Loneliness as a Public Health Challenge: A Systematic Review and Meta-Analysis to Inform Policy and Practice
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
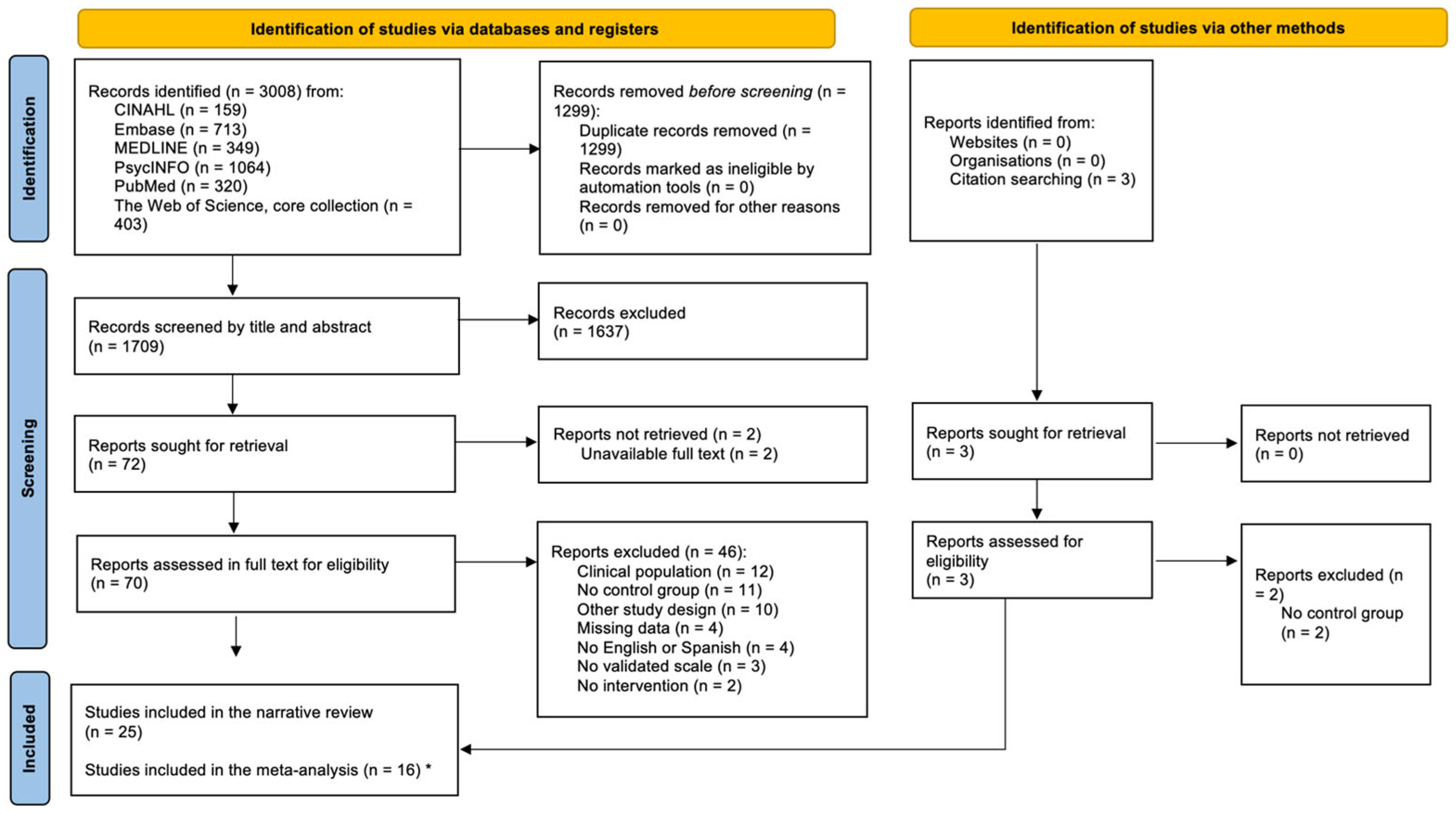
2.2. Search Strategy and Study Selection
2.3. Data Extraction and Quality Assessment
2.4. Statistical Analysis
3. Results
3.1. Characteristics of the Included Studies
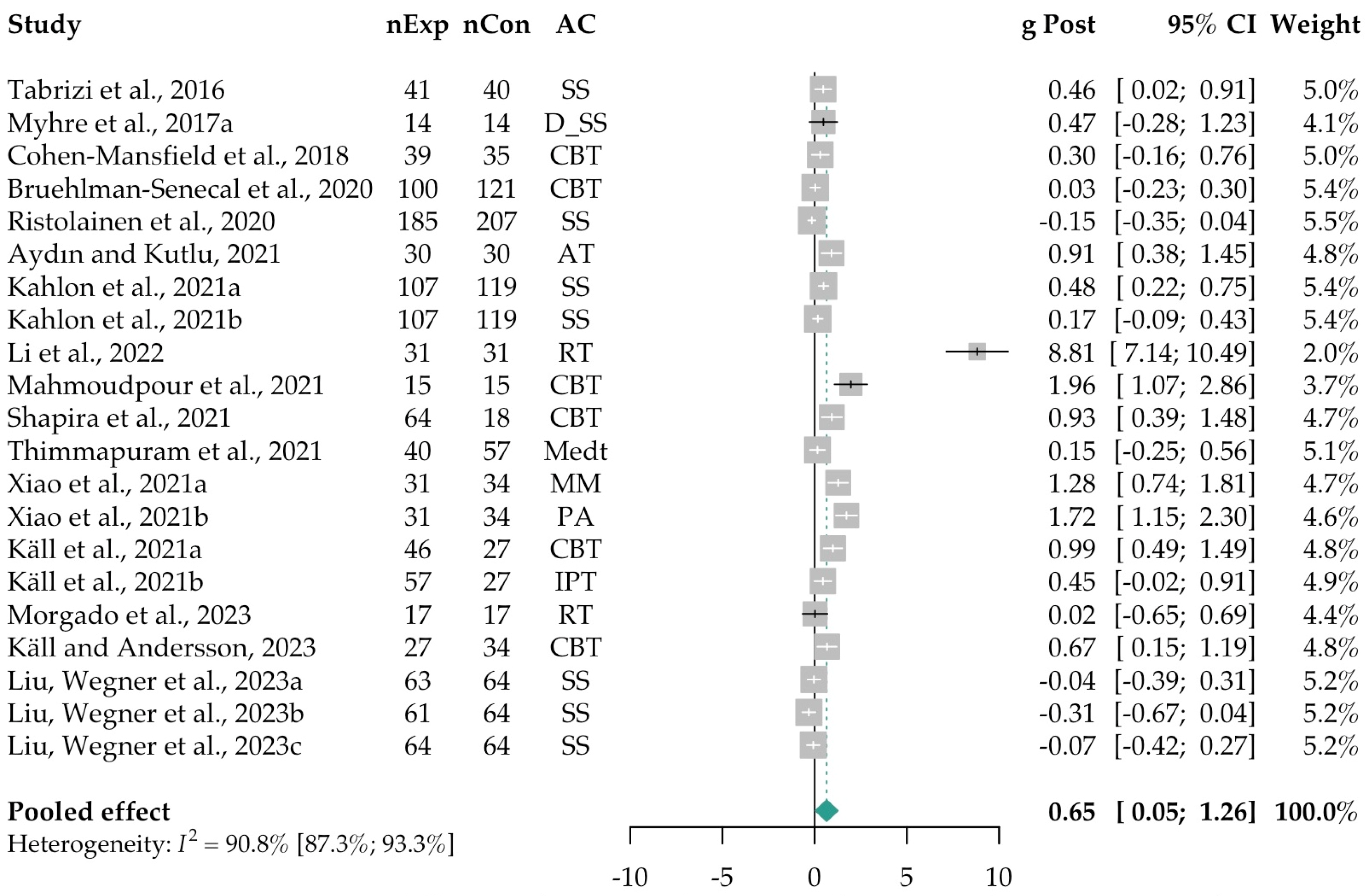
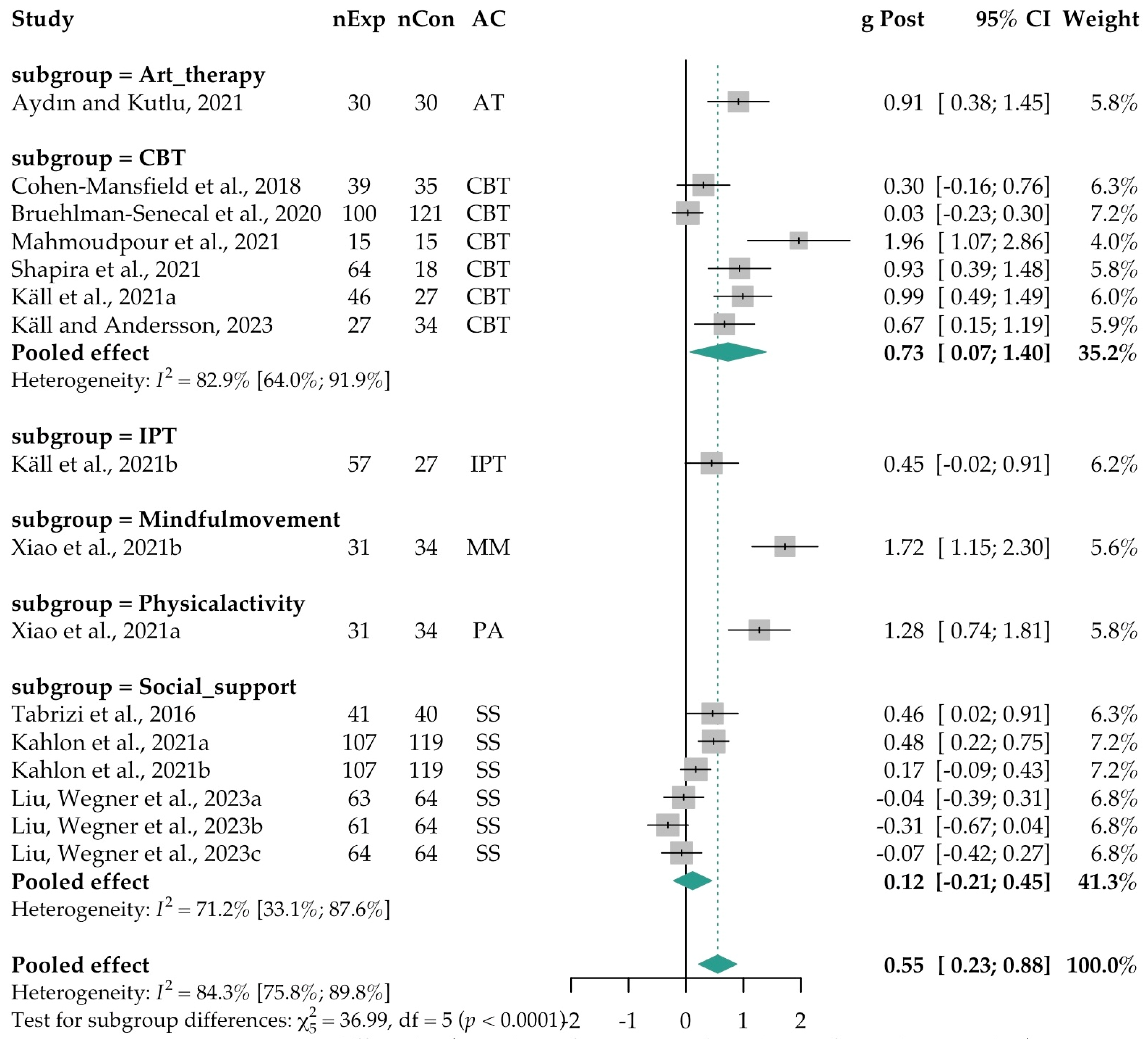
3.2. Meta-Analysis
3.3. Risk of Publication Bias
3.4. Moderation and Subgroup Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| AC | Main Active Component used in the intervention |
| ACT | Acceptance and Commitment Therapy |
| AT | Art Therapy |
| CBT | Cognitive Behavioral Therapy |
| CI | Confidence Interval |
| CG | Control Group |
| Coll | Collectivistic |
| DA | Delayed Access |
| DJLS | de Jong–Gierveld Loneliness scale |
| D-SS | Digital Social Support |
| I-C | Intervention vs. Control |
| I-I | Intervention vs. Intervention |
| Ind | Individualistic |
| INSPECT-SR | INveStigating ProblEmatic Clinical Trials in Systematic Reviews |
| IPT | Internet-Based Interpersonal Therapy |
| MM | Mindful Movement |
| Medt | Meditation |
| NHS | National Health System |
| NI | No Intervention |
| NNT | Number Needed to Treat |
| N-On | Non-online Interaction Group |
| N/r | Number of sessions not reported |
| n/r | Length or age not reported |
| OD | Online Diary |
| OSF | Open Science Framework |
| PA | Physical Activity |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| RCT | Randomized Controlled Trial |
| RoB | Risk of Bias |
| SS | Social Support |
| SMD | Standardized Mean Differences |
| UCLA (v3) | University of Los Angeles Loneliness scale (version three) |
| UK | United Kingdom |
| VI | Virtual Interaction with Strangers |
| WL | Waiting List |
| WHO | World Health Organization |
| YT-i | YouTube interaction |
References
- Arsenijevic, J., & Groot, W. (2018). Does household help prevent loneliness among the elderly? An evaluation of a policy reform in the Netherlands. BMC Public Health, 18(1), 1104. [Google Scholar] [CrossRef]
- Astell-Burt, T., Hartig, T., Putra, I. G. N. E., Walsan, R., Dendup, T., & Feng, X. (2022). Green space and loneliness: A systematic review with theoretical and methodological guidance for future research. Science of the Total Environment, 847, 157521. [Google Scholar] [CrossRef]
- **Aydın, M., & Kutlu, F. Y. (2021). The effect of group art therapy on loneliness and hopelessness levels of older adults living alone: A randomized controlled study. Florence Nightingale Journal of Nursing, 29(3), 271–284. [Google Scholar] [CrossRef]
- Barreto, M., Victor, C., Hammond, C., Eccles, A., Richins, M. T., & Qualter, P. (2021). Loneliness around the world: Age, gender, and cultural differences in loneliness. Personality and Individual Differences, 169, 110066. [Google Scholar] [CrossRef]
- Barton, J., & Pretty, J. (2010). What is the best dose of nature and green exercise for improving mental health? A multi-study analysis. Environmental Science & Technology, 44(10), 3947–3955. [Google Scholar] [CrossRef]
- Begg, C. B., & Mazumdar, M. (1994). Operating characteristics of a rank correlation test for publication bias. Biometrics, 50(4), 1088–1101. [Google Scholar] [CrossRef]
- **Bruehlman-Senecal, E., Hook, C. J., Pfeifer, J. H., FitzGerald, C., Davis, B., Delucchi, K. L., Haritatos, J., & Ramo, D. E. (2020). Smartphone app to address loneliness among college students: Pilot randomized controlled trial. JMIR Mental Health, 7(10), e21496. [Google Scholar] [CrossRef]
- Cacioppo, J. T., & Hawkley, L. C. (2009). Perceived social isolation and cognition. Trends in Cognitive Sciences, 13(10), 447–454. [Google Scholar] [CrossRef]
- Cacioppo, J. T., Hawkley, L. C., Crawford, L. E., Ernst, J. M., Burleson, M. H., Kowalewski, R. B., Malarkey, W. B., Van Cauter, E., & Berntson, G. G. (2002). Loneliness and health: Potential mechanisms. Psychosomatic Medicine, 64(3), 407–417. [Google Scholar] [CrossRef]
- Cacioppo, J. T., & Patrick, W. (2008). Loneliness: Human nature and the need for social connection. WW Norton & Company. [Google Scholar]
- Cacioppo, S., & Cacioppo, J. T. (2012). Decoding the invisible forces of social connections. Frontiers in Integrative Neuroscience, 6, 51. [Google Scholar] [CrossRef]
- Cacioppo, S., Capitanio, J. P., & Cacioppo, J. T. (2014). Toward a neurology of loneliness. Psychological Bulletin, 140(6), 1464–1504. [Google Scholar] [CrossRef]
- Carstensen, L. L., Fung, H. H., & Charles, S. T. (2003). Socioemotional selectivity theory and the regulation of emotion in the second half of life. Motivation and Emotion, 27, 103–123. [Google Scholar] [CrossRef]
- Cohen, J. (1992). A power primer. Psychological Bulletin, 112(1), 155–159. [Google Scholar] [CrossRef]
- Cohen, S., & Wills, T. A. (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98(2), 310–357. [Google Scholar] [CrossRef]
- **Cohen-Mansfield, J., Hazan, H., Lerman, Y., Shalom, V., Birkenfeld, S., & Cohen, R. (2018). Efficacy of the I-SOCIAL intervention for loneliness in old age: Lessons from a randomized controlled trial. Journal of Psychiatric Research, 99, 69–75. [Google Scholar] [CrossRef]
- Cohen-Mansfield, J., & Perach, R. (2015). Interventions for alleviating loneliness among older persons: A critical review. American Journal of Health Promotion, 29(3), e109–e125. [Google Scholar] [CrossRef]
- Cuijpers, P. (2016). Meta-analyses in mental health research: A practical guide (Vol. 15). Vrije Universiteit Amsterdam. [Google Scholar]
- de Oliveira, A. M., Radanovic, M., de Mello, P. C., Buchain, P. C., Vizzotto, A. D., Celestino, D. L., Stella, F., Piersol, C. V., & Forlenza, O. V. (2015). Nonpharmacological interventions to reduce behavioral and psychological symptoms of dementia: A systematic review. BioMed Research International, 2015, 218980. [Google Scholar] [CrossRef]
- DerSimonian, R., & Kacker, R. (2007). Random-effects model for meta-analysis of clinical trials: An update. Contemporary Clinical Trials, 28(2), 105–114. [Google Scholar] [CrossRef]
- DerSimonian, R., & Laird, N. (2015). Meta-analysis in clinical trials revisited. Contemporary Clinical Trials, 45, 139–145. [Google Scholar] [CrossRef]
- Duval, S., & Tweedie, R. (2000). Trim and fill: A simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics, 56(2), 455–463. [Google Scholar] [CrossRef]
- Eccles, A. M., & Qualter, P. (2021). Alleviating loneliness in young people—A meta-analysis of interventions. Child and Adolescent Mental Health, 26(1), 17–33. [Google Scholar] [CrossRef]
- Egger, M., Smith, G. D., Schneider, M., & Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. British Medical Journal, 315(7109), 629–634. [Google Scholar] [CrossRef]
- Fu, Z., Yan, M., & Meng, C. (2022). The effectiveness of remote delivered intervention for loneliness reduction in older adults: A systematic review and meta-analysis. Frontiers in Psychology, 13, 935544. [Google Scholar] [CrossRef]
- Gardiner, C., Geldenhuys, G., & Gott, M. (2018). Interventions to reduce social isolation and loneliness among older people: An integrative review. Health & Social Care in the Community, 26(2), 147–157. [Google Scholar] [CrossRef]
- Hammoud, R., Tognin, S., Bakolis, I., Ivanova, D., Fitzpatrick, N., Burgess, L., Smythe, M., Gibbons, J., Davidson, N., & Mechelli, A. (2021). Lonely in a crowd: Investigating the association between overcrowding and loneliness using smartphone technologies. Scientific Reports, 11(1), 24134. [Google Scholar] [CrossRef]
- Hickin, N., Käll, A., Shafran, R., Sutcliffe, S., Manzotti, G., & Langan, D. (2021). The effectiveness of psychological interventions for loneliness: A systematic review and meta-analysis. Clinical Psychology Review, 88, 102066. [Google Scholar] [CrossRef]
- Higgins, J. P., Altman, D. G., & Sterne, J. A. (2011). Chapter 8: Assessing risk of bias in included studies. Cochrane Handbook for Systematic Reviews of Interventions Version, 5, 182–228. [Google Scholar]
- Higgins, J. P., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. British Medical Journal, 327(7414), 557–560. [Google Scholar] [CrossRef]
- Higgins, J. P. T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M. J., & Welch, V. A. (Eds.). (2023). Cochrane handbook for systematic reviews of interventions version 6.4. (Updated August 2023) (2nd ed.). Cochrane. Available online: www.training.cochrane.org/handbook (accessed on 20 March 2023).
- Hoang, P., King, J. A., Moore, S., Moore, K., Reich, K., Sidhu, H., Tan, C. V., Whaley, C., & McMillan, J. (2022). Interventions associated with reduced loneliness and social isolation in older adults: A systematic review and meta-analysis. JAMA Network Open, 5(10), e2236676. [Google Scholar] [CrossRef]
- Hofstede, G., Hofstede, G. J., & Minkov, M. (2010). Cultures and organizations: Software of the mind (3rd ed.). McGraw-Hill Professional. [Google Scholar]
- Holt-Lunstad, J. (2017). The potential public health relevance of social isolation and loneliness: Prevalence, epidemiology, and risk factors. Public Policy & Aging Report, 27(4), 127–130. [Google Scholar] [CrossRef]
- Holt-Lunstad, J., Smith, T. B., Baker, M., Harris, T., & Stephenson, D. (2015). Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspectives on Psychological Science, 10(2), 227–237. [Google Scholar] [CrossRef]
- Holt-Lunstad, J., Smith, T. B., & Layton, J. B. (2010). Social relationships and mortality risk: A meta-analytic review. PLoS Med, 7(7), e1000316. [Google Scholar] [CrossRef]
- Hom, M. A., Chu, C., Rogers, M. L., & Joiner, T. E. (2020). A Meta-Analysis of the Relationship Between Sleep Problems and Loneliness. Clinical Psychological Science, 8(5), 799–824. [Google Scholar] [CrossRef]
- *Hussain, Z., Ferreira, R., & Kuss, D. J. (2023). The feasibility of smartphone interventions to decrease problematic use of social networking sites: A randomised controlled trial. Psychiatry Research Communications, 100132. [Google Scholar] [CrossRef]
- IntHout, J., Ioannidis, J. P., Rovers, M. M., & Goeman, J. J. (2016). Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open, 6(7), e010247. [Google Scholar] [CrossRef]
- Jarvis, M. A., Padmanabhanunni, A., Balakrishna, Y., & Chipps, J. (2020). The effectiveness of interventions addressing loneliness in older persons: An umbrella review. International Journal of Africa Nursing Sciences, 12, 100177. [Google Scholar] [CrossRef]
- **Kahlon, M. K., Aksan, N., Aubrey, R., Clark, N., Cowley-Morillo, M., Jacobs, E. A., Mundhenk, R., Sebastian, K. R., & Tomlinson, S. (2021). Effect of layperson-delivered, empathy-focused program of telephone calls on loneliness, depression, and anxiety among adults during the COVID-19 pandemic: A randomized clinical trial. Journal of American Medical Association Psychiatry, 78(6), 616–622. [Google Scholar] [CrossRef]
- **Käll, A., & Andersson, G. (2023). Knowledge acquisition following internet-based cognitive behavioural therapy for loneliness—A secondary analysis of a randomised controlled trial. Journal of Behavior Therapy and Experimental Psychiatry, 81, 101872. [Google Scholar] [CrossRef]
- **Käll, A., Backlund, U., Shafran, R., & Andersson, G. (2020a). Lonesome no more? A two-year follow-up of internet-administered cognitive behavioral therapy for loneliness. Internet Interventions, 19, 100301. [Google Scholar] [CrossRef]
- **Käll, A., Bäck, M., Welin, C., Åman, H., Bjerkander, R., Wänman, M., Lindegaard, T., Berg, M., Moche, H., Shafran, R., & Andersson, G. (2021). Therapist-guided internet-based treatments for loneliness: A randomized controlled three-arm trial comparing cognitive behavioral therapy and interpersonal psychotherapy. Psychotherapy and Psychosomatics, 90(5), 351–358. [Google Scholar] [CrossRef]
- **Käll, A., Jägholm, S., Hesser, H., Andersson, F., Mathaldi, A., Norkvist, B. T., Shafran, R., & Andersson, G. (2020b). Internet-based cognitive behavior therapy for loneliness: A pilot randomized controlled trial. Behavior Therapy, 51(1), 54–68. [Google Scholar] [CrossRef]
- Kraemer, H. C., & Kupfer, D. J. (2006). Size of treatment effects and their importance to clinical research and practice. Biological Psychiatry, 59(11), 990–996. [Google Scholar] [CrossRef] [PubMed]
- Lang, T., & Rayner, G. (2012). Ecological public health: The 21st century’s big idea? BMJ, 345, e5466. [Google Scholar] [CrossRef] [PubMed]
- *Lanser, I., & Eisenberger, N. I. (2023). Prosocial behavior reliably reduces loneliness: An investigation across two studies. Emotion, 23(6), 1781. [Google Scholar] [CrossRef]
- Laupacis, A., Sackett, D. L., & Roberts, R. S. (1988). An assessment of clinically useful measures of the consequences of treatment. New England Journal of Medicine, 318(26), 1728–1733. [Google Scholar] [CrossRef] [PubMed]
- Leavell, M. A., Leiferman, J. A., Gascon, M., Braddick, F., Gonzalez, J. C., & Litt, J. S. (2019). Nature-Based Social Prescribing in Urban Settings to Improve Social Connectedness and Mental Well-being: A Review. Current Environment Health Report, 6, 297–308. [Google Scholar] [CrossRef]
- **Li, S., Dai, Y., Zhou, Y., Zhang, J., & Zhou, C. (2022). Efficacy of group reminiscence therapy based on Chinese traditional festival activities (CTFA-GRT) on loneliness and perceived stress of rural older adults living alone in China: A randomized controlled trial. Aging & Mental Health, 26(7), 1377–1384. [Google Scholar] [CrossRef]
- *Lindsay, E. K., Young, S., Brown, K. W., Smyth, J. M., & Creswell, J. D. (2019). Mindfulness training reduces loneliness and increases social contact in a randomized controlled trial. Proceedings of the National Academy of Sciences, 116(9), 3488–3493. [Google Scholar] [CrossRef]
- *Liu, C. W., Hsieh, P. L., Yang, S. Y., Lin, Y. L., & Wang, J. Y. (2023). The effectiveness of facilitator-led remote interactive intervention for loneliness, quality of life, and social support among seniors in communities during the COVID-19 pandemic: A randomized controlled experiment. Psychology & Health, 39, 1675–1688. [Google Scholar] [CrossRef]
- **Liu, S., Wegner, L., Haucke, M., Gates, J., Adam, M., & Bärnighausen, T. (2023). An entertainment-education video and written messages to alleviate loneliness in Germany: Pilot randomized controlled study. Journal of Medical Internet Research Formative Research, 7(1), e43036. [Google Scholar] [CrossRef]
- Lykes, V. A., & Kemmelmeier, M. (2014). What predicts loneliness? Cultural difference between individualistic and collectivistic societies in Europe. Journal of Cross-Cultural Psychology, 45(3), 468–490. [Google Scholar] [CrossRef]
- Maes, M., Qualter, P., Vanhalst, J., Van den Noortgate, W., & Goossens, L. (2019). Gender differences in loneliness across the lifespan: A meta–analysis. European Journal of Personality, 33(6), 642–654. [Google Scholar] [CrossRef]
- **Mahmoudpour, A., Rayesh, N., Ghanbarian, E., & Rezaee, M. (2021). Effectiveness of acceptance and commitment therapy (ACT) on emotional regulation and loneliness of divorced women in Iran. Journal of Marital and Family Therapy, 47(4), 831–842. [Google Scholar] [CrossRef]
- Masi, C. M., Chen, H. Y., Hawkley, L. C., & Cacioppo, J. T. (2011). A meta-analysis of interventions to reduce loneliness. Personality and Social Psychology Review, 15(3), 219–266. [Google Scholar] [CrossRef] [PubMed]
- Mezuk, B., Rock, A., Lohman, M. C., & Choi, M. (2014). Suicide risk in long-term care facilities: A systematic review. International Journal of Geriatric Psychiatry, 29(12), 1198–1211. [Google Scholar] [CrossRef]
- **Morgado, B., Fonseca, C., Afonso, A., Amaro, P., Lopes, M., & de Pinho, L. G. (2023). “Geriatric Proximity” Intervention in COVID-19 Context: Contribution to Reducing Loneliness and Improving Affectivity. Geriatrics, 8(2), 39. [Google Scholar] [CrossRef]
- **Myhre, J. W., Mehl, M. R., & Glisky, E. L. (2017). Cognitive benefits of online social networking for healthy older adults. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 72(5), 752–760. [Google Scholar] [CrossRef]
- NHS England. (2019). Social prescribing and community-based support: Summary guide. Available online: https://www.england.nhs.uk/personalisedcare/social-prescribing/ (accessed on 4 January 2025).
- Nowland, R., Robinson, S. J., Bradley, B. F., Summers, V., & Qualter, P. (2018). Loneliness, HPA stress reactivity and social threat sensitivity: Analyzing naturalistic social challenges. Scandinavian Journal of Psychology, 59(5), 540–546. [Google Scholar] [CrossRef]
- Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan—A web and mobile app for systematic reviews. Systematic Reviews, 5, 210. [Google Scholar] [CrossRef]
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. British Medical Journal, 372, n71. [Google Scholar] [CrossRef]
- Perry, G. R. (1990). Loneliness and coping among tertiary-level adult cancer patients in the home. Cancer Nursing, 13(5), 293–302. [Google Scholar] [CrossRef] [PubMed]
- *Razani, N., Morshed, S., Kohn, M. A., Wells, N. M., Thompson, D., Alqassari, M., Agodi, A., & Rutherford, G. W. (2018). Effect of park prescriptions with and without group visits to parks on stress reduction in low-income parents: SHINE randomized trial. PLoS ONE, 13(2), e0192921. [Google Scholar] [CrossRef] [PubMed]
- **Ristolainen, H., Kannasoja, S., Tiilikainen, E., Hakala, M., Närhi, K., & Rissanen, S. (2020). Effects of ‘participatory group-based care management’ on wellbeing of older people living alone: A randomized controlled trial. Archives of Gerontology and Geriatrics, 89, 104095. [Google Scholar] [CrossRef]
- Rose, G. (1985). Sick individuals and sick populations. International Journal of Epidemiology, 14(1), 32–38. [Google Scholar] [CrossRef]
- Ruisoto, P., López-Guerra, V. M., Lopez-Nunez, C., Sanchez-Puertas, R., Paladines-Costa, M. B., & Pineda-Cabrera, N. J. (2022). Transdiagnostic model of psychological factors and sex differences in depression in a large sample of Ecuador. International Journal of Clinical and Health Psychology, 22(3), 100322. [Google Scholar] [CrossRef]
- **Shapira, S., Yeshua-Katz, D., Cohn-Schwartz, E., Aharonson-Daniel, L., Sarid, O., & Clarfield, A. M. (2021). A pilot randomized controlled trial of a group intervention via Zoom to relieve loneliness and depressive symptoms among older persons during the COVID-19 outbreak. Internet Interventions, 24, 100368. [Google Scholar] [CrossRef] [PubMed]
- Steptoe, A., Shankar, A., Demakakos, P., & Wardle, J. (2013). Social isolation, loneliness, and all-cause mortality in older men and women. Proceedings of the National Academy of Sciences, 110(15), 5797–5801. [Google Scholar] [CrossRef]
- Sterne, J. A., Savović, J., Page, M. J., Elbers, R. G., Blencowe, N. S., Boutron, I., Cates, C. J., Cheng, H. Y., Corbett, M. S., Eldridge, S. M., Emberson, J. R., Hernán, M. A., Hopewell, S., Asbjørn, H., Junqueira, D. R., Jüni, P., Kirkham, J. J., Lasserson, T., Li, T., … Higgins, J. P. (2019). RoB 2: A revised tool for assessing risk of bias in randomised trials. British Medical Journal, 366. [Google Scholar] [CrossRef]
- **Tabrizi, F. M., Radfar, M., & Taei, Z. (2016). Effects of supportive-expressive discussion groups on loneliness, hope and quality of life in breast cancer survivors: A randomized control trial. Psycho-Oncology, 25(9), 1057–1063. [Google Scholar] [CrossRef]
- Tan, X. R., Wilson, I. M., Tay, P. K. C., Win, P. P. S., Song, C. F., & Wee, S. L. (2024). Mapping of technological strategies for reducing social isolation in homebound older adults: A scoping review. Archives of Gerontology and Geriatrics, 125, 105478. [Google Scholar] [CrossRef]
- Taras, V., Kirkman, B. L., & Steel, P. (2010). Examining the impact of Culture’s consequences: A three-decade, multilevel, meta-analytic review of Hofstede’s cultural value dimensions. Journal of Applied Psychology, 95(3), 405–439. [Google Scholar] [CrossRef]
- **Thimmapuram, J., Pargament, R., Bell, T., Schurk, H., & Madhusudhan, D. K. (2021). Heartfulness meditation improves loneliness and sleep in physicians and advance practice providers during COVID-19 pandemic. Hospital Practice, 49(3), 194–202. [Google Scholar] [CrossRef] [PubMed]
- Tomova, L., Wang, K. L., Thompson, T., Matthews, G. A., Takahashi, A., Tye, K. M., & Saxe, R. (2020). Acute social isolation evokes midbrain craving responses similar to hunger. Nature Neuroscience, 23(12), 1597–1605. [Google Scholar] [CrossRef] [PubMed]
- Valtorta, N. K., Kanaan, M., Gilbody, S., & Hanratty, B. (2018). Loneliness, social isolation and risk of cardiovascular disease in the English Longitudinal Study of Ageing. European Journal of Preventive Cardiology, 25(13), 1387–1396. [Google Scholar] [CrossRef]
- Vanhalst, J., Klimstra, T. A., Luyckx, K., Scholte, R. H., Engels, R. C., & Goossens, L. (2012). The interplay of loneliness and depressive symptoms across adolescence: Exploring the role of personality traits. Journal of Youth and Adolescence, 41, 776–787. [Google Scholar] [CrossRef]
- *Van Orden, K. A., Conwell, Y., Chapman, B. P., Buttaccio, A., VanBergen, A., Beckwith, E., Santee, A., Rowe, J., Palumbos, D., Williams, G., Messing, S., Sörensen, S., & Tu, X. (2022). The helping older people engage (HOPE) study: Protocol & COVID modifications for a randomized trial. Contemporary Clinical Trials Communications, 30, 101040. [Google Scholar] [CrossRef] [PubMed]
- Viechtbauer, W. (2010). Conducting Meta-Analyses in R with the metafor Package. Journal of Statistical Software, 36(3), 1–48. [Google Scholar] [CrossRef]
- Wang, J. A., Wang, H. F., Cao, B., Lei, X., & Long, C. (2024). Cultural dimensions moderate the association between loneliness and mental health during adolescence and younger adulthood: A systematic review and meta-analysis. Journal of Youth and Adolescence, 53(8), 1774–1819. [Google Scholar] [CrossRef]
- Whitmee, S., Haines, A., Beyrer, C., Boltz, F., Capon, A. G., de Souza Dias, B. F., Ezeh, A., Frumkin, H., Gong, P., Head, P., Horton, R., Mace, G. M., Marten, R., Myers, S. S., Nishtar, S., Osofsky, S. A., Pattanayak, S. K., Pongsiri, M. J., Romanelli, C., … Yach, D. (2015). Safeguarding human health in the Anthropocene epoch: The Rockefeller Foundation–Lancet Commission on planetary health. The Lancet, 386(10007), 1973–2028. [Google Scholar] [CrossRef]
- Wilkinson, J., Heal, C., Antoniou, G. A., & Kirkham, J. J. (2023, September 4–6). Introducing INSPECT-SR: A tool for detecting problematic randomised controlled trials in health systematic reviews. Workshop presented at the Cochrane Colloquium 2023, London, UK. Available online: https://abstracts.cochrane.org/2023-london/introducing-inspect-sr-tool-detecting-problematic-randomised-controlled-trials-health (accessed on 11 January 2025).
- Wilson, E. O. (1986). Biophilia. Harvard University Press. [Google Scholar]
- World Health Organization. (2016). Urban health initiative. Available online: https://www.who.int/initiatives/urban-health-initiative (accessed on 11 April 2025).
- World Health Organization. (2020). Mental health and psychological resilience during the COVID-19 pandemic. Available online: https://www.who.int/europe/news/item/27-03-2020-mental-health-and-psychological-resilience-during-the-covid-19-pandemic (accessed on 11 April 2023).
- **Xiao, T., Jiao, C., Yao, J., Yang, L., Zhang, Y., Liu, S., Grabovac, I., Yu, Q., Kong, Z., Yu, J., & Zhang, J. (2021). Effects of basketball and Baduanjin exercise interventions on problematic smartphone use and mental health among college students: A randomized controlled trial. Evidence-Based Complementary and Alternative Medicine, 2021, 8880716. [Google Scholar] [CrossRef]
- *Yang, S. Y., Yang, C. C., Lee, Y. C., Hsieh, P. L., & Lin, Y. L. (2023). Investigating the effectiveness of online interactive courses on loneliness and quality of life of older adults in the community during the COVID-19 pandemic: A pilot study and a randomized controlled trial. Geriatrics & Gerontology International, 23(2), 91–97. [Google Scholar] [CrossRef]
- **Zhang, W., Jhang, J., & Greenwell, M. R. (2023). Effects of replay and rehearsal expressive writing on mental health: A randomized controlled trial. Journal of Mental Health, 32(3), 582–591. [Google Scholar] [CrossRef] [PubMed]

| Study RoB: Overall Risk | Sample (Type of Sample) % Women Mean Age (SD) | Country (Culture) | Contrast: Main Active Component vs. CG Type | Duration: # Sessions (Length per Session | Delivery-Mode; Format; Focus (Centered) | Follow-Up (Months) | Severity-Based Inclusion Criteria |
|---|---|---|---|---|---|---|---|
| Aydın and Kutlu (2021) RoB: Some concerns | 60 (Older Adults) 78.3% 72.56 (±1.01) | Turkey (Coll) | Art therapy vs. NI | ×6 (60–90 min); length (n/r) | In person; group; person-centered | No | Yes |
| Bruehlman-Senecal et al. (2020) RoB: Some concerns | 221 (College Students) 59.3% 18.68 (0.35) | United States (Ind) | CBT vs. DA | n/r (n/r); 4 weeks | Virtual; individual; person-centered | No | Yes |
| Cohen-Mansfield et al. (2018) RoB: Some concerns | 74 (Older Adults) CBT 79.49% NI 82.86% CBT 76.6 (6.8) NI 79 (6.62) | Israel (Coll) | CBT vs. NI | ×7 individual (n/r) ×10 group (n/r); length (n/r) | In person; group; person-centered | Yes (3) | No |
| Kahlon et al. (2021) RoB: Low | 240 (Older Adults) 79% SS 69.4 (11.5) NI 68.7 (12.8) | United States (Ind) | Social Support vs. NI | ×20 (~less than 10 min; 5 per week); 4 weeks | Virtual; individual; person-centered | No | No |
| Käll and Andersson (2023) c RoB: Some concerns | 73 (Adults) 71.2% 47.2 (17.63) | Sweden (Ind) | CBT vs. DA | ×8 (n/r); 8 weeks | Virtual; individual; person-centered | Yes (24) | Yes |
| Käll et al. (2021) b RoB: Some concerns | 170 (Adults) 75.9% 47.5 (16.4) | Sweden (Ind) | CBT vs. WL IPT vs. WL | ×9 (n/r); 9 weeks | Virtual; individual; person-centered | Yes (4) | No |
| Li et al. (2022) RoB: Some concerns | 64 (Older Adults) 63.3% 65.7 (3.69) | China (Coll) | Reminiscence therapy vs. NI | ×8 (4 h); length (n/r) | In person; group; person-centered | Yes (3) | No |
| S. Liu et al. (2023) RoB: Some concerns | 252 (Adults) 73% 33.93 (11.84) | Germany (Ind) | Social support vs. NI | ×1 (~4 min); 1 day | Virtual; individual; person–context-centered | No | No |
| Mahmoudpour et al. (2021) RoB: Some concerns | 83 (Divorced Women) 100% 32 (n/r) | Iran (Coll) | ACT vs. NI | ×8 (90 min); 1 month | In person; group; person-centered | No | No |
| Morgado et al. (2023) RoB: High | 34 (Older Adults) 50% 81.97 (8.03) | Portugal (Ind) | Reminiscence therapy vs. NI | ×10 (45 min); length (n/r) | In person; group; person-centered | No | No |
| Myhre et al. (2017) a RoB: High | 121 (Older Adults) D-SS 36% OD 31% WL 21% D-SS 80 (7.34) OD 78.38 (7.32) WL 79.29 (6.76) | United States (Ind) | Digital-Social Support vs. WL | nr (n/r); 8 weeks | Virtual; individual; person-centered | No | No |
| Ristolainen et al. (2020) RoB: High | 392 (Older Adults) 82.9% 76.8 (7.5) | Finland (Ind) | Social support vs. NI | ×5 (2–3 h); 6 months | In person; group; person-centered | No | No |
| Shapira et al. (2021) RoB: Some concerns | 82 (Older Adults) CBT 81% WL 78% CBT 72.1 (5.3) WL 71.7 (6.8) | Israel (Ind) | CBT vs. WL | ×7 (60–90 min); ~4 weeks | In person; group; person-centered | No | No |
| Tabrizi et al. (2016) RoB: Some concerns | 140 (Breast Cancer survivors) 100% 47.9 (11.4) | Iran (Coll) | Social Support vs. NI | ×12 (90 min); 12 weeks | In person; group; person-centered | Yes (2) | No |
| Thimmapuram et al. (2021) RoB: High | 155 (Physicians) 66% 46 (11.03) | United States (Ind) | Meditation vs. DA. | ×~28 Sessions (15 min); 4 weeks | Virtual; individual; person-centered | No | No |
| Xiao et al. (2021) RoB: Some concerns | 96 (University Students) ~26.04% PA 18.95 (0.89) MM 19.21 (1.02) NI 19.71 (1.77) | China (Coll) | Physical Activity vs. NI Mindful Movement vs. NI | ×36 (90 min); 12 weeks | Virtual; individual; person-centered | No | No |
| Hussain et al. (2023) RoB: Some concerns | 110 (College students) 79% 20.97(4.83) | United Kingdom (Ind) | Mindfulness vs. Happier Life Intervention | nr (n/r); 4 weeks | Virtual; individual; person-centered | Yes (0.5) | No |
| Lanser and Eisenberger (2023) ** RoB: Some concerns | 300 (Undergraduate students) 79.7% 20.08 (n/r) | United States (Ind) | Prosocial behavior-Giving vs. Logo viewing Prosocial behaviour-Keeping vs. Logo viewing | ×1 (task done only once); length (n/r) | Virtual; individual; person-centered | No | No |
| Lanser and Eisenberger (2023) ** RoB: Some concerns | 300 (Undergraduate students) 77.1% 20.50 (n/r) | United States (Ind) | Prosocial behavior-Gratitude vs. TV-show writing Prosocial behaviour-Reflection vs. TV-show writing | ×1 (task done only once); length (n/r) | Virtual; individual; person-centered | No | No |
| Lindsay et al. (2019) RoB: Some concerns | 153 (Young Adults) 67.32% 32.42 (13.68) | United States (Ind) | Mindfulness vs. Coping control | ×14 sessions (20 min); 2 weeks | Virtual; individual; person-centered | No | No |
| C. W. Liu et al. (2023) RoB: Some concerns | 100 (Older Adults) D-SS 74% YT-i 70% D-SS 72.90 (4.45) YT-i 72.78 (±4.52) | Taiwan (Coll) | Digital-Social Support vs. YouTube Interaction | ×60 (1 h); 12-weeks | Virtual; group; person-centered | No | No |
| Razani et al. (2018) RoB: Some concerns | 78 (Child-parent pairs) 87% 38 (n/r) | United States (Ind) | Nature exposure vs. Independent Park prescription | ×3 (n/r); 3 weeks | In person; individual; context-centered | No | No |
| Van Orden et al. (2022) RoB: Low | 291 (Older Adults) 75.3% 72 (9.07) | United States (Ind) | Volunteering vs. Life Review | n/r (n/r); 12 months | In person; individual; person-centered | No | No |
| Yang et al. (2023) RoB: Some concerns | 90 (Older Adults) 64.04% VI 68.07 (6.68) N-On 69.00 (6.04) | Taiwan (Coll) | Virtual interaction with strangers vs. Non-online interaction group | ×40 (n/r); 8 weeks | Virtual; individual; person-centered | No | No |
| Zhang et al. (2023) RoB: Some concerns | 132 (University Students) 62.9% 24.4 (10.1) | United States (Ind) | Art therapy vs. Hobbies-writing | ×4 (15 min); 4 days | Virtual; individual; person-centered | No | No |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the University Association of Education and Psychology. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zeas-Sigüenza, A.; Voldstad, A.; Ruisoto, P.; Ganho-Ávila, A.; Guiomar, R.; Cacho, R.; Muntané, F.; Benach, J. Loneliness as a Public Health Challenge: A Systematic Review and Meta-Analysis to Inform Policy and Practice. Eur. J. Investig. Health Psychol. Educ. 2025, 15, 131. https://doi.org/10.3390/ejihpe15070131
Zeas-Sigüenza A, Voldstad A, Ruisoto P, Ganho-Ávila A, Guiomar R, Cacho R, Muntané F, Benach J. Loneliness as a Public Health Challenge: A Systematic Review and Meta-Analysis to Inform Policy and Practice. European Journal of Investigation in Health, Psychology and Education. 2025; 15(7):131. https://doi.org/10.3390/ejihpe15070131
Chicago/Turabian StyleZeas-Sigüenza, Ananda, Andreas Voldstad, Pablo Ruisoto, Ana Ganho-Ávila, Raquel Guiomar, Raúl Cacho, Ferran Muntané, and Joan Benach. 2025. "Loneliness as a Public Health Challenge: A Systematic Review and Meta-Analysis to Inform Policy and Practice" European Journal of Investigation in Health, Psychology and Education 15, no. 7: 131. https://doi.org/10.3390/ejihpe15070131
APA StyleZeas-Sigüenza, A., Voldstad, A., Ruisoto, P., Ganho-Ávila, A., Guiomar, R., Cacho, R., Muntané, F., & Benach, J. (2025). Loneliness as a Public Health Challenge: A Systematic Review and Meta-Analysis to Inform Policy and Practice. European Journal of Investigation in Health, Psychology and Education, 15(7), 131. https://doi.org/10.3390/ejihpe15070131







