Effectiveness of Therapeutic Interventions in the Treatment of Internet Gaming Disorder: A Systematic Review
Abstract
1. Introduction
Aim and Research Question
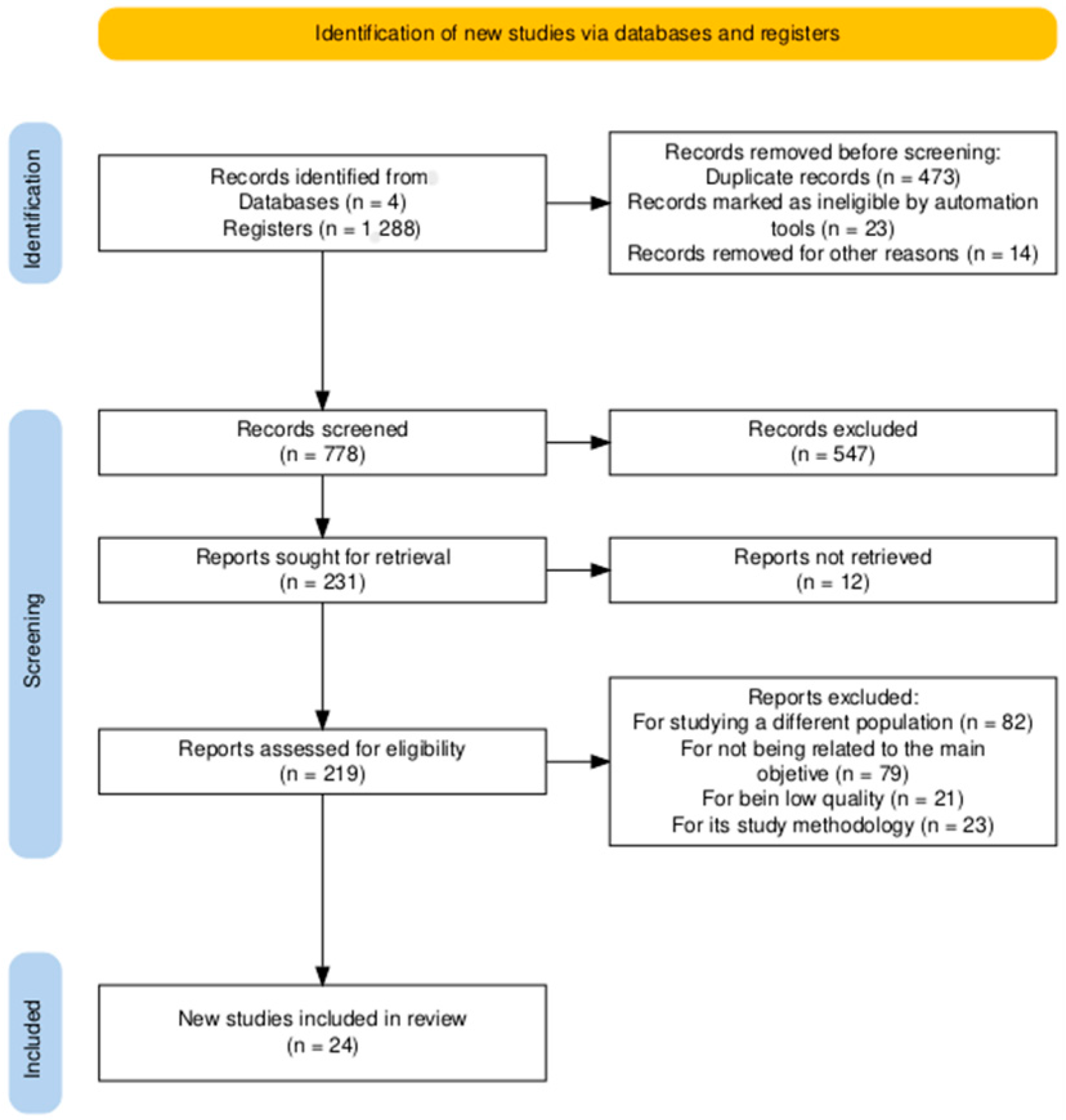
2. Materials and Methods
3. Results
3.1. Description of the Characteristics of the Studies
Differentiation Between Clinical and Subclinical Samples
3.2. Description of the Results
3.2.1. Internet Gambling Disorder
3.2.2. Treatment Effectiveness in Reducing Anxious and Depressive Symptoms
3.2.3. Effectiveness of Treatment in Improving Interpersonal Relationships and Family Functioning
3.2.4. Changes in Brain Connectivity and Neurophysiology
3.2.5. Differential Outcomes Based in Follow-Up
4. Discussion
Limitations and Future Research Directions
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Characteristics of the Studies Included in the Systematic Review
| Study/Author | Typology/Main Objective | Participants | Variables/Instruments | Main Findings | JBI |
| (Shin et al., 2021) | Design: Non-randomized experimental Objective: To examine the potential use of a virtual reality application in managing conflict related to games with young adults with TGI and matched controls. | N = 50 Sex: Male Average age: 21.78 (SD 2.33) | Intelligence Quotient (IQ): Wechsler Adult Intelligence Scale (revised) Internet gaming behavior: Frequency measured in hours of gameplay per week Gaming cravings, intensity of anger, coping skills: VAS Motivation to Change: Modified readiness to change questionnaire Virtual Reality System Experience: PQ and SSQ Tasks Behavioral Reactions: Initial expression of anger and choice to stop or continue playing Data recorded by the VR system: Response time, head movement, hand gestures, speech content, and conversation duration | There were no significant differences between the IGD and control groups in terms of age (p = 0.83), education (p = 0.11), or IQ (p = 0.36). The IGD group showed higher gaming cravings (p < 0.001), greater severity of the disorder (N/A), and more hours of gameplay per week (p < 0.001) compared to the control group. In the Presence Questionnaire (PQ), participants with IGD showed significantly lower scores than the controls (p < 0.001). The IGD group experienced higher levels of anger compared to the control group (p = 0.006). Furthermore, anger was higher when the stimulus was the virtual father compared to the virtual mother (p = 0.04) and increased in the second expression of anger compared to the first (p = 0.03). Participants in the control group perceived significantly more benefits than risks when stopping the game (p = 0.003). In the IGD group, a greater perception of benefits was associated with higher motivation to change their gaming behavior (r = 0.488, p = 0.01). The evaluation of benefits had a stronger effect than the evaluation of risks (p < 0.001), and the control group showed greater sensitivity to benefits than to risks compared to the IGD group (p < 0.001). The IGD group showed a higher tendency to continue playing compared to the control group (p < 0.001). However, both groups showed a greater willingness to stop playing after the risk–benefit evaluation compared to the start (p = 0.003) and after the expression of anger (p = 0.02). The control group showed a better understanding of the perspective of the virtual parents than the IGD group (p < 0.001), and the perspective of the virtual mother was better understood than that of the virtual father (p = 0.04). The control group perceived the coping strategy as more helpful in resolving conflicts compared to the IGD group (p = 0.004), but there were no significant differences in the perceived usefulness of anger expression (p = 0.71). In the control group, more hours of gameplay were associated with a greater perception of the usefulness of coping strategies over anger expression (r = 0.556, p = 0.003). In contrast, in the IGD group, fewer hours of gameplay were associated with a greater perception of coping strategies over anger expression (r = −0.468, p = 0.02). | 8/9 |
| (Ni et al., 2024) | Study type: Randomized clinical trial Objective: Explore the efficacy of mindfulness used to treat adults with IGD and identify the neural mechanisms underlying mindfulness. | N = 80 Sex: 33 women, 31 men Age: >18 years | Addiction: DSM-5-TR and Internet Addiction Test (IAT) Craving: Gaming Urge Questionnaire (Adaptation of Tiffany’s Questionnaire) Brain Responses: BOLD Signals Functional Brain Connectivity: CONN Toolbox, Version 22a, Regions of Interest (ROI) | The final analysis included a total of 64 adults with IGD, with 32 participants assigned to the Mindfulness (MM) group and 32 to the Progressive Muscle Relaxation (PMR) group. After the intervention, IGD severity decreased from 7 to 3.6 points in the MM group (p < 0.001) and from 7.1 to 6.0 points in the PMR group (p = 0.04). The IAT score significantly decreased in the MM group from 70.1 to 43.0 points (p < 0.001), whereas no significant changes were observed in the PMR group (69.3 to 69.2, p = 0.11). Gaming craving significantly decreased in the MM group from 58.8 to 33.6 points (p < 0.001), while no significant reduction was found in the PMR group. Neuroimaging results showed that the MM group exhibited a significant reduction in activity within the bilateral lentiform nuclei (associated with reward processing and habit formation) (p = 0.02), the left medial frontal gyrus (MFG) (involved in cognitive control and emotional regulation) (p = 0.01), the right insula (linked to emotion perception and self-awareness) (p = 0.047), and the right sublobar region (related to sensory and emotional integration). Additionally, the MM group showed a significant increase in connectivity between the left medial frontal gyrus and the left lentiform nucleus (p = 0.03). | 10/13 |
| (Hong et al., 2020) | Design: Randomized trial Objective: To evaluate the effect and neurophysiological mechanisms of a physical exercise + cognitive behavioral therapy (CBT) intervention in individuals with IGD. | N = 54 Age: 13–18 years Sex: Male Intervention Groups:
| Internet Addiction: YIAS (Young Internet Addiction Scale) Depression: BDI (Beck Depression Inventory) Anxiety: BAI (Beck Anxiety Inventory) Hyperactivity/ADHD: K-ARS Frontal Brain Activity: EEG Physical Exercise: Heart Rate | Both interventions started under similar conditions. The TCC+EF group showed a significant reduction in BDI (p = 0.001), BAI (p < 0.05), K-ARS (p < 0.05), and YIAS (p < 0.001) scores. The TCC-only group achieved a significant reduction in BDI (p < 0.05) and YIAS (p = 0.001) scores. Improvements in BDI and YIAS scores were significantly greater in the TCC+EF group compared to the TCC-only group. Both interventions were effective, but the TCC+EF group demonstrated a greater impact. In the TCC+EF group, a significant increase in frontal alpha asymmetry (FAA) values at F4-F3 (p < 0.001) was observed, along with a trend-level increase in FAA at F8-F7 (p = 0.05). However, no significant changes were found in these values for the TCC-only group. | 10/13 |
| (Park et al., 2016) | Design: Randomized clinical trial Objective: Investigate the therapeutic efficacy of virtual reality therapy (VRT) for gaming addiction. | N: 36 Sex: Male Age: >18 Group Distribution: 12 CBT, 12 VRT, 12 occasional users | Game Addiction: YIAS Depression: BDI Anxiety: BAI ADHD: ASRS-K Brain Activity (fMRI): Philips Achieva 3.0 T. Scanner, DPARSFA, and SPM8 | After the treatment, both groups (CBT p = 0.05 and VRT p < 0.01) showed a significant reduction in YIAS scores. No significant differences were found in YIAS score changes between the CBT and VRT groups (p = 0.52). Following the intervention, the VRT group showed a significant increase in connectivity from the PCC seed to the right parietal precuneus, right superior temporal gyrus, left middle frontal gyrus, and left temporal fusiform gyrus. This change may suggest improved brain integration and greater activation in areas related to attention, memory, and emotional control. In the CBT group, significant increased connectivity was observed from the PCC to the right cerebellum, bilateral thalamus, and left occipital lingual gyrus. These changes may be associated with improved cognitive skills and emotional regulation, which are key processes in cognitive behavioral therapy. | 11/13 |
| (Maden et al., 2022) | Design: Randomized controlled trial Objective: To compare the effects of virtual reality training (VRT) and aerobic training (AT) programs on gaming disorder severity, physical activity, physical fitness, and anxiety, compared to a control group. | N = 45 Sex: Male Age: 18–28 years | Gaming Addiction: IGDS9-SF Physical Activity/Sedentary Level: IPAQ Functional Capacity: 6-MWT Physical Fitness (Strength and Flexibility): CST, ACT, CSRT, BST Maximal Oxygen Consumption: 20-meter shuttle run test Anxiety: BAI Perceived exertion during exercise: RPE | There were no demographic differences between groups except for age: the VRT group was older than both the AT and control groups (p = 0.040). Both the VRT and AT groups significantly reduced gaming time (p = 0.04 and p = 0.039, respectively) and sedentary time (p = 0.000 and p = 0.025) compared to the control group. Both intervention groups showed a significant increase in weekly physical activity levels (p = 0.032 for VRT and p = 0.042 for AT) compared to the control group. There was a significant reduction in IGDS9-SF scores in the VRT and AT groups compared to the control group (p = 0.041 and p = 0.045, respectively). Both groups improved their physical fitness, with significant differences in the following:
In the physical fitness analysis (Senior Fitness Test parameters and VO2 max), CSRT significantly influenced BST within the control group (p = 0.004). However, no other significant interactions were observed in the MANOVA analysis. Both intervention programs (VRT and AT) proved effective in reducing gaming disorder severity, sedentary time, and anxiety levels while improving physical activity levels, physical fitness (6-MWT, ACT, VO2 max), and flexibility. However, the VRT group showed greater effects on limb flexibility. These findings suggest that physical activity-based interventions can be a valuable tool in the treatment of gaming disorder. | |
| (Zheng et al., 2022) | Design: Randomized controlled trial Objective: To investigate whether there were different effects of a single intervention targeting either impulsive action or reward sensitivity compared to a combined intervention in individuals with Internet Gaming Disorder. | N = 80 Age: ≈14.75 years Sex: Male | Online Gaming Addiction: OGAS Impulsivity: Barratt-11 Depression, Anxiety, and Stress: DASS-21 Gaming Craving: Gaming Cue Exposure Craving Questionnaire (developed by researchers) Behavioral Impulsivity: Stop-Signal Task (STT) Reward Sensitivity: Stimulus-Response Compatibility Task (SRC) Behavioral Training: Go/No-go Task and SRC Task | No significant differences were found between the groups in demographic characteristics or baseline-related indices (p > 0.05). The response inhibition (RI) training group and the combined training group showed significant reductions in reaction times (SSRT) in the post-test (p < 0.001), while the ApBM and control groups showed no significant changes. The ApBM group and the combined training group exhibited significant reductions in SRC scores in the post-test (p < 0.001), whereas the RI and control groups showed no significant changes. The combined training group demonstrated significant reductions in IGD scores in both the post-test and follow-up assessments (p < 0.01 and p < 0.001, respectively). The RI and ApBM groups showed marginally significant reductions at certain points (p = 0.065 and p = 0.054, respectively). The control group showed no significant differences between measurements. The combined training group showed significant reductions in depression scores in both the post-test and follow-up (p < 0.001), whereas the RI and ApBM groups had less consistent results. The control group showed no significant changes. There was a significant reduction in general anxiety across assessments (p < 0.001), but no significant interaction between groups and measurements. Regarding stress and craving, no significant effects were found (p > 0.05). Changes in impulsivity (SSRT) and stimulus–response compatibility (SRC) scores explained 12.4% of the variations in IGD scores (adjusted R2 = 0.124, p < 0.01). Both SSRT and SRC were significant predictors of IGD scores (p < 0.05). | 9/13 |
| (Kochuchakkalackal Kuriala & Reyes, 2023) | Design: Randomized controlled trial (RCT) Objective: To evaluate the effectiveness of a psychological intervention program (ACRIP) aimed at adolescents with Internet Gaming Disorder (IGD). | N = 30 Age: 16–19 years Sex: Male and female | Internet Gaming Disorder: IGDS9-SF Psychological Well-being: Ryff’s PWB | A significant reduction in IGD symptoms was observed after the intervention (t = 15.98, p = 0.001). A significant improvement in psychological well-being was also noted (t = −42.56, p = 0.001). The ACRIP intervention had a significant effect on both outcomes: reduction in IGD (F = 493.42) and improvement in psychological well-being (PWB) (F = 2210.54), with an effect size of 0.90. No significant differences were found between pre-test and post-test scores for IGD or PWB in the control group. | 10/13 |
| (André et al., 2023) | Design: Unblinded randomized controlled trial Objective: To determine the efficacy of cognitive behavioral therapy (CBT) as a treatment for individual conduct disorder and problematic gaming (IGD) in adolescents. | N = 102 Age: 13–18 years Sex: Male and female | Internet Gaming Disorder: GASA (Game Addiction Screening Assessment) Psychological Well-being: PWB | Both the control and treatment groups showed a reduction in GASA scores over time, but the improvement was significantly greater in the treatment group. In the treatment group, the mean score decreased by 9.9 points (p < 0.001), while in the control group, the reduction was 5.1 points (p < 0.001). Demographic variables (age, gender, living situation) and common diagnoses did not have a significant impact on the improvement. The proportion of problematic and addicted gamers significantly decreased in the treatment group at follow-up compared to baseline. However, there were no significant differences in the prevalence of player categories in the control group between baseline and follow-up. | |
| (Torres-Rodríguez et al., 2018) | Study Design: Non-randomized experimental study Objective: To evaluate the effectiveness of a specialized psychotherapy program for adolescents with Internet Gaming Disorder (IGD), specifically the Individualized Psychotherapeutic Program for Addiction to Information and Communication Technologies (PIPATIC). | N = 31 Age: 12–18 years Sex: Male | Internet Gaming Disorder: IGD-20 Test Comorbid Disorders: YSR/11-18 and CBCL/6-18 Intrapersonal Concerns: MACI Emotional Intelligence: TMMS-24 (Trait Meta-Mood Scale) Interpersonal Skills: Social Skills Scale (EHS) Family Relationships: Family Discord G Clinical Severity: CGI-SI and CGI-GI General Functioning: GAF (Global Assessment of Functioning) | Before the treatment, no significant differences were observed between the experimental group (EG) and the control group (CG), with a p-value of 0.384. The EG showed a significant reduction in weekly gaming time (11.15 hours), whereas the CG did not experience a significant change (31.80 hours), with p = 0.0001. The EG significantly reduced delay to 1.81, while the CG maintained a higher value (3.27), with a significant difference (p = 0.0001). The EG experienced a significant reduction in subjective addiction (3.13) compared to the CG (6.47), with p = 0.0001. The EG showed a significant improvement in addiction reduction (32.19) compared to the CG (51.93), with p = 0.001. The EG demonstrated a significant improvement in attention problems (53.25) compared to the CG (64.33), with p = 0.003. The EG significantly improved in reducing aggressive behavior problems (52.69), whereas the CG remained higher (59.80), with p = 0.005. The EG showed a significant improvement in engagement in activities (39.56) compared to the CG (29.64), with p = 0.001. The EG significantly improved in self-devaluation (42.40), while the CG showed no major changes (57.00), with p = 0.044. The EG exhibited a significant improvement in mood repair (28.80), whereas the CG remained nearly unchanged (23.20), with p = 0.045. The EG showed a significant improvement in CGI (18.5) compared to the CG (10), with p = 0.001. The EG significantly improved in the global functioning assessment (10), while the CG had a lower score (7), with p = 0.001. The PIPATIC program demonstrated superiority in the development of a therapeutic alliance compared to cognitive behavioral therapy and in the outcomes of therapeutic change, with p < 0.0001 across all compared subscales. | 9/9 |
| (L. Wu et al., 2021). | Design: Randomized controlled trial Objective: Investigate the effects of transcranial direct current stimulation (tDCS) on gaming cravings in individuals with Internet Gaming Disorder (IGD). | N = 33 Sex: Male Age: 18–25 years | Internet Gaming Disorder: IAT Craving for Gaming: Cue reactivity task + 9-point scale (1 = “no craving at all,” 9 = “high craving”) Inhibitory control over distractors: Letter categorization area Adverse effects of tDCS: Likert scale for perceived intensity of side effects Perceived differences between active and sham tDCS sessions: Open-ended response | In the active condition, baseline craving significantly decreased after stimulation (from 6.21 to 4.24; p < 0.001). In the sham condition, no significant changes were observed in baseline craving (5.94 vs. 5.85; p > 0.1). No significant differences were found in cue-induced craving ratings between the active and sham conditions. No clinically significant adverse effects were reported. Participants were unable to reliably distinguish between the active and sham conditions (only 21% attempted, result not different from chance). Active tDCS significantly improved inhibitory control over addiction-related distractors (p = 0.004). | 11/13 |
| (Nielsen et al., 2021) | Design: Randomized controlled trial Objective: To evaluate the impact of two family therapies—Multidimensional Family Therapy (MDFT) and Traditional Family Therapy (TFT)—on the prevalence and symptoms of Internet Gaming Disorder (IGD). | N = 42 Age = 12–19 years Sex = Male and female (97.6% male) | Internet Gaming Disorder (IGD): Petry IGD Criteria (DSM-5) Gaming Frequency: Timeline Followback Method (TLFB) Quality of Life: Addiction Severity Index (ASC T-ASI) Treatment Satisfaction: Satisfaction Questionnaires | At the 6-month follow-up, the completion rate was 100% in the MDFT group and 86.7% in the FTAU group. At 12 months, 91.7% of adolescents in the MDFT group and 70.0% in the FTAU group completed the follow-up. Regarding the reduction in IGD symptoms, at 6 months, the number of IGD criteria significantly decreased in the MDFT group (83.3%) compared to the FTAU group (60.3%) (p < 0.01). At 12 months, the reduction remained greater in the MDFT group (87.9% vs. 63.3%) (p < 0.01). At the 6-month follow-up, no adolescents in the MDFT group met IGD criteria, whereas 11.5% of those in the FTAU group still did. At 12 months, IGD was present in 19.0% of the MDFT group compared to 63.3% in the FTAU group (p < 0.01). Although IGD criteria significantly decreased in both groups, the reduction was more pronounced in the MDFT group. For instance, “continued gaming despite problems” showed a significantly greater improvement in MDFT compared to FTAU (p < 0.01). Gaming time decreased in both groups at 6 months (MDFT: 2.6 hours, FTAU: 3.1 hours); however, at 12 months, gaming time rebounded in both groups, with no significant difference between them (p > 0.05). Regarding quality of life, both groups showed significant improvements, but the MDFT group demonstrated a greater reduction in gaming-related problems compared to FTAU (MDFT: −60.9% vs. FTAU: −41.2%) (p < 0.05). At 12 months, parents of adolescents in the MDFT group reported a more significant reduction in gaming-related problems (MDFT: −46.8% vs. FTAU: −36.2%) (p < 0.05). The MDFT group had a 100% treatment completion rate, while the FTAU group had a significantly lower compliance rate (70%) (p < 0.05). The MDFT group attended more treatment sessions (26.33 vs. 17.50 in FTAU), with significantly longer session durations (MDFT: 85.8 min vs. 65.4 min in FTAU) (p < 0.01). The number of family therapy sessions was the only factor significantly correlated with a reduction in IGD symptoms at 12 months (p < 0.01). | 11/13 |
| (Igarashi et al., 2024) | Design: Non-randomized experimental study Objective: To examine the efficacy of a brief mindfulness-based virtual reality intervention on IGD symptomatology. | N = 27 Sex: Men and women Mean age: 20.33 ± 1.12 | Internet Gaming Disorder: IGDT-10 and IAT Perceived Stress: PSS-10 Positive and Negative Affect: PANAS-SF | For the IGD group, gaming time had a significant effect on IGD symptoms (p = 0.029), indicating that the intervention had a positive impact on IGD symptoms. No significant effect of time on IGD symptoms was found in the control groups (p = 0.168). The IGD group showed a significant improvement in IGD symptoms after the 4-week mindfulness-based virtual reality intervention (p = 0.014). A significant decrease in weekend gaming time was observed in the IGD group (p = 0.034), but no significant change was found in weekday gaming time (p = 0.334). After treatment, correlations in the IGD group showed no significant relationships between IGD symptoms and other variables such as perceived stress (PSS), positive affect (PANAS-P), negative affect (PANAS-N), internet addiction (IAT), or gaming time during the week and weekend. | 8/9 |
| (Marcelle et al., 2019) | Design: Non-randomized experimental study Objective: To develop and evaluate a multimodal therapy model for Internet Gaming Disorder that includes all relevant psychological factors associated with the disorder. | N = 33 Age: 18–30 years Sex: Men and women | Internet Gaming Disorder: IGD-20 and IAT Quality of Life: WHOQOL-BREF (World Health Organization Quality of Life—Brief Version) Personality: MINI-IPIP (MINI International Personality Item Pool) | A significant difference was found in pre- and post-intervention scores, with a reduction of 10.09 points (p < 0.05) in internet addiction. A significant improvement was observed, with a decrease of 9.09 points (p < 0.05) in Internet Gaming Disorder. Quality of life dimensions, including the physical domain (p < 0.001), psychological domain (p = 0.001), and social relationships domain (p < 0.001), showed significant improvements after the intervention. However, the environmental domain did not show a statistically significant improvement (p = 0.379). | 8/9 |
| (Zhang et al., 2016) | Design: Non-randomized experimental study Objective: To examine the effects of a Craving Behavioral Intervention (CBI), developed to reduce gaming-related craving. | N = 59 Sex: Men | Internet Gaming Disorder: CIAS (Chen Internet Addiction Scale) Depression: BDI (Beck Depression Inventory) Anxiety: BAI (Beck Anxiety Inventory) Nicotine Dependence: Fagerstrom Test Hazardous Alcohol Consumption: Alcohol Use Disorders Identification Test (AUDIT) Gaming Craving: Cue-reactivity Task (fMRI) Brain Activation: fMRI (functional magnetic resonance imaging) Brain Connectivity: Functional Connectivity Analysis (PPI—Psychophysiological Interaction) | The CBI+ group showed a significant decrease in CIAS scores (t(22) = 9.49, p < 0.001), whereas the CBI− group exhibited a smaller reduction (t(16) = 3.16, p < 0.001). There was a significant interaction between session and group in weekly gaming duration (p = 0.04). The CBI+ group significantly reduced weekly gaming hours (p < 0.001), whereas the CBI− group showed a smaller reduction (p = 0.007). The CBI+ group experienced a significant reduction in gaming-related anxiety (p < 0.001), while the CBI− group also improved, but to a lesser extent (p = 0.008). Individuals with IGD showed greater activation in the dorsal striatum (caudate), brainstem, substantia nigra, anterior cingulate cortex, and posterior cingulate cortex (p < 0.05), along with reduced activation in the right insula (p < 0.05). A significant positive association was found in the middle temporal gyrus (MTG) between brain activation and gaming craving (p = 0.035). A significant interaction was observed between group (CBI+ and CBI−) and session in right anterior insula activation (p = 0.04 for CBI+, p = 0.008 for CBI−). The CBI+ group exhibited significant connectivity between the right insula and the left lingual gyrus and right precuneus (p = 0.001, p = 0.006), while the CBI− group showed the opposite pattern in connectivity (p = 0.005; p = 0.01). | 8/9 |
| (Zhao et al., 2022) | Design: Randomized trial Objective: To investigate the effects of different recovery-extinction training (RET) intervals on cue-induced craving, neural activity, and behavioral responses in young individuals with Internet Gaming Disorder. | N = 60 Age: 18–23 years; M = 20.56 ± 1.63 Sex: 2 females/22 males | Anxiety: BAI (Beck Anxiety Inventory) Depression: BDI (Beck Depression Inventory) Intelligence: Raven’s Progressive Matrices Personality: TPQ (Tridimensional Personality Questionnaire) Craving for gaming: EAV (gaming desire before and after exposure to a video) Neural activity related to rewards or punishments: MIDT (Monetary Incentive Delay Task) Memory: MST (Modified Sternberg Task) Neural Activity: EEG (Electroencephalography) Physiological Responses: ECG (Electrocardiogram), SCR (Skin Conductance Response) | A significant reduction in gaming craving was observed in the R-10min-E group three months after the intervention compared to the R-6h-E group (p = 0.042). The R-10min-E group showed a significantly faster reaction time compared to the R-6h-E group after training (p = 0.028). The R-10min-E group exhibited a significant increase (p = 0.039) in P3 amplitude evoked by gain cues in the MIDT, whereas the R-6h-E group showed no changes. A significant improvement in functional connectivity was observed in the R-10min-E group compared to the R-6h-E group with gain cues in the MIDT (p < 0.05). No significant training effects were found on working memory, as measured by differences in reaction times (RT) and P3 amplitudes evoked by intrusion cues or new cues (p = 0.476). | 12/13 |
| (Pornnoppadol et al., 2020) | Design: Non-randomized experimental study Objective: To evaluate and compare the effectiveness of four psychosocial interventions for Internet Gaming Disorder (IGD) in adolescents aged 13 to 17 years. | N = 104 Sex: 82 males, 22 females Age: 13–17 years | Internet Gaming Disorder (IGD): GAST (Game Addiction Screening Test) Quality of Life: GAME-Q (Game Addiction Quality of Life Scale) Protective Factors: GAME-P (Game Addiction Protection Scale) Emotional and Behavioral Symptoms: PSC-17 (Pediatric Symptom Checklist-17) | The severity of Internet Gaming Disorder (IGD) significantly decreased in all intervention groups compared to the control group (p ≤ 0.001, 0.002, and 0.005 at 1, 3, and 6 months, respectively). Adolescents who participated in the Siriraj Therapeutic Residential Camp (S-TRC) and the combination of S-TRC and Parent Management Training for Game Addiction (PMT-G) showed a more sustained reduction in online gaming addiction compared to those who received only PMT-G or psychoeducation (p ≤ 0.001). Quality of life significantly improved in the intervention groups compared to the control group (p ≤ 0.003 at 3 months and p ≤ 0.033 at 6 months). Protective factors against addiction significantly increased 3 months post-intervention in the S-TRC and PMT-G groups (p ≤ 0.043), although the difference was no longer significant at 6 months (p = 0.486). Emotional and behavioral symptoms significantly decreased in the S-TRC and S-TRC + PMT-G groups compared to the other groups (p ≤ 0.001 at 3 months). In the control group, most adolescents remained classified as “addicted” or “probably addicted” at 6 months post-intervention, whereas in the S-TRC and PMT-G groups, the percentage of adolescents in these categories was below 50%. | 9/9 |
| (Zhang et al., 2018) | Design: Non-randomized experimental study Objective: To investigate how Craving Behavioral Intervention (CBI) affects the functional connectivity of the ventral striatum (VS) circuit in individuals with Internet Gaming Disorder. | N = 115 Sex: Men Age: 18–30 years | Internet Gaming Disorder: CIAS (Chinese Internet Addiction Scale) Anxiety: BAI (Beck Anxiety Inventory) Depression: BDI (Beck Depression Inventory) Impulsivity: BIS-11 (Barratt Impulsiveness Scale—Version 11) Craving for Gaming: QSU-Brief (Adapted version of the Questionnaire of Smoking Urges) Brain Activity: fMRI (Functional Magnetic Resonance Imaging) | Individuals with Internet Gaming Disorder (IGD) exhibited significantly higher resting-state functional connectivity between the ventral striatum (VS) and the left inferior parietal lobule (lIPL), left middle frontal gyrus (lMFG), and right inferior frontal gyrus (rIFG) compared to the healthy control group (p < 0.01). Connectivity between the vs. and lIPL showed a significant positive correlation with IGD severity (CIAS) (r = 0.31, p = 0.01) and impulsivity levels (BIS-11) (r = 0.26, p = 0.03). Participants who received Craving Behavioral Intervention (CBI+) showed a significant reduction in IGD severity, as measured by the CIAS (F(1,34) = 26.60, p < 0.001, η2 = 0.43), as well as a decrease in time spent on online gaming (F(1,34) = 7.07, p = 0.012, η2 = 0.17). Functional connectivity between the vs. and lIPL significantly decreased following the intervention in the CBI+ group (F(1,34) = 13.89, p = 0.001, η2 = 0.29), whereas no changes were observed in the non-intervention group (CBI−). | 8/9 |
| (Kang et al., 2018) | Design: Non-randomized experimental study Objective: To investigate the effect of equine-assisted activities and therapies (EAAT) on the affective network of adolescents with Internet Gaming Disorder (IGD). | N = 30 Sex: Male Mean Age: 15.6 years | Internet Gaming Disorder: YIAS (Young Internet Addiction Scale) Attachment: K-ECRS (Korean Experiences in Close Relationships Scales—Revised) Depression: CDI (Children’s Depression Inventory) ADHD Symptoms: K-ARS (Korean ADHD Rating Scale) Functional Connectivity in the Affective Network: Resting-State fMRI (rs-fMRI) | After 7 days of EAAT, adolescents with IGD showed a significant improvement in avoidant attachment, with a reduction in K-ECRS scores (p < 0.01) compared to the control group. Video game addiction symptoms significantly decreased in the IGD group (p < 0.01), while no relevant changes were observed in the control group. Depressive symptoms improved in the IGD group following EAAT intervention (p < 0.01). Functional MRI analysis revealed an increase in functional connectivity within the affective network, specifically from the left amygdala to the medial frontal gyrus (BA 25), which correlated with improvements in avoidant attachment (r = −0.56, p = 0.001). In the IGD group, functional connectivity between the left amygdala and the left orbitofrontal gyrus (BA 11) significantly increased after EAAT (p < 0.001), suggesting a potential improvement in emotional regulation. | 9/9 |
| (J. Han et al., 2020) | Design: Non-randomized experimental study Objective: To evaluate the efficacy of cognitive behavioral therapy (CBT) in the treatment of Internet Gaming Disorder (IGD). | N = 205 Sex: Male Age: 25.9 years | Internet Gaming Disorder: YIAS (Young Internet Addiction Scale) ADHD Symptoms: K-ADHD (Korean ADHD Rating Scale) Depression: BDI (Beck Depression Inventory) Anxiety: BAI (Beck Anxiety Inventory) Impulsivity: BIS/BAS (Behavioral Inhibition System/Behavioral Activation System Scale) Social Avoidance: SADS (Social Avoidance and Distress Scale) Family Cohesion: FES (Family Environment Scale) Clinical Improvement: CGI-I (Clinical Global Impressions—Improvement Scale) | Cognitive behavioral therapy (CBT) was more effective than supportive therapy in improving symptoms of Internet Gaming Disorder (IGD), with a 66.3% improvement in the CBT group vs. 49.0% in the supportive therapy group (χ2 = 6.25, p = 0.02). In the CBT group, patients showed significant reductions in IGD severity (YIAS: F = 11.76, p = 0.001), anxiety (BAI: F = 9.06, p = 0.003), impulsivity (BIS/BAS: F = 8.84, p = 0.003), and social avoidance (SADS: F = 9.90, p = 0.002) compared to the supportive therapy group. Among patients who improved in the CBT group, significant reductions were observed in IGD severity (YIAS: F = 52.48, p < 0.001), ADHD symptoms (F = 16.85, p < 0.001), depression (BDI: F = 25.11, p < 0.001), anxiety (BAI: F = 9.41, p = 0.003), impulsivity (BIS/BAS: F = 7.48, p = 0.004), social avoidance (SADS: F = 35.19, p < 0.001), and family cohesion (FES: F = 9.71, p = 0.002). In the supportive therapy group, significant improvements were only observed in IGD severity (YIAS: F = 61.05, p < 0.001), ADHD symptoms (F = 28.55, p < 0.001), depression (BDI: F = 23.83, p < 0.001), and impulsivity (BIS/BAS: F = 10.02, p = 0.002), but not in anxiety (p = 0.793), social avoidance (p = 0.961), or family cohesion (p = 0.491). Predictors of better response to CBT included lower ADHD scores (p < 0.01), lower depression levels (p < 0.05), and not using medication (p < 0.01). | 9/9 |
| (Li et al., 2018) | Design: Non-randomized experimental study Objective: To investigate the therapeutic effectiveness of the Mindfulness-Oriented Recovery Enhancement (MORE) intervention in reducing Internet Gaming Disorder (IGD). | N = 30 Sex: Male (80%), Female (16.7%), Non-binary (3.3%) Mean Age: 25 years | Internet Gaming Disorder: DSM-5 Criteria Craving: VAS (Visual Analog Scale) Dysfunctional Beliefs About Gaming: Negative Thoughts and Feelings Subscale of the Online Cognition Scale Positive Reappraisal: Cognitive Emotion Regulation Questionnaire (CERQ) | The treatment with MORE significantly reduced dysfunctional cognitions about video games compared to the control group (SG) (p = 0.003). Post-treatment dysfunctional cognitions significantly predicted IGD severity at the 3-month follow-up (p < 0.001). MORE had a significant indirect effect on reducing IGD criteria through the reduction in dysfunctional cognitions (b = −0.27, 95% CI [−0.53, −0.06]). Craving for video games significantly decreased after the MORE treatment (p = 0.001), mediated by the reduction in dysfunctional cognitions (b = −0.20, 95% CI [−0.42, −0.04]). Positive reappraisal significantly increased in the MORE group, but it did not directly predict reductions in IGD or craving (p = 0.12 and p = 0.07, respectively). | 9/9 |
| (Sakuma et al., 2017) | Design: Non-randomized experimental study Objective: To evaluate the efficacy of the Self-Discovery Camp (SDiC), a Japanese residential therapeutic camp, in improving the symptoms of Internet Gaming Disorder (IGD). | N = 10 Sex: Male Mean Age: 16.2 years | Internet Gaming Disorder: Hours per day/week (Questionnaire + Interview) Problem Recognition: SOCRATES (Stages of Change Readiness and Treatment Eagerness Scale) | The total internet gaming time significantly decreased three months after treatment at the Self-Discovery Camp, with an average reduction of 3.18 h per day (p = 0.044, d = 1.15). The number of hours spent gaming per week significantly decreased, with a reduction of 27.04 hours per week (p = 0.024, d = 1.26). The number of days per week participants played did not show significant changes post-treatment (p = 0.18, d = 0.31). Self-efficacy significantly improved, with an increase in the “Taking Action” subscale score of the SOCRATES scale (p = 0.012, d = 1.00), indicating greater confidence among participants in reducing their addictive behavior. No significant differences were found in the “Problem Recognition” subscale (p = 0.45) or the “Ambivalence” subscale (p = 0.28), suggesting that the perception of the disorder did not change substantially. A significant positive correlation was found between the age of onset of IGD and problem recognition (r = 0.781, p = 0.008), indicating that participants who developed the disorder at an older age were more aware of their addiction. | 8/9 |
| (Yao et al., 2017) | Desing: Experimental Study non-randomized Objective: Valuate the efficacy of a group behavioral intervention combining reality therapy and mindfulness meditation in reducing decisional impulsivity and IGD severity. | N = 46 Sex: Not specified Age: 18–26 years | Internet Gaming Disorder: CIAS (Chinese Internet Addiction Scale) Impulsivity in Decision-Making: DDT (Decision Delay Task), BART (Balloon Analog Risk Task) Anxiety: BAI (Beck Anxiety Inventory) Depression: BDI (Beck Depression Inventory) | The IGD and HC groups did not differ significantly in age or years of education (p > 0.05). The IGD group scored significantly higher than the HC group on CIAS, BAI, and BDI (ps < 0.001), with effects remaining significant after Bonferroni correction (p < 0.01). In the DDT, the IGD group showed higher impulsivity in decision-making, reflected in a higher log-transformed k value compared to the HC group (p = 0.001). In the BART, the IGD group exploded more balloons than the HC group (p = 0.023), but no significant differences were found in the adjusted average number of pumps. After the intervention, the IGD group showed a significant reduction in the k value on the DDT compared to baseline measurement (F(1,35) = 15.90, p < 0.001, η2 = 0.31), whereas the HC group showed no significant changes (F(1,35) = 0.06, p = 0.81). The IGD group experienced a significant decrease in CIAS, BAI, and BDI scores after the intervention (ps < 0.001). In the multiple linear regression, only changes in the k value on the DDT were significantly associated with changes in CIAS scores (Beta = 0.53, p = 0.04). | 8/9 |
References
- André, F., Kapetanovic, S., Einarsson, I., Trebbin Harvard, S., Franzén, L., Möttus, A., Håkansson, A., & Claesdotter-Knutsson, E. (2023). Relapse prevention therapy for internet gaming disorder in Swedish child and adolescent psychiatric clinics: A randomized controlled trial. Frontiers in Psychiatry, 14, 1256413. [Google Scholar] [CrossRef]
- Auerbach, R. P., Mortier, P., Bruffaerts, R., Alonso, J., Benjet, C., Cuijpers, P., Demyttenaere, K., Ebert, D. D., Green, J. G., Hasking, P., Murray, E., Nock, M. K., Pinder-Amaker, S., Sampson, N. A., Stein, D. J., Vilagut, G., Zaslavsky, A. M., & Kessler, R. C. (2018). WHO world mental health surveys international college student project: Prevalence and distribution of mental disorders. Journal of Abnormal Psychology, 127(7), 623–638. [Google Scholar] [CrossRef]
- Balhara, Y. P. S., Singh, S., Saini, R., Dahiya, N., Singh, A. B., & Kumar, R. (2021). Should internet gaming disorder be considered a subtype of generalized problematic internet use? Findings from a study among medical college students. Perspectives in Psychiatric Care, 57(1), 272–278. [Google Scholar] [CrossRef]
- Bargeron, A. H., & Hormes, J. M. (2017). Psychosocial correlates of internet gaming disorder: Psychopathology, life satisfaction, and impulsivity. Computers in Human Behavior, 68, 388–394. [Google Scholar] [CrossRef]
- Castro-Calvo, J., King, D. L., Stein, D. J., Brand, M., Carmi, L., Chamberlain, S. R., Demetrovics, Z., Fineberg, N. A., Rumpf, H., Yücel, M., Achab, S., Ambekar, A., Bahar, N., Blaszczynski, A., Bowden-Jones, H., Carbonell, X., Chan, E. M. L., Ko, C., de Timary, P., … Billieux, J. (2021). Expert appraisal of criteria for assessing gaming disorder: An international Delphi study. Addiction, 116(9), 2463–2475. [Google Scholar] [CrossRef]
- De Pasquale, C., Sciacca, F., Martinelli, V., Chiappedi, M., Dinaro, C., & Hichy, Z. (2020). Relationship of internet gaming disorder with psychopathology and social adaptation in italian young adults. International Journal of Environmental Research and Public Health, 17(21), 8201. [Google Scholar] [CrossRef]
- Dong, G.-H., Dai, J., & Potenza, M. N. (2024). Ten years of research on the treatments of internet gaming disorder: A scoping review and directions for future research. Journal of Behavioral Addictions, 13(1), 51–65. [Google Scholar] [CrossRef]
- Feng, W., Ramo, D. E., Chan, S. R., & Bourgeois, J. A. (2017). Internet gaming disorder: Trends in prevalence 1998–2016. Addictive Behaviors, 75, 17–24. [Google Scholar] [CrossRef]
- Fumero, A., Marrero, R. J., Bethencourt, J. M., & Peñate, W. (2020). Risk factors of internet gaming disorder symptoms in Spanish adolescents. Computers in Human Behavior, 111, 106416. [Google Scholar] [CrossRef]
- Han, J., Seo, Y., Hwang, H., Kim, S. M., & Han, D. H. (2020). Efficacy of cognitive behavioural therapy for internet gaming disorder. Clinical Psychology & Psychotherapy, 27(2), 203–213. [Google Scholar] [CrossRef]
- Han, X., Wang, Y., Jiang, W., Bao, X., Sun, Y., Ding, W., Cao, M., Wu, X., Du, Y., & Zhou, Y. (2018). Resting-state activity of prefrontal-striatal circuits in internet gaming disorder: Changes with cognitive behavior therapy and predictors of treatment response. Frontiers in Psychiatry, 9, 341. [Google Scholar] [CrossRef]
- Hong, J. S., Kim, S. M., Kang, K. D., Han, D. H., Kim, J. S., Hwang, H., Min, K. J., Choi, T. Y., & Lee, Y. S. (2020). Effect of physical exercise intervention on mood and frontal alpha asymmetry in internet gaming disorder. Mental Health and Physical Activity, 18, 100318. [Google Scholar] [CrossRef]
- Igarashi, R., Bhoumik, K., & Thompson, J. (2024). Investigating the effectiveness of virtual influencers in prosocial marketing. Psychology & Marketing, 41(9), 2121–2135. [Google Scholar] [CrossRef]
- Jo, Y. S., Bhang, S. Y., Choi, J. S., Lee, H. K., Lee, S. Y., & Kweon, Y.-S. (2019). Clinical characteristics of diagnosis for internet gaming disorder: Comparison of DSM-5 IGD and ICD-11 GD diagnosis. Journal of Clinical Medicine, 8(7), 945. [Google Scholar] [CrossRef]
- Kang, K. D., Jung, T. W., Park, I. H., & Han, D. H. (2018). Effects of equine-assisted activities and therapies on the affective network of adolescents with internet gaming disorder. The Journal of Alternative and Complementary Medicine, 24(8), 841–849. [Google Scholar] [CrossRef]
- Kochuchakkalackal Kuriala, G., & Reyes, M. E. S. (2023). Cross-cultural efficacy of the acceptance and cognitive restructuring intervention program (ACRIP) on the internet gaming disorder symptoms of selected asian adolescents. Psychological Studies, 68(3), 326–334. [Google Scholar] [CrossRef]
- Lee, J., Bae, S., Kim, B. N., & Han, D. H. (2021). Impact of attention-deficit/hyperactivity disorder comorbidity on longitudinal course in Internet gaming disorder: A 3-year clinical cohort study. Journal of Child Psychology and Psychiatry, 62(9), 1110–1119. [Google Scholar] [CrossRef]
- Li, W., Garland, E. L., & Howard, M. O. (2018). Therapeutic mechanisms of mindfulness-oriented recovery enhancement for internet gaming disorder: Reducing craving and addictive behavior by targeting cognitive processes. Journal of Addictive Diseases, 37(1–2), 5–13. [Google Scholar] [CrossRef]
- Li, W., Garland, E. L., McGovern, P., O’Brien, J. E., Tronnier, C., & Howard, M. O. (2017). Mindfulness-oriented recovery enhancement for internet gaming disorder in U.S. adults: A stage I randomized controlled trial. Psychology of Addictive Behaviors, 31(4), 393–402. [Google Scholar] [CrossRef]
- Maden, Ç., Bayramlar, K., Arıcak, O. T., & Yagli, N. V. (2022). Effects of virtual reality-based training and aerobic training on gaming disorder, physical activity, physical fitness, and anxiety: A randomized, controlled trial. Mental Health and Physical Activity, 23, 100465. [Google Scholar] [CrossRef]
- Magill, M., Ray, L., Kiluk, B., Hoadley, A., Bernstein, M., Tonigan, J. S., & Carroll, K. (2019). A meta-analysis of cognitive-behavioral therapy for alcohol or other drug use disorders: Treatment efficacy by contrast condition. Journal of Consulting and Clinical Psychology, 87(12), 1093–1105. [Google Scholar] [CrossRef]
- Marcelle, E. T., Nolting, L., Hinshaw, S. P., & Aguilera, A. (2019). Effectiveness of a multimodal digital psychotherapy platform for adult depression: A naturalistic feasibility study. JMIR MHealth and UHealth, 7(1), e10948. [Google Scholar] [CrossRef]
- Moghaddas, F., Assarian, F., Ahmadvand, A., Rahimi, H., & Ramezani, S. (2023). Treatment outcomes of acceptance and commitment therapy on severity of internet gaming disorder comorbid with ADHD in adolescents. International Archives of Health Sciences, 10(1), 20. [Google Scholar] [CrossRef]
- Ni, H., Wang, H., Ma, X., Li, S., Liu, C., Song, X., Potenza, M. N., & Dong, G. H. (2024). Efficacy and neural mechanisms of mindfulness meditation among adults with internet gaming disorder: A randomized clinical trial. JAMA Network Open, 7(6), e2416684. [Google Scholar] [CrossRef]
- Nielsen, P., Christensen, M., Henderson, C., Liddle, H. A., Croquette-Krokar, M., Favez, N., & Rigter, H. (2021). Multidimensional family therapy reduces problematic gaming in adolescents: A randomised controlled trial. Journal of Behavioral Addictions, 10(2), 234–243. [Google Scholar] [CrossRef]
- Nielsen, P., Favez, N., & Rigter, H. (2020). Parental and family factors associated with problematic gaming and problematic internet use in adolescents: A systematic literature review. Current Addiction Reports, 7(3), 365–386. [Google Scholar] [CrossRef]
- Park, S. Y., Kim, S. M., Roh, S., Soh, M.-A., Lee, S. H., Kim, H., Lee, Y. S., & Han, D. H. (2016). The effects of a virtual reality treatment program for online gaming addiction. Computer Methods and Programs in Biomedicine, 129, 99–108. [Google Scholar] [CrossRef]
- Pascoe, M., Bailey, A. P., Craike, M., Carter, T., Patten, R., Stepto, N., & Parker, A. (2020). Physical activity and exercise in youth mental health promotion: A scoping review. BMJ Open Sport & Exercise Medicine, 6(1), e000677. [Google Scholar] [CrossRef]
- Paulus, F. W., Ohmann, S., von Gontard, A., & Popow, C. (2018). Internet gaming disorder in children and adolescents: A systematic review. Developmental Medicine & Child Neurology, 60(7), 645–659. [Google Scholar] [CrossRef]
- Pearcy, B. T. D., McEvoy, P. M., & Roberts, L. D. (2017). Internet gaming disorder explains unique variance in psychological distress and disability after controlling for comorbid depression, OCD, ADHD, and anxiety. Cyberpsychology, Behavior, and Social Networking, 20(2), 126–132. [Google Scholar] [CrossRef]
- Pornnoppadol, C., Ratta-apha, W., Chanpen, S., Wattananond, S., Dumrongrungruang, N., Thongchoi, K., Panchasilawut, S., Wongyuen, B., Chotivichit, A., Laothavorn, J., & Vasupanrajit, A. (2020). A comparative study of psychosocial interventions for internet gaming disorder among adolescents aged 13–17 years. International Journal of Mental Health and Addiction, 18(4), 932–948. [Google Scholar] [CrossRef]
- Sakuma, H., Mihara, S., Nakayama, H., Miura, K., Kitayuguchi, T., Maezono, M., Hashimoto, T., & Higuchi, S. (2017). Treatment with the self-discovery camp (SDiC) improves internet gaming disorder. Addictive Behaviors, 64, 357–362. [Google Scholar] [CrossRef]
- Shin, Y.-B., Kim, J.-J., Kim, H., Kim, S.-J., Eom, H., Jung, Y. H., & Kim, E. (2021). Managing game-related conflict with parents of young adults with internet gaming disorder: Development and feasibility study of a virtual reality app. JMIR Serious Games, 9(1), e22494. [Google Scholar] [CrossRef]
- Smith, P. J., & Merwin, R. M. (2021). The role of exercise in management of mental health disorders: An integrative review. Annual Review of Medicine, 72(1), 45–62. [Google Scholar] [CrossRef]
- Teng, Z., Pontes, H. M., Nie, Q., Xiang, G., Griffiths, M. D., & Guo, C. (2020). Internet gaming disorder and psychosocial well-being: A longitudinal study of older-aged adolescents and emerging adults. Addictive Behaviors, 110, 106530. [Google Scholar] [CrossRef]
- Torres-Rodríguez, A., Griffiths, M. D., Carbonell, X., & Oberst, U. (2018). Treatment efficacy of a specialized psychotherapy program for internet gaming disorder. Journal of Behavioral Addictions, 7(4), 939–952. [Google Scholar] [CrossRef]
- Wu, A. M. S., Chen, J. H., Tong, K.-K., Yu, S., & Lau, J. T. F. (2018). Prevalence and associated factors of Internet gaming disorder among community dwelling adults in Macao, China. Journal of Behavioral Addictions, 7(1), 62–69. [Google Scholar] [CrossRef]
- Wu, L., Potenza, M. N., Zhou, N., Kober, H., Shi, X., Yip, S. W., Xu, J., Zhu, L., Wang, R., Liu, G., & Zhang, J. (2021). Efficacy of single-session transcranial direct current stimulation on addiction-related inhibitory control and craving: A randomized trial in males with Internet gaming disorder. Journal of Psychiatry and Neuroscience, 46(1), E111–E118. [Google Scholar] [CrossRef]
- Yao, Y.-W., Chen, P.-R., Li, C. R., Hare, T. A., Li, S., Zhang, J.-T., Liu, L., Ma, S.-S., & Fang, X.-Y. (2017). Combined reality therapy and mindfulness meditation decrease intertemporal decisional impulsivity in young adults with internet gaming disorder. Computers in Human Behavior, 68, 210–216. [Google Scholar] [CrossRef]
- Yen, J.-Y., Higuchi, S., Lin, P.-Y., Lin, P.-C., Chou, W.-P., & Ko, C.-H. (2022). Functional impairment, insight, and comparison between criteria for gaming disorder in the international classification of diseases, 11 edition and internet gaming disorder in diagnostic and statistical manual of mental disorders, fifth edition. Journal of Behavioral Addictions, 11(4), 1012–1023. [Google Scholar] [CrossRef]
- Zhang, J. T., Ma, S., Li, C. R., Liu, L., Xia, C., Lan, J., Wang, L., Liu, B., Yao, Y., & Fang, X. (2018). Craving behavioral intervention for internet gaming disorder: Remediation of functional connectivity of the ventral striatum. Addiction Biology, 23(1), 337–346. [Google Scholar] [CrossRef]
- Zhang, J. T., Yao, Y. W., Potenza, M. N., Xia, C. C., Lan, J., Liu, L., Wang, L. J., Liu, B., Ma, S. S., & Fang, X. Y. (2016). Effects of craving behavioral intervention on neural substrates of cue-induced craving in Internet gaming disorder. NeuroImage: Clinical, 12, 591–599. [Google Scholar] [CrossRef]
- Zhao, Q., Zhang, Y., Wang, M., Ren, J., Chen, Y., Chen, X., Wei, Z., Sun, J., & Zhang, X. (2022). Effects of retrieval-extinction training on internet gaming disorder. Journal of Behavioral Addictions, 11(1), 49–62. [Google Scholar] [CrossRef]
- Zheng, Y., He, J., Fan, L., & Qiu, Y. (2022). Reduction of symptom after a combined behavioral intervention for reward sensitivity and rash impulsiveness in internet gaming disorder: A comparative study. Journal of Psychiatric Research, 153, 159–166. [Google Scholar] [CrossRef]
- Zheng, Y., Zhao, Y., Chen, X., & Li, S. (2024). Effect of physical exercise on the emotional and cognitive levels of patients with substance use disorder: A meta-analysis. Frontiers in Psychology, 15, 1348224. [Google Scholar] [CrossRef]
| Population | Adolescents and Young Adults (10–30 Years Old) Diagnosed with Gaming Disorder |
|---|---|
| Intervention | Treatment strategies, therapeutic interventions |
| Outcomes | Reduction in IGD symptoms |
| Research Question | What is the effectiveness of therapeutic interventions in reducing IGD symptoms in adolescents and young adults diagnosed with this disorder? |
| Database | Search Strategy |
|---|---|
| Pubmed | (“Gaming Disorder” OR “Video Game Addiction” OR “Internet Gaming Disorder” OR “Problematic Gaming” OR “Gaming Dependency” OR “Video Game Overuse” OR “Excessive Gaming”) AND (“adolescents” OR “young adults” OR “children” OR “teenagers” OR “youth”) AND (“therapy” OR “treatment” OR “psychological intervention” OR “cognitive therapy” OR “behavioral therapy” OR “mental health therapy” OR “CBT” OR “cognitive behavioral therapy”) AND (“outcomes” OR “symptoms” OR “improvement” OR “reduction” OR “health improvement” OR “clinical improvement”) |
| Web of Science | TS = (“Gaming Disorder” OR “IGD” OE “Video Game Addiction” OR “Internet Gaming Disorder” OR “Problematic Gaming” OR “Gaming Dependency” OR “Video Game Overuse” OR “Excessive Gaming”) AND TS = (“therapy” OR “treatment” OR “psychological intervention” OR “cognitive therapy” OR “behavioral therapy” OR “CBT” OR “cognitive behavioral therapy” OR “mental health therapy”) AND TS = (“symptoms” OR “outcomes” OR “improvement” OR “reduction” OR “health improvement” OR “clinical improvement”) |
| Scopus | TITLE-ABS-KEY(“Gaming Disorder” OR “Video Game Addiction” OR “Internet Gaming Disorder” OR “Problematic Video Gaming” OR “Gaming Dependency” OR “Excessive Gaming”) AND TITLE-ABS-KEY(“adolescents” OR “young adults” OR “children” OR “teenagers” OR “youth”) AND TITLE-ABS-KEY(“therapy” OR “treatment” OR “intervention” OR “psychological therapy” OR “behavioral therapy” OR “CBT”) AND TITLE-ABS-KEY(“symptoms” OR “outcomes” OR “improvement” OR “reduction”) |
| Science Direct | (“Gaming Disorder” OR “IGD” OR “Internet Gaming Disorder” OR “Video Game Addiction”) (“therapy” OR “treatment” OR “psychological intervention”) (“adolescents” OR “young adults” OR “youth”) (“symptoms” OR “outcomes” OR “clinical improvement”) |
| Study | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (Ni et al., 2024) | + | + | + | - | - | - | + | + | + | + | + | + | + |
| (Hong et al., 2020) | + | + | + | - | - | - | + | + | + | + | + | + | + |
| (Park et al., 2016) | + | + | + | - | - | + | + | + | + | + | + | + | + |
| (Maden et al., 2022) | |||||||||||||
| (Zheng et al., 2022) | + | - | + | - | + | - | + | - | + | + | + | + | + |
| (Kochuchakkalackal Kuriala & Reyes, 2023) | + | - | + | + | - | - | + | + | + | + | + | + | + |
| (L. Wu et al., 2021) | + | + | + | + | + | + | + | - | - | + | + | + | + |
| (Nielsen et al., 2021) | + | + | + | - | - | + | + | + | + | + | + | + | + |
| (Zhao et al., 2022) | + | + | + | + | - | + | + | + | + | + | + | + | + |
| Study | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 |
|---|---|---|---|---|---|---|---|---|---|
| (Shin et al., 2021) | + | + | + | + | + | - | + | + | + |
| (André et al., 2023) | + | + | + | + | + | + | + | + | + |
| (Torres-Rodríguez et al., 2018) | + | + | + | + | + | + | + | + | + |
| (Igarashi et al., 2024) | + | + | - | + | + | + | + | + | + |
| (Marcelle et al., 2019) | + | + | - | + | + | + | + | + | + |
| (Zhang et al., 2016) | + | + | - | + | + | + | + | + | + |
| (Pornnoppadol et al., 2020) | + | + | + | + | + | + | + | + | + |
| (Zhang et al., 2018) | + | + | - | + | + | + | + | + | + |
| (Kang et al., 2018) | |||||||||
| (J. Han et al., 2020) | + | + | + | + | + | + | + | + | + |
| (Li et al., 2018) | + | + | + | + | + | + | + | + | + |
| (Sakuma et al., 2017) | + | + | + | - | + | + | + | + | + |
| (Yao et al., 2017) | + | + | + | + | + | - | + | + | + |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the University Association of Education and Psychology. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Núñez-Rodríguez, S.; Burgos-González, D.; Mínguez-Mínguez, L.A.; Menéndez-Vega, F.; Antoñanzas-Laborda, J.L.; González-Bernal, J.J.; González-Santos, J. Effectiveness of Therapeutic Interventions in the Treatment of Internet Gaming Disorder: A Systematic Review. Eur. J. Investig. Health Psychol. Educ. 2025, 15, 49. https://doi.org/10.3390/ejihpe15040049
Núñez-Rodríguez S, Burgos-González D, Mínguez-Mínguez LA, Menéndez-Vega F, Antoñanzas-Laborda JL, González-Bernal JJ, González-Santos J. Effectiveness of Therapeutic Interventions in the Treatment of Internet Gaming Disorder: A Systematic Review. European Journal of Investigation in Health, Psychology and Education. 2025; 15(4):49. https://doi.org/10.3390/ejihpe15040049
Chicago/Turabian StyleNúñez-Rodríguez, Sandra, David Burgos-González, Luis Alberto Mínguez-Mínguez, Félix Menéndez-Vega, José Luis Antoñanzas-Laborda, Jerónimo Javier González-Bernal, and Josefa González-Santos. 2025. "Effectiveness of Therapeutic Interventions in the Treatment of Internet Gaming Disorder: A Systematic Review" European Journal of Investigation in Health, Psychology and Education 15, no. 4: 49. https://doi.org/10.3390/ejihpe15040049
APA StyleNúñez-Rodríguez, S., Burgos-González, D., Mínguez-Mínguez, L. A., Menéndez-Vega, F., Antoñanzas-Laborda, J. L., González-Bernal, J. J., & González-Santos, J. (2025). Effectiveness of Therapeutic Interventions in the Treatment of Internet Gaming Disorder: A Systematic Review. European Journal of Investigation in Health, Psychology and Education, 15(4), 49. https://doi.org/10.3390/ejihpe15040049







