The Impact of Wearing Different Face Masks on Vigorous Physical Exercise Performance and Perceived Exertion among COVID-19 Infected vs. Uninfected Female Students
Abstract
:1. Introduction
2. Materials and Methods
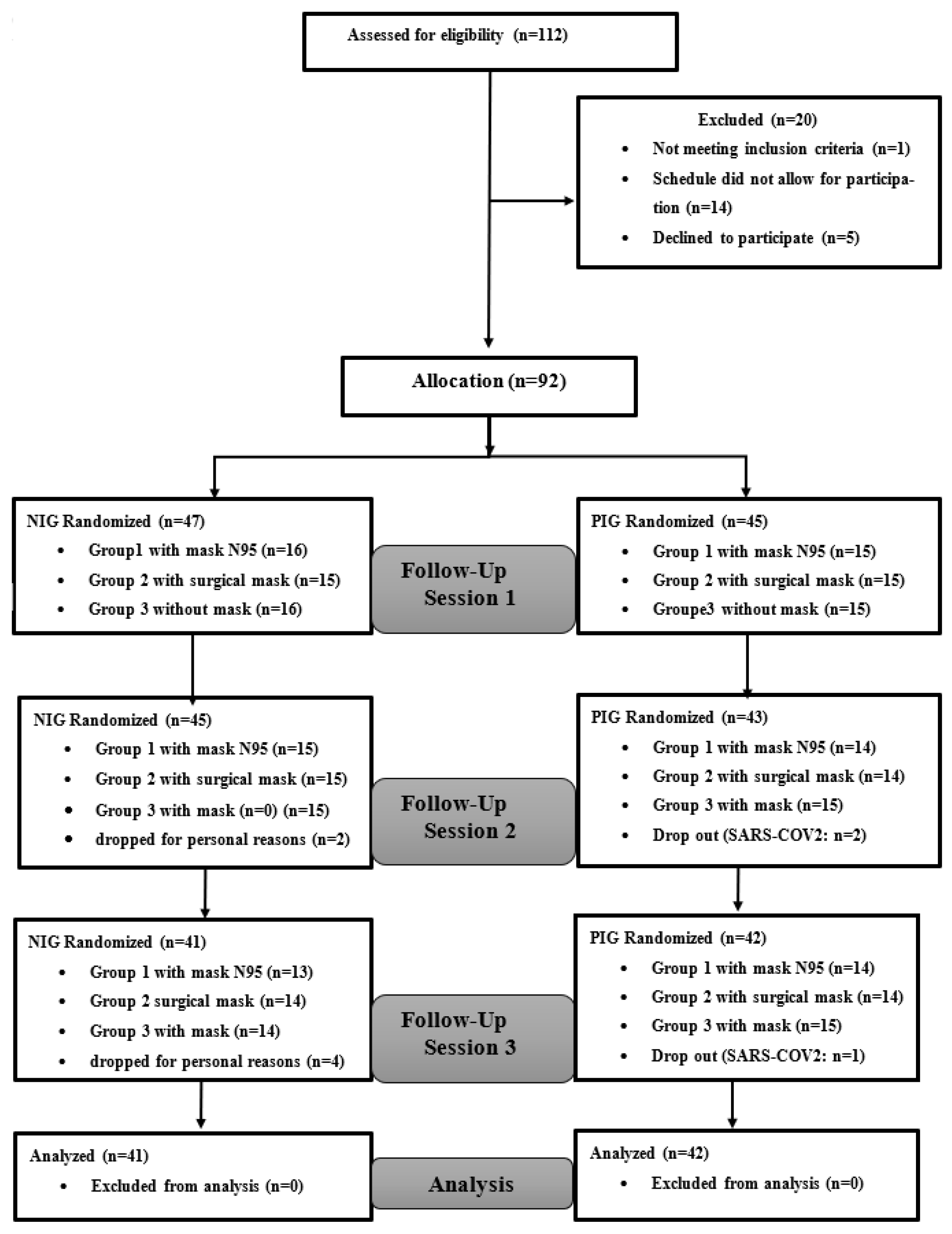
2.1. Participants
2.2. Experimental Design
2.2.1. 5 m Shuttle Run Test (5mSRT)
- BD (m) = the greatest distance covered during a 30 s shuttle,
- TD (m) = total distance covered during the six 30 s shuttles,
- FI (%) was calculated as follows:
2.2.2. Rating of Perceived Exertion (RPE) Scale
2.2.3. International Physical Activity Questionnaire Short Form (IPAQ-SF)
2.2.4. Sleep-Related Measures
2.3. Statistical Analyses
3. Results
3.1. Participant Characteristics
3.2. 5 m Shuttle Run Test and RPE
3.3. Sleep Parameters
3.4. Physical Activity Behaviors
4. Discussion
Limitations of the Study
5. Practical Recommendation
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. WHO Coronavirus (COVID-19) Dashboard. 2023. Available online: https://covid19.who.int/ (accessed on 1 September 2023).
- Davis, H.E.; McCorkell, L.; Vogel, J.M.; Topol, E.J. Long COVID: Major findings, mechanisms and recommendations. Nat. Rev. Microbiol. 2023, 21, 133–146. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Xu, E.; Bowe, B.; Al-Aly, Z. Long-term cardiovascular outcomes of COVID-19. Nat. Med. 2022, 28, 583–590. [Google Scholar] [CrossRef]
- Seeßle, J.; Waterboer, T.; Hippchen, T.; Simon, J.; Kirchner, M.; Lim, A.; Müller, B.; Merle, U. Persistent symptoms in adult patients 1 year after coronavirus disease 2019 (COVID-19): A prospective cohort study. Clin. Infect. Dis. 2022, 74, 1191–1198. [Google Scholar] [CrossRef] [PubMed]
- Demko, Z.O.; Yu, T.; Mullapudi, S.K.; Varela Heslin, M.G.; Dorsey, C.A.; Payton, C.B.; Tornheim, J.A.; Blair, P.W.; Mehta, S.H.; Thomas, D.L.; et al. Post-acute sequelae of SARS-CoV-2 (PASC) impact quality of life at 6, 12 and 18 months post-infection. medRxiv 2022, 22278543. [Google Scholar] [CrossRef]
- Bai, F.; Tomasoni, D.; Falcinella, C.; Barbanotti, D.; Castoldi, R.; Mulè, G.; Augello, M.; Mondatore, D.; Allegrini, M.; Cona, A.; et al. Female gender is associated with long COVID syndrome: A prospective cohort study. Clin. Microbiol. Infect. 2022, 28, 611.e9–611.e16. [Google Scholar] [CrossRef] [PubMed]
- Organisation des Nations Unies (ONU). COVID-19: L’OMS S’attend à un Hiver Difficile. Available online: https://news.un.org/fr/story/2022/09/1126272 (accessed on 25 September 2022).
- Chu, D.K.; Akl, E.A.; Duda, S.; Solo, K.; Yaacoub, S.; Schünemann, H.J.; COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. Lancet 2020, 395, 1973–1987. [Google Scholar] [CrossRef]
- Hopkins, S.R.; Dominelli, P.B.; Davis, C.K.; Guenette, J.A.; Luks, A.M.; Molgat-Seon, Y.; Sá, R.C.; Sheel, A.W.; Swenson, E.R.; Stickland, M.K. Face masks and the cardiorespiratory response to physical activity in health and disease. Ann. Am. Thorac. Soc. 2021, 18, 399–407. [Google Scholar] [CrossRef]
- Matuschek, C.; Moll, F.; Fangerau, H.; Fischer, J.C.; Zänker, K.; Van Griensven, M.; Schneider, M.; Kindgen-Milles, D.; Knoefel, W.T.; Lichtenberg, A.; et al. Face Masks: Benefits and risks during the COVID-19 crisis. Eur. J. Med. Res. 2020, 25, 32. [Google Scholar] [CrossRef]
- Shaw, K.A.; Zello, G.A.; Butcher, S.J.; Ko, J.B.; Bertrand, L.; Chilibeck, P.D. The impact of face masks on performance and physiological outcomes during exercise: A systematic review and meta-analysis. Appl. Physiol. Nutr. Metab. 2021, 46, 693–703. [Google Scholar] [CrossRef]
- O’Kelly, E.; Arora, A.; Pirog, S.; Ward, J.; Clarkson, P.J. Comparing the fit of N95, KN95, surgical, and cloth face masks and assessing the accuracy of fit checking. PLoS ONE 2021, 16, e0245688. [Google Scholar] [CrossRef]
- Barycka, K.; Szarpak, L.; Filipiak, K.J.; Jaguszewski, M.; Smereka, J.; Ladny, J.R.; Turan, O. Comparative effectiveness of N95 respirators and surgical/face masks in preventing airborne infections in the era of SARS-CoV2 pandemic: A meta-analysis of randomized trials. PLoS ONE 2020, 15, e0242901. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Chen, T.; Li, Z.; Tan, Q.; Meng, Z.; Qiu, H.; Liu, X.; Zheng, J. Comparison of filtration efficiency and respiratory resistance of COVID-19 protective masks by multi-national standards. Am. J. Infect. Control 2022, 50, 516–524. [Google Scholar] [CrossRef] [PubMed]
- Zangmeister, C.D.; Radney, J.G.; Vicenzi, E.P.; Weaver, J.L. Filtration efficiencies of nanoscale aerosol by cloth mask materials used to slow the spread of SARS-CoV-2. ACS Nano 2020, 14, 9188–9200. [Google Scholar] [CrossRef] [PubMed]
- Grande, A.J.; Keogh, J.; Silva, V.; Scott, A.M. Exercise versus no exercise for the occurrence, severity, and duration of acute respiratory infections. Cochrane Database Syst. Rev. 2020, 4, CD010596. [Google Scholar] [CrossRef] [PubMed]
- Dixit, S. Can moderate intensity aerobic exercise be an effective and valuable therapy in preventing and controlling the pandemic of COVID-19? Med. Hypotheses 2020, 143, 109854. [Google Scholar] [CrossRef] [PubMed]
- Baker, F.L.; Smith, K.A.; Zúñiga, T.M.; Batatinha, H.; Niemiro, G.M.; Pedlar, C.R.; Burgess, S.C.; Katsanis, E.; Simpson, R.J. Acute exercise increases immune responses to SARS CoV-2 in a previously infected man. Brain Behav. Immun. Health 2021, 18, 100343. [Google Scholar] [CrossRef]
- Jimeno-Almazán, A.; Pallarés, J.G.; Buendía-Romero, Á.; Martínez-Cava, A.; Franco-López, F.; Sánchez-Alcaraz Martínez, B.J.; Bernal-Morel, E.; Courel-Ibáñez, J. Post-COVID-19 syndrome and the potential benefits of exercise. Int. J. Environ. Res. Public Health 2021, 18, 5329. [Google Scholar] [CrossRef]
- Nishiga, M.; Wang, D.W.; Han, Y.; Lewis, D.B.; Wu, J.C. COVID-19 and cardiovascular disease: From basic mechanisms to clinical perspectives. Nat. Rev. Cardiol. 2020, 17, 543–558. [Google Scholar] [CrossRef]
- Shaw, K.A.; Butcher, S.; Ko, J.B.; Absher, A.; Gordon, J.; Tkachuk, C.; Zello, G.A.; Chilibeck, P.D. Wearing a surgical face mask has minimal effect on performance and physiological measures during high-intensity exercise in youth ice-hockey players: A randomized cross-over trial. Int. J. Environ. Res. Public Health 2021, 18, 10766. [Google Scholar] [CrossRef]
- Valenzuela, P.L.; Simpson, R.J.; Castillo-García, A.; Lucia, A. Physical activity: A coadjuvant treatment to covid-19 vaccination? Brain Behav. Immun. 2021, 94, 1–3. [Google Scholar] [CrossRef]
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: Results of the ECLB-COVID-19 international online survey. Nutrients 2020, 12, 1583. [Google Scholar] [CrossRef]
- Wahl, P.; Bloch, W.; Proschinger, S. The molecular signature of high-intensity training in the human body. Int. J. Sports Med. 2022, 43, 195–205. [Google Scholar] [CrossRef]
- Jones, N.R.; Qureshi, Z.U.; Temple, R.J.; Larwood, J.P.J.; Greenhalgh, T.; Bourouiba, L. Two metres or one: What is the evidence for physical distancing in covid-19? BMJ 2020, 370, m3223. [Google Scholar] [CrossRef] [PubMed]
- Atrubin, D.; Wiese, M.; Bohinc, B. An Outbreak of COVID-19 associated with a recreational hockey game—Florida, June 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1492–1493. [Google Scholar] [CrossRef] [PubMed]
- Jang, S.; Han, S.H.; Rhee, J.Y. Cluster of coronavirus disease associated with fitness dance classes, South Korea. Emerg. Infect. Dis. 2020, 26, 1917–1920. [Google Scholar] [CrossRef]
- Lendacki, F.R.; Teran, R.A.; Gretsch, S.; Fricchione, M.J.; Kerins, J.L. COVID-19 outbreak among attendees of an exercise facility—Chicago, Illinois, August-September 2020. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 321–325. [Google Scholar] [CrossRef] [PubMed]
- Slimani, M.; Miarka, B.; Znazen, H.; Moalla, W.; Hammami, A.; Paravlic, A.; Bragazzi, N.L. Effect of a Warm-Up protocol with and without facemask-use against COVID-19 on cognitive function: A pilot, randomized counterbalanced, cross-sectional study. Int. J. Environ. Res. Public Health 2021, 18, 5885. [Google Scholar] [CrossRef]
- Chandrasekaran, B.; Fernandes, S. “Exercise with facemask; are we handling a devil's sword?”—A physiological hypothesis. Med. Hypotheses 2020, 144, 110002. [Google Scholar] [CrossRef]
- Epstein, D.; Korytny, A.; Isenberg, Y.; Marcusohn, E.; Zukermann, R.; Bishop, B.; Minha, S.; Raz, A.; Miller, A. Return to training in the COVID-19 era: The physiological effects of face masks during exercise. Scand. J. Med. Sci. Sports 2021, 31, 70–75. [Google Scholar] [CrossRef]
- Do Prado, D.M.L.; Silvino, V.O.; Motta-Santos, D.; Dos Santos, M.A.P. The effect of the protective face mask on cardiorespiratory response during aerobic exercise. Clin. Exp. Pharmacol. Physiol. 2022, 49, 453–461. [Google Scholar] [CrossRef]
- Fikenzer, S.; Uhe, T.; Lavall, D.; Rudolph, U.; Falz, R.; Busse, M.; Hepp, P.; Laufs, U. Effects of surgical and FFP2/N95 face masks on cardiopulmonary exercise capacity. Clin. Res. Cardiol. 2020, 109, 1598–1599. [Google Scholar] [CrossRef] [PubMed]
- Boukhris, O.; Abdessalem, R.; Ammar, A.; Hsouna, H.; Trabelsi, K.; Engel, F.A.; Sperlich, B.; Hill, D.W.; Chtourou, H. Nap Opportunity during the daytime affects performance and perceived exertion in 5-m shuttle run test. Front. Physiol. 2019, 10, 779. [Google Scholar] [CrossRef] [PubMed]
- Waterhouse, J.; Atkinson, G.; Edwards, B.; Reilly, T. The role of a short post-lunch nap in improving cognitive, motor, and sprint performance in participants with partial sleep deprivation. J. Sports Sci. 2007, 25, 1557–1566. [Google Scholar] [CrossRef] [PubMed]
- Boukhris, O.; Trabelsi, K.; Hill, D.W.; Hsouna, H.; Abdessalem, R.; Ammar, A.; Hammouda, O.; Clark, C.C.T.; Zmijewski, P.; Duking, P.; et al. Physiological response and physical performance after 40 min and 90 min daytime nap opportunities. Res. Sports Med. 2022, 31, 881–894. [Google Scholar] [CrossRef]
- Boddington, M.K.; Lambert, M.I.; Gibson, A.S.C.; Noakes, T.D. Reliability of a 5-m multiple shuttle test. J. Sports Sci. 2001, 19, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Boukhris, O.; Trabelsi, K.; Abdessalem, R.; Hsouna, H.; Ammar, A.; Glenn, J.M.; Bott, N.; Irandoust, K.; Taheri, M.; Turki, M.; et al. Effects of the 5-m shuttle run test on markers of muscle damage, inflammation, and fatigue in healthy male athletes. Int. J. Environ. Res. Public Health 2020, 17, 4375. [Google Scholar] [CrossRef] [PubMed]
- Haddad, M.; Chaouachi, A.; Castagna, C.; Hue, O.; Wong, D.P.; Tabben, M.; Behm, D.G.; Chamari, K. Validity and psychometric evaluation of the French version of RPE Scale in young fit males when monitoring training loads. Sci. Sports 2013, 28, e29–e35. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.L.F.; Yngve, A.; Sallis, J.F. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.H.; Stewart, S.M. Validity of the international physical activity questionnaire short form (PAQ-SF): A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef]
- Clark-Carter, D. The account taken of statistical power in research published in the British Journal of Psychology. Br. J. Psychol. 1997, 88, 71–83. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Shaw, K.; Butcher, S.; Ko, J.; Zello, G.A.; Chilibeck, P.D. Wearing of cloth or disposable surgical face masks has no effect on vigorous exercise performance in healthy individuals. Int. J. Environ. Res. Public Health 2020, 17, 8110. [Google Scholar] [CrossRef] [PubMed]
- Vonbank, K.; Lehmann, A.; Bernitzky, D.; Gysan, M.R.; Simon, S.; Schrott, A.; Burtscher, M.; Idzko, M.; Gompelmann, D. Predictors of prolonged cardiopulmonary exercise impairment after covid-19 infection: A prospective observational study. Front. Med. 2021, 8, 773788. [Google Scholar] [CrossRef] [PubMed]
- Driver, S.; Reynolds, M.; Brown, K.; Vingren, J.L.; Hill, D.W.; Bennett, M.; Gilliland, T.; McShan, E.; Callender, L.; Reynolds, E.; et al. Effects of wearing a cloth face mask on performance, physiological and perceptual responses during a graded treadmill running exercise test. Br. J. Sports Med. 2022, 56, 107–113. [Google Scholar] [CrossRef]
- Wong, A.Y.Y.; Ling, S.K.K.; Louie, L.H.T.; Law, G.Y.K.; So, R.C.H.; Lee, D.C.W.; Yau, F.C.F.; Yung, P.S.H. Impact of the COVID-19 Pandemic on Sports and Exercise. Asia-Pac. J. Sports Med. Arthrosc. Rehabil. Technol. 2020, 22, 39–44. [Google Scholar] [CrossRef]
- Steinbeis, F.; Knape, P.; Mittermaier, M.; Helbig, E.T.; Tober-Lau, P.; Thibeault, C.; Lippert, L.J.; Xiang, W.; Müller-Plathe, M.; Steinbrecher, S.; et al. Functional limitations 12 months after SARS-CoV-2 infection correlate with initial disease severity: An observational study of cardiopulmonary exercise capacity testing in COVID-19 convalescents. Respir. Med. 2022, 202, 106968. [Google Scholar] [CrossRef] [PubMed]
- Debeaumont, D.; Boujibar, F.; Ferrand-Devouge, E.; Artaud-Macari, E.; Tamion, F.; Gravier, F.E.; Smondack, P.; Cuvelier, A.; Muir, J.F.; Alexandre, K.; et al. Cardiopulmonary exercise testing to assess persistent symptoms at 6 months in people with COVID-19 who survived hospitalization: A pilot study. Phys. Ther. 2021, 101, pzab099. [Google Scholar] [CrossRef]
- Dorelli, G.; Braggio, M.; Gabbiani, D.; Busti, F.; Caminati, M.; Senna, G.; Girelli, D.; Laveneziana, P.; Ferrari, M.; Sartori, G.; et al. Importance of cardiopulmonary exercise testing amongst subjects recovering from COVID-19. Diagnostics 2021, 11, 507. [Google Scholar] [CrossRef]
- Skjørten, I.; Ankerstjerne, O.A.W.; Trebinjac, D.; Brønstad, E.; Rasch-Halvorsen, Ø.; Einvik, G.; Lerum, T.V.; Stavem, K.; Edvardsen, A.; Ingul, C.B. Cardiopulmonary exercise capacity and limitations 3 months after COVID-19 hospitalisation. Eur. Respir. J. 2021, 58, 2100996. [Google Scholar] [CrossRef]
- Barbagelata, L.; Masson, W.; Iglesias, D.; Lillo, E.; Migone, J.F.; Orazi, M.L.; Maritano Furcada, J. Cardiopulmonary exercise testing in patients with post-COVID-19 syndrome. Med. Clin. 2022, 159, 6–11. [Google Scholar] [CrossRef]
- Aparisi, Á.; Ybarra-Falcón, C.; García-Gómez, M.; Tobar, J.; Iglesias-Echeverría, C.; Jaurrieta-Largo, S.; Ladrón, R.; Uribarri, A.; Catalá, P.; Hinojosa, W.; et al. Exercise ventilatory inefficiency in post-COVID-19 syndrome: Insights from a prospective evaluation. J. Clin. Med. 2021, 10, 2591. [Google Scholar] [CrossRef] [PubMed]
- Johnsen, S.; Sattler, S.M.; Miskowiak, K.W.; Kunalan, K.; Victor, A.; Pedersen, L.; Andreassen, H.F.; Jørgensen, B.J.; Heebøll, H.; Andersen, M.B.; et al. Descriptive analysis of long COVID sequelae identified in a multidisciplinary clinic serving hospitalised and non-hospitalised patients. ERJ Open Res. 2021, 7, 00205–2021. [Google Scholar] [CrossRef] [PubMed]
- Salati, H.; Khamooshi, M.; Vahaji, S.; Christo, F.C.; Fletcher, D.F.; Inthavong, K. N95 respirator mask breathing leads to excessive carbon dioxide inhalation and reduced heat transfer in a human nasal cavity. Phys. Fluids 2021, 33, 081913. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Tokura, H.; Guo, Y.P.; Wong, A.S.; Wong, T.; Chung, J.; Newton, E. Effects of wearing N95 and surgical facemasks on heart rate, thermal stress, and subjective sensations. Int. Arch. Occup. Environ. Health 2005, 78, 501–509. [Google Scholar] [CrossRef]
- Sinkule, E.J.; Powell, J.B.; Goss, F.L. Evaluation of N95 respirator use with a surgical mask cover: Effects on breathing resistance and inhaled carbon dioxide. Ann. Occup. Hyg. 2013, 57, 384–398. [Google Scholar] [CrossRef]
- Geiss, O. Effect of wearing face masks on the carbon dioxide concentration in the breathing zone. Aerosol Air Qual. Res. 2021, 21, 200403. [Google Scholar] [CrossRef]
| Parameters | Means ± SD | Groups Effect | Mask Effect | Groups × Mask Interaction | |||
|---|---|---|---|---|---|---|---|
| NIG (N = 41) | PIG (N = 42) | All Groups (N = 83) | F(1,81), p-Value, ηp2 | F(1,81), p-Value, ηp2 | F(1,81), p-Value, ηp2 | ||
| BD (m) | Without mask | 100.4 ± 11.5 | 100.8 ± 18.9 | 100.6 ± 15.6 | F(1,81) = 1.512, p = 0.222, ηp2 = 0.018 | F(1,81) = 2.072, p = 0.129, ηp2 = 0.025 | F(1,81) = 1.204, p = 0.303, ηp2 = 0.015 |
| With surgical mask | 101.2 ± 12.3 | 119.9 ± 97.6 | 110.6 ± 69.4 | ||||
| With mask N95 | 98.3 ± 12.2 | 99.2 ± 12.1 | 98.7 ± 12.1 | ||||
| TD (m) | Without mask | 501.1 ± 73.6 | 522 ± 106.8 | 511.6 ± 91.4 | F(1,81) = 1.061, p = 0.306, ηp2 = 0.013 | F(1,81) = 0.794, p = 0.454, ηp2 = 0.010 | F(1,81) = 3.566, p = 0.031, ηp2 = 0.042 |
| With surgical mask | 520.2 ± 95.7 | 479.2 ± 120.3 ab | 499.7 ± 109 | ||||
| With mask N95 | 516 ± 62.7 | 516.5 ± 77.2 c | 516.2 ± 69.8 | ||||
| FI (%) | Without mask | 0.22 ± 0.23 | 0.18 ± 0.32 | 0.2 ± 0.28 | F(1,81) = 1.997, p = 0.161, ηp2 = 0.024 | F(1,81) = 2.586, p = 0.078, ηp2 = 0.031 | F(1,81) = 2.086, p = 0.128, ηp2 = 0.025 |
| With surgical mask | 0.2 ± 0.27 | 0.28 ± 0.29 | 0.24 ± 0.28 | ||||
| With mask N95 | 0.16 ± 0.09 | 0.17 ± 0.22 | 0.17 ± 0.17 | ||||
| PD (%) | Without mask | 0.12 ± 0.07 | 0.42 ± 1.87 | 0.27 ± 1.33 | F(1,81) = 2.660, p = 0.107, ηp2 = 0.032 | F(1,81) = 0.153, p = 0.858, ηp2 = 0.002 | F(1,81) = 0.156, p = 0.856, ηp2 = 0.002 |
| With surgical mask | 0.11 ± 0.05 | 0.36 ± 1.63 | 0.24 ± 1.14 | ||||
| With mask N95 | 0.12 ± 0.06 | 0.24 ± 0.84 | 0.18 ± 0.59 | ||||
| RPE (a. u.) | Without mask | 5.4 ± 1.81 | 5.11 ± 1.7 | 5.25 ± 1.76 | F(1,81) = 1.524, p = 0.221, ηp2 = 0.018 | F(1,81) = 0.901, p = 0.408, ηp2 = 0.011 | F(1,81) = 0.932, p = 0.396, ηp2 = 0.011 |
| With surgical mask | 5.18 ± 1.76 | 5.08 ± 1.6 | 5.13 ± 1.68 | ||||
| With mask N95 | 5.35 ± 1.77 | 4.67 ± 1.64 | 5.01 ± 1.73 | ||||
| Parameters | Means ± SD | Groups Effect | Mask Effect | Groups × Mask Interaction | |||
|---|---|---|---|---|---|---|---|
| NIG (N = 41) | PIG (N = 42) | All Groups (N = 83) | F(1,81), p-Value, ηp2 | F(1,81), p-Value, ηp2 | F(1,81), p-Value, ηp2 | ||
| Sleeping hours last night (hours) | Without mask | 4.89 ± 2.99 | 5.32 ± 3.01 | 5.11 ± 2.99 | F(1,81) = 1.010, p = 0.922, ηp2 = 0.000 | F(1,81) = 0.837, p = 0.435, ηp2 = 0.010 | F(1,81) = 0.451, p = 0.638, ηp2 = 0.006 |
| With surgical mask | 4.74 ± 2.39 | 4.58 ± 2.43 | 4.66 ± 2.39 | ||||
| With mask N95 | 5.02 ± 2.23 | 4.67 ± 2.46 | 4.85 ± 2.34 | ||||
| Average hours of sleeping last week (Hours/week) | Without mask | 11.37 ± 11.37 | 7.68 ± 5.97 a | 9.53 ± 9.21 | F(1,81) = 0.031, p = 0.860, ηp2 = 0.000 | F(1,81) = 0.548, p = 0.579, ηp2 = 0.007 | F(1,81) = 5.384, p = 0.005, ηp2 = 0.062 |
| With surgical mask | 8.34 ± 7.36 | 9.07 ± 6.02 | 8.71 ± 6.7 | ||||
| With mask N95 | 7.88 ± 6.79 b | 12.08 ± 14.89 ab | 9.98 ± 11.63 | ||||
| Sleep quality (a. u.) | Without mask | 5.46 ± 2.65 | 5.77 ± 2.77 | 5.62 ± 2.69 | F(1,81) = 0.176, p = 0.676, ηp2 = 0.002 | F(1,81) = 0.341, p = 0.712, ηp2 = 0.004 | F(1,81) = 0.059, p = 0.943, ηp2 = 0.001 |
| With surgical mask | 5.66 ± 2.6 | 5.88 ± 2.43 | 5.77 ± 2.51 | ||||
| With mask N95 | 5.37 ± 2.78 | 5.64 ± 2.57 | 5.5 ± 2.67 | ||||
| Parameters | Means ± SD | Groups Effect | Mask Effect | Groups × Mask Interaction | ||||
|---|---|---|---|---|---|---|---|---|
| NIG (N = 41) | PIG (N = 42) | All Groups (N = 83) | F(1,81), p-Value, ηp2 | F(1,81), p-Value, ηp2 | F(1,81), p-Value, ηp2 | |||
| Vigorous Intensity | (Days/week) | Without mask | 0.49 ± 1.45 | 0.68 ± 1.43 | 0.59 ± 1.44 | F(1,81) = 7.095, p = 0.009, ηp2 = 0.081 | F(1,81) = 0.952, p = 0.388, ηp2 = 0.012 | F(1,81) = 3.616, p = 0.029, ηp2 = 0.043 |
| With surgical mask | 0.37 ± 0.7 | 1.22 ± 2.18 ab | 0.79 ± 1.65 | |||||
| With mask N95 | 0.29 ± 0.54 | 1.32 ± 1.72 ab | 0.8 ± 1.37 | |||||
| (Hours/week) | Without mask | 0.29 ± 0.99 | 0.4 ± 0.65 | 0.34 ± 0.83 | F(1,81) = 3.899, p = 0.052, ηp2 = 0.046 | F(1,81) = 0.647, p = 0.525, ηp2 = 0.008 | F(1,81) = 2.494, p = 0.086, ηp2 = 0.030 | |
| With surgical mask | 0.28 ± 0.64 | 0.61 ± 1.06 | 0.45 ± 0.88 | |||||
| With mask N95 | 0.2 ± 0.46 | 0.73 ± 1.65 | 0.47 ± 1.24 | |||||
| (MET values) | Without mask | 311 ± 915 | 371 ± 877 | 341 ± 891 | F(1,81) = 3.204, p = 0.077, ηp2 = 0.038 | F(1,81) = 1.336, p = 0.266, ηp2 = 0.016 | F(1,81) = 2.663, p = 0.073, ηp2 = 0.032 | |
| With surgical mask | 145 ± 372 | 1274 ± 4060 | 709 ± 2904 | |||||
| With mask N95 | 196 ± 355 | 1270 ± 3905 | 733 ± 2803 | |||||
| Moderate Intensity | (Days/week) | Without mask | 1.8 ± 1.48 | 1.71 ± 1.69 | 1.76 ± 1.58 | F(1,81) = 0.419, p = 0.520, ηp2 = 0.005 | F(1,81) = 1.624, p = 0.200, ηp2 = 0.020 | F(1,81) = 2.513, p = 0.084, ηp2 = 0.030 |
| With surgical mask | 1.51 ± 1.82 | 1.37 ± 1.75 | 1.44 ± 1.78 | |||||
| With mask N95 | 1.51 ± 1.53 | 2.2 ± 2.02 | 1.85 ± 1.81 | |||||
| (Hours/week) | Without mask | 0.82 ± 0.8 | 0.84 ± 0.94 | 0.83 ± 0.87 | F(1,81) = 0.021, p = 0.885, ηp2 = 0.000 | F(1,81) = 0.635, p = 0.531, ηp2 = 0.008 | F(1,81) = 1.103, p = 0.334, ηp2 = 0.013 | |
| With surgical mask | 0.89 ± 0.96 | 1.06 ± 1.22 | 0.98 ± 1.09 | |||||
| With mask N95 | 1.03 ± 1.11 | 0.8 ± 1.07 | 0.92 ± 1.09 | |||||
| (MET values) | Without mask | 476 ± 555 | 439 ± 630 | 457 ± 590 | F(1,81) = 0.120, p = 0.730, ηp2 = 0.001 | F(1,81) = 0.714, p = 0.491, ηp2 = 0.009 | F(1,81) = 0.634, p = 0.532, ηp2 = 0.008 | |
| With surgical mask | 483 ± 634 | 697 ± 1502 | 590 ± 1147 | |||||
| With mask N95 | 563 ± 741 | 565 ± 987 | 564 ± 866 | |||||
| Walking | (Days/week) | Without mask | 5.12 ± 2.29 | 5.12 ± 2.44 | 5.12 ± 2.35 | F(1,81) = 0.191, p = 0.663, ηp2 = 0.002 | F(1,81) = 0.450, p = 0.638, ηp2 = 0.006 | F(1,81) = 0.150, p = 0.861, ηp2 = 0.002 |
| With surgical mask | 5.05 ± 1.97 | 4.98 ± 2.03 | 5.01 ± 1.99 | |||||
| With mask N95 | 5 ± 2.03 | 4.83 ± 2.08 | 4.91 ± 2.04 | |||||
| (Hours/week) | Without mask | 2.01 ± 2.3 | 1.35 ± 1.59 | 1.68 ± 2 | F(1,81) = 3.979, p = 0.049, ηp2 = 0.047 | F(1,81) = 1.249, p = 0.290, ηp2 = 0.015 | F(1,81) = 0.070, p = 0.933, ηp2 = 0.001 | |
| With surgical mask | 2.01 ± 2.2 | 1.4 ± 1.19 | 1.7 ± 1.8 | |||||
| With mask N95 | 2.56 ± 3.79 | 1.68 ± 2.13 | 2.12 ± 3.1 | |||||
| (MET values) | Without mask | 2231 ± 2851 | 1600 ± 2189 | 1916 ± 2552 | F(1,81) = 4.068, p = 0.047, ηp2 = 0.048 | F(1,81) = 0.641, p = 0.528, ηp2 = 0.008 | F(1,81) = 0.257, p = 0.774, ηp2 = 0.003 | |
| With surgical mask | 2202 ± 2881 | 1397 ± 1437 | 1799 ± 2310 | |||||
| With mask N95 | 2751 ± 3827 | 1569 ± 1944 | 2160 ± 3087 | |||||
| All PA | (Days/week) | Without mask | 5.95 ± 1.73 | 5.88 ± 1.92 | 5.91 ± 1.82 | F(1,81) = 0.002, p = 0.965, ηp2 = 0.000 | F(1,81) = 0.368, p = 0.693, ηp2 = 0.005 | F(1,81) = 0.899, p = 0.409, ηp2 = 0.011 |
| With surgical mask | 5.68 ± 1.89 | 5.76 ± 1.81 | 5.72 ± 1.84 | |||||
| With mask N95 | 5.78 ± 1.8 | 6.02 ± 1.8 | 5.9 ± 1.79 | |||||
| (Hours/week) | Without mask | 3.12 ± 2.86 | 2.59 ± 1.94 | 2.85 ± 2.45 | F(1,81) = 0.698, p = 0.406, ηp2 = 0.009 | F(1,81) = 1.543, p = 0.217, ηp2 = 0.019 | F(1,81) = 0.191, p = 0.827, ηp2 = 0.002 | |
| With surgical mask | 3.18 ± 2.76 | 3.07 ± 2.41 | 3.13 ± 2.58 | |||||
| With mask N95 | 3.79 ± 3.97 | 3.21 ± 3.93 | 3.5 ± 3.94 | |||||
| (MET values) | Without mask | 3019 ± 3205 | 2410 ± 2321 | 2714 ± 2804 | F(1,81) = 0.025, p = 0.876, ηp2 = 0.000 | F(1,81) = 1.214, p = 0.300, ηp2 = 0.015 | F(1,81) = 0.816, p = 0.444, ηp2 = 0.010 | |
| With surgical mask | 2830 ± 3064 | 3368 ± 5702 | 3099 ± 4540 | |||||
| With mask N95 | 3509 ± 3968 | 3404 ± 5827 | 3457 ± 4942 | |||||
| Sitting | (Hours/day) | Without mask | 9.43 ± 4.89 | 9.2 ± 4.59 | 9.31 ± 4.72 | F(1,81) = 0.008, p = 0.930, ηp2 = 0.000 | F(1,81) = 4.585, p = 0.012, ηp2 = 0.054 | F(1,81) = 0.735, p = 0.481, ηp2 = 0.009 |
| With surgical mask | 8.65 ± 3.89 | 8.75 ± 5.55 | 8.7 ± 4.75 | |||||
| With mask N95 | 8.48 ± 3.99 | 7.63 ± 4.15 b | 8.06 ± 4.06 b | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mezghani, N.; Ammar, A.; Boukhris, O.; Masmoudi, L.; Boujelbane, M.A.; Ben Ayed, R.; Alzahrani, T.M.; Hadadi, A.; Abid, R.; Ouergui, I.; et al. The Impact of Wearing Different Face Masks on Vigorous Physical Exercise Performance and Perceived Exertion among COVID-19 Infected vs. Uninfected Female Students. Eur. J. Investig. Health Psychol. Educ. 2023, 13, 2709-2723. https://doi.org/10.3390/ejihpe13110187
Mezghani N, Ammar A, Boukhris O, Masmoudi L, Boujelbane MA, Ben Ayed R, Alzahrani TM, Hadadi A, Abid R, Ouergui I, et al. The Impact of Wearing Different Face Masks on Vigorous Physical Exercise Performance and Perceived Exertion among COVID-19 Infected vs. Uninfected Female Students. European Journal of Investigation in Health, Psychology and Education. 2023; 13(11):2709-2723. https://doi.org/10.3390/ejihpe13110187
Chicago/Turabian StyleMezghani, Nourhen, Achraf Ammar, Omar Boukhris, Liwa Masmoudi, Mohamed Ali Boujelbane, Rayda Ben Ayed, Turki Mohsen Alzahrani, Atyh Hadadi, Rihab Abid, Ibrahim Ouergui, and et al. 2023. "The Impact of Wearing Different Face Masks on Vigorous Physical Exercise Performance and Perceived Exertion among COVID-19 Infected vs. Uninfected Female Students" European Journal of Investigation in Health, Psychology and Education 13, no. 11: 2709-2723. https://doi.org/10.3390/ejihpe13110187
APA StyleMezghani, N., Ammar, A., Boukhris, O., Masmoudi, L., Boujelbane, M. A., Ben Ayed, R., Alzahrani, T. M., Hadadi, A., Abid, R., Ouergui, I., Glenn, J. M., Trabelsi, K., & Chtourou, H. (2023). The Impact of Wearing Different Face Masks on Vigorous Physical Exercise Performance and Perceived Exertion among COVID-19 Infected vs. Uninfected Female Students. European Journal of Investigation in Health, Psychology and Education, 13(11), 2709-2723. https://doi.org/10.3390/ejihpe13110187












