The Effects of Nature Exposure Therapies on Stress, Depression, and Anxiety Levels: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Selection Criteria
2.2. Information Resources and Search Strategy
2.3. Study Selection and Data Collection Process
2.4. Risk of Bias
2.5. Strategy for Data Synthesis and Quality of Evidence Assessment
3. Results
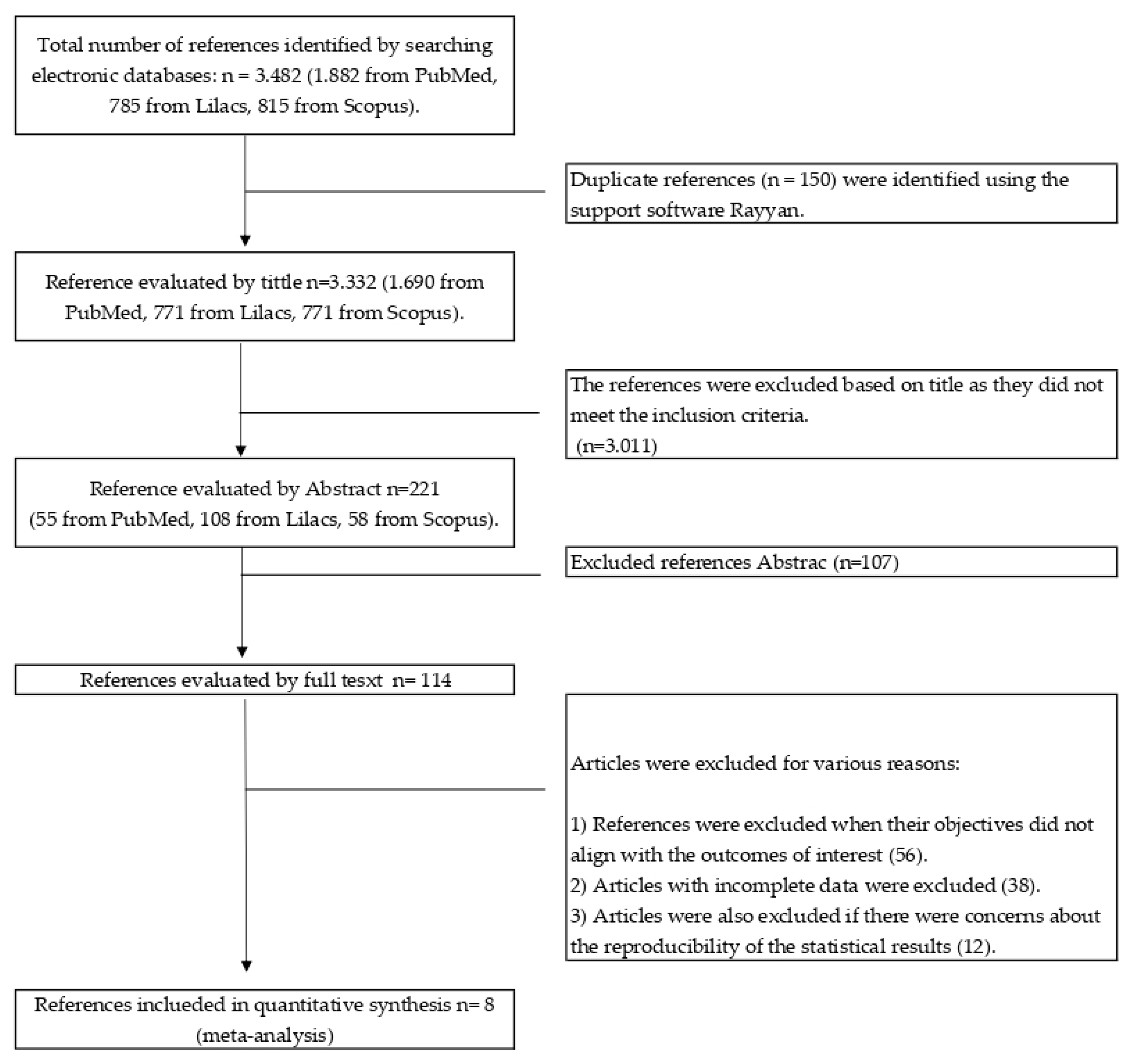
3.1. Search Results
| Reference (Country) | N | Age | Control Group | Intervention Group | Outcomes (Unit) | Duration of the Intervention | Full Description of the Intervention |
|---|---|---|---|---|---|---|---|
| Mean ± SD | |||||||
| Bang et al. [37] (South Korea) | 99 | 24.3 ± 4.19 | No intervention | Nature therapy | Physiological: | 6 weeks | The campus forest-walking program was conducted once per week during lunch. The university campus has many different trees, and there are nearby forest roads and trails. |
| M = 21 | M = 26 | Blood pressure (mm Hg) | |||||
| F = 27 | F = 25 | ||||||
| Bielinis et al. [38] (Poland) | 62 | 21.5 ± 0.18 | City intervention | Nature therapy | Psychological: POMS, PANAS and ROS. | 1 day | The field experiment was winter season. Two locations were selected: the urban and the forest environment (deciduous, broad-leaved urban forest situated near the city centre). |
| M = 18 | M = 18 | ||||||
| F = 13 | F = 13 | ||||||
| Jia et al. [35] (China) | 18 | 61–79 | City intervention | Nature therapy | Physiological: Cortisol (ng/mL) | 7 days | The study was performed at two different sites (nature and city). On the day before the study, blood samples were taken from the participants in the morning before breakfast. |
| M/F = 8 | M/F = 10 | ||||||
| Choe et al. [42] (United Kingdom) | 66 | 16–62 | Indoor environment | Natural environment | Psychological: PANAS | 6 weeks | The study consisted of an experiment of three different environments: natural outdoor, built outdoor, and indoor environments. The intervention was in groups of between 6 and 10 participants. Each weekly session lasted one hour and included mindfulness meditation/exercises and group discussion. |
| M/F = 33 | M/F = 33 | ||||||
| Janeczko et al. [39] (Poland) | 75 | 19–24 | Urban area | Nature therapy | Psychological: POMS, PANAS, and ROS. | 1 day | The outdoor experiment was conducted in four different settings: (1) an urban environment with a noticeably higher level of noise, (2) the scenery of urban housing, (3) the Sobieski Forest, and (4) a coniferous forest. |
| M/F = 45 | M/F = 30 | Physiological: Blood pressure (mmHg). | |||||
| Kim et al. [40] (South Korea) | 38 | 22 | No intervention M/F = 19 | Nature therapy | Psychological: POMS and SRI-MF | 2 months | An eight-session forest therapy program was performed once per week, and each session lasted for 1.5 h. Participants were involved in many activities, such as forest dance, forest meditation, forest exercise, walking, and others. The main purpose of the program was to reduce stress and improve the self-esteem of the participants. |
| M/F = 19 | |||||||
| Kim et al. [41] (Korea) | 38 | 22.1 ± 1.6 | No intervention | Nature therapy | Psychological: POMS and SRI-MF. | 8 weeks | The participants were instructed to perform individualized, voluntary forest activities for a one hour-long session per week. The activities included stretching, breathing, walking, meditation, and exercise. |
| M/F = 19 | M/F = 19 | ||||||
| Razani et al. [36] (United States) | 75 | >18 | Independent park prescription | Supported park prescription | Psychological: PSS10 | 3 weeks | The outdoor experiment was conducted in three different sceneries: a bayfront park with a beach, a lake with woodlands, and a redwood forest. Outings concluded with quiet reflection and an opportunity to share experiences. |
3.2. Risk of Bias
3.3. Physiological Parameters
3.4. Psychological Parameters
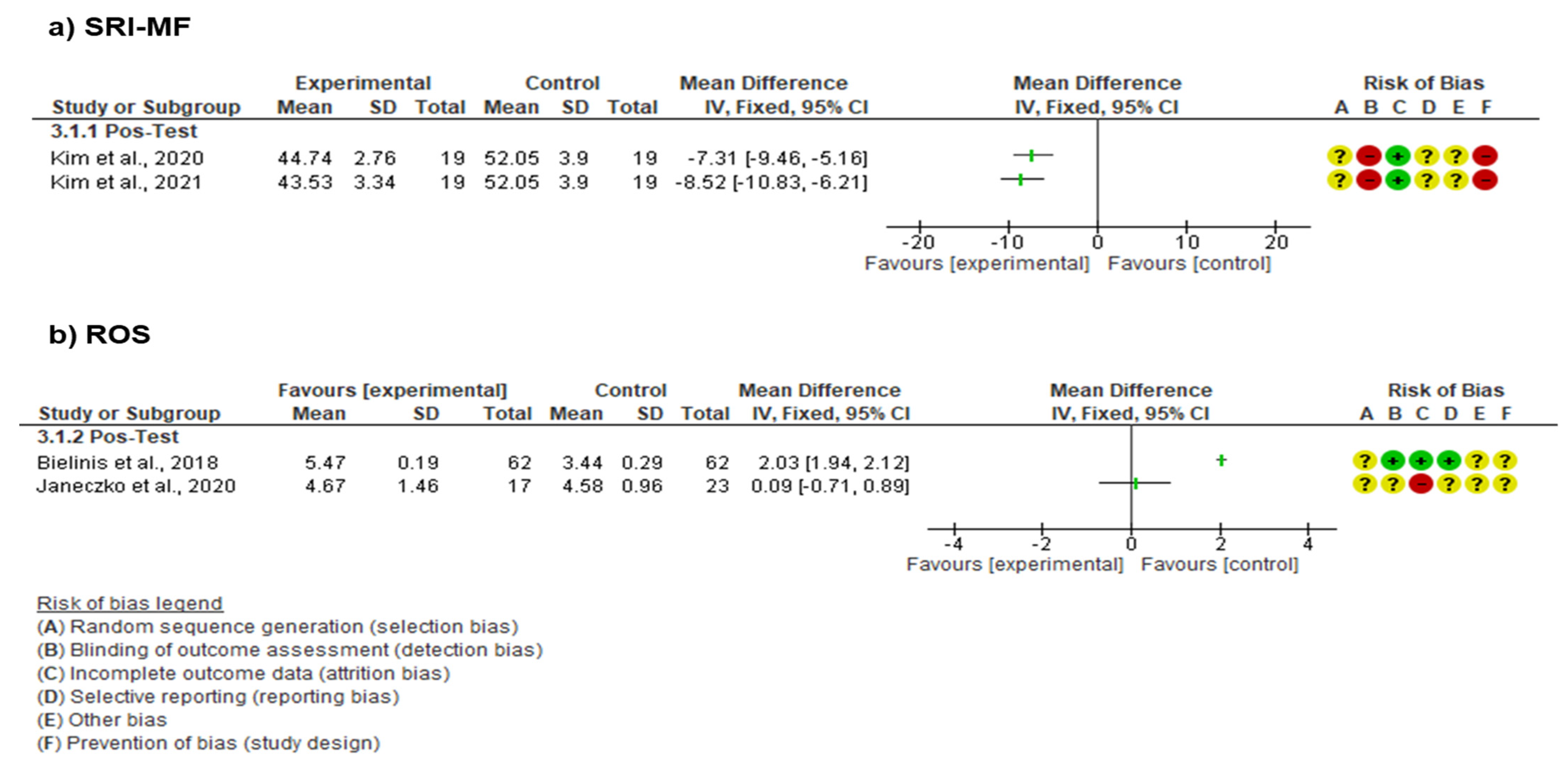
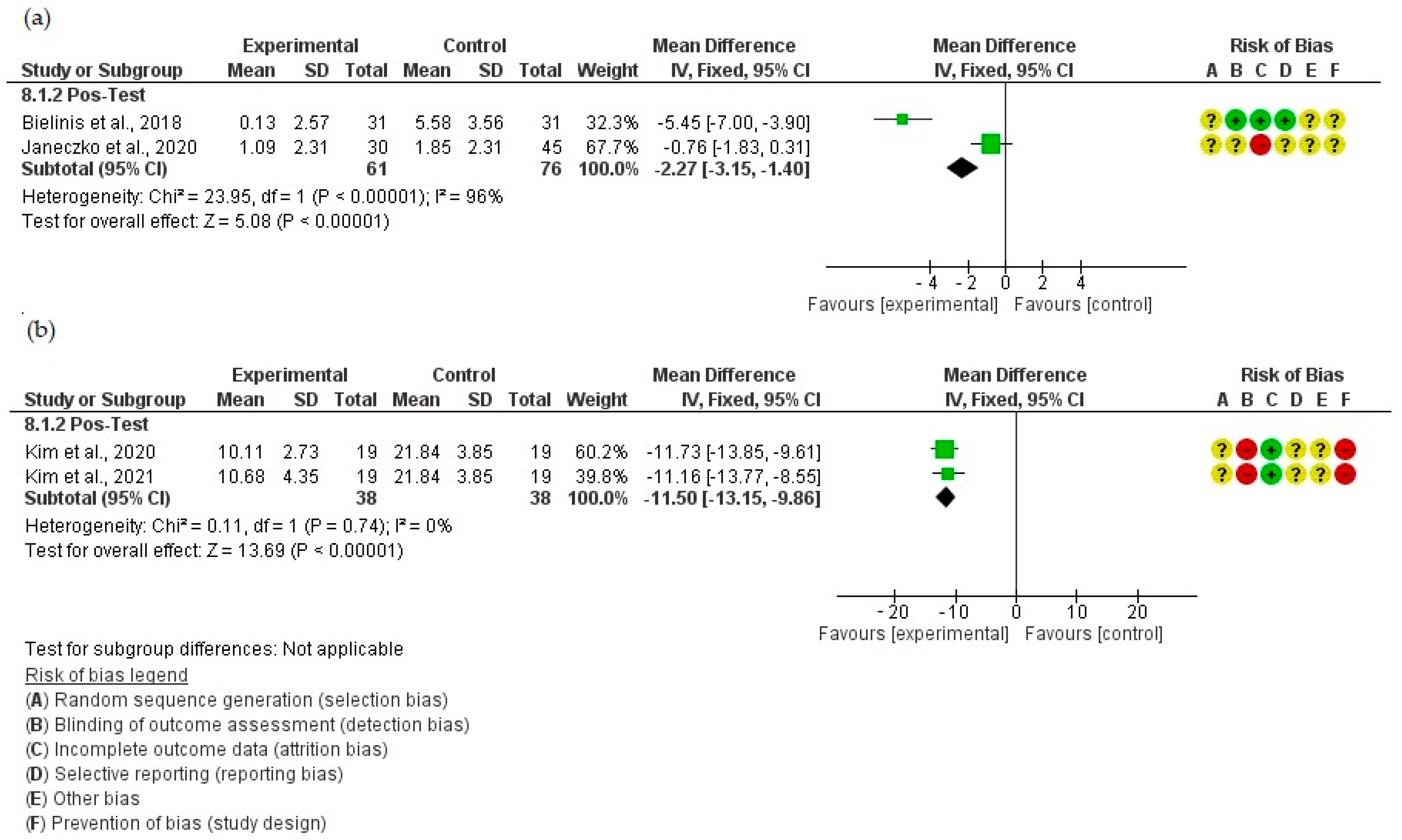
3.4.1. Scales Used to Evaluate Stress
3.4.2. Scales Used to Evaluate Anxiety and Depression
3.4.3. Scales Used to Evaluate Other Psychological Dimensions
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vigo, D.; Thornicroft, G.; Atun, R. Estimating the true global burden of mental illness. Lancet Psychiatry 2016, 3, 171–178. [Google Scholar] [CrossRef]
- Vujcic, M.; Tomicevic-Dubljevic, J.; Grbic, M.; Lecic-Tosevski, D.; Vukovic, O.; Toskovic, O. Nature based solution for improving mental health and well-being in urban areas. Environ. Res. 2017, 158, 385–392. [Google Scholar] [CrossRef]
- Yeshaw, Y.; Mossie, A. Depression, anxiety, stress, and their associated factors among Jimma University staff, Jimma, Southwest Ethiopia, 2016: A cross-sectional study. Neuropsychiatr. Dis. Treat. 2017, 13, 2803–2812. [Google Scholar] [CrossRef]
- World Health Organization. WHO QualityRights Tool Kit: Assessing and Improving Quality and Human Rights in Mental Health and Social Care Facilities; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- Morres, I.D.; Hatzigeorgiadis, A.; Stathi, A.; Comoutos, N.; Arpin-Cribbie, C.; Krommidas, C.; Theodorakis, Y. Aerobic exercise for adult patients with major depressive disorder in mental health services: A systematic review and meta-analysis. Depress. Anxiety 2019, 36, 39–53. [Google Scholar] [CrossRef]
- Dhabhar, F.S. Effects of stress on immune function: The good, the bad, and the beautiful. Immunol. Res. 2014, 58, 193–210. [Google Scholar] [CrossRef]
- Melchior, M.; Caspi, A.; Milne, B.J.; Danese, A.; Poulton, R.; Moffitt, T.E. Work stress precipitates depression and anxiety in young, working women and men. Psychol. Med. 2007, 37, 1119–1129. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W.; Monahan, P.O.; Löwe, B. Anxiety Disorders in Primary Care: Prevalence, Impairment, Comorbidity, and Detection. Ann. Intern. Med. 2007, 146, 317. [Google Scholar] [CrossRef]
- Testa, A.; Giannuzzi, R.; Sollazzo, F.; Petrongolo, L.; Bernardini, L.; Daini, S. Psychiatric emergencies (part I): Psychiatric disorders causing organic symptoms. Eur. Rev. Med. Pharmacol. Sci. 2013, 17 (Suppl. 1), 55–64. [Google Scholar]
- Canuto, A.; Weber, K.; Baertschi, M.; Andreas, S.; Volkert, J.; Dehoust, M.C.; Sehner, S.; Suling, A.; Wegscheider, K.; Ausín, B.; et al. Anxiety Disorders in Old Age: Psychiatric Comorbidities, Quality of Life, and Prevalence According to Age, Gender, and Country. Am. J. Geriatr. Psychiatry 2018, 26, 174–185. [Google Scholar] [CrossRef]
- Lim, P.Y.; Dillon, D.; Chew, P.K.H. A Guide to Nature Immersion: Psychological and Physiological Benefits. Int. J. Environ. Res. Public Health 2020, 17, 5989. [Google Scholar] [CrossRef]
- Hunter, M.R.; Gillespie, B.W.; Chen, S.Y.-P. Urban Nature Experiences Reduce Stress in the Context of Daily Life Based on Salivary Biomarkers. Front. Psychol. 2019, 10, 722. [Google Scholar] [CrossRef]
- Choi, H.; Jeon, Y.-H.; Han, J.-W.; Moon, J.; Kim, S.-Y.; Woo, J.-M. The Effects of a Forest Therapy on Work-Related Stress for Employees in the Manufacturing Industry: Randomized Control Study. Glob. Adv. Health Med. 2022, 11, 2164957X2211004. [Google Scholar] [CrossRef]
- Song, C.; Ikei, H.; Miyazaki, Y. Physiological Effects of Nature Therapy: A Review of the Research in Japan. Int. J. Environ. Res. Public Health 2016, 13, 781. [Google Scholar] [CrossRef]
- Lee, J.; Li, Q.; Tyrvinen, L.; Tsunetsugu, Y.; Park, B.-J.; Kagawa, T.; Miyazaki, Y. Nature Therapy and Preventive Medicine. In Public Health—Social and Behavioral Health; Maddock, J., Ed.; InTech: London, UK, 2012; ISBN 978-953-51-0620-3. [Google Scholar]
- Smyth, N.; Rossi, E.; Wood, C. Effectiveness of stress-relieving strategies in regulating patterns of cortisol secretion and promoting brain health. In International Review of Neurobiology; Elsevier: Amsterdam, The Netherlands, 2020; Volume 150, pp. 219–246. [Google Scholar]
- Ibes, D.; Hirama, I.; Schuyler, C. Greenspace Ecotherapy Interventions: The Stress-Reduction Potential of Green Micro-Breaks Integrating Nature Connection and Mind-Body Skills. Ecopsychology 2018, 10, 137–150. [Google Scholar] [CrossRef]
- Clarke, F.J.; Kotera, Y.; McEwan, K. A Qualitative Study Comparing Mindfulness and Shinrin-Yoku (Forest Bathing): Practitioners’ Perspectives. Sustainability 2021, 13, 6761. [Google Scholar] [CrossRef]
- Selhub, E.M.; Logan, A.C. Your Brain on Nature: The Science of Nature’s Influence on Your Health, Happiness and Vitality; John Wiley & Sons: Mississauga, ON, Canada, 2012; ISBN 978-1-118-10674-7. [Google Scholar]
- Craig, J.M.; Logan, A.C.; Prescott, S.L. Natural environments, nature relatedness and the ecological theater: Connecting satellites and sequencing to shinrin-yoku. J. Physiol. Anthropol. 2016, 35, 1. [Google Scholar] [CrossRef] [PubMed]
- Loureiro, G.; Rabaça, M.A.; Blanco, B.; Andrade, S.; Chieira, C.; Pereira, C. Urban versus rural environment--any differences in aeroallergens sensitization in an allergic population of Cova da Beira, Portugal? Eur. Ann. Allergy Clin. Immunol. 2005, 37, 187–193. [Google Scholar] [PubMed]
- Li, Q. Effect of forest bathing trips on human immune function. Environ. Health Prev. Med. 2010, 15, 9–17. [Google Scholar] [CrossRef]
- Wen, Y.; Yan, Q.; Pan, Y.; Gu, X.; Liu, Y. Medical empirical research on forest bathing (Shinrin-yoku): A systematic review. Environ. Health Prev. Med. 2019, 24, 70. [Google Scholar] [CrossRef]
- Arlt Mutch, V.K.; Evans, S.; Wyka, K. The role of acceptance in mood improvement during Mindfulness-Based Stress Reduction. J. Clin. Psychol. 2021, 77, 7–19. [Google Scholar] [CrossRef]
- Díaz-García, A.; González-Robles, A.; Mor, S.; Mira, A.; Quero, S.; García-Palacios, A.; Baños, R.M.; Botella, C. Positive and Negative Affect Schedule (PANAS): Psychometric properties of the online Spanish version in a clinical sample with emotional disorders. BMC Psychiatry 2020, 20, 56. [Google Scholar] [CrossRef]
- Bielinis, E.; Łukowski, A.; Omelan, A.; Boiko, S.; Takayama, N.; Grebner, D.L. The Effect of Recreation in a Snow-Covered Forest Environment on the Psychological Wellbeing of Young Adults: Randomized Controlled Study. Forests 2019, 10, 827. [Google Scholar] [CrossRef]
- Lee, D.-H.; Park, H.Y.; Lee, U.S.; Lee, K.-J.; Noh, E.C.; Jang, J.H.; Kang, D.-H. The effects of brain wave vibration on oxidative stress response and psychological symptoms. Compr. Psychiatry 2015, 60, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Maund, P.R.; Irvine, K.N.; Reeves, J.; Strong, E.; Cromie, R.; Dallimer, M.; Davies, Z.G. Wetlands for Wellbeing: Piloting a Nature-Based Health Intervention for the Management of Anxiety and Depression. Int. J. Environ. Res. Public Health 2019, 16, 4413. [Google Scholar] [CrossRef]
- Stalder, T.; Lupien, S.J.; Kudielka, B.M.; Adam, E.K.; Pruessner, J.C.; Wüst, S.; Dockray, S.; Smyth, N.; Evans, P.; Kirschbaum, C.; et al. Evaluation and update of the expert consensus guidelines for the assessment of the cortisol awakening response (CAR). Psychoneuroendocrinology 2022, 146, 105946. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gotzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Green, S.; Cochrane Collaboration (Eds.) Cochrane Handbook for Systematic Reviews of Interventions; Cochrane Book Series; Wiley-Blackwell: Chichester, UK; Hoboken, NJ, USA, 2008; ISBN 978-0-470-69951-5. [Google Scholar]
- RevMan. Available online: https://training.cochrane.org/online-learning/core-software/revman (accessed on 7 September 2022).
- Catalá-López, F. Metaanálisis de ensayos clínicos aleatorizados, heterogeneidad e intervalos de predicción. Med. Clin. 2014, 142, 270–274. [Google Scholar] [CrossRef]
- Pértega, S.; Pita, S. Guía: Revisiones Sistemáticas y Metaanálisis (II)—Fisterra. Available online: https://www.fisterra.com/formacion/metodologia-investigacion/revisiones-sistematicas-metaanalisis-ii/ (accessed on 7 September 2022).
- Jia, B.; Yang, Z.; Mao, G.; Lyu, Y.; Wen, X.; Xu, W.; Lyu, X.; Cao, Y.; Wang, G. Health Effect of Forest Bathing Trip on Elderly Patients with Chronic Obstructive Pulmonary Disease. Biomed. Environ. Sci. 2016, 29, 212–218. [Google Scholar]
- Razani, N.; Morshed, S.; Kohn, M.A.; Wells, N.M.; Thompson, D.; Alqassari, M.; Agodi, A.; Rutherford, G.W. Effect of park prescriptions with and without group visits to parks on stress reduction in low-income parents: SHINE randomized trial. PLoS ONE 2018, 13, e0192921. [Google Scholar] [CrossRef]
- Bang, K.-S.; Lee, I.; Kim, S.; Lim, C.S.; Joh, H.-K.; Park, B.-J.; Song, M.K. The Effects of a Campus Forest-Walking Program on Undergraduate and Graduate Students’ Physical and Psychological Health. Int. J. Environ. Res. Public Health 2017, 14, 728. [Google Scholar] [CrossRef]
- Bielinis, E.; Takayama, N.; Boiko, S.; Omelan, A.; Bielinis, L. The effect of winter forest bathing on psychological relaxation of young Polish adults. Urban For. Urban Green. 2018, 29, 276–283. [Google Scholar] [CrossRef]
- Janeczko, E.; Bielinis, E.; Wójcik, R.; Woźnicka, M.; Kędziora, W.; Łukowski, A.; Elsadek, M.; Szyc, K.; Janeczko, K. When Urban Environment Is Restorative: The Effect of Walking in Suburbs and Forests on Psychological and Physiological Relaxation of Young Polish Adults. Forests 2020, 11, 591. [Google Scholar] [CrossRef]
- Kim, J.G.; Khil, T.G.; Lim, Y.; Park, K.; Shin, M.; Shin, W.S. The Psychological Effects of a Campus Forest Therapy Program. Int. J. Environ. Res. Public Health 2020, 17, 3409. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.G.; Jeon, J.; Shin, W.S. The Influence of Forest Activities in a University Campus Forest on Student’s Psychological Effects. Int. J. Environ. Res. Public Health 2021, 18, 2457. [Google Scholar] [CrossRef]
- Choe, E.Y.; Jorgensen, A.; Sheffield, D. Does a natural environment enhance the effectiveness of Mindfulness-Based Stress Reduction (MBSR)? Examining the mental health and wellbeing, and nature connectedness benefits. Landsc. Urban Plan. 2020, 202, 103886. [Google Scholar] [CrossRef]
- Contreras, C.M.; Gutierrez-Garcia, A.G. Cortisol Awakening Response: An Ancient Adaptive Feature. J. Psychiatry Psychiatr. Disord. 2018, 02, 29–40. [Google Scholar] [CrossRef]
- Oh, B.; Lee, K.J.; Zaslawski, C.; Yeung, A.; Rosenthal, D.; Larkey, L.; Back, M. Health and well-being benefits of spending time in forests: Systematic review. Environ. Health Prev. Med. 2017, 22, 71. [Google Scholar] [CrossRef]
- Rajoo, K.S.; Karam, D.S.; Abdullah, M.Z. The physiological and psychosocial effects of forest therapy: A systematic review. Urban For. Urban Green. 2020, 54, 126744. [Google Scholar] [CrossRef]
- Stier-Jarmer, M.; Throner, V.; Kirschneck, M.; Immich, G.; Frisch, D.; Schuh, A. The Psychological and Physical Effects of Forests on Human Health: A Systematic Review of Systematic Reviews and Meta-Analyses. Int. J. Environ. Res. Public Health 2021, 18, 1770. [Google Scholar] [CrossRef] [PubMed]
- Wen, Y.; Gu, X.; Deng, W.; Zou, Q.; Hu, Y.; Yan, Q.; Pan, Y.; Wen, Z.; Wan, R.; Sheng, G.; et al. The Effects of Dynamic and Static Forest Bathing (Shinrin-yoku) on Physiological and Psychological Health in Males and Females. Forests 2023, 14, 1592. [Google Scholar] [CrossRef]
- Kotera, Y.; Richardson, M.; Sheffield, D. Effects of Shinrin-Yoku (Forest Bathing) and Nature Therapy on Mental Health: A Systematic Review and Meta-analysis. Int. J. Ment. Health Addict. 2022, 20, 337–361. [Google Scholar] [CrossRef]
- Zhu, S.; Hu, F.; He, S.; Qiu, Q.; Su, Y.; He, Q.; Li, J. Comprehensive Evaluation of Healthcare Benefits of Different Forest Types: A Case Study in Shimen National Forest Park, China. Forests 2021, 12, 207. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paredes-Céspedes, D.M.; Vélez, N.; Parada-López, A.; Toloza-Pérez, Y.G.; Téllez, E.M.; Portilla, C.; González, C.; Blandón, L.; Santacruz, J.C.; Malagón-Rojas, J. The Effects of Nature Exposure Therapies on Stress, Depression, and Anxiety Levels: A Systematic Review. Eur. J. Investig. Health Psychol. Educ. 2024, 14, 609-622. https://doi.org/10.3390/ejihpe14030040
Paredes-Céspedes DM, Vélez N, Parada-López A, Toloza-Pérez YG, Téllez EM, Portilla C, González C, Blandón L, Santacruz JC, Malagón-Rojas J. The Effects of Nature Exposure Therapies on Stress, Depression, and Anxiety Levels: A Systematic Review. European Journal of Investigation in Health, Psychology and Education. 2024; 14(3):609-622. https://doi.org/10.3390/ejihpe14030040
Chicago/Turabian StyleParedes-Céspedes, Diana Marcela, Norida Vélez, Alejandra Parada-López, Yesith Guillermo Toloza-Pérez, Eliana M. Téllez, Claudia Portilla, Carolina González, Leany Blandón, Juan Carlos Santacruz, and Jeadran Malagón-Rojas. 2024. "The Effects of Nature Exposure Therapies on Stress, Depression, and Anxiety Levels: A Systematic Review" European Journal of Investigation in Health, Psychology and Education 14, no. 3: 609-622. https://doi.org/10.3390/ejihpe14030040
APA StyleParedes-Céspedes, D. M., Vélez, N., Parada-López, A., Toloza-Pérez, Y. G., Téllez, E. M., Portilla, C., González, C., Blandón, L., Santacruz, J. C., & Malagón-Rojas, J. (2024). The Effects of Nature Exposure Therapies on Stress, Depression, and Anxiety Levels: A Systematic Review. European Journal of Investigation in Health, Psychology and Education, 14(3), 609-622. https://doi.org/10.3390/ejihpe14030040