Coping Strategies and Health-Related Quality of Life in Breast Cancer Survivors
Abstract
1. Introduction
2. Materials and Methods
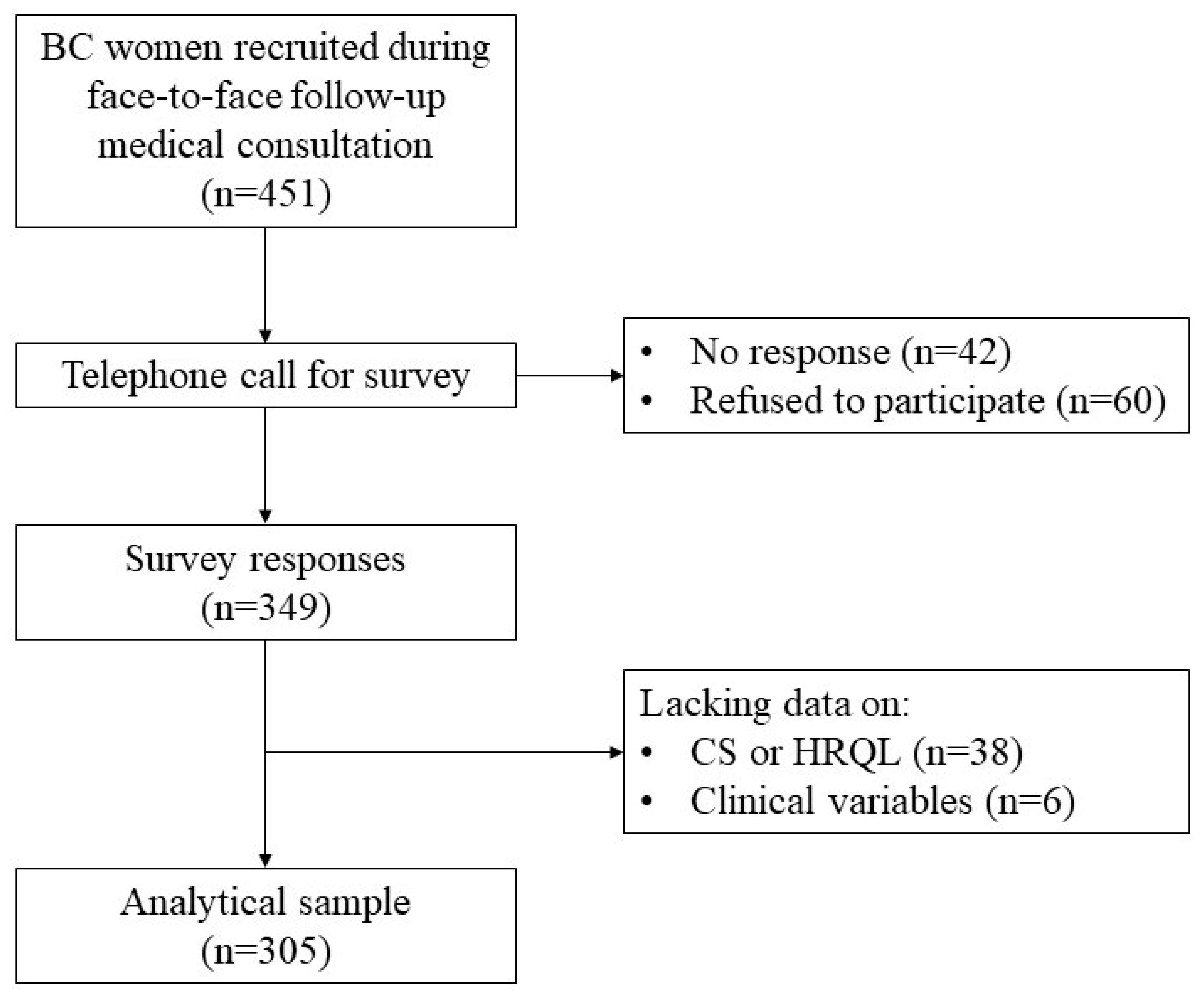
2.1. Study Design and Participants
2.2. Study Variables
2.2.1. Coping Strategies
2.2.2. Health-Related Quality of Life
2.2.3. Other Study Variables
2.2.4. Data Analysis
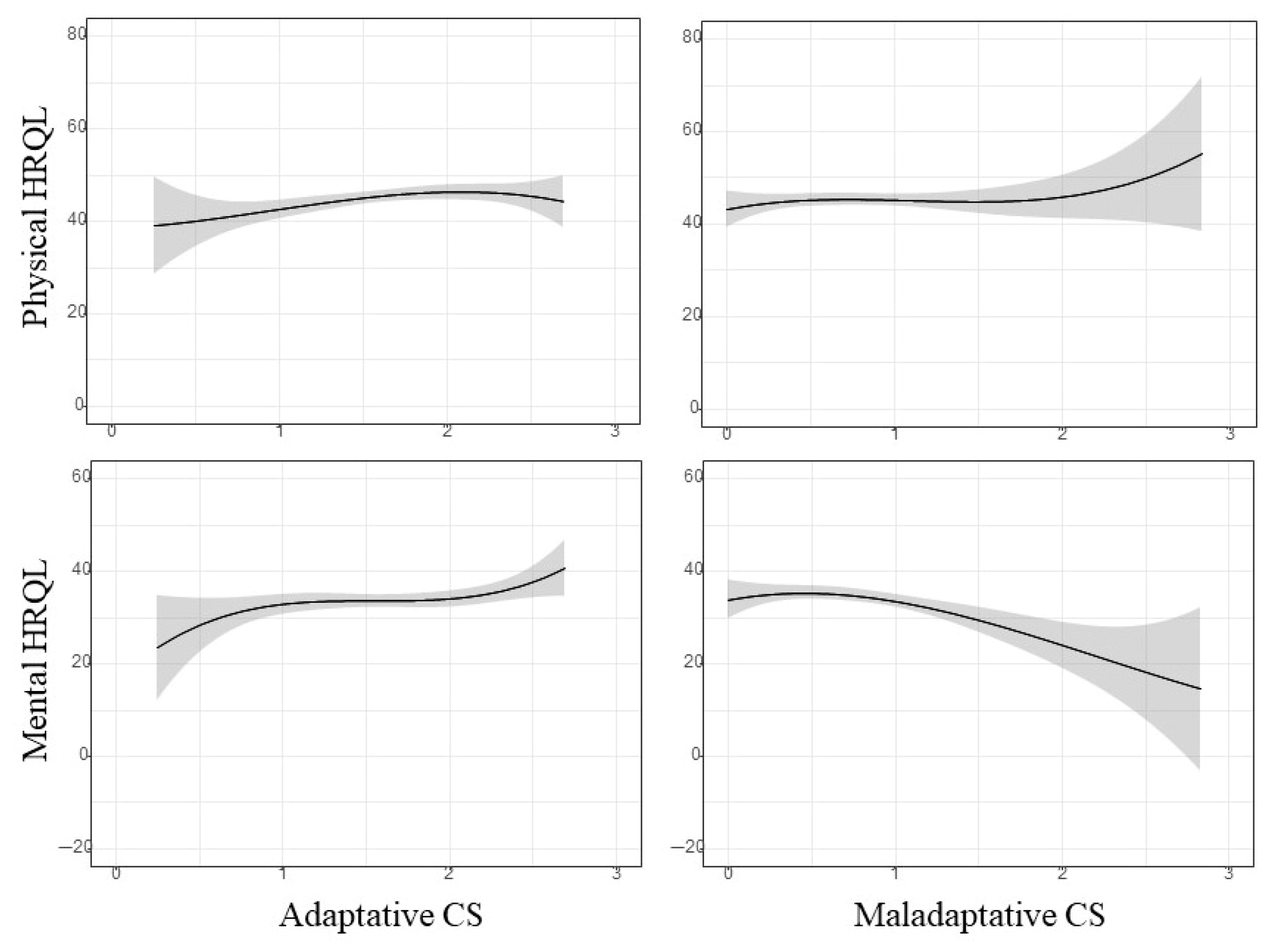
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BC | Breast cancer |
| CSs | Coping strategies |
| HRQoL | Health-related quality of life |
| STROBE | Strengthening the Reporting of Observational Studies in Epidemiology |
References
- Allemani, C., Matsuda, T., Di Carlo, V., Harewood, R., Matz, M., Nikšić, M., Bonaventure, A., Valkov, M., Johnson, C. J., Estève, J., Ogunbiyi, O. J., Azevedo E Silva, G., Chen, W. Q., Eser, S., Engholm, G., Stiller, C. A., Monnereau, A., Woods, R. R., Visser, O., … CONCORD Working Group. (2018). Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): Analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. The Lancet, 391(10125), 1023–1075. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Molero, J., Dierssen-Sotos, T., Gomez-Acebo, I., Fernandez de Larrea Baz, N., Guevara, M., Amiano, P., Castaño-Vinyals, G., Fernandez-Villa, T., Moreno, V., Bayo, J., Molina-Barceloa, A., Fernández-Ortíz, M., Suarez-Calleja, C., Marcos-Gragera, R., Castells, X., Gil-Majuelo, L., Ardanaz, E., Pérez-Gómez, B., Kogevinas, M., … Llorca, J. (2020). Quality of life in a cohort of 1078 women diagnosed with breast cancer in Spain: 7-year follow-up results in the MCC-Spain study. International Journal of Environmental Research and Public Health, 17(22), 8411. [Google Scholar] [CrossRef] [PubMed]
- Avis, N. E., Crawford, S., & Manuel, J. (2005). Quality of life among younger women with breast cancer. Journal of Clinical Oncology, 23(15), 3322–3330. [Google Scholar] [CrossRef]
- Ben-Zur, H. (2009). Coping styles and affect. International Journal of Stress Management, 16(2), 87–101. [Google Scholar] [CrossRef]
- Biggs, A., Brough, P., & Drummond, S. (2017). Lazarus and Folkman’s psychological stress and coping theory. In C. L. Cooper, & J. C. Quick (Eds.), The handbook of stress and health: A guide to research and practice (pp. 351–364). Wiley Blackwell. [Google Scholar] [CrossRef]
- Bray, F., Laversanne, M., Sung, H., Ferlay, J., Siegel, R. L., Soerjomataram, I., & Jemal, A. (2024). Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 74(3), 229–263. [Google Scholar] [CrossRef]
- Calderon, C., Gómez, D., Carmona-Bayonas, A., Hernández, R., Ghanem, I., Gil Raga, M., Ostios, L., García, M., Lopez de Ceballos, M. H., Ferreira, E., & Jiménez-Fonseca, P. (2021). Social support, coping strategies and sociodemographic factors in women with breast cancer. Clinical and Translational Oncology, 23(9), 1955–1960. [Google Scholar] [CrossRef]
- Carver, C. S. (1997). You want to measure coping but your protocol’s too long: Consider the brief COPE. International Journal of Behavioral Medicine, 4(1), 92–100. [Google Scholar] [CrossRef]
- Carver, C. S., Pozo, C., Harris, S. D., Noriega, V., Scheier, M. F., Robinson, D. S., Ketcham, A. S., Moffat, F. L., Jr., & Clark, K. C. (1993). How coping mediates the effect of optimism on distress: A study of women with early stage breast cancer. Journal of Personality Social Psychology, 65(2), 375–390. [Google Scholar] [CrossRef]
- Cathcart-Rake, E. J., Tevaarwerk, A. J., Haddad, T. C., D’Andre, S. D., & Ruddy, K. J. (2023). Advances in the care of breast cancer survivors. British Medical Journal, 382, e071565. [Google Scholar] [CrossRef]
- Chaaya, R., Sfeir, M., Khoury, S. E., Malhab, S. B., & Khoury-Malhame, M. E. (2025). Adaptive versus maladaptive coping strategies: Insight from Lebanese young adults navigating multiple crises. BMC Public Health, 25(1), 1464. [Google Scholar] [CrossRef]
- Compas, B. E., Beckjord, E., Agocha, B., Sherman, M. L., Langrock, A., Grossman, C. I., Dausch, B., Glinder, J., Kaiser, C., Anderson-Hanley, C., & Luecken, L. (2006). Measurement of coping and stress responses in women with breast cancer. Psychooncology, 15(12), 1038–1054. [Google Scholar] [CrossRef]
- Danhauer, S. C., Crawford, S. L., Farmer, D. F., & Avis, N. E. (2009). A longitudinal investigation of coping strategies and quality of life among younger women with breast cancer. Journal of Behavioral Medicine, 32(4), 371–379. [Google Scholar] [CrossRef]
- Deng, T., Zi, H., Guo, X. P., Luo, L. S., Yang, Y. L., Hou, J. X., Zhou, R., Yuan, Q. Q., Liu, Q., Huang, Q., & Wu, G. S. (2025). Global, regional, and national burden of breast cancer, 1990–2021, and projections to 2050: A systematic analysis of the global burden of disease study 2021. Thoracic Cancer, 16(9), e70052. [Google Scholar] [CrossRef] [PubMed]
- Dev, R., Agosta, M., Fellman, B., Reddy, A., Baldwin, S., Arthur, J., Haider, A., Carmack, C., Hui, D., & Bruera, E. (2024). Coping strategies and associated symptom burden among patients with advanced cancer. The Oncologist, 29(2), 166–175. [Google Scholar] [CrossRef] [PubMed]
- Durá-Ferrandis, E., Mandelblatt, J. S., Clapp, J., Luta, G., Faul, L., Kimmick, G., Cohen, H. J., Yung, R. L., & Hurria, A. (2017). Personality, coping, and social support as predictors of long-term quality-of-life trajectories in older breast cancer survivors: CALGB protocol 369901 (Alliance). Psychooncology, 26(11), 1914–1921. [Google Scholar] [CrossRef] [PubMed]
- Durosini, I., Triberti, S., Savioni, L., Sebri, V., & Pravettoni, G. (2022). The role of emotion-related abilities in the quality of life of breast cancer survivors: A systematic review. International Journal of Environmental Research and Public Health, 19(19), 12704. [Google Scholar] [CrossRef]
- Giaquinto, A. N., Sung, H., Miller, K. D., Kramer, J. L., Newman, L. A., Minihan, A., Jemal, A., & Siegel, R. L. (2022). Breast cancer statistics, 2022. CA: A Cancer Journal for Clinicians, 72(6), 524–541. [Google Scholar] [CrossRef]
- Graves, K., Campos, C., Sampayo, I., Duron, Y., Torres, M., & Rush, C. (2020). Community-based workshops to improve quality of life for latina breast cancer survivors and their caregivers. Patient-Centered Outcomes Research Institute (PCORI). [Google Scholar]
- Gudenkauf, L. M., & Ehlers, S. L. (2018). Psychosocial interventions in breast cancer survivorship care. Breast, 38, 1–6. [Google Scholar] [CrossRef]
- Gutiérrez-Hermoso, L., Velasco-Furlong, L., Sánchez-Román, S., Berzal-Pérez, E., Alcocer-Castillejos, N., & Quiroz-Friedman, P. (2022). The effect of treatment and coping on the quality of life in breast cancer patients: A moderated mediation model. Quality of Life Research, 31(1), 147–158. [Google Scholar] [CrossRef]
- Harel, K., Czamanski-Cohen, J., Cohen, M., Caspi, O., & Weihs, K. L. (2025). Coping, emotional processing, and cancer-related symptoms in breast cancer survivors: Cross-sectional secondary analysis of the REPAT study. Psycho-Oncology, 34(2), e70094. [Google Scholar] [CrossRef]
- Hasan, M., Khonji, L., & Narayanan, G. (2024). Review article|relationship between social support, coping strategies, spirituality and psychological status among breast cancer survivors. The Gulf Journal of Oncology, 1(46), 49–53. [Google Scholar]
- Hernández, R., Calderon, C., Carmona-Bayonas, A., Rodríguez-Capote, A., Jara, C., Padilla-Álvarez, A., Gómez-Camacho, M. L., Beato, C., Castelo, B., Majem, M., Muñoz, M. M., Ivars, A., Mangas-Izquierdo, M., Rogado-Revuelta, J., & Jiménez-Fonseca, P. (2019). Differences in coping strategies among young adults and the elderly with cancer. Psychogeriatrics, 19(5), 426–434. [Google Scholar] [CrossRef] [PubMed]
- Jones, L., Barnett, A., & Vagenas, D. (2025). Common misconceptions held by health researchers when interpreting linear regression assumptions, a cross-sectional study. PLoS ONE, 20(6), e0299617. [Google Scholar] [CrossRef] [PubMed]
- Kang, N. E., Kim, H. Y., Kim, J. Y., & Kim, S. R. (2020). Relationship between cancer stigma, social support, coping strategies and psychosocial adjustment among breast cancer survivors. Journal of Clinical Nursing, 29(21–22), 4368–4378. [Google Scholar] [CrossRef] [PubMed]
- Kim, J., Harper, A., McCormack, V., Sung, H., Houssami, N., Morgan, E., Mutebi, M., Garvey, G., Soerjomataram, I., & Fidler-Benaoudia, M. M. (2025). Global patterns and trends in breast cancer incidence and mortality across 185 countries. Nature Medicine, 31(4), 1154–1162. [Google Scholar] [CrossRef]
- Kornblith, A. B., Powell, M., Regan, M. M., Bennett, S., Krasner, C., Moy, B., Younger, J., Goodman, A., Berkowitz, R., & Winer, E. (2007). Long-term psychosocial adjustment of older vs. younger survivors of breast and endometrial cancer. Psychooncology, 16(10), 895–903. [Google Scholar] [CrossRef]
- Kosinski, M., Ware, J. E., Turner-Bowker, D. M., & Gandek, B. (2007). User’s manual for the SF-12v2 health survey: With a supplement documenting the SF-12® health survey. QualityMetric Incorporated. [Google Scholar]
- Lazarus, R. S., & Folkman, S. (2015). Stress, appraisal, and coping. Springer Publishing Company. [Google Scholar]
- Li, J., & Lambert, V. A. (2007). Coping strategies and predictors of general well-being in women with breast cancer in the People’s Republic of China. Nursing & Health Sciences, 9(3), 199–204. [Google Scholar] [CrossRef]
- Mardani, A., Maleki, M., Hanifi, N., Turunen, H., & Vaismoradi, M. (2025). Coping strategies for fear of cancer recurrence among breast cancer survivors: A systematic review and thematic synthesis of qualitative studies. Supportive Care in Cancer: Official Journal of the Multinational Association of Supportive Care in Cancer, 33(6), 459. [Google Scholar] [CrossRef]
- Mehrabi, E., Hajian, S., Simbar, M., Hoshyari, M., & Zayeri, F. (2015). Coping response following a diagnosis of breast cancer: A systematic review. Electronic Physician Journal, 7(8), 1575–1583. [Google Scholar] [CrossRef]
- Mishra, A., Nair, J., & Sharan, A. M. (2023). Coping in post-mastectomy breast cancer survivors and need for intervention: Systematic review. Breast Cancer: Basic and Clinical Research, 17, 11782234231209126. [Google Scholar] [CrossRef]
- Mohammadipour, M., & Pidad, F. (2021). Coping strategies, locus of control, and quality of life in patients with early-stage breast cancer. The Journal of Psychology, 155(4), 375–386. [Google Scholar] [CrossRef] [PubMed]
- Omari, M., Zarrouq, B., Amaadour, L., Benbrahim, Z., El Asri, A., Mellas, N., El Rhazi, K., Ragala, M. A., & Halim, K. (2022). Psychological distress, coping strategies, and quality of life in breast cancer patients under neoadjuvant therapy: Protocol of a systematic review. Cancer Control, 29, 10732748221074735. [Google Scholar] [CrossRef] [PubMed]
- Ośmiałowska, E., Misiąg, W., Chabowski, M., & Jankowska-Polańska, B. (2021). Coping strategies, pain, and quality of life in patients with breast cancer. Journal of Clinical Medicine, 10(19), 4469. [Google Scholar] [CrossRef] [PubMed]
- Paek, M. S., Ip, E. H., Levine, B., & Avis, N. E. (2016). Longitudinal reciprocal relationships between quality of life and coping strategies among women with breast cancer. Annals of Behavioral Medicine, 50(5), 775–783. [Google Scholar] [CrossRef]
- Rand, K. L., Cohee, A. A., Monahan, P. O., Wagner, L. I., Shanahan, M. L., & Champion, V. L. (2019). Coping among breast cancer survivors: A confirmatory factor analysis of the brief COPE. Journal of Nursing Measurement, 27(2), 259–276. [Google Scholar] [CrossRef]
- Reynolds, P., Hurley, S., Torres, M., Jackson, J., Boyd, P., & Chen, V. W. (2000). Use of coping strategies and breast cancer survival: Results from the black/white cancer survival study. American Journal of Epidemiology, 152, 940–949. [Google Scholar] [CrossRef]
- Rodrigues, F., Figueiredo, N., Rodrigues, J., Ferreira, R., Hernández-Mendo, A., & Monteiro, D. (2022). A comprehensive review and bifactor modeling analysis of the brief COPE. Inquiry, 59, 469580221108127. [Google Scholar] [CrossRef]
- Roszkowska, M., & Białczyk, K. (2023). Coping styles and quality of life in breast cancer patients undergoing radiotherapy. Cancers, 15(23), 5515. [Google Scholar] [CrossRef]
- Senger, A. R., G Ratcliff, C., K Semelsberger, R., Chaoul, A., & Cohen, L. (2024). The role of coping and posttraumatic stress in fostering posttraumatic growth and quality of life among women with breast cancer. Journal of Clinical Psychology in Medical Settings, 31(2), 368–378. [Google Scholar] [CrossRef]
- Skinner, E. A., Edge, K., Altman, J., & Sherwood, H. (2003). Searching for the structure of coping: A review and critique of category systems for classifying ways of coping. Psychological Bulletin, 129, 216–269. [Google Scholar] [CrossRef]
- Solberg, M. A., Gridley, M. K., & Peters, R. M. (2022). The factor structure of the brief cope: A systematic review. Wester Journal of Nursing Research, 44(6), 612–627. [Google Scholar] [CrossRef] [PubMed]
- Stallman, H. M. (2020). Health theory of coping. Australian Psychologist, 55(4), 295–306. [Google Scholar] [CrossRef]
- Taylor, T. R., Adams-Campbell, L. L., Hicks, J., Barrow, J., Makambi, K. H., Warren, J., Vinod, N., & Dash, C. (2025). The relationship between psychosocial support service utilization, coping and post-traumatic growth among breast cancer survivors. Journal of Psychosocial Oncology, 9, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Torralba-Martínez, E., Quintana, M. J., Carbonell, M. C., de Las Sias, E., Carrillo, C. P. S., & Codern-Bové, N. (2022). Coping experiences of women in the different phases of breast cancer. Supportive Care of Cancer, 30(1), 197–206. [Google Scholar] [CrossRef]
- Toscano, A., Blanchin, M., Bourdon, M., Bonnaud-Antignac, A., & Sébille, V. (2020). Longitudinal associations between coping strategies, locus of control and health-related quality of life in patients with breast cancer or melanoma. Quality of Life Research, 29(5), 1271–1279. [Google Scholar] [CrossRef]
- Velasco, L., Gutiérrez-Hermoso, L., Alcocer-Castillejos, N., Quiroz-Friedman, P., Peñacoba, C., Catalá, P., & Sánchez-Román, S. (2020). Association between quality of life and positive coping strategies in breast cancer patients. Women Health, 60(9), 1063–1069. [Google Scholar] [CrossRef]
- Vilagut, G., Valderas, J. M., Ferrer, M., Garin, O., López-García, E., & Alonso, J. (2008). Interpretation of SF-36 and SF-12 questionnaires in Spain: Physical and mental components. Medicina Clinica, 130(19), 726–735. [Google Scholar] [CrossRef]
- Walsh, L. E., Dunderdale, L., Horick, N., Temel, J. S., Greer, J. A., & Jacobs, J. M. (2024). Intervention-related changes in coping ability drives improvements in mood and quality of life for patients taking adjuvant endocrine therapy. Psycho-Oncology, 33(12), e70049. [Google Scholar] [CrossRef]
- Watson, M., Homewood, J., & Haviland, J. (2012). Coping response and survival in breast cancer patients: A new analysis. Stress Health, 28(5), 376–380. [Google Scholar] [CrossRef]
- Zamanian, H., Amini-Tehrani, M., Mahdavi-Adeli, A., Daryaafzoon, M., Arsalani, M., Enzevaei, A., & Farjami, M. (2021). Sense of coherence and coping strategies: How they influence quality of life in Iranian women with breast cancer. Nursing Open, 8(4), 1731–1740. [Google Scholar] [CrossRef]
- Zhou, K., Ning, F., Wang, X., Wang, W., Han, D., & Li, X. (2022). Perceived social support and coping style as mediators between resilience and health-related quality of life in women newly diagnosed with breast cancer: A cross-sectional study. BMC Womens Health, 22(1), 198. [Google Scholar] [CrossRef]
| Total, n (%) | Physical HRQoL, Mean (sd) | Mental HRQoL, Mean (sd) | ||
|---|---|---|---|---|
| Participants | 305 (100) | 45.0 (9.09) | 33.9 (9.76) | |
| Age at diagnosis | ||||
| <45 years | 80 (26.2) | 46.0 (9.91) | 32.7 (8.33) | |
| 45–59 years | 160 (52.5) | 46.0 (8.47) | 33.5 (9.92) | |
| ≥60 years | 65 (21.3) | 41.4 (9.99) | 36.0 (10.7) | |
| Living arrangement | ||||
| Lives alone | 54 (17.7) | 44.6 (9.22) | 33.8 (10.5) | |
| Accompanied | 251 (82.3) | 45.1 (9.08) | 33.9 (9.61) | |
| Children | ||||
| None | 69 (22.6) | 48.1 (6.27) | 33.8 (8.52) | |
| 1 child | 91 (29.8) | 46.4 (8.29) | 33.8 (9.84) | |
| 2 or more children | 145 (47.6) | 42.7 (10.1) | 33.9 (10.3) | |
| Level of studies | ||||
| Primary | 47 (15.4) | 39.5 (11.1) | 33.5 (9.96) | |
| Secondary | 168 (55.1) | 44.5 (8.68) | 33.5 (10.1) | |
| University | 90 (29.5) | 49.0 (6.71) | 34.7 (8.93) | |
| Multiple cancers | ||||
| No | 266 (87.2) | 45.1 (9.02) | 34.1 (9.42) | |
| Yes | 39 (12.8) | 44.3 (9.69) | 32.5 (11.9) | |
| Stage of BC | ||||
| Local | 184 (60.3) | 44.9 (9.40) | 32.3 (9.97) | |
| Regional or advanced | 121 (39.7) | 45.1 (8.64) | 36.2 (8.96) | |
| Diagnostic delay a | ||||
| ≤1 week | 148 (48.5) | 46.1 (8.25) | 34.3 (9.72) | |
| >1 week | 157 (51.5) | 44.0 (9.75) | 33.4 (9.80) | |
| Therapeutic delay a | ||||
| ≤4 weeks | 149 (48.9) | 44.7 (9.19) | 34.1 (9.67) | |
| >4 weeks | 156 (51.1) | 45.3 (9.02) | 33.6 (9.86) | |
| Chemotherapy | ||||
| No | 204 (66.9) | 45.1 (9.21) | 33.1 (9.70) | |
| Yes | 101 (33.1) | 44.8 (8.89) | 35.3 (9.75) | |
| Radiotherapy | ||||
| No | 142 (46.6) | 46.1 (9.01) | 33.0 (9.88) | |
| Yes | 163 (53.4) | 44.0 (9.08) | 34.6 (9.62) | |
| Hormone therapy | ||||
| No | 207 (67.9) | 45.9 (9.03) | 33.9 (9.92) | |
| Yes | 98 (32.1) | 43.1 (8.98) | 33.8 (9.44) | |
| Targeted/Immunotherapy | ||||
| No | 289 (94.7) | 45.0 (9.14) | 33.8 (9.79) | |
| Yes | 16 (5.25) | 45.8 (8.37) | 34.9 (9.41) | |
| Physical HRQoL | Mental HRQoL | ||||
|---|---|---|---|---|---|
| Coefficient (95%CI) | p-Value | Coefficient (95%CI) | p-Value | ||
| Adaptive CS | |||||
| Model 1 a | 2.10 (0.04; 4.16) | 0.046 | 2.77 (0.37; 5.16) | 0.024 | |
| Model 2 b | 2.19 (0.11; 4.27) | 0.039 | 2.65 (0.25; 5.04) | 0.030 | |
| Maladaptive CS | |||||
| Model 1 a | 0.10 (−2.26; 2.46) | 0.931 | −3.97 (−6.69; −1.27) | 0.004 | |
| Model 2 b | 0.02 (−2.35; 2.40) | 0.984 | −3.92 (−6.62; −1.22) | 0.005 | |
| Physical HRQoL | Mental HRQoL | ||||
|---|---|---|---|---|---|
| Coefficient (95%CI) a | p-Value | Coefficient (95%CI) a | p-Value | ||
| Adaptive CSs | |||||
| Emotional support | 0.04 (−1.11; 1.19) | 0.941 | −0.10 (−1.43; 1.22) | 0.877 | |
| Positive reframing | 0.73 (−0.34; 1.80) | 0.182 | 0.63 (−0.56; 1.91) | 0.280 | |
| Acceptance | 0.93 (−0.55; 2.40) | 0.217 | 2.78 (1.11; 4.46) | 0.001 | |
| Religion | 0.55 (−0.36; 1.47) | 0.235 | 0.28 (−077; 1.34) | 0.598 | |
| Humor | 1.01 (−0.19; 2.21) | 0.100 | 0.52 (−0.87; 1.91) | 0.465 | |
| Active coping | 0.84 (−0.31; 1.99) | 0.153 | 2.26 (0.95; 3.57) | 0.001 | |
| Planning | 1.11 (0.00; 2.21) | 0.050 | 1.43 (0.16; 2.71) | 0.027 | |
| Instrumental support | 0.04 (−1.01; 1.10) | 0.937 | −0.55 (−1.77; 0.66) | 0.371 | |
| Maladaptive CSs | |||||
| Denial | −0.90 (−1.90; 0.09) | 0.075 | −1.91 (−3.05; −0.78) | 0.001 | |
| Substance use | 0.70 (−2.12; 3.53) | 0.624 | −1.73 (−4.98; 1.51) | 0.293 | |
| Behavioral disengagement | −0.81 (−2.47; 0.84) | 0.334 | −1.81 (−3.71; 0.08) | 0.060 | |
| Self-distraction | 0.83 (−0.15; 1.82) | 0.099 | 0.76 (−0.37; 1.90) | 0.188 | |
| Self-blame | 0.09 (−1.59; 1.78) | 0.911 | −2.41 (−4.33; −0.49) | 0.014 | |
| Venting | 0.34 (−0.81; 1.50) | 0.554 | −1.73 (−3.04; −0.42) | 0.010 | |
| Physical HRQoL | Mental HRQoL | ||||
|---|---|---|---|---|---|
| Coefficient (95%CI) a | p-Value | Coefficient (95%CI) a | p-Value | ||
| Adaptive CSs | |||||
| <45 years old | 2.98 (0.40; 5.56) | 0.024 | 2.99 (−0.11; 6.10) | 0.059 | |
| High school or less | 2.79 (0.15; 5.43) | 0.038 | 2.85 (−0.03; 5.74) | 0.053 | |
| Total delay b ≥6 weeks | 4.27 (0.96; 7.58) | 0.012 | 0.92 (−3.08; 4.92) | 0.649 | |
| Regional/advanced stage | −1.86 (−4.99; 1.26) | 0.240 | 0.61 (−2.90; 4.13) | 0.730 | |
| ≥2 additional treatments | 1.46 (−2.11; 5.02) | 0.420 | 1.51 (−2.71; 5.73) | 0.480 | |
| Maladaptive CSs | |||||
| <45 years old | −1.07 (−3.98; 1.82) | 0.465 | −4.66 (−8.09; −1.24) | 0.008 | |
| High school or less | 1.32 (−1.60; 4.25) | 0.373 | −3.80 (−6.96; −0.64) | 0.019 | |
| Total delay b ≥6 weeks | 1.52 (−1.87; 4.92) | 0.376 | −4.68 (−8.61; −0.76) | 0.020 | |
| Regional/advanced stage | −0.92 (−4.64; 2.78) | 0.621 | 0.13 (−4.03; 4.29) | 0.952 | |
| ≥2 additional treatments | −3.22 (−7.24; 0.80) | 0.115 | −3.11 (−7.88; 1.66) | 0.199 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the University Association of Education and Psychology. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Agrelo-Fernández, A.; Fernández-Arce, L.; Llaneza-Folgueras, A.; Encinas-Muñiz, A.I.; del Valle, M.O.; Lana, A. Coping Strategies and Health-Related Quality of Life in Breast Cancer Survivors. Eur. J. Investig. Health Psychol. Educ. 2025, 15, 139. https://doi.org/10.3390/ejihpe15070139
Agrelo-Fernández A, Fernández-Arce L, Llaneza-Folgueras A, Encinas-Muñiz AI, del Valle MO, Lana A. Coping Strategies and Health-Related Quality of Life in Breast Cancer Survivors. European Journal of Investigation in Health, Psychology and Education. 2025; 15(7):139. https://doi.org/10.3390/ejihpe15070139
Chicago/Turabian StyleAgrelo-Fernández, Ana, Lucía Fernández-Arce, Ana Llaneza-Folgueras, Ana Isabel Encinas-Muñiz, María Olivo del Valle, and Alberto Lana. 2025. "Coping Strategies and Health-Related Quality of Life in Breast Cancer Survivors" European Journal of Investigation in Health, Psychology and Education 15, no. 7: 139. https://doi.org/10.3390/ejihpe15070139
APA StyleAgrelo-Fernández, A., Fernández-Arce, L., Llaneza-Folgueras, A., Encinas-Muñiz, A. I., del Valle, M. O., & Lana, A. (2025). Coping Strategies and Health-Related Quality of Life in Breast Cancer Survivors. European Journal of Investigation in Health, Psychology and Education, 15(7), 139. https://doi.org/10.3390/ejihpe15070139






