2016). Development of a brief measure of intimate partner violence experiences: The Composite Abuse Scale (Revised)—Short Form (CASR-SF). BMJ Open, 6(12), e012824. [Google Scholar] [CrossRef]
- Gamio Cuervo, Á., Herrawi, F., Horne, S. G., & Wilkins-Yel, K. G. (2022). “I’m just so glad that i saved my life”: A grounded theory analysis of transgender and non-binary Latinx people navigating family rejection and intergenerational violence. LGBTQ+ Family: An Interdisciplinary Journal, 18(5), 403–428. [Google Scholar] [CrossRef]
- Garthe, R. C., Blackburn, A. M., Kaur, A., Sarol, J. N., Goffnett, J., Rieger, A., Reinhart, C., & Smith, D. C. (2022). Suicidal ideation among transgender and gender expansive youth: Mechanisms of risk. Transgender Health, 7(5), 416–422. [Google Scholar] [CrossRef] [PubMed]
- Garthe, R. C., Rieger, A., Goffnett, J., Kaur, A., N. Sarol, J., Blackburn, A. M., Kim, S., Hereth, J., & Kennedy, A. C. (2023). Grade-level differences of peer and dating victimization among transgender, gender expansive, female, and male adolescents. Journal of LGBT Youth, 20(3), 603–631. [Google Scholar] [CrossRef]
- Joanna Briggs Institute. (2017). Checklist for analytical cross sectional studies. The Joanna Briggs Institute. [Google Scholar]
- Kaltiala, R., & Ellonen, N. (2022). Transgender identity and experiences of sexual harassment in adolescence. Child Abuse Review, 31(4), 1–14. [Google Scholar] [CrossRef]
- Karatekin, C., & Hill, M. (2019). Expanding the original definition of adverse childhood experiences (ACEs). Journal of Child & Adolescent Trauma, 12(3), 289–306. [Google Scholar]
- Keating, L., & Muller, R. T. (2020). LGBTQ+ based discrimination is associated with PTSD symptoms, dissociation, emotion dysregulation, and attachment insecurity among LGBTQ+ adults who have experienced trauma. Journal of Trauma & Dissociation, 21(1), 124–141. [Google Scholar]
- Klemmer, C. L., Rusow, J., Goldbach, J., Kattari, S. K., & Rice, E. (2021). Socially assigned gender nonconformity and school violence experience among transgender and cisgender adolescents. Journal of Interpersonal Violence, 36(15–16), NP8567–NP8589. [Google Scholar] [CrossRef]
- Kozlowska, K., Chudleigh, C., McClure, G., Maguire, A. M., & Ambler, G. R. (2021). Attachment patterns in children and adolescents with gender dysphoria. Frontiers in Psychology, 11, 582688. [Google Scholar] [CrossRef]
- Lacombe-Duncan, A., & Olawale, R. (2022). Context, types, and consequences of violence across the life course: A qualitative study of the lived experiences of transgender women living with HIV. Journal of Interpersonal Violence, 37(5–6), 2242–2266. [Google Scholar] [CrossRef]
- Lian, Q. G., Li, R. L., Liu, Z. H., Li, X. N., Su, Q. R., & Zheng, D. P. (2022). Associations of nonconforming gender expression and gender identity with bullying victimization: An analysis of the 2017 youth risk behavior survey. BMC Public Health, 22(1), 650. [Google Scholar] [CrossRef]
- Lockwood, C., Munn, Z., & Porritt, K. (2015). Qualitative research synthesis: Methodological guidance for systematic reviewers utilizing meta-aggregation. International Journal of Evidence-Based Healthcare, 13(3), 179–187. [Google Scholar] [CrossRef] [PubMed]
- Lowry, R., Johns, M. M., & Robin, L. E. (2020). Violence victimization, substance use disparities, and gender-nonconforming youth. American Journal of Preventive Medicine, 58(5), e159–e169. [Google Scholar] [CrossRef]
- Marquez-Velarde, G., Miller, G. H., Shircliff, J. E., & Suárez, M. I. (2023). The impact of family support and rejection on suicide ideation and attempt among transgender adults in the U.S. LGBTQ+ Family: An Interdisciplinary Journal, 19(4), 275–287. [Google Scholar] [CrossRef]
- Marx, R. A., Hatchel, T., Mehring, C. B., & Espelage, D. L. (2021). Predictors of sexual victimisation and suicidal ideation among transgender and gender-nonconforming adolescents. Psychology and Sexuality, 12(1–2), 79–95. [Google Scholar] [CrossRef]
- McBride, R. S., & Neary, A. (2021). Trans and gender diverse youth resisting cisnormativity in school. Gender and Education, 33(8), 1090–1107. [Google Scholar] [CrossRef]
- Meyer, I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, bisexual, and transgender populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. [Google Scholar] [CrossRef]
- Newcomb, M. E., Hill, R., Buehler, K., Ryan, D. T., Whitton, S. W., & Mustanski, B. (2020). High burden of mental health problems, substance use, violence, and related psychosocial factors in transgender, non-binary, and gender diverse youth and young adults. Archives of Sexual Behavior, 49(2), 645–659. [Google Scholar] [CrossRef] [PubMed]
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. The BMJ, 372, n71. [Google Scholar] [CrossRef]
- Price, M. A., Hollinsaid, N. L., Bokhour, E. J., Johnston, C., Skov, H. E., Kaufman, G. W., Sheridan, M. K., & Olezeski, C. (2023). Transgender and gender diverse youth’s experiences of gender-related adversity. Child and Adolescent Social Work Journal, 40(3), 361–380. [Google Scholar] [CrossRef]
- Price, M. N., & Green, A. E. (2023). Association of gender identity acceptance with fewer suicide attempts among transgender and nonbinary youth. Transgender Health, 8(1), 56–63. [Google Scholar] [CrossRef]
- Ramos, N., & Marr, M. C. (2023). Traumatic stress and resilience among transgender and gender diverse youth. Child and Adolescent Psychiatric Clinics of North America, 32(4), 667–682. [Google Scholar] [CrossRef]
- Ricks, J. N. M., & Horan, J. (2023). Associations between childhood sexual abuse, intimate partner violence trauma exposure, mental health, and social gender affirmation among black transgender women. Health Equity, 7(1), 743–752. [Google Scholar] [CrossRef]
- Sizemore, K. M., Talan, A., Forbes, N., Gray, S., Park, H. H., & Rendina, H. J. (2022). Attachment buffers against the association between childhood sexual abuse, depression, and substance use problems among transgender women: A moderated-mediation model. Psychology & Sexuality, 13(5), 1319–1335. [Google Scholar] [CrossRef]
- Spielmann, J., Feng, S., & Briley, D. A. (2022). Mental health contributors among transgender people in a non-WEIRD society: Evidence from China. Social Psychological and Personality Science, 13, 747–757. [Google Scholar] [CrossRef]
- Strauss, P., Cook, A., Winter, S., Watson, V., Wright Toussaint, D., & Lin, A. (2019). Associations between negative life experiences and the mental health of trans and gender diverse young people in Australia: Findings from trans pathways. Psychological Medicine, 50(5), 808–817. [Google Scholar] [CrossRef] [PubMed]
- Strauss, P., Cook, A., Winter, S., Watson, V., Wright Toussaint, D., & Lin, A. (2020). Mental health issues and complex experiences of abuse among trans and gender diverse young people: Findings from trans pathways. LGBT Health, 7(3), 128–136. [Google Scholar] [CrossRef] [PubMed]
- Strenth, C. R., Smith, M., Gonzalez, L., Grant, A., Thakur, B., & Kamugisha, E. I. L. (2024). Mediational pathways exploring the link between adverse childhood experiences and physical health in a transgender population. Child Abuse & Neglect, 149, 106678. [Google Scholar] [CrossRef]
- Suarez, N. A., Peitzmeier, S. M., Potter, J., Samandur, A., & Reisner, S. L. (2021). Preliminary findings for adverse childhood experiences and associations with negative physical and mental health and victimization in transmasculine adults. Child Abuse & Neglect, 118, 105161. [Google Scholar] [CrossRef]
- Testa, R. J., Habarth, J., Peta, J., Balsam, K., & Bockting, W. (2015). Development of the gender minority stress and resilience measure. Psychology of Sexual Orientation and Gender Diversity, 2(1), 65–77. [Google Scholar] [CrossRef]
- Thoma, B. C., Rezeppa, T. L., Choukas-Bradley, S., Salk, R. H., & Marshal, M. P. (2021). Disparities in childhood abuse between transgender and cisgender adolescents. Pediatrics, 148(2), e2020016907. [Google Scholar] [CrossRef]
- Thomeer, M. B., LeBlanc, A. J., Paine, E. A., Frost, D. M., Singh, A., & Bockting, W. O. (2022). Past experiences and anticipated futures in the lives of transgender and nonbinary people. Advances in Life Course Research, 53, 100482. [Google Scholar] [CrossRef]
- Tobin, V., & Delaney, K. R. (2019). Child abuse victimization among transgender and gender nonconforming people: A systematic review. Perspectives in Psychiatric Care, 55(4), 576–583. [Google Scholar] [CrossRef]
- Tran, N. M., Mann, S., Cortez, M. G., Harrell, B., & Nettuno, L. (2023). Adverse childhood experiences (ACEs) and mental health by gender identity in the United States, 2019–2021. Preventive Medicine, 175, 107705. [Google Scholar] [CrossRef] [PubMed]
- Tubman, J. G., Lee, J., & Moore, C. (2024). Factors associated with sexual victimization among transgender emerging adults. Journal of Interpersonal Violence, 39(11–12), 2832–2852. [Google Scholar] [CrossRef]
- van Beusekom, G., Collier, K. L., Bos, H. M. W., Sandfort, T. G. M., & Overbeek, G. (2020). Gender nonconformity and peer victimization: Sex and sexual attraction differences by age. Journal of Sex Research, 57(2), 234–246. [Google Scholar] [CrossRef] [PubMed]
- Wichaidit, W., Assanangkornchai, S., & Chongsuvivatwong, V. (2021). Disparities in behavioral health and experience of violence between cisgender and transgender Thai adolescents. PLoS ONE, 16, e0252520. [Google Scholar] [CrossRef] [PubMed]
- Xu, L., Chang, R., Chen, Y., Xia, D., Xu, C., Yu, X., Chen, H., Wang, R., Liu, Y., Liu, S., Ge, X., Ma, T., Zhou, Y., Wang, Y., Ma, S., & Cai, Y. (2023). The prevalence of childhood sexual experiences and intimate partner violence among transgender women in China: Risk factors for lifetime suicidal ideation. Frontiers in Public Health, 10, 1037622. [Google Scholar] [CrossRef] [PubMed]
- Ybarra, M. L., Goodman, K. L., Saewyc, E., Scheer, J. R., & Stroem, I. F. (2022). Youth characteristics associated with sexual violence perpetration among transgender boys and girls, cisgender boys and girls, and nonbinary youth. JAMA Network Open, 5(6), e2215863. [Google Scholar] [CrossRef]
| “gender dysphoria” or “gender identity disorder” or “transsexualism” or “transgender” or “gender identity” or “transsexual” or “transsexualism” or “gender variant” or “transgender” or “transgenderism” or “gender variant” or “gender variance” or “atypical gender identity” or “cross sex” or “cross-gender” or “gender incongruence” or “gender reassignment” or “gender reaffirmation surgery” or “gender transition” or “gender atypicality” or “non-conformed gender” or “reassignment surgery” or “sexual reassignment” |
| AND |
| “dissociative” or “dissociation” or “trauma” or “abuse” or “neglect” or “maltreatment” or “posttraumatic” or “ptsd” or “disorganized attachment” or “violence” |
| Author, Year, Country | Sample Characteristics | Type of ACEs or Trauma | Study Design and Methodological Approach | Health Impacts and Clinical Implications | |
|---|---|---|---|---|---|
| Sample Size and Participants’ Age | Sex Assigned at Birth | ||||
| Arayasirikul et al. (2022) United States | N = 300 Age = 16–24 years | AMAB | Transphobia Verbal abuse Physical abuse Sexual abuse | Quantitative Cross-sectional | Exposure to high levels of ACEs is detrimental to mental and sexual health and is associated with unsafe sexual practices. |
| Austin et al. (2022) United States–Canada | N = 372 Age = 14–18 years M. Age = 15.99 (1.232) years | AMAB AFAB | Transphobia Rejection Verbal abuse Physical abuse Emotional neglect Internalized self-stigma Microaggressions | Quantitative Cross-sectional | Interpersonal identity-based microaggressions are significantly associated with suicide attempts, but not ideation. Emotional neglect by family, school belonging, and internalized self-stigma are significantly related to past 6-month suicidality. Feeling disconnected from school is associated with higher past 6-month suicidality. Internalized self-stigma is related to suicidal ideation. Early interventions with caregivers are essential to fostering supportive attitudes toward gender diversity. It is important to provide caregivers with updated information on the importance of adopting an affirming approach; what affirmative parenting looks and sounds like; and the harmful effects of rejecting, invalidating, or minimizing a child’s transgender identity. |
| Barboza-Salerno and Meshelemiah (2024) United States | N = 1368 (N = 274 transgender and N = 1162 cisgender) Age = 18–72 years M. Age = 54.83 (15.2) years | AMAB AFAB TGNB | Household mental illness Household intimate partner violence Emotional abuse Physical abuse Sexual abuse Parental divorce or separation Household substance use Living with an incarcerated household member | Quantitative Cross-sectional | Gender minorities have higher LSA risk and more ACEs, with depressive symptoms mediating this link. Transgender groups face up to eight times higher LSA risk, showing non-linear risk patterns. Depressive symptoms have a stronger mediating effect for transgender people; alcohol use and social support were not mediators. |
| Belloir et al. (2023) United States | N = 166 (99 AFAB + 67 AMAB) Age = 21–74 years M. Age = 38.6 (12.2) years | AMAB AFAB | ACE | Quantitative Multi-site longitudinal study | ACEs are an important predictor of psychological distress. General self-efficacy partially mediates the positive association between ACEs and psychological distress. Increasing general self-efficacy in gender minorities may have therapeutic benefits for mental health. Early screening of gender minority youth can help identify potential abuse or neglect, enabling timely interventions like psychological first aid or cognitive behavioral therapy to prevent further adverse experiences. |
| Biedermann et al. (2021) Germany | N = 187 (94 AMAB + 93 AFAB) M. Age AMAB = 40.9 (13.0) years M. Age AFAB =30.9 (10.9) years | AMAB AFAB | Emotional abuse Physical abuse Sexual abuse Emotional neglect Physical neglect Parents showing violent behavior Bullying Forced to behave according to sex | Quantitative Cross-sectional | Association of ACEs with adult depression and suicidality. Time since the beginning of hormone therapy does not influence adult depressive symptoms or suicidality. In light of the high prevalence and the associated psychological burden, ACEs should be assessed regularly in trans people, especially when clinical symptoms suggest it. |
| Brangwin et al. (2023) United States | N = 121,150 (60,973 female + 57,873 male + 203 T AMAB + 175 T AFAB + 344 T do not identify + 1052 gender not sure) Age = 11–19 years M. Age = 14.74 (1.78) years | AMAB AFAB | Family physical abuse | Quantitative Cross-sectional | GM adolescents experience higher levels of family physical abuse and remain at greater overall risk for suicide attempts compared to cisgender adolescents. No significant differences are found within gender minority groups, indicating that all GMY face similarly high levels of family physical abuse. Adolescents with multiple minority identities (e.g., GM, sexual minority, female) report higher levels of family physical abuse than those with fewer or no minority identities. Family physical abuse is linked to increased odds of suicidal behavior across all gender identity groups. The strength of the association between family physical abuse and suicide attempts is similar for both cisgender and gender minority adolescents. |
| Cao et al. (2023) China | N = 971 (296 AFAB + 675 AMAB) M. Age = 24.5 (6.4) years | AMAB AFAB | Emotional abuse Physical abuse Sexual abuse Emotional neglect Physical neglect | Quantitative Cross-sectional cohort study | NSSI behaviors in transgender individuals are linked to childhood abuse and emotional dysregulation traits. Emotional dysregulation partially mediates the connection between childhood abuse and NSSI behaviors. Screening for emotional dysregulation traits and providing timely interventions are crucial. Efforts should focus on improving the environment for transgender people to reduce childhood abuse. Reducing childhood abuse may decrease NSSI behaviors and extreme events in the transgender population. |
| Chakrapani et al. (2022) India | N = 27 M. Age = 25 (3.0) years | AFAB | Stigma Discrimination Violence in diverse settings/structural violence (family, schools, workplace) Bullying | Qualitative | Findings reveal the impacts of structural violence. Fear of discrimination and anticipated stigma can lead individuals to conceal their gender identity or expression, resulting in negative mental health outcomes. Family (non)acceptance is linked to mental health. Heavy alcohol use or smoking are coping strategies that negatively impact health and may be associated with masculinity or stress coping. Participants with family or friend support do not engage in such behaviors. |
| Chan et al. (2024) China | N = 1063 Age = 18–30+ years | AMAB AFAB | Gender identity and expression change efforts Physical abuse Emotional abuse Sexual abuse Financial abuse | Quantitative | 76% of TNB individuals reported having encountered at least one form of violence perpetrated by their family members. Transfeminine individuals reported experiencing emotional and physical abuse; transmasculine individuals were more likely to be subjected to gender identity and/or expression change efforts. |
| Cussino et al. (2021) Italy | N = 52 (25 AFAB + 27 AMAB) Age = 17–52 years M. Age = 31.33 (10.46) years | AMAB AFAB | Prostitution Violence by the father/mother Father/mother alcoholics Death of mother/father/brother/sister Rejection by mother/father Neglect by mother/father | Quantitative Cross-sectional | A total of 92.3% of participants have an insecure attachment state of mind. Among those with GD, 71.2% exhibit a dismissing attachment state, while 21.2% have an entangled state. Half of the sample reports one or more traumatic life events. AAI data reveal frequent unresolved trauma among those with insecure attachment. No traumatic experiences related to attachment are reported by securely attached participants. Findings suggest that interventions for transgender patients should focus on promoting a secure state of mind regarding attachment and traumatic experiences. |
| Domínguez-Martínez et al. (2023) Mexico | N = 245 (198 AMAB + 47 AFAB) Age = 18–65 years M. Age = 30.9 (10.2) years | AMAB AFAB | Physical violence Psychological violence Sexual violence Family rejection Peer rejection | Qualitative Descriptive study Retrospective research interviews | Transgender people face a high risk of various forms of violence during adolescence, with psychological violence being the most common, followed by physical and sexual violence. Transgender people are at high risk of social rejection from an early age across various contexts. Rejection, seeking recognition of gender identity, and requesting to be called by their chosen name are the strongest predictors of all types of violence. |
| Eastwood et al. (2021) United States | N = 102 Age = 18–24 years M. Age = 22.30 (1.62) years | AMAB | Childhood sexual abuse Forced or coerced sexual contact Housing instability and homelessness Poverty and food insecurity Social marginalization and discrimination Engagement in high-risk survival behaviors (e.g., sex work, drug use) Lack of social support from family and transgender peers | Quantitative Cross-sectional | A total of 75.5% of young transgender women of color experienced homelessness, with 92.9% living in poverty and 50% relying on sex work. Mental health distress was widespread, with 51.3% screening positive for depression, while only 26.5% achieved HIV viral suppression and 12.7% maintained consistent HIV care. Childhood sexual abuse was strongly linked to homelessness, high-risk behaviors, and poor health outcomes. Trauma exposure, economic instability, and lack of support create a syndemic effect, exacerbating health disparities and underscoring the need for integrated housing, mental health, and HIV care interventions. |
| Feil et al. (2023) Austria | N = 70 (35 GNC + 35 cisgender) GNC = 35 (18 AFAB + 12 AMAB + 5 nonbinary) M. Age = 29.5 (2.2) years | AMAB AFAB | Emotional abuse Physical abuse Neglect Witnessing violence Peer abuse/bullying Sexual violence | Quantitative Cross-sectional | TGD people are significantly more likely to experience ACEs than cisgender people (parental and peer abuse are especially common). Sexual abuse is not more prevalent. TGD individuals report an earlier onset of ACEs at 5 years of age and a higher prevalence of depression, PTSD symptoms, and anxiety. There is an urgent need to prevent childhood trauma and foster resilience. Healthcare providers should assess ACEs in TGD people and ensure a safe, affirming care environment. |
| Gamio Cuervo et al. (2022) Unites States | N = 12 Age = 23–32 years | AMAB AFAB | Family rejection Intergenerational violence | Qualitative | Family rejection in Latinx families is connected to the cycle of family violence and intergenerational trauma and is a manifestation of cumulative trauma that influences decisions. Understanding cultural values in individual and family environments is crucial to understanding rejection. These factors may increase the need for Latinx trans children to negotiate or distance themselves relationally. |
| Garthe et al. (2022) United States | N = 4464 (1116 male + 1116 female + 1116 T + 1116 GE) (Students in grades 8 to 12) | AMAB AFAB | Peer victimization Dating violence | Quantitative Cross-sectional | Transgender and gender-expansive youth face an alarming risk of suicidal ideation, highlighting the urgent need for suicide prevention efforts. Suicidal ideation is mediated by peer victimization, dating violence, substance use problems, and depressive symptoms. Programs that promote mental health and prevent bullying, dating violence, substance use, and related problems are essential. |
| Garthe et al. (2023) United States | N = 4464 (1116 male + 1116 female + 1116 T + 1116 GE) (Students in grades 8 to 12) | AMAB AFAB | Peer victimization (physical, verbal, or cyber forms of bullying) Dating violence (physical or psychological abuse from dating partners) | Quantitative Cross-sectional | Peer victimization decreases as youth progress through high school among GNC youth. Transgender and gender-expansive youth experience more physical, verbal, and cyber victimization than their peers. Eighth- to tenth-grade gender-expansive youth report higher rates than twelfth graders. Eighth graders experience the highest levels of physical peer victimization; verbal victimization remained high across all grades. Cyber-victimization is higher among female, transgender, and gender-expansive youth in eighth grade. Transgender and gender-expansive youth report higher levels of physical and psychological dating violence. |
| Kaltiala and Ellonen (2022) Finland | N = 123,663 (790 opposite sex + 4351 nonbinary + 118,522 cisgender) Age = 14–20 years | AMAB AFAB | Sexual harassment (gender harassment, unwelcome sexual attention, and sexual coercion) | Quantitative Cross-sectional | GMY report higher rates of sexual harassment compared to cisgender youth. Both gender identity issues and sexual harassment are linked to mental health problems (e.g., emotional and behavioral disorders) Excessive experiences of sexual harassment among transgender adolescents are partially explained by confounding family-related and mental health factors and not exclusively by gender identity per se. Teaching coping skills and reducing internalized heterosexism can help alleviate minority stress. Interventions should prioritize identifying and treating mental health issues in gender minority youth. Addressing emotional and behavioral disorders can help reduce vulnerability to sexual harassment and improve overall well-being. |
| Klemmer et al. (2021) United States | N = 1496 (26 T + 717 cisgender boys + 753 cisgender girls) Age = 14–18 years M. Age = 16.0 years | AMAB AFAB | Bullying | Quantitative Cross-sectional | Socially assigned gender nonconforming adolescents face increased rates of bullying, school-related violence, and safety concerns compared to their gender-conforming peers. They are also more likely to miss school due to these safety concerns and experiences of bullying. |
| Kozlowska et al. (2021) Australia | N = 57 (24 AMAB + 33 AFAB) Age = 8.42–15.92 years M. Age = 12.96 (1.91) years | AMAB AFAB | Family conflict Loss via separation from a loved one or a close friend Bullying Maternal mental illness (most commonly depression) Paternal mental illness Financial stress Moving house that was stressful Domestic violence Maternal physical illness Physical abuse Sexual abuse Placement changes (foster care or between parents) Neglect Custody battle Intelligence | Quantitative Cross-sectional | Children with gender dysphoria are often in a context where multiple risk factors interact, including insecure attachment, unresolved loss or trauma, family conflict and disintegration, and exposure to various ACEs. GD in children is linked to developmental pathways involving insecure attachment, unresolved loss, and trauma. These pathways are shaped by family instability, ACEs such as maltreatment, and SES. A broad perspective is essential for understanding GD, considering its impact on distress, adaptation difficulties, multimorbidity, and overall well-being. Effective treatment requires a comprehensive biopsychosocial assessment of both the child and family. Therapeutic interventions should address the interconnected factors influencing the child’s experience. Efforts should focus on enhancing the child’s sense of acceptance and safety within family and peer relationships. |
| Lacombe-Duncan and Olawale (2022) Canada | N = 11 Age = 20–60 years | AMAB | Familial exclusion Bullying ACE | Qualitative | TW experience ACEs such as parental substance use, mental health issues, and lack of security. Some ACEs, which are directly linked to transgender and gender nonconformity stigma, such as abuse, neglect, homelessness, familial rejection, and bullying, contribute to internalized trans stigma. |
| Lian et al. (2022) United States | N = 728 (334 T + 394 not sure) T = 137 AFAB + 197 AMAB not sure = 196 AFAB + 198 AMAB Students in grades 9 to 12 | AMAB AFAB | Bullying | Quantitative Cross-sectional | TGNC students are more vulnerable to bullying victimization (higher rates of traditional and electronic bullying) than cisgender peers. AMAB GNC adolescents are linked with higher bullying victimization, while AFAB GNC are not. |
| Lowry et al. (2020) United States | N = 6082 | AMAB AFAB | Bullying | Quantitative Cross-sectional | GNC males are at a greater risk for victimization than GNC females. Substance use among GNC male students may be a response to the higher prevalence of violence victimization they experience. No association between GNC female students and substance use. |
| M. A. Price et al. (2023) United States | N = 49 (44 T + 5 nonbinary/ 11 AMAB + 38 AFAB) Age = 11–20 years M. Age = 15.53 (1.73) years | AMAB AFAB | Bullying ACE Gender-related adversity | Qualitative | The results emphasize the significance of gender-related challenges faced by TGD youth, including verbal abuse, threats or acts of physical and sexual assault, discrimination, lack of affirmation, and rejection. A comprehensive assessment of both gender-related and non-gender-related adversity is essential to understanding the unique mental health challenges faced by TGD youth, given the highly distressing impact of gender-related adversities. |
| M. N. Price and Green (2023) United States | N = 8221 (3610 T + 4611 nonbinary) Age = 13–24 years | AMAB AFAB | Rejection | Quantitative Cross-sectional | TGNB youth with at least one accepting adult have 33% lower odds of attempting suicide in the past year; peer acceptance also plays a comparable key role in reducing suicide attempts. Acceptance has a greater impact on those AMAB compared to those AFAB. |
| Marquez-Velarde et al. (2023) United States | N = 27,715 TNB Age = 18–65+ years | AMAB AFAB | Family rejection Physical violence by family members Expulsion from home due to gender identity Emotional rejection (loss of family relationships) Restriction of gender expression | Quantitative Cross-sectional | Cumulative ACEs significantly increase suicidality, with predicted probabilities of suicide ideation rising from 72% (no rejection) to 97% (all five rejection experiences), and suicide attempts rising from 35% to 75% when all forms of family rejection are experienced. These findings underscore the need for family-focused interventions and structural policy changes to mitigate the impact of early-life rejection on transgender mental health. |
| Marx et al. (2021) United States | N = 610 Age = 13–18 years | AMAB AFAB | Childhood sexual abuse Sexual harassment/victimization Gender-based violence | Quantitative Cross-sectional | Sexual victimization, prejudiced peer victimization, problematic substance use, and AFAB are significant predictors of sexual victimization among TGNC adolescents. Sexual victimization, prejudiced peer victimization, sexual harassment victimization, and problematic substance use are associated with increased suicidal ideation. Greater parental support and a sense of school belonging are associated with lower levels of suicidal ideation. |
| McBride and Neary (2021) Ireland | N = 13 Age = 15–24 years | AMAB AFAB | Structural vulnerability | Qualitative | Trans youth experience harm due to institutionalized cisnormativity that fosters insecurity and confusion about gender identity. Trans youth resist exclusion through activism, education, and policy advocacy, but these actions also expose them to further risks. Coming out, educating peers, and challenging school norms are survival strategies that also confront cisnormative power structures. |
| Newcomb et al. (2020) United States | N = 214 (128 AFAB + 86 AMAB) M. Age AFAB = 19.04 (3.18) years M. Age AMAB = 21.91 (3.25) years | AMAB AFAB | Childhood sexual abuse | Quantitative Cross-sectional | Over one-third of TW and nonbinary AMAB youth reported experiencing CSA; nearly one-third of TW experienced penetrative CSA. Nonbinary AMAB youth had the highest rates of lifetime trauma (82.1%), followed by nonbinary AFAB youth (78%), TW (72.4%), and TM (59.1%). CSA and other violent experiences contribute to depression, suicidality, substance use, and sexual risk behaviors. Individual and structural interventions are essential to prevent and mitigate these experiences for TGD youth. |
| Ricks and Horan (2023) United States | N = 138 Age = 18–65 M. Age = 30.8 (10.0) years | AMAB | Childhood sexual abuse | Quantitative Cross-sectional | CSA is a common lifetime experience (40.6% of participants) but does not diminish the significant association between social GA and mental health outcomes. |
| Sizemore et al. (2022) United States | N = 213 M. Age = 34.27 (11.67) | AFAB | Childhood sexual abuse | Quantitative Cross-sectional | In TW, depression acts as a mediator between CSA and substance use problems, including alcohol use disorder. Secure attachment reduces the impact of CSA on both depression symptoms and substance use issues. |
| Strauss et al. (2020) Australia | N = 859 (639 AFAB + 220 AMAB) Age = 14–25 M. Age = 19.37 (3.15) years | AMAB AFAB | Familial physical abuse Extrafamilial physical abuse Familial sexual abuse Extrafamilial sexual abuse Other familial abuse Abuse within an intimate relationship | Quantitative Cross-sectional | A total of 24.8% of participants report familial physical abuse, and 7.5% experience familial sexual abuse. All forms of abuse are linked to poor mental health, with varying risk levels. Familial physical abuse is associated with a fourfold increase in lifetime suicide attempts. The six forms of abuse studied are linked to self-harm, suicide, and psychiatric diagnoses. Most participants do not attribute their abuse to their TGD status. High prevalence of abuse among TGD youth requires clinician awareness; enhanced education and sensitivity among healthcare providers are essential. |
| Strauss et al. (2019) Australia | N = 859 (T + GNC) Age = 14–25 years | AMAB AFAB | Peer rejection Bullying precarious housing | Quantitative Cross-sectional | Of the participants, 89.0% experience peer rejection, 22.0% face unstable housing situations, 74.0% experience bullying, and 68.9% face discrimination. Poor mental health outcomes are most strongly linked to negative experiences, particularly unstable housing and educational challenges. Participants with a history of suicide attempts are nearly six times more likely to have faced housing issues, including homelessness. These results emphasize the urgent need for improved mental healthcare and targeted interventions. |
| Strenth et al. (2024) United States | N = 274 | AMAB AFAB | Psychological abuse Physical abuse Sexual abuse Neglect Witness domestic violence (psychological) Witness domestic violence (physical) Mental illness Household death Household divorce Household criminal behavior Household drug use | Quantitative Cross-sectional | ACEs led to increased mental distress, which was linked to worse general health and more days physically ill. ACEs increased discrimination, which led to more mental distress and thus worse general health and more days physically ill. ACEs led to more discrimination and gender non-affirmation, increasing mental distress and leading to worse general health and more days physically ill. |
| Suarez et al. (2021) United States | N = 131 Age = 21–64 years | AFAB | Psychological abuse Physical abuse Sexual abuse Neglect Witness domestic violence (psychological) Witness domestic violence (physical) Mental illness Household death Household divorce Household criminal behavior Household drug use | Quantitative Cross-sectional | A total of 92% of TM adults experience ACEs. ACEs are strongly linked to mental health issues (those with 4+ ACEs have over five times the odds of depression and suicidality), victimization, worse health outcomes (increased obesity, raising risks for diabetes, heart attack, and stroke), and risky behaviors in adulthood. |
| Thoma et al. (2021) United States | N = 1836 (1055 T + 773 cisgender) Age = 14–18 M. Age = 15.9 (1.2) | AMAB AFAB | Physical abuse Emotional abuse Sexual abuse | Quantitative Cross-sectional | Transgender adolescents report more psychological, physical, and sexual abuse in childhood than heterosexual cisgender adolescents. AFAB transgender adolescents are more likely to report psychological abuse from parents or other adults. Transgender males have higher odds of psychological abuse compared to female cisgender adolescents, while nonbinary AFAB adolescents do not show the same elevated risk when accounting for other abuse types. Higher childhood abuse rates may contribute to disproportionate mental health challenges among transgender adolescents. Providers should focus on parent–adolescent relationships when treating AFAB transgender adolescents. |
| Thomeer et al. (2022) Unites States | N = 87 TGNB M. Age = 37.55 (18.64) years | AMAB AFAB | Rejection Sexual abuse | Qualitative | Rejection and experiences of violence are common during childhood. These findings offer valuable insights into the lived experiences of transgender and nonbinary individuals, emphasizing the need for supportive interventions across different life stages. |
| Tran et al. (2023) United States | N = 141,615 (556 GM + 141,059 cisgender) Age = 18– | AMAB AFAB | Physical abuse Emotional abuse Sexual abuse Household mental illness Household substance misuse Household domestic violence Incarcerated household member Parental separation or divorce | Quantitative Cross-sectional | GM adults report more emotional and physical abuse, as well as a higher overall prevalence of ACEs. Greater ACE exposure is linked to higher rates of frequent mental distress and lifetime depression diagnoses. ACEs disproportionately affect GM populations, emphasizing the need for prevention strategies. Routine pediatric ACE screening could help mitigate long-term mental health impacts, especially for GM youth. Mental health and primary care providers should receive education on transgender health to ensure inclusive and effective care. |
| Tubman et al. (2024) United States | N = 248 (172 AFAB + 76 AMAB) M. Age = 22.61 (3.06) years | AMAB AFAB | Sexual abuse | Quantitative Cross-sectional | Participants with a history of CSA experience more substance use, minority stress, and relational issues, show higher alcohol-related problems and negative consequences from substance use, and report greater daily discrimination. These findings highlight the importance of addressing the impacts of CSA in therapeutic interventions for transgender emerging adults. |
| van Beusekom et al. (2020) Netherlands | N = 2185 (1069 boys + 1116 girls) Age = 11–18 years M. Age = 15.13 (1.89) | AMAB AFAB | Bullying | Quantitative Cross-sectional | Adolescents with high gender nonconformity experience more peer victimization and homophobic name-calling than those with low gender nonconformity. Gender nonconformity elicits stronger peer victimization in boys than in girls and stronger victimization (both general and homophobic) among youth with high same-sex attraction. Findings highlight the need to promote acceptance of gender diversity and strengthen social support for gender-nonconforming youth. Age-appropriate education on gender and sexual diversity should be introduced before early adolescence to reduce victimization risks. |
| Wichaidit et al. (2021) Thailand | N = 421 AFAB + 334 AMAB Students in the general education system: Year 7 (Matthayom 1) Year 9 (Matthayom 3) Year 11(Matthayom 5) and the vocational education system: Vocational Certificate Year 2. | AMAB AFAB | Being threatened Severe physical violence Intimate partner violence Sexual violence | Quantitative Cross-sectional | One-third of transgender girls report experiencing sexual violence in the past year. Both transgender boys and girls are significantly more likely than cisgender girls to experience all types of violence. Transgender boys have the highest levels of depressive symptoms, suicidality, and alcohol consumption. Transgender girls have the highest prevalence of experiencing sexual violence in the past year. Suicidality is higher among transgender youth compared to cisgender youth, with transgender boys reporting the highest rates. Transgender boys have a higher prevalence of alcohol consumption than cisgender boys, while transgender girls have lower rates. |
| Xu et al. (2023) China | N = 247 Age = 18–61 years | AMAB | Childhood sexual abuse | Quantitative Cross-sectional | Respondents who experience CSA and IPV are more likely to report negative general health and suicidal thoughts. CSAs are strongly linked to suicidal ideation. Multivariate logistic analysis shows no significant difference in the odds of suicidality between participants exposed to CSAs and those who were not. |
| Ybarra et al. (2022) United States | N = 582 nonbinary + 329 transgender Age = 13–17 years M. Age = 14.8 (0.7) years | AMAB AFAB | Sexual violence | Quantitative Cross-sectional | GMY are more likely to report experiencing sexual violence but not more likely to report perpetrating it. Risk factors for perpetrating sexual violence vary across gender identities (cisgender, transgender, and nonbinary), which should be considered in prevention programs. Transgender youth exposed to spousal abuse are more likely to report perpetrating sexual violence, compared to those not exposed to such abuse. Nonbinary youth who had experienced sexual harassment are almost 3 times more likely to report perpetrating sexual violence than those who had not. Nonbinary youth exposed to violent or nonviolent pornography are more likely to report using sexual violence. Among nonbinary youth, past-year aggression is associated with increased likelihood of sexual violence perpetration. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the University Association of Education and Psychology. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Fini, G.; Civilotti, C.; Bolognino, A.; Einaudi, G.; Molo, M.; Veglia, F.; Gandino, G.; Finzi, S. The Burden of the Past: A Systematic Review of Childhood Trauma and Mental Health in Transgender and Gender Nonconforming Individuals. Eur. J. Investig. Health Psychol. Educ. 2025, 15, 183. https://doi.org/10.3390/ejihpe15090183
Di Fini G, Civilotti C, Bolognino A, Einaudi G, Molo M, Veglia F, Gandino G, Finzi S. The Burden of the Past: A Systematic Review of Childhood Trauma and Mental Health in Transgender and Gender Nonconforming Individuals. European Journal of Investigation in Health, Psychology and Education. 2025; 15(9):183. https://doi.org/10.3390/ejihpe15090183
Chicago/Turabian StyleDi Fini, Giulia, Cristina Civilotti, Annalisa Bolognino, Gabriele Einaudi, Mariateresa Molo, Fabio Veglia, Gabriella Gandino, and Sarah Finzi. 2025. "The Burden of the Past: A Systematic Review of Childhood Trauma and Mental Health in Transgender and Gender Nonconforming Individuals" European Journal of Investigation in Health, Psychology and Education 15, no. 9: 183. https://doi.org/10.3390/ejihpe15090183
APA StyleDi Fini, G., Civilotti, C., Bolognino, A., Einaudi, G., Molo, M., Veglia, F., Gandino, G., & Finzi, S. (2025). The Burden of the Past: A Systematic Review of Childhood Trauma and Mental Health in Transgender and Gender Nonconforming Individuals. European Journal of Investigation in Health, Psychology and Education, 15(9), 183. https://doi.org/10.3390/ejihpe15090183






