Development of Internalizing Mental Health Symptoms from Early Childhood to Late Adolescence
Abstract
1. Introduction
1.1. Development and Discontinuity in Children’s Internalising Symptoms
1.2. Transitioning to Adolescence as a Turning Point for Internalising Symptoms’ Development
1.3. The Present Study
2. Materials and Method
2.1. Participants and Dataset
2.2. Measures
Internalizing Mental Health Symptoms
2.3. Covariates
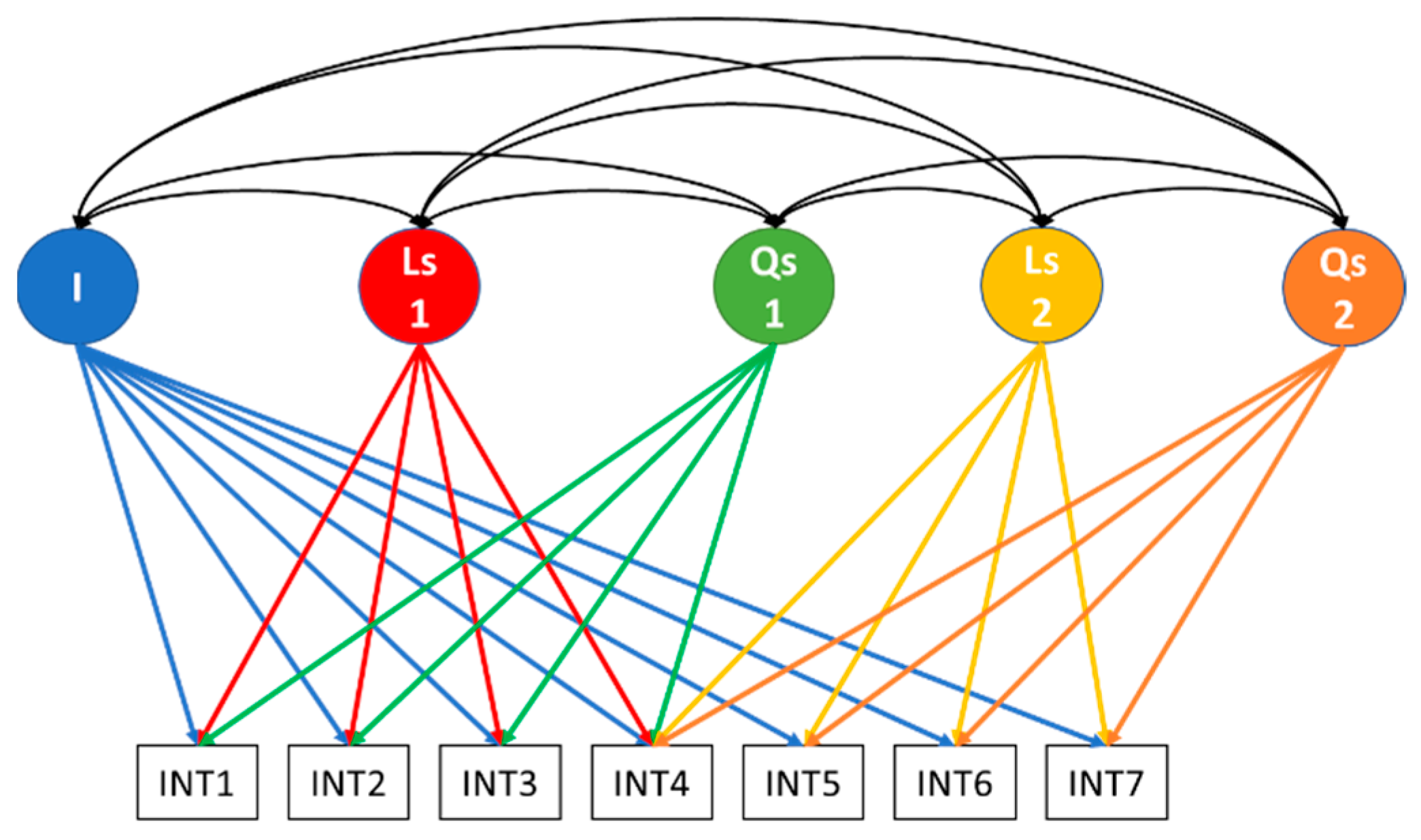
2.4. Statistical Analyses
2.5. Procedure
3. Results
3.1. Missing Data Analysis and Descriptive Statistics
3.2. Longitudinal Measurement Invariance of Internalising Symptoms
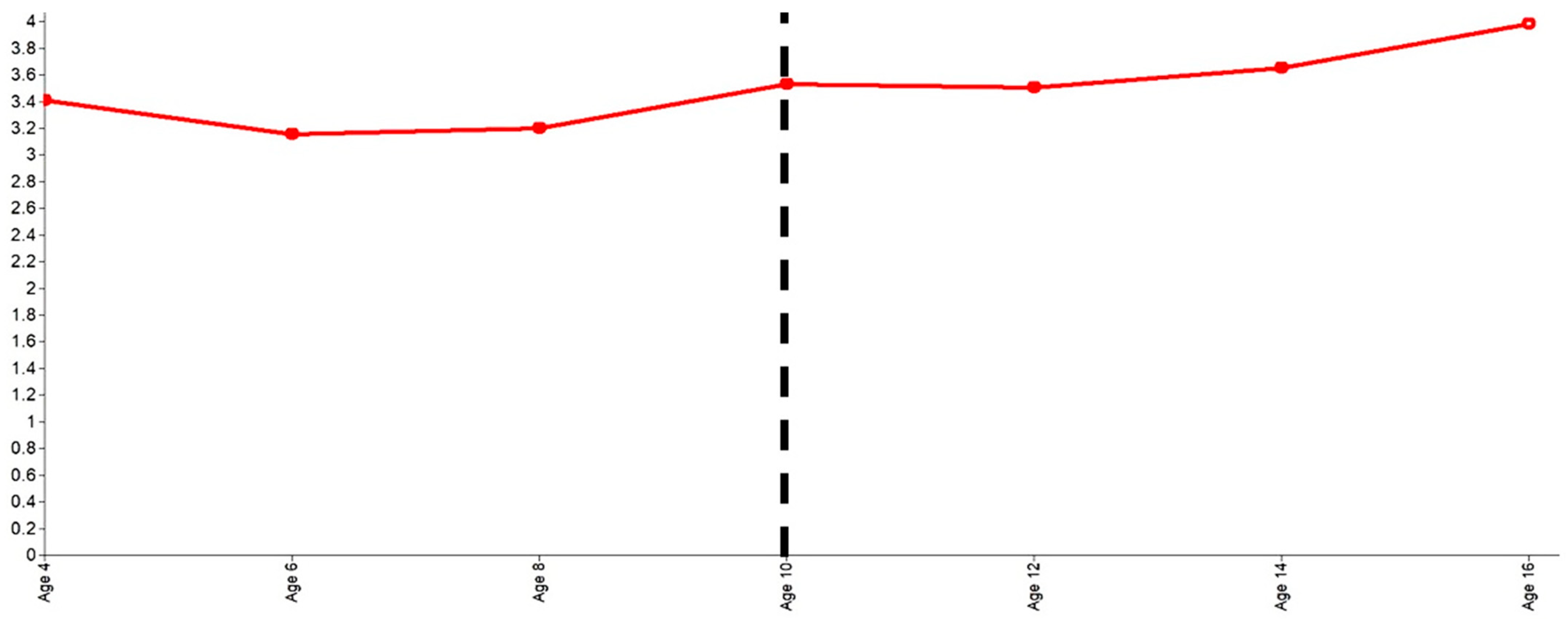
3.3. The Developmental Trajectory of Internalising Symptoms
3.4. Controlling for Standard Demographic Factors
4. Discussion
4.1. Strengths and Limitations
4.2. Future Directions
5. Conclusions
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Armitage, J.M.; Kwong, A.S.F.; Tseliou, F.; Sellers, R.; Blakey, R.; Anthony, R.; Rice, F.; Thapar, A.; Collishaw, S. Cross-Cohort Change in Parent-Reported Emotional Problem Trajectories across Childhood and Adolescence in the UK. Lancet Psychiatry 2023, 10, 509–517. [Google Scholar] [CrossRef] [PubMed]
- Katsantonis, I.; Symonds, J.E. Population Heterogeneity in Developmental Trajectories of Internalising and Externalising Mental Health Symptoms in Childhood: Differential Effects of Parenting Styles. Epidemiol. Psychiatr. Sci. 2023, 32, e16. [Google Scholar] [CrossRef] [PubMed]
- Brumariu, L.E.; Kerns, K.A. Parent–Child Attachment and Internalizing Symptoms in Childhood and Adolescence: A Review of Empirical Findings and Future Directions. Dev. Psychopathol. 2010, 22, 177–203. [Google Scholar] [CrossRef] [PubMed]
- Bor, W.; Dean, A.J.; Najman, J.; Hayatbakhsh, R. Are Child and Adolescent Mental Health Problems Increasing in the 21st Century? A Systematic Review. Aust. N. Z. J. Psychiatry 2014, 48, 606–616. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.R.; Andrews, A.R.; Davis, M.M.; Rudolph, K.D. Anxiety and Depression during Childhood and Adolescence: Testing Theoretical Models of Continuity and Discontinuity. J. Abnorm. Child. Psychol. 2018, 46, 1295–1308. [Google Scholar] [CrossRef] [PubMed]
- Rothenberg, W.A.; Lansford, J.E.; Bornstein, M.H.; Chang, L.; Deater-Deckard, K.; Di Giunta, L.; Dodge, K.A.; Malone, P.S.; Oburu, P.; Pastorelli, C.; et al. Effects of Parental Warmth and Behavioral Control on Adolescent Externalizing and Internalizing Trajectories across Cultures. J. Res. Adolesc. 2020, 30, 835–855. [Google Scholar] [CrossRef]
- Anthony, R.; Moore, G.; Page, N.; Ollerhead, C.; Parker, J.; Murphy, S.; Rice, F.; Armitage, J.M.; Collishaw, S. Trends in Adolescent Emotional Problems in Wales between 2013 and 2019: The Contribution of Peer Relationships. J. Child Psychol. Psychiatry 2024, 65, 887–898. [Google Scholar] [CrossRef] [PubMed]
- Goodman, A.; Lamping, D.L.; Ploubidis, G.B. When to Use Broader Internalising and Externalising Subscales Instead of the Hypothesised Five Subscales on the Strengths and Difficulties Questionnaire (SDQ): Data from British Parents, Teachers and Children. J. Abnorm. Child. Psychol. 2010, 38, 1179–1191. [Google Scholar] [CrossRef]
- Forrest, C.L.; Gibson, J.L.; Halligan, S.L.; St Clair, M.C. A Cross-Lagged Analysis of Emotion Regulation, Peer Problems, and Emotional Problems in Children with and without Early Language Difficulties: Evidence from the Millennium Cohort Study. J. Speech Lang. Hear. Res. 2020, 63, 1227–1239. [Google Scholar] [CrossRef]
- Katsantonis, I. Dynamic Interplay of Developing Internalising and Externalising Mental Health from Early Childhood to Mid-Adolescence: Teasing Apart Trait, State, and Cross-Cohort Effects. PLoS ONE 2024, 19, e0306978. [Google Scholar] [CrossRef]
- McElroy, E.; Belsky, J.; Carragher, N.; Fearon, P.; Patalay, P. Developmental Stability of General and Specific Factors of Psychopathology from Early Childhood to Adolescence: Dynamic Mutualism or p-Differentiation? J. Child Psychol. Psychiatry 2018, 59, 667–675. [Google Scholar] [CrossRef] [PubMed]
- Bayer, J.K.; Hastings, P.D.; Sanson, A.V.; Ukoumunne, O.C.; Rubin, K.H. Predicting Mid-Childhood Internalising Symptoms: A Longitudinal Community Study. Int. J. Ment. Health Promot. 2010, 12, 5–17. [Google Scholar] [CrossRef]
- Murray, A.L.; Eisner, M.; Ribeaud, D. Within-Person Analysis of Developmental Cascades between Externalising and Internalising Problems. J. Child Psychol. Psychiatry 2020, 61, 681–688. [Google Scholar] [CrossRef]
- Flouri, E.; Papachristou, E.; Midouhas, E.; Joshi, H.; Ploubidis, G.B.; Lewis, G. Early Adolescent Outcomes of Joint Developmental Trajectories of Problem Behavior and IQ in Childhood. Eur. Child Adolesc. Psychiatry 2018, 27, 1595–1605. [Google Scholar] [CrossRef]
- Murray, A.L.; Eisner, M.; Nagin, D.; Ribeaud, D. A Multi-Trajectory Analysis of Commonly Co-Occurring Mental Health Issues across Childhood and Adolescence. Eur. Child Adolesc. Psychiatry 2022, 31, 145–159. [Google Scholar] [CrossRef]
- Schulenberg, J.E.; Maggs, J.L.; O’Malley, P.M. How and Why the Understanding of Developmental Continuity and Discontinuity Is Important. In Handbook of the Life Course; Mortimer, J.T., Shanahan, M.J., Eds.; Handbooks of Sociology and Social Research; Springer: Boston, MA, USA, 2003; pp. 413–436. ISBN 978-0-306-48247-2. [Google Scholar]
- Bornstein, M.H.; Putnick, D.L.; Esposito, G. Continuity and Stability in Development. Child Dev. Perspect. 2017, 11, 113–119. [Google Scholar] [CrossRef]
- Rutter, M. Transitions and Turning Points in Developmental Psychopathology: As Applied to the Age Span between Childhood and Mid-Adulthood. Int. J. Behav. Dev. 1996, 19, 603–626. [Google Scholar] [CrossRef]
- Wong, K.K.-Y.; Francesconi, M.; Flouri, E. Internalizing and Externalizing Problems across Childhood and Psychotic-like Experiences in Young-Adulthood: The Role of Developmental Period. Schizophr. Res. 2021, 231, 108–114. [Google Scholar] [CrossRef]
- Graber, J.A.; Brooks-Gunn, J. Transitions and Turning Points: Navigating the Passage from Childhood through Adolescence. Dev. Psychol. 1996, 32, 768–776. [Google Scholar] [CrossRef]
- Zarrella, I.; Russolillo, L.A.; Caviglia, G.; Perrella, R. Continuity and Discontinuity between Psychopathology of Childhood and Adulthood: A Review on Retrospective and Prospective Studies. Res. Psychother. 2017, 20, 248. [Google Scholar] [CrossRef]
- Katsantonis, I.; McLellan, R.; Marquez, J. Development of Subjective Well-being and Its Relationship with Self-esteem in Early Adolescence. Br. J. Dev. Psychol. 2023, 41, 157–171. [Google Scholar] [CrossRef]
- Blakemore, S.-J. Adolescence and Mental Health. Lancet 2019, 393, 2030–2031. [Google Scholar] [CrossRef]
- Sawyer, S.M.; Azzopardi, P.S.; Wickremarathne, D.; Patton, G.C. The Age of Adolescence. Lancet Child Adolesc. Health 2018, 2, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Sawyer, S.M.; Afifi, R.A.; Bearinger, L.H.; Blakemore, S.-J.; Dick, B.; Ezeh, A.C.; Patton, G.C. Adolescence: A Foundation for Future Health. Lancet 2012, 379, 1630–1640. [Google Scholar] [CrossRef]
- Evans, D.; Borriello, G.A.; Field, A.P. A Review of the Academic and Psychological Impact of the Transition to Secondary Education. Front. Psychol. 2018, 9, 1482. [Google Scholar] [CrossRef]
- Kessler, R.C.; Barker, P.R.; Colpe, L.J.; Epstein, J.F.; Gfroerer, J.C.; Hiripi, E.; Howes, M.J.; Normand, S.-L.T.; Manderscheid, R.W.; Walters, E.E.; et al. Screening for Serious Mental Illness in the General Population. Arch. Gen. Psychiatry 2003, 60, 184–189. [Google Scholar] [CrossRef] [PubMed]
- Merikangas, K.R.; Nakamura, E.F.; Kessler, R.C. Epidemiology of Mental Disorders in Children and Adolescents. Dialogues Clin. Neurosci. 2009, 11, 7–20. [Google Scholar] [CrossRef]
- Polanczyk, G.V.; Salum, G.A.; Sugaya, L.S.; Caye, A.; Rohde, L.A. Annual Research Review: A Meta-Analysis of the Worldwide Prevalence of Mental Disorders in Children and Adolescents. J. Child Psychol. Psychiatry 2015, 56, 345–365. [Google Scholar] [CrossRef] [PubMed]
- Barican, J.L.; Yung, D.; Schwartz, C.; Zheng, Y.; Georgiades, K.; Waddell, C. Prevalence of Childhood Mental Disorders in High-Income Countries: A Systematic Review and Meta-Analysis to Inform Policymaking. BMJ Ment. Health 2022, 25, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Mohal, J.; Lansangan, C.; Gasser, C.; Howell, L.; Duffy, J.; Renda, J.; Scovelle, A.; Jessup, K.; Daraganova, G.; Mundy, L. Growing Up in Australia: The Longitudinal Study of Australian Children—Data User Guide, Release 9.0C2, June 2022; Australian Institute of Family Studies: Melbourne, Australia, 2022.
- Katsantonis, I. I Belong; Hence, I Engage? A Cohort Study of Transitions between School Engagement Classes and Academic Achievement: The Role of Relational School Climate. Aust. Educ. Res. 2024. [Google Scholar] [CrossRef]
- Sanson, A.; Nicholson, J.; Ungerer, J.; Zubrick, S.; Wilson, K.; Ainley, J.; Berthelsen, D.; Bittman, M.; Broom, D.; Harrison, L.; et al. (Eds.) Introducing the Longitudinal Study of Australian Children; LSAC Discussion Paper; Australian Institute of Family Studies: Melbourne, Australia, 2002; ISBN 978-0-642-39496-5.
- Heeringa, S.G.; West, B.T.; Berglund, P.A. Applied Survey Data Analysis; Chapman and Hall/CRC: Boca Raton, FL, USA, 2017; ISBN 978-1-315-15327-8. [Google Scholar]
- Goodman, R. The Strengths and Difficulties Questionnaire: A Research Note. J. Child Psychol. Psychiatry 1997, 38, 581–586. [Google Scholar] [CrossRef]
- Goodman, A.; Goodman, R. Population Mean Scores Predict Child Mental Disorder Rates: Validating SDQ Prevalence Estimators in Britain. J. Child Psychol. Psychiatry 2011, 52, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Katsantonis, I.; McLellan, R. The Role of Parent–Child Interactions in the Association between Mental Health and Prosocial Behavior: Evidence from Early Childhood to Late Adolescence. Int. J. Behav. Dev. 2023, 48, 59–70. [Google Scholar] [CrossRef]
- Newsom, J.T. Longitudinal Structural Equation Modeling: A Comprehensive Introduction, 1st ed.; Routledge: New York, NY, USA, 2015; ISBN 978-1-84872-697-0. [Google Scholar]
- Patalay, P.; Moulton, V.; Goodman, A.; Ploubidis, G.B. Cross-Domain Symptom Development Typologies and Their Antecedents: Results from the UK Millennium Cohort Study. J. Am. Acad. Child Adolesc. Psychiatry 2017, 56, 765–776.e2. [Google Scholar] [CrossRef] [PubMed]
- Crosnoe, R. Family-School Connections, Early Learning, and Socioeconomic Inequality in the US. Multidiscip. J. Educ. Res. 2012, 2, 1–36. [Google Scholar] [CrossRef]
- Fakhrunnisak, D.; Patria, B. The Positive Effects of Parents’ Education Level on Children’s Mental Health in Indonesia: A Result of Longitudinal Survey. BMC Public Health 2022, 22, 949. [Google Scholar] [CrossRef]
- Chilcoat, H.D.; Breslau, N.; Anthony, J.C. Potential Barriers to Parent Monitoring: Social Disadvantage, Marital Status, and Maternal Psychiatric Disorder. J. Am. Acad. Child Adolesc. Psychiatry 1996, 35, 1673–1682. [Google Scholar] [CrossRef] [PubMed]
- Downey, D.B.; Cao, R. Number of Siblings and Mental Health among Adolescents: Evidence from the U.S. and China. J. Fam. Issues 2023, 0192513X231220045. [Google Scholar] [CrossRef]
- Liu, J.; Sekine, M.; Tatsuse, T.; Fujimura, Y.; Hamanishi, S.; Zheng, X. Association among Number, Order and Type of Siblings and Adolescent Mental Health at Age 12. Pediatr. Int. 2015, 57, 849–855. [Google Scholar] [CrossRef]
- Bartkowski, J.P.; Xu, X.; Bartkowski, S. Mixed Blessing: The Beneficial and Detrimental Effects of Religion on Child Development among Third-Graders. Religions 2019, 10, 37. [Google Scholar] [CrossRef]
- Liu, Y.; Millsap, R.E.; West, S.G.; Tein, J.; Tanaka, R.; Grimm, K.J. Testing Measurement Invariance in Longitudinal Data with Ordered-Categorical Measures. Psychol. Methods 2017, 22, 486–506. [Google Scholar] [CrossRef] [PubMed]
- Geiser, C.; Lockhart, G. A Comparison of Four Approaches to Account for Method Effects in Latent State–Trait Analyses. Psychol. Methods 2012, 17, 255–283. [Google Scholar] [CrossRef] [PubMed]
- Bollen, K.A.; Curran, P.J. Latent Curve Models: A Structural Equation Perspective; Wiley-Interscience: Hoboken, NJ, USA, 2006. [Google Scholar]
- Flora, D.B. Specifying Piecewise Latent Trajectory Models for Longitudinal Data. Struct. Equ. Model. Multidiscip. J. 2008, 15, 513–533. [Google Scholar] [CrossRef]
- Harring, J.R.; Strazzeri, M.M.; Blozis, S.A. Piecewise Latent Growth Models: Beyond Modeling Linear-Linear Processes. Behav. Res. 2021, 53, 593–608. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 5th ed.; Guilford Press: New York, NY, USA, 2023. [Google Scholar]
- Hu, L.; Bentler, P.M. Cutoff Criteria for Fit Indexes in Covariance Structure Analysis: Conventional Criteria versus New Alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Chen, F.F. Sensitivity of Goodness of Fit Indexes to Lack of Measurement Invariance. Struct. Equ. Model. 2007, 14, 464–504. [Google Scholar] [CrossRef]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide, 8th ed.; Muthén & Muthén: Los Angeles, CA, USA, 2017. [Google Scholar]
- StataCorp. User’s Guide, Release 17; STATA Corporation: College Station, TX, USA, 2021. [Google Scholar]
- Little, R.J.A. A Test of Missing Completely at Random for Multivariate Data with Missing Values. J. Am. Stat. Assoc. 1988, 83, 1198–1202. [Google Scholar] [CrossRef]
- Salmela-Aro, K. Stages of Adolescence. In Encyclopedia of Adolescence; Brown, B.B., Prinstein, M.J., Eds.; Academic Press: San Diego, CA, USA, 2011; pp. 360–368. ISBN 978-0-12-373951-3. [Google Scholar]
| Variable | Descriptive Statistic (Mean, SD or %) |
|---|---|
| Responding parent’s sex (ref: Male) | |
| Female | 97.17% |
| Sex (ref: Male) | |
| Female | 49.10% |
| Parent’s income (ref: lowest category) | |
| $500–$999 pw $26,000–$51,999 per year | 25.6% |
| $1000–$1999 pw $52,000–$103,999 per year | 7.98% |
| $2000 or more per week $104,000 or more per year | 1.01% |
| Language spoken at home by child (ref: not English) | |
| English | 90.8% |
| Highest parental education (ref: not university) | |
| University-level education | 49.90% |
| Parent’s marital status (ref: not married) | |
| Married | 84.01% |
| Parent attending religious services (ref: no) | |
| Yes | 35.49% |
| Number of siblings in household | M = 1.48, SD = 0.99 |
| Internalizing symptoms (age 4) | M = 3.39, SD = 2.69 |
| Internalizing symptoms (age 6) | M = 3.20, SD = 2.78 |
| Internalizing symptoms (age 8) | M = 3.13, SD = 2.90 |
| Internalizing symptoms (age 10) | M = 3.52, SD = 3.19 |
| Internalizing symptoms (age 12) | M = 3.51, SD = 3.12 |
| Internalizing symptoms (age 14) | M = 3.59, SD = 3.16 |
| Internalizing symptoms (age 16) | M = 3.95, SD = 3.45 |
| Invariance Level | Scaled χ2 (df) | CFI | |ΔCFI| | RMSEA | |ΔRMSEA| |
|---|---|---|---|---|---|
| Emotional symptoms | |||||
| Configural | 1599.634 (529) *** | 0.964 | 0.027 | ||
| Metric | 1740.096 (553) *** | 0.960 | 0.004 | 0.028 | 0.001 |
| Scalar | 1696.709 (577) *** | 0.962 | 0.002 | 0.026 | 0.002 |
| Strict | 2022.697 (607) *** | 0.952 | 0.010 | 0.029 | 0.003 |
| Peer problems | |||||
| Configural | 1141.673 (529) *** | 0.970 | 0.020 | ||
| Metric | 1230.926 (553) *** | 0.967 | 0.003 | 0.021 | 0.001 |
| Scalar | 1339.942 (577) *** | 0.963 | 0.004 | 0.022 | 0.001 |
| Strict | 1516.078 (607) *** | 0.956 | 0.007 | 0.023 | 0.001 |
| Trajectory Shape Specification | Scaled χ2 (df) | CFI | TLI | RMSEA | SRMR |
|---|---|---|---|---|---|
| Linear | 313.449 (23) *** | 0.938 | 0.943 | 0.067 | 0.066 |
| Quadratic | 139.758 (19) *** | 0.974 | 0.972 | 0.048 | 0.028 |
| Piecewise linear-linear knot at age 8 | 127.564 (19) *** | 0.977 | 0.974 | 0.045 | 0.028 |
| Piecewise linear-quadratic knot at age 8 | 60.123 (14) *** | 0.990 | 0.985 | 0.034 | 0.019 |
| Piecewise linear-linear knot at age 10 | 146.586 (19) *** | 0.973 | 0.970 | 0.049 | 0.030 |
| Piecewise linear-quadratic knot at age 10 | 109.475 (14) *** | 0.980 | 0.969 | 0.049 | 0.026 |
| Piecewise quadratic-quadratic knot at age 10 | 11.902 (8) ns | 0.999 | 0.998 | 0.013 | 0.009 |
| Piecewise linear-linear knot at age 12 | 175.730 (19) *** | 0.967 | 0.963 | 0.054 | 0.042 |
| Piecewise quadratic-linear knot at age 12 | 66.419 (14) *** | 0.989 | 0.983 | 0.037 | 0.020 |
| Path Specification | Parameter Estimate (S.E.) | Two-Tailed p-Value |
|---|---|---|
| Correlations | ||
| Linear slope 1—Intercept | −0.379 (0.098) | 0.000 |
| Quadratic slope 1—Intercept | 0.315 (0.106) | 0.003 |
| Linear slope 1 –Quadratic slope 1 | −0.922 (0.017) | 0.000 |
| Linear slope 2—Intercept | −0.158 (0.067) | 0.019 |
| Linear slope 1—Linear slope 2 | −0.250 (0.131) | 0.057 |
| Linear slope 2—Quadratic slope 1 | 0.258 (0.204) | 0.205 |
| Quadratic slope 2—Intercept | 0.070 (0.056) | 0.194 |
| Quadratic slope 2—Linear slope 1 | 0.157 (0.088) | 0.072 |
| Quadratic slope 1—Quadratic slope 2 | −0.179 (0.129) | 0.165 |
| Quadratic slope 2—Linear slope 2 | −0.852 (0.027) | 0.000 |
| Latent means (unstandardized) | ||
| Intercept | 3.407 (0.067) | 0.000 |
| Linear slope 1 | −0.198 (0.035) | 0.000 |
| Quadratic slope 1 | 0.036 (0.005) | 0.000 |
| Linear slope 2 | −0.059 (0.034) | 0.086 |
| Quadratic slope 2 | 0.022 (0.006) | 0.000 |
| Latent variances (unstandardized) | ||
| Intercept | 5.247 (0.564) | 0.000 |
| Linear slope 1 | 0.889 (0.177) | 0.000 |
| Quadratic slope 1 | 0.016 (0.003) | 0.000 |
| Linear slope 2 | 0.412 (0.113) | 0.000 |
| Quadratic slope 2 | 0.017 (0.003) | 0.000 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Katsantonis, I.G. Development of Internalizing Mental Health Symptoms from Early Childhood to Late Adolescence. Eur. J. Investig. Health Psychol. Educ. 2024, 14, 2404-2416. https://doi.org/10.3390/ejihpe14080159
Katsantonis IG. Development of Internalizing Mental Health Symptoms from Early Childhood to Late Adolescence. European Journal of Investigation in Health, Psychology and Education. 2024; 14(8):2404-2416. https://doi.org/10.3390/ejihpe14080159
Chicago/Turabian StyleKatsantonis, Ioannis G. 2024. "Development of Internalizing Mental Health Symptoms from Early Childhood to Late Adolescence" European Journal of Investigation in Health, Psychology and Education 14, no. 8: 2404-2416. https://doi.org/10.3390/ejihpe14080159
APA StyleKatsantonis, I. G. (2024). Development of Internalizing Mental Health Symptoms from Early Childhood to Late Adolescence. European Journal of Investigation in Health, Psychology and Education, 14(8), 2404-2416. https://doi.org/10.3390/ejihpe14080159







