Analysis of the Factorial Structure and Reliability of the Social Determinants of Mental Health Questionnaire for Young Adults (SDMH)
Abstract
:1. Introduction
2. Method
2.1. Participant Characteristics
2.2. Inclusion and Exclusion Criteria
2.3. Sampling Procedures
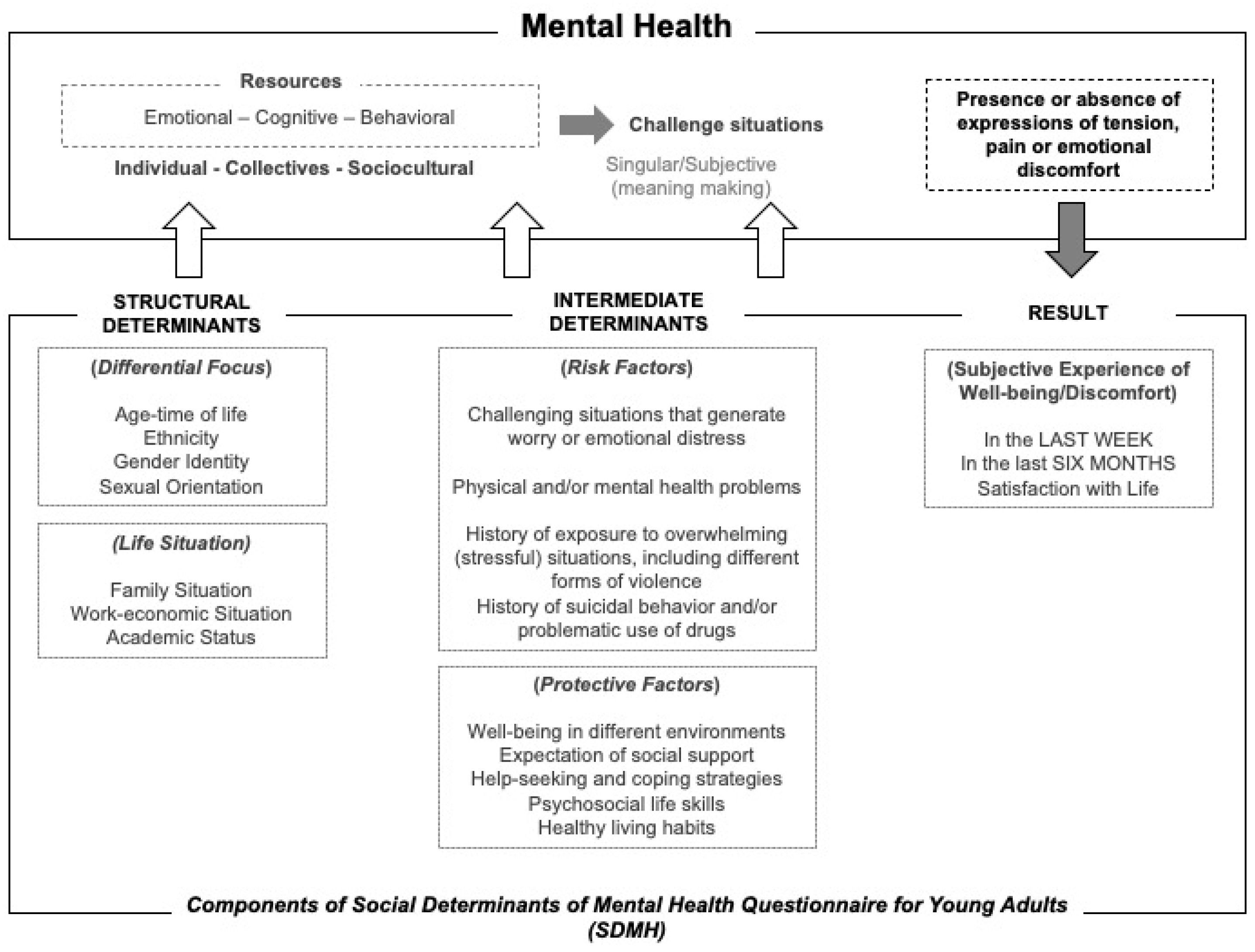
2.4. Instrument
2.5. Measurement of Constructs and Procedure
2.6. Data Collection
2.7. Analytic Strategy
3. Results
3.1. Reliability
3.2. Evidence of the Factorial Structure of the Questionnaire
3.3. Invariance Analysis
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ai, X., Yang, J., Lin, Z., & Wan, X. (2021). Mental health and the role of physical activity during the COVID-19 pandemic. Frontiers in Psychology, 12, 759987. [Google Scholar] [CrossRef]
- American Educational Research Association, American Psychological Association & National Council on Measurement in Education. (2014). Standards for educational and psychological testing. American Educational Research Association. Available online: https://www.testingstandards.net/open-access-files.html (accessed on 20 March 2024).
- Bener, A., Morgul, E., Tokaç, M., Ventriglio, A., & Jordan, T. R. (2024). Sleep quality, quality of life, fatigue, and mental health in COVID-19 post-pandemic Türkiye: A cross-sectional study. Frontiers in Public Health, 12, 1250085. [Google Scholar] [CrossRef]
- Bentler, P. M. (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107(2), 234–246. [Google Scholar] [CrossRef] [PubMed]
- Browne, M., & Cudeck, R. (1993). Alternative ways of assessing model fit. In K. A. Bollen, & J. S. Long (Eds.), Testing structural equation models (pp. 136–162). SAGE Publicatons. [Google Scholar]
- Carod-Artal, F. J. (2017). Social determinants of mental health. In S. Bährer-Kohler, & F. J. Carod-Artal (Eds.), Global mental health: Prevention and promotion (pp. 33–46). Springer International Publishing/Springer Nature. [Google Scholar] [CrossRef]
- Cheung, G. W., & Rensvold, R. B. (2002). Evaluating goodness-of-fit indexes for testing measurement invariance. Structural Equation Modeling, 9(2), 233–255. [Google Scholar] [CrossRef]
- Chirikov, I., Soria, K. M., Horgos, B., & Jones-White, D. (2020). Undergraduate and graduate students’ mental health during the COVID-19 pandemic. UC Berkeley, Center for Studies in Higher Education. Available online: https://escholarship.org/uc/item/80k5d5hw (accessed on 10 April 2023).
- Colby, A., Fereday, B., Le, N. Q., & Malin, H. (2023). A longitudinal study of US college students before and during the COVID-19 pandemic. Journal of American College Health, 73(1), 290–300. [Google Scholar] [CrossRef]
- Costa, A. C. D. S., Menon, V., Phadke, R., Dapke, K., Miranda, A. V., Ahmad, S., Essar, M. Y., & Hashim, H. T. (2022). Mental health in the post COVID-19 era: Future perspectives. Einstein, 20, eCE6760. [Google Scholar] [CrossRef] [PubMed]
- Departamento Administrativo Nacional de Estadística—DANE. (2020). Guía para la inclusión del enfoque diferencial e interseccional. Available online: https://www.dane.gov.co/files/investigaciones/genero/guia-inclusion-enfoque-difencias-intersecciones-produccion-estadistica-SEN.pdf (accessed on 12 July 2022).
- Farfán-Latorre, M., Estrada-Araoz, E. G., Lavilla-Condori, W. G., Ulloa-Gallardo, N. J., Calcina-Álvarez, D. A., Meza-Orue, L. A., Yancachajlla-Quispe, L. I., & Rengifo Ramírez, S. S. (2023). Mental health in the post-pandemic period: Depression, anxiety, and stress in peruvian university students upon return to face-to-face classes. Sustainability, 15(15), 11924. [Google Scholar] [CrossRef]
- Fernández-Theoduloz, G., Chirullo, V., Montero, F., Ruiz, P., Selma, H., & Paz, V. (2024). Longitudinal changes in depression and anxiety during COVID-19 crisis in Uruguay. Current Psychology, 43, 13841–13849. [Google Scholar] [CrossRef]
- Foster, S., Estévez-Lamorte, N., Walitza, S., Dzemaili, S., & Mohler-Kuo, M. (2023a). Perceived stress, coping strategies, and mental health status among adolescents during the COVID-19 pandemic in Switzerland: A longitudinal study. European Child & Adolescent Psychiatry, 32(6), 937–949. [Google Scholar] [CrossRef]
- Foster, S., Estévez-Lamorte, N., Walitza, S., & Mohler-Kuo, M. (2023b). The impact of the COVID-19 pandemic on young adults’ mental health in Switzerland: A longitudinal cohort study from 2018 to 2021. International Journal of Environmental Research and Public Health, 20(3), 2598. [Google Scholar] [CrossRef] [PubMed]
- Fruehwirth, J., Huang, L., Tompson, C., & Perreira, K. (2025). Mental health symptoms among US college students before, early, and late into the COVID-19 Pandemic: A longitudinal analysis. Journal of Adolescent Health, 76(2), 246–253. [Google Scholar] [CrossRef] [PubMed]
- Galvani-Townsend, S., Martinez, I., & Pandey, A. (2022). Is life expectancy higher in countries and territories with publicly funded healthcare? Global analysis of healthcare access and the social determinants of health. Journal of Global Health, 12, 04091. [Google Scholar] [CrossRef]
- Gori, A., & Topino, E. (2021). Across the COVID-19 waves; assessing temporal fluctuations in perceived stress, post-traumatic symptoms, worry, anxiety and civic moral disengagement over one year of pandemic. International Journal of Environmental Research and Public Health, 18(11), 5651. [Google Scholar] [CrossRef]
- Hyland, P., Shevlin, M., Murphy, J., McBride, O., Fox, R., Bondjers, K., Karatzias, T., Bentall, R. P., Martinez, A., & Vallières, F. (2021). A longitudinal assessment of depression and anxiety in the Republic of Ireland before and during the COVID-19 pandemic. Psychiatry Research, 300, 113905. [Google Scholar] [CrossRef] [PubMed]
- IBM. (2019). Guía del usuario de IBM SPSS Statistics 26. IBM Software Group. Available online: https://www.ibm.com/docs/en/SSLVMB_26.0.0/pdf/es/IBM_SPSS_Statistics_Core_System_User_Guide.pdf (accessed on 18 March 2023).
- Kauhanen, L., Wan Mohd Yunus, W. M. A., Lempinen, L., Peltonen, K., Gyllenberg, D., Mishina, K., Gilbert, S., Bastola, K., Brown, J. S. L., & Sourander, A. (2023). A systematic review of the mental health changes of children and young people before and during the COVID-19 pandemic. European Child & Adolescent Psychiatry, 32(6), 995–1013. [Google Scholar] [CrossRef]
- Kirkbride, J. B., Anglin, D. M., Colman, I., Dykxhoorn, J., Jones, P. B., Patalay, P., Pitman, A., Soneson, E., Steare, T., Wright, T., & Griffiths, S. L. (2024). The social determinants of mental health and disorder: Evidence, prevention and recommendations. World Psychiatry, 23(1), 58–90. [Google Scholar] [CrossRef] [PubMed]
- Kwan, B., & Rickwood, D. J. (2015). A systematic review of mental health outcome measures for young people aged 12 to 25 years. BMC Psychiatry, 15, 279. [Google Scholar] [CrossRef] [PubMed]
- Lee, K. X., Quek, K. F., & Ramadas, A. (2024). Factors Associated with the Health-Related Quality of Life of Malaysian Young Adults Post-Pandemic. Nursing Reports, 14(2), 1158–1169. [Google Scholar] [CrossRef]
- Ley 1616 de 2013. (2013) January 21. Congreso de la República. Diario Oficial No. 48.680. Available online: http://www.secretariasenado.gov.co/senado/basedoc/ley_1616_2013.html (accessed on 10 April 2023).
- Ministerio de Salud y Protección Social. (1993). Resolución No. 008430 de 1993. Available online: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/DIJ/RESOLUCION-8430-DE-1993.pdf (accessed on 1 February 2023).
- Ministerio de Salud y Protección Social. (2018). Política nacional de salud mental [National mental health policy]. Available online: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/PP/politica-nacional-salud-mental.pdf (accessed on 1 February 2023).
- Mundfrom, D. J., Shaw, D. G., & Ke, T. L. (2005). Minimum sample size recommendations for conducting factor analyses. International Journal of Testing, 5(2), 159–168. [Google Scholar] [CrossRef]
- Muñiz, J., & Fonseca-Pedrero, E. (2019). Diez pasos para la construcción de un test [Ten steps to build a test]. Psicothema, 31(1), 7–16. [Google Scholar] [CrossRef]
- Organización Panamericana de la Salud. (2023). Informe mundial sobre la salud mental: Transformar la salud mental para todos [World mental health report: Transforming mental health for all]. Organización Panamericana de la Salud. [Google Scholar] [CrossRef]
- Puime, Á. O., & Zunzunegui, M. V. (2011). Determinantes sociales de la salud y su influencia en la atención sanitaria [Social determinants of health and their influence on health care]. In A. Martín, G. Jodar, J. M. Bosch, & C. Albéniz (Eds.), Atención familiar y salud comunitaria: Conceptos y materiales para docentes y estudiantes [Family care and community health: Concepts and materials for teachers and students] (pp. 87–99). Elsevier España. Available online: https://dsp.facmed.unam.mx/wp-content/uploads/2022/02/Determinantes-Sociales-de-la-Salud.pdf (accessed on 15 July 2023).
- Rodríguez, V., Moreno, S., Camacho, J., Gómez-Restrepo, C., de Santacruz, C., Rodríguez, M. N., & Martínez, N. T. (2016). Diseño e implementación de los instrumentos de recolección de la Encuesta Nacional de Salud Mental Colombia 2015 [Design and implementation of the data collection tools for national mental health survey of Colombia, 2015]. Revista Colombiana de Psiquiatría, 45, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Sanabria-Mazo, J. P., Useche-Aldana, B., Ochoa, P. P., Rojas-Gualdrón, D. F., & Sanz, A. (2021). Impacto de la pandemia de COVID-19 en la salud mental en Colombia [Impact of the COVID-19 pandemic on mental health in Colombia]. Editorial CES. Available online: https://www.colpsic.org.co/wp-content/uploads/2021/09/Libro-Impacto-de-la-pandemia-de-COVID-19-en-la-salud-mental-en-Colombia.pdf (accessed on 15 July 2023).
- Scorsolini-Comin, F., Patias, N. D., Cozzer, A. J., Flores, P. A. W., & Hohendorff, J. V. (2021). Mental health and coping strategies in graduate students in the COVID-19 pandemic. Revista Latino-Americana de Enfermagem, 29, e3491. [Google Scholar] [CrossRef] [PubMed]
- Scott, L. L., Hanson, A. R., & Aubuchon-Endsley, N. L. (2025). Social determinants of maternal antenatal depression. Journal of Rural Mental Health. [Google Scholar] [CrossRef]
- Slaney, K. L., Storey, J. E., & Barnes, J. (2011). Is my test valid? Guidelines for the practicing psychologist for evaluating the psychometric properties of measures. The International Journal of Forensic Mental Health, 10(4), 261–283. [Google Scholar] [CrossRef]
- Steiger, J. H., & Lind, J. C. (1980, May 30). Statistically based tests for the number of common factors. Annual Spring Meeting of the Psychometric Society, Iowa City, IA, USA. [Google Scholar]
- Tabachnick, B. G., & Fidell, L. S. (2013). Using multivariate statistics (6th ed.). Pearson Education Inc. [Google Scholar]
- Tucker, L. R., & Lewis, C. (1973). A reliability coefficient for maximum likelihood factor analysis. Psychometrika, 38(1), 1–10. [Google Scholar] [CrossRef]
- Volpe, V. V., & Smith, N. A. (2024). To social distance or to not social distance? COVID-19 social impact and safety profiles, social determinants, and mental health of Black adults. American Journal of Orthopsychiatry, 94(2), 202–211. [Google Scholar] [CrossRef]
- World Health Organization. (1994). Life skills education for children and adolescents in schools. Available online: https://iris.who.int/handle/10665/63552 (accessed on 14 January 2023).
- World Health Organization. (2009). Comisión sobre determinantes sociales de la Salud [Commission on social determinants of health]. Available online: https://apps.who.int/gb/ebwha/pdf_files/A62/A62_9-sp.pdf (accessed on 14 January 2023).
- World Health Organization. (2022). Informe mundial sobre salud mental: Transformar la salud mental para todos. Panorama general [World mental health report: Transforming mental health for all. Executive summary]. Available online: https://www.who.int/es/publications/i/item/9789240050860 (accessed on 14 January 2023).
- Zhou, D. H. R., & Kwok, H. L. (2023). Navigating the landscape of mental health: Post-pandemic era and beyond. Asia Pacific Journal of Counselling and Psychotherapy, 14(2), 83–85. [Google Scholar] [CrossRef]
| Variable | Items | Women | Men | ||
|---|---|---|---|---|---|
| Sociodemographic data | |||||
| n | % | n | % | ||
| Sex | 576 | 46.8 | 656 | 53.2 | |
| Ethnicity | Mestizo | 396 | 68.8 | 499 | 76.1 |
| Afro-descendant | 146 | 25.3 | 110 | 16.8 | |
| Indigenous | 33 | 5.7 | 46 | 7.0 | |
| Roma | 1 | 0.2 | 1 | 0.2 | |
| Structural determinants associated with the vital transition | |||||
| Family nucleus | Family of origin | 549 | 95.3 | 627 | 95.6 |
| Other relatives | 20 | 3.5 | 20 | 3.0 | |
| Other people, not relatives | 2 | 0.3 | 4 | 0.6 | |
| Couple and children | 1 | 0.2 | 2 | 0.3 | |
| Single couple | 1 | 0.2 | 1 | 0.2 | |
| Alone | 3 | 0.5 | 2 | 0.3 | |
| Marital status | Single | 532 | 92.4 | 621 | 94.7 |
| Married | 9 | 1.6 | 3 | 0.5 | |
| Free union | 34 | 5.9 | 30 | 4.6 | |
| Divorced | 1 | 0.2 | 1 | 0.2 | |
| Widower | 1 | 0.2 | |||
| Currently in a relationship | Yes | 181 | 31.4 | 189 | 28.8 |
| Study | Yes | 576 | 100 | 656 | 100 |
| Satisfaction with studies | Do not know | 22 | 3.8 | 23 | 3.5 |
| Very low | 12 | 2.1 | 8 | 1.2 | |
| Low | 36 | 6.3 | 47 | 7.2 | |
| Medium | 153 | 26.6 | 173 | 26.4 | |
| High | 267 | 46.4 | 296 | 45.1 | |
| Very high | 86 | 14.9 | 109 | 16.6 | |
| Works | Yes | 174 | 30.2 | 209 | 31.9 |
| Dependent persons | Yes | 44 | 7.6 | 55 | 8.4 |
| Affiliated with health services | Yes | 558 | 96.9 | 621 | 94.7 |
| Intermediate determinants | |||||
| Chronic health problem | Yes | 67 | 11.6 | 77 | 11.7 |
| Treatment effectiveness: health problems | Yes | 48 | 8.3 | 53 | 8.1 |
| Functional diversity | Yes | 101 | 17.5 | 132 | 20.1 |
| Treatment or rehabilitation | Yes | 50 | 8.7 | 81 | 12.3 |
| Diagnosis in mental health | Yes | 115 | 20.0 | 137 | 20.9 |
| In treatment: mental health | Yes | 67 | 11.6 | 69 | 10.5 |
| Exposure to stressful situations | Yes | 473 | 82.1 | 530 | 80.8 |
| Many years ago | 242 | 42.0 | 279 | 42.5 | |
| More than six months ago | 122 | 21.2 | 125 | 19.1 | |
| In the last six months | 61 | 10.6 | 87 | 13.3 | |
| Currently | 46 | 8.0 | 36 | 5.5 | |
| Victim of violence | Yes | 309 | 53.6 | 347 | 52.9 |
| Physical | 76 | 13.2 | 88 | 13.4 | |
| Sexual | 47 | 8.2 | 51 | 7.8 | |
| Psychological | 112 | 19.4 | 122 | 18.6 | |
| In social networks | 10 | 1.7 | 8 | 1.2 | |
| Bullying | 43 | 7.5 | 59 | 9.0 | |
| Forced displacement | 21 | 3.6 | 19 | 2.9 | |
| Factor | Items | Scale Score | Minimum and Maximum Scores | Women (n = 576) | Men (n = 656) | α | ω | |||
|---|---|---|---|---|---|---|---|---|---|---|
| M | Of | M | Of | |||||||
| Well-being in the environment | Well-being at home | 4 | 0–6 | 0–24 | 17.44 | 3.70 | 17.54 | 3.77 | 0.71 | 0.71 |
| Well-being in the neighborhood | 4 | 0–6 | 0–24 | 13.72 | 4.89 | 13.80 | 4.93 | 0.59 | 0.63 | |
| Well-being in religious organizations | 4 | 0–6 | 0–24 | 7.02 | 7.61 | 6.26 | 7.65 | 0.87 | 0.88 | |
| Social welfare, culture, and recreation | 4 | 0–6 | 0–24 | 8.78 | 8.64 | 9.66 | 8.81 | 0.90 | 0.92 | |
| School wellness | 4 | 0–6 | 0–24 | 16.74 | 3.67 | 17.22 | 3.50 | 0.38 | 0.39 | |
| Well-being at work | 4 | 0–6 | 0–24 | 16.50 | 3.97 | 16.44 | 4.10 | 0.92 | 0.93 | |
| Protective factors | Expectation of social support | 8 | 0–6 | 0–48 | 25.79 | 9.08 | 26.36 | 9.16 | 0.67 | 0.69 |
| Healthy lifestyle habits | 8 | 1–6 | 1–48 | 25.15 | 5.88 | 25.64 | 6.11 | 0.71 | 0.69 | |
| Psychosocial skills for life | 10 | 1–5 | 10–50 | 36.19 | 7.91 | 36.34 | 7.88 | 0.90 | 0.90 | |
| Risk factors | Worry and emotional distress | 5 | 0–4 | 0–20 | 10.82 | 3.75 | 10.54 | 3.545 | 0.66 | 0.67 |
| Suicidal behavior | 3 | 0–1 | 0–3 | 1.04 | 1.03 | 0.97 | 1.05 | 0.63 | 0.63 | |
| Drug use | 5 | 0–4 | 0–20 | 2.70 | 2.68 | 2.78 | 2.61 | 0.63 | 0.62 | |
| Conflicts due to drug use | 7 | 0–2 | 0–14 | 4.37 | 3.52 | 4.73 | 3.56 | 0.93 | 0.93 | |
| Problematic internet use | 4 | 0–4 | 0–16 | 6.27 | 2.62 | 6.73 | 2.77 | 0.45 | 0.55 | |
| Problems due to problematic internet use | 7 | 0–2 | 0–14 | 6.31 | 2.805 | 6.20 | 2.94 | 0.85 | 0.85 | |
| Well-being and discomfort in the last week and the last six months | Emotional symptoms in the last week | 8 | 1–5 | 8–40 | 24.08 | 8.19 | 23.72 | 7.86 | 0.91 | 0.91 |
| Physical symptoms in the last week | 5 | 1–5 | 5–25 | 14.03 | 5.31 | 13.60 | 4.91 | 0.82 | 0.82 | |
| Well-being in the last week | 4 | 1–4 | 4–20 | 12.49 | 3.52 | 12.93 | 3.54 | 0.78 | 0.79 | |
| Emotional symptoms in the last six months | 8 | 1–5 | 8–40 | 23.43 | 8.17 | 23.86 | 8.49 | 0.94 | 0.93 | |
| Physical symptoms in the last six months | 5 | 1–5 | 5–25 | 13.72 | 5.5 | 13.37 | 5.30 | 0.88 | 0.88 | |
| Well-being in the last six months | 4 | 1–4 | 4–20 | 12.65 | 3.81 | 12.85 | 3.86 | 0.85 | 0.85 | |
| Domain | χ2 | gl | CFI | TLI | RMSEA (90% CI) |
|---|---|---|---|---|---|
| Well-being in various settings | 2127.48 | 234 | 0.874 | 0.851 | 0.081 (0.078, 0.084) |
| Protection factors | 1173.18 | 290 | 0.902 | 0.913 | 0.050 (0.047, 0.053) |
| Risk factors | 1721.05 | 415 | 0.908 | 0.918 | 0.051 (0.048, 0.053) |
| Well-being and discomfort in the last week | 867.78 | 114 | 0.912 | 0.926 | 0.073 (0.069, 0.078) |
| Well-being and discomfort in the last six months | 997.89 | 114 | 0.929 | 0.940 | 0.079 (0.075, 0.084) |
| Total scale (115 items) | 19,642.11 | 6211 | 0.829 | 0.820 | 0.042 (0.041, 0.043) |
| χ2 | gl | p | IFI | TLI | CFI | RMSEA (90% CI) | ∆gl | ∆CFI | |
|---|---|---|---|---|---|---|---|---|---|
| First-order model, 115 items, 21 factors (n = 1232) | 19,642.116 | 6211 | <0.001 | 0.830 | 0.820 | 0.829 | 0.042 (0.041, 0.043) | ||
| Females: First-order model, 115 items, 21 factors (n = 576) | 13,092.82 | 6211 | <0.001 | 0.823 | 0.811 | 0.821 | 0.044 (0.043, 0.045) | ||
| Males: First-order model, 115 items, 21 factors (n = 656) | 13,978.52 | 6211 | <0.001 | 0.815 | 0.803 | 0.814 | 0.044 (0.043, 0.045) | ||
| Invariance by gender | |||||||||
| Configural invariance | 27,071.44 | 12,422 | <0.001 | 0.819 | 0.807 | 0.817 | 0.031 (0.030, 0.031) | ||
| Metric invariance | 27,185.07 | 12,516 | <0.001 | 0.818 | 0.808 | 0.817 | 0.031 (0.030, 0.031) | 113.63 | 0.001 |
| Scalar invariance | 27,331.15 | 12,631 | <0.001 | 0.818 | 0.810 | 0.817 | 0.031 (0.030, 0.031) | 146.08 | 0.001 |
| Structural invariance | 27,653.76 | 12,863 | <0.001 | 0.816 | 0.812 | 0.815 | 0.031 (0.030, 0.031) | 322.61 | −0.002 |
| Residual invariance | 27,939.72 | 12,996 | <0.001 | 0.814 | 0.812 | 0.814 | 0.031 (0.030, 0.031) | 285.96 | −0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the University Association of Education and Psychology. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roncancio-Moreno, M.; Ocampo-Cepeda, R.P.; Zúñiga, W.M.; Cardona-Isaza, A.d.J. Analysis of the Factorial Structure and Reliability of the Social Determinants of Mental Health Questionnaire for Young Adults (SDMH). Eur. J. Investig. Health Psychol. Educ. 2025, 15, 18. https://doi.org/10.3390/ejihpe15020018
Roncancio-Moreno M, Ocampo-Cepeda RP, Zúñiga WM, Cardona-Isaza AdJ. Analysis of the Factorial Structure and Reliability of the Social Determinants of Mental Health Questionnaire for Young Adults (SDMH). European Journal of Investigation in Health, Psychology and Education. 2025; 15(2):18. https://doi.org/10.3390/ejihpe15020018
Chicago/Turabian StyleRoncancio-Moreno, Monica, Rita Patricia Ocampo-Cepeda, Walther M. Zúñiga, and Arcadio de Jesús Cardona-Isaza. 2025. "Analysis of the Factorial Structure and Reliability of the Social Determinants of Mental Health Questionnaire for Young Adults (SDMH)" European Journal of Investigation in Health, Psychology and Education 15, no. 2: 18. https://doi.org/10.3390/ejihpe15020018
APA StyleRoncancio-Moreno, M., Ocampo-Cepeda, R. P., Zúñiga, W. M., & Cardona-Isaza, A. d. J. (2025). Analysis of the Factorial Structure and Reliability of the Social Determinants of Mental Health Questionnaire for Young Adults (SDMH). European Journal of Investigation in Health, Psychology and Education, 15(2), 18. https://doi.org/10.3390/ejihpe15020018






