Medical Communication Perceived Self-Efficacy (ME-CO) Scale: Construction and Validation of a New Measuring Instrument from a Socio-Cognitive Perspective
Abstract
1. Introduction
2. The Current Study
Aim and Hypotheses
3. Materials and Methods
3.1. Development of the Preliminary Version of the Scale
3.2. Participants and Procedures
3.3. Measures
3.4. Statistical Analyses (Study 1 and Study 2)
4. Results
4.1. Results of Study 1
4.2. Results of Study 2
4.2.1. Descriptive Analyses
- (1)
- Young physicians: 1 to 9 years in the medical profession (N = 190).
- (2)
- Career professionals: 10 to 20 years in the medical profession (N = 218).
- (3)
- Veterans: 21 to 44 years in the medical profession (N = 222).
4.2.2. Analysis of Psychometric Properties of the 55-Item ME-CO Version
4.2.3. Exploratory Factor Analysis of the 31-Item ME-CO Final Version
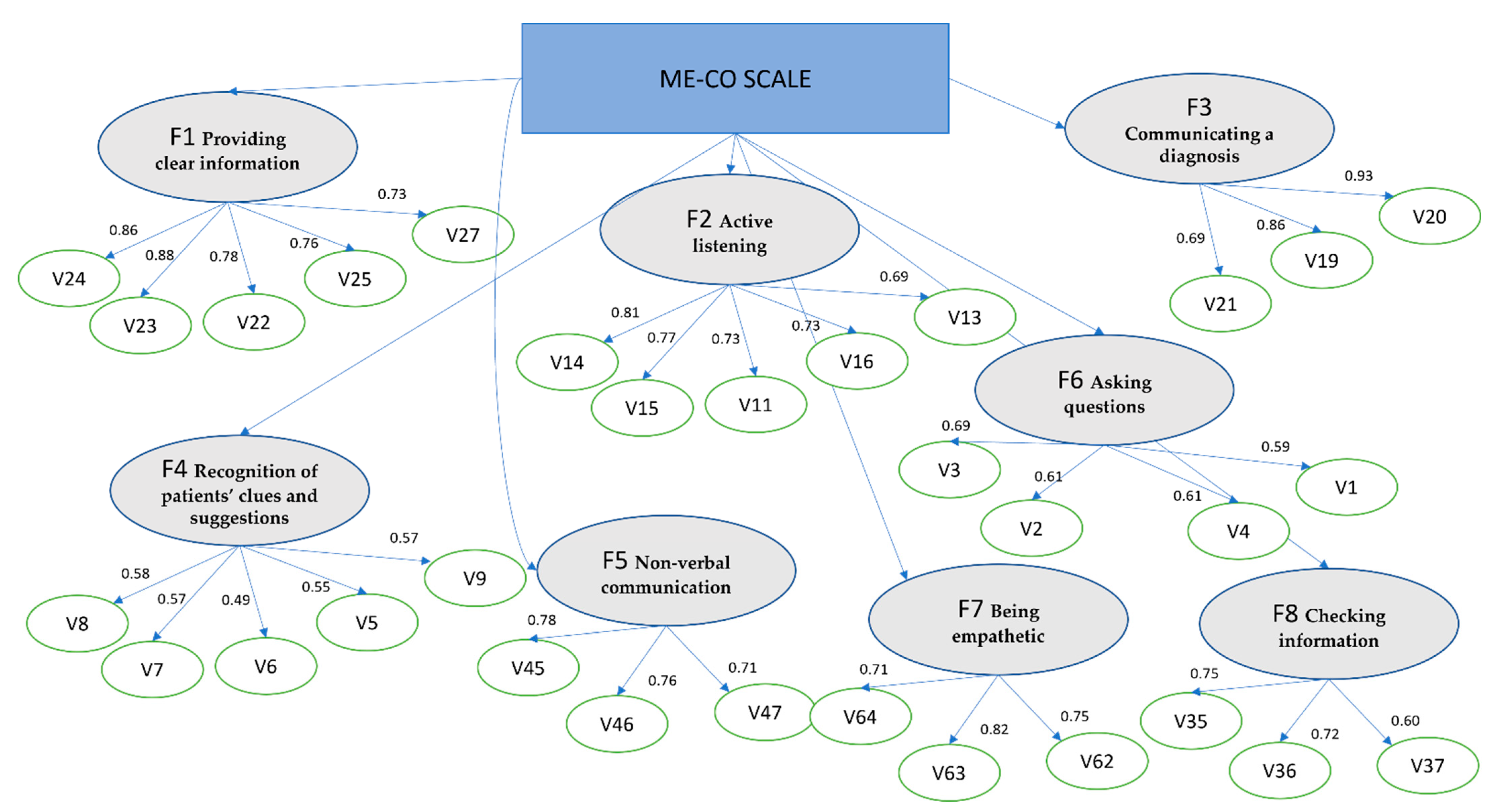
4.2.4. Confirmatory Factor Analysis of the 31-Item Final Version of the ME-CO Scale
4.2.5. External Validity of the ME-CO Scale
5. Discussion
Limitation of the Study
6. Conclusions and Implications for Research
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Capone, V. Le Aspettative di Risultato Nella Comunicazione Medica: Un Nuovo Strumento di Misura. G. Ital. Psicol. 2014, 41, 833–864. [Google Scholar] [CrossRef]
- Capone, V.; Borrelli, R.; Marino, L.; Schettino, G. Mental Well-Being and Job Satisfaction of Hospital Physicians during COVID-19: Relationships with Efficacy Beliefs, Organizational Support, and Organizational Non-Technical Skills. Int. J. Environ. Res. Public Health 2022, 19, 3734. [Google Scholar] [CrossRef] [PubMed]
- Zani, B.; Cicognani, E. Psicologia della Salute; Il Mulino: Bologna, Italy, 2000; ISBN 88-15-07641-7. [Google Scholar]
- Mehta, S.J. Patient satisfaction reporting and its implications for patient care. AMA J. Ethics 2013, 17, 616–621. [Google Scholar] [CrossRef]
- Jones, S.M.W.; Andersen, M.R.; Litwin, P. Avoidance and reassurance seeking in response to health anxiety are differentially related to use of healthcare. J. Public Health 2022, 30, 475–480. [Google Scholar] [CrossRef]
- Capone, V. Percezioni di efficacia comunicativa e burnout dei medici ospedalieri. Psicol. Salut. 2011, 2, 29–47. [Google Scholar] [CrossRef]
- Suchman, A.L.; Roter, D.; Green, M.; Lipkin, M.J.; The Collaborative Study Group of the American Academy on Physician and Patient. Physician Satisfaction with Primary Care Office Visits. Med. Care 1993, 31, 1083–1092. [Google Scholar] [CrossRef]
- Dooley, J.; Bailey, C.; McCabe, R. Communication in healthcare interactions in dementia: A systematic review of observational studies. Int. Psychogeriatr. 2015, 27, 1277–13000. [Google Scholar] [CrossRef]
- Laidlaw, T.S.; Kaufman, D.M.; Sargeant, J.; MacLeod, H.; Blake, K.; Simpson, D. What Makes a Physician an Exemplary Communicator with Patients? Patient. Educ. Couns. 2007, 68, 153–160. [Google Scholar] [CrossRef]
- Sibiya, M.N. Effective Communication in Nursing. Nursing 2018, 19, 20–34. [Google Scholar] [CrossRef]
- Simpson, M.; Buckman, R.; Stewart, M.; Maguire, P.; Lipkin, M.; Novack, D.; Till, J. Doctor-Patient Communication: The Toronto Consensus Statement. BMJ 1991, 303, 1385–1387. [Google Scholar] [CrossRef]
- Maguire, P.; Pitceathly, C. Key Communication Skills and How to Acquire Them. BMJ 2002, 325, 697. [Google Scholar] [CrossRef] [PubMed]
- Barello, S.; Graffigna, G.; Vegni, E. Patient Engagement as an Emerging Challenge for Healthcare Services: Mapping the Literature. Nurs. Res. Pract. 2012, 2012, 905934. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self-Efficacy: The Exercise of Control; W. H. Freeman: New York, NY, USA; Times Books: New York, NY, USA; Henry Holt & Co.: New York, NY, USA, 1997. [Google Scholar]
- Lent, R.W.; Brown, S.D.; Larkin, K.C. Comparison of Three Theoretically Derived Variables in Predicting Career and Academic Behavior: Self-Efficacy, Interest Congruence, and Consequence Thinking. J. Couns. Psychol. 1987, 34, 293–298. [Google Scholar] [CrossRef]
- Bandura, A. Social Cognitive Theory: An Agentic Perspective. Annu. Rev. Psychol. 2001, 52, 1–26. [Google Scholar] [CrossRef]
- Caprara, G.V.; Gerbino, M.; Delle Fratte, A. La Valutazione Dell’autoefficacia [Self-Efficacy Assessment]; Edizioni Erickson: Trento, Italy, 2001. [Google Scholar]
- Thompson, S.C.; Schwankovsky, L.; Pitts, J. Counselling Patients to Make Lifestyle Changes: The Role of Physician Self-Efficacy, Training and Beliefs About Causes. Fam. Pract. 1993, 10, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Capone, V.; Romano, A.; Petrillo, G. La soddisfazione lavorativa e per la vita di medici e infermieri ospedalieri: Relazioni con il senso di appartenenza all’azienda ospedaliera, le percezioni di efficacia collettiva e il sostegno sociale percepito. Psicol. Salut. 2013, 115–130. [Google Scholar] [CrossRef]
- Hyman, D.J.; Maibach, E.W.; Flora, J.A.; Fortmann, S.P. Cholesterol Treatment Practices of Primary Care Physicians. Public Health Rep. 1992, 107, 441. [Google Scholar]
- Gramling, R.; Nash, J.; Siren, K.; Eaton, C.; Culpepper, L. Family Physician Self-Efficacy with Screening for Inherited Cancer Risk. Ann. Fam. Med. 2004, 2, 130. [Google Scholar] [CrossRef][Green Version]
- Rushforth, B.; McCrorie, C.; Glidewell, L.; Midgley, E.; Foy, R. Barriers to Effective Management of Type 2 Diabetes in Primary Care: Qualitative Systematic Review. Br. J. Gen. Pract. 2016, 66, e114. [Google Scholar] [CrossRef]
- Parle, M.; Maguire, P.; Heaven, C. The Development of a Training Model to Improve Health Professionals’ Skills, Self-Efficacy and Outcome Expectancies When Communicating with Cancer Patients. Soc. Sci. Med. 1997, 44, 231–240. [Google Scholar] [CrossRef]
- Nørgaard, B.; Ammentorp, J.; Ohm Kyvik, K.; Kofoed, P.-E. Communication Skills Training Increases Self-Efficacy of Health Care Professionals. J. Contin. Educ. Health Prof. 2012, 32, 90–97. [Google Scholar] [CrossRef]
- Feldman, D.B.; O’Rourke, M.A.; Corn, B.W.; Hudson, M.F.; Agarwal, R.; Fraser, V.L.; Deininger, H.; Fowler, L.A.; Subbiah, I.M. Development and Validation of the Self-Efficacy for Medical Communication Scale. J. Clin. Oncol. 2021, 39, 12124. [Google Scholar] [CrossRef]
- Delle Fave, A.; Bassi, M. Psicologia e Salute: L’esperienza di Utenti e Operatori; UTET Università: Milan, Italy, 2007; ISBN 88-6008-136-X. [Google Scholar]
- Inui, T.S.; Carter, W.B. Problems and Prospects for Health Services Research on Provider-Patient Communication. Med. Care 1985, 23, 521–538. [Google Scholar] [CrossRef] [PubMed]
- Pastorelli, C.; Picconi, L. Autoefficacia scolastica, sociale e regolatoria. In La Valutazione Dell’autoefficacia: Costrutti E Strumenti; Caprara, G.V., Ed.; Edizioni Erikson: Trento, Italy, 2001; pp. 87–104. [Google Scholar]
- Bandura, A. Guide for constructing self-efficacy scales. In Self-Efficacy Beliefs of Adolescents; Pajares, F., Urdan, T., Eds.; Information Age Publishing: Greenwich, CT, USA, 2006; Volume 5, pp. 307–337. [Google Scholar]
- Stein, T.; Frankel, R.M.; Krupat, E. Enhancing Clinician Communication Skills in a Large Healthcare Organization: A Longitudinal Case Study. Patient Educ. Couns. 2005, 58, 4–12. [Google Scholar] [CrossRef]
- Moja, E.A.; Vegni, E. La Visita Medica Centrata sul Paziente; Cortina: Milan, Italy, 2000; ISBN 88-7078-632-3. [Google Scholar]
- Frankel, R.M.; Stein, T. Getting the Most out of the Clinical Encounter: The Four Habits Model. Perm. J. 1999, 3, 79–88. [Google Scholar] [CrossRef]
- Brown, J.; Stewart, M.; McCracken, E.; McWhinney, I.R.; Levenstein, J. The Patient-Centred Clinical Method. 2. Definition and Application. Fam. Pract. 1986, 3, 75–79. [Google Scholar] [CrossRef]
- Lipkin, M.; Putnam, S.M.; Lazare, A. The Medical Interview; Springer: New York, NY, USA, 1995; ISBN 978-1-4612-2488-4. [Google Scholar]
- Epstein, R.M.; Campbell, T.L.; Cohen-Cole, S.A.; McWhinney, I.R.; Smilkstein, G. Perspectives on Patient-Doctor Communication. J. Fam. Pract. 1993, 37, 377. [Google Scholar]
- Back, A.L.; Arnold, R.M.; Baile, W.F.; Tulsky, J.A.; Fryer-Edwards, K. Approaching Difficult Communication Tasks in Oncology. CA Cancer J. Clin. 2005, 55, 164–177. [Google Scholar] [CrossRef]
- Capone, V. Doctor’s self-efficacy perception in communication with patient: A survey among Campanian hospital doctors. Psicol. Salut. 2009, 2, 81–97. [Google Scholar] [CrossRef]
- Lewkonia, R.M. The Medical Interview: The Three-Function Approach. 1991. By Steven A. Cohen-Cole. Published by Mosby Year Book Inc. Can. J. Neurol. Sci. 1991, 18, 368–369. [Google Scholar] [CrossRef]
- Cox, A.; Hopkinson, K.; Rutter, M. Psychiatric Interviewing Techniques II. Naturalistic Study: Eliciting Factual Information. Br. J. Psychiatry 1981, 138, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Cohen-Cole, M.D.; Steven, A. The Medical Interview; Mosby Year Book Inc.: Maryland Heights, MO, USA, 1991. [Google Scholar]
- Bensing, J.; Schreurs, K.; Rijk, A.D. The Role of the General Practitioner’s Affective Behaviour in Medical Encounters. Psychol. Health 1996, 11, 825–838. [Google Scholar] [CrossRef]
- Borella, V.M. La Comunicazione Medico-Sanitaria. le Transazioni Sulla Salute Nella Comunicazione Ospedaliera, Ambulatoriale e di Pronto Soccorso; FrancoAngeli: Milan, Italy, 2004; Volume 11, ISBN 88-464-5264-X. [Google Scholar]
- Silverman, J.; Kurtz, S.; Draper, J. Skills for Communicating with Patients; Crc Press: Boca Raton, FL, USA, 2016; ISBN 0-429-09124-9. [Google Scholar]
- Osterlind, S.J. Constructing Test Items; Kluwer Academic Publishers: London, UK, 1998; ISBN 978-94-009-1071-3. [Google Scholar]
- Sher, T.G.; Cella, D.; Leslie, W.T.; Bonomi, P.; Taylor, I.S.G.; Serafian, B. Communication Differences Between Physicians and Their Patients in an Oncology Setting. J. Clin. Psychol. Med Settings 1997, 4, 281–293. [Google Scholar] [CrossRef]
- Fabrigar, L.R.; Wegener, D.T.; MacCallum, R.C.; Strahan, E.J. Evaluating the Use of Exploratory Factor Analysis in Psychological Research. Psychol. Methods 1999, 4, 272–299. [Google Scholar] [CrossRef]
- Nunnally, J.C.; Bernstein, I.H. Psychometric Theory, 3rd ed.; McGraw-Hill: New York, NY, USA, 1994; ISBN 0-07-047849-X. [Google Scholar]
- Stevens, J.P. Applied Multivariate Statistics for the Social Sciences; Routledge: London, UK, 2012; ISBN 1-136-91069-7. [Google Scholar]
- McDonald, R.P. Comments on D. J. Bartholomew, “Foundations of Factor Analysis: Some Practical Implications”. Br. J. Math. Stat. Psychol. 1985, 38, 134–137. [Google Scholar] [CrossRef]
- Bentler, P.M. EQS Structural Equations Program Manual. Available online: http://www.econ.upf.edu/~satorra/CourseSEMVienna2010/EQSManual.pdf (accessed on 15 January 2022).
- Byrne, B.M. Structural Equation Modeling with EQS and EQS/Windows: Basic Concepts, Applications, and Programming; Sage: Thousand Oaks, CA, USA, 1994; ISBN 0-8039-5092-6. [Google Scholar]
- Hu, L.; Bentler, P.M. Cutoff Criteria for Fit Indexes in Covariance Structure Analysis: Conventional Criteria versus New Alternatives. Struct. Equ. Modeling A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Briones, E.; Tabernero, C.; Tramontano, C.; Caprara, G.V.; Arenas, A. Development of a Cultural Self-Efficacy Scale for Adolescents (CSES-A). Int. J. Intercult. Relat. 2009, 33, 301–312. [Google Scholar] [CrossRef]
- Hebert, J.R.; Ma, Y.; Clemow, L.; Ockene, I.S.; Saperia, G.; Stanek, I.; Edward, J.; Merriam, P.A.; Ockene, J.K. Gender Differences in Social Desirability and Social Approval Bias in Dietary Self-Report. Am. J. Epidemiol. 1997, 146, 1046–1055. [Google Scholar] [CrossRef]
- Matt, G.E.; Garcia, M.; Primicias, W.W.; Frericks, L.; Fabia, F.D. Exploring Biases in Self-Reported Exercising Behavior: Heuristics Based on Recency, Frequency, and Preference. Percept. Mot. Ski. 1999, 88, 126–128. [Google Scholar] [CrossRef]
- Capone, V.; Petrillo, G. Costruzione e validazione della Scala di Autoefficacia Percepita nella Comunicazione Infermieristica. Psicol. Soc. Soc. Psychol. Theory Res. 2011, 3, 387–390. [Google Scholar] [CrossRef]
- Hernández-Padilla, J.M.; Cortés-Rodríguez, A.E.; Granero-Molina, J.; Fernández-Sola, C.; Correa-Casado, M.; Fernández-Medina, I.M.; López-Rodríguez, M.M. Design and Psychometric Evaluation of the ‘Clinical Communication Self-Efficacy Toolkit’. Int. J. Environ. Res. Public Health 2019, 16, 4534. [Google Scholar] [CrossRef] [PubMed]
- Borgogni, L.; Petitta, L.; Steca, P. Efficacia personale e collettiva nei contesti organizzativi. In La Valutazione Dell’autoefficacia: Costrutti e Strumenti; Caprara, G.V., Ed.; Edizioni Erikson: Trento, Italy, 2001; pp. 123–145. [Google Scholar]
- Capone, V.; Petrillo, G. Organizational efficacy, job satisfaction and well-being. The Italian adaptation and validation of Bohn organizational efficacy scale. J. Manag. Dev. 2015, 34, 374–394. [Google Scholar] [CrossRef]
- Barello, S.; Graffigna, G.; Vegni, E.; Bosio, A.C. The challenges of conceptualizing patient engagement in healthcare: A lexicographic literature review. J. Particip. Med. 2014, 6, e9. [Google Scholar]
- Capone, V.; Petrillo, G. Patient’s Communication Perceived Self-efficacy Scale (PCSS): Construction and validation of a new measure in a socio-cognitive perspective. Patient Educ. Couns. 2014, 95, 340–347. [Google Scholar] [CrossRef]
- Capone, V.; Marino, L.; Donizzetti, A.R. The English Version of the Health Profession Communication Collective Efficacy Scale (HPCCE Scale) by Capone and Petrillo, 2012. Eur. J. Investig. Health Psychol. Educ. 2020, 10, 1065–1079. [Google Scholar] [CrossRef]
| Skill | Definition | Example of Item |
|---|---|---|
| Area 1: Information gathering phase | ||
| Questioning skills | Encouraging the expression of the patient’s point of view, identifying symptoms and information necessary to frame his/her condition from a clinical and psycho-social perspective, and using trigger questions appropriately | How much do you feel able to encourage a low-talking patient to express his/her expectations about the outcome of your encounter? |
| Prompts and cues skills | Recognizing and using the clues and the patient’s suggestions, promoting the expression of the underlying information | How much do you feel able to understand from the few hints given by the patient that he/she has difficulties in accepting the therapy? |
| Active listening skills | Listening carefully to the patient, managing non-verbal communication, respecting the turn to speak | How much do you feel able to listen carefully to the patient, even in the presence of colleagues who see this practice as a waste of time? |
| Area 2: Feedback phase | ||
| Talking skills | Talking to the patient using a non-technical language | How much do you feel able to explain a clinical report, for example, a CT scan, in simple language? |
| Communication of the diagnosis | Communicating an inauspicious diagnosis | How much do you feel able to communicate an inauspicious diagnosis to a very sensitive patient? |
| Checking skills | Ensuring that the patient has understood the doctor’s words, testing whether he or she has understood him/her. Checking whether what the doctor understood matches the information provided by the patient | How much do you feel able to check through direct questions whether the patient has understood the diagnosis, even if it seems from the patient’s statements that he/she has understood it? How much do you feel able to repeat the information expressed by the patient synthetically at different times during the visit, even if the interview has already lasted a long time? |
| Area 3: Relationship building and maintenance phase | ||
| Non-verbal use | Using facial expressions, gaze, and proxemic to put the patient at ease | How much do you feel able to look into the patient’s eyes while you are proposing an instrumental investigation that the patient does not agree with? |
| Empathy | Respecting and caring for the patient, empathically returning information taking into account the patient’s agenda, particularly the dimension of their feelings | How do you feel able to show “warmth” to a patient who has had a negative experience with one of your ward colleagues? |
| ME-CO Factors | M | SD |
|---|---|---|
| ME-CO—Providing clear information | 4.02 | 0.71 |
| ME-CO—Active listening | 3.62 | 0.77 |
| ME-CO—Communicating a diagnosis | 3.04 | 0.86 |
| ME-CO—Recognition of patient’s clues and suggestions | 3.61 | 0.64 |
| ME-CO—Non-verbal communication | 3.74 | 0.79 |
| ME-CO—Asking questions | 3.71 | 0.69 |
| ME-CO—Being empathetic | 3.16 | 0.78 |
| ME-CO—Information checking | 3.45 | 0.78 |
| Young N = 190 | Professionals N = 218 | Veterans N = 221 | F (df) | Sig. | |
|---|---|---|---|---|---|
| ME-CO | 3.62 a | 3.61 a | 3.92 b | 3.84(2, 630) | 0.02 |
| ME-CO—Providing clear information | 3.88 a | 4.02 a b | 4.14 b | 5.04(2, 630) | 0.00 |
| ME-CO—Asking questions | 3.60 a | 3.78 a b | 3.83 b | 4.04(2, 630) | 0.01 |
| ME-CO—Information checking | 3.28 a | 3.48 b | 3.53 b | 4.52(2, 630) | 0.01 |
| ITEM | M | SD | Ske | Kur | ITEM | M | SD | Ske | Kur |
|---|---|---|---|---|---|---|---|---|---|
| v25 | 4.10 | 0.84 | −0.56 | −0.31 | v15 | 3.64 | 0.90 | 0.00 | −0.65 |
| v24 | 4.09 | 0.87 | −0.60 | −0.23 | v2 | 3.62 | 0.84 | 0.05 | −0.51 |
| v23 | 3.98 | 0.89 | −0.41 | −0.78 | v34 | 3.59 | 0.82 | −0.04 | −0.19 |
| v27 | 3.94 | 0.86 | −0.38 | −0.40 | v29 | 3.58 | 0.85 | −0.01 | −0.24 |
| v61 | 3.88 | 0.93 | −0.44 | −0.41 | v7 | 3.58 | 0.84 | −0.06 | −0.19 |
| v51 | 3.87 | 0.88 | −0.26 | −0.72 | v4 | 3.57 | 0.88 | −0.05 | −0.50 |
| v1 | 3.84 | 0.92 | −0.22 | −0.72 | v18 | 3.57 | 0.95 | −0.07 | −0.71 |
| v47 | 3.84 | 0.89 | −0.33 | −0.46 | v14 | 3.52 | 0.98 | −0.11 | −0.57 |
| v40 | 3.84 | 0.88 | −0.32 | −0.58 | v57 | 3.52 | 0.92 | −0.11 | −0.27 |
| v56 | 3.83 | 0.96 | −0.51 | −0.21 | v16 | 3.51 | 0.96 | −0.13 | −0.59 |
| v22 | 3.82 | 0.94 | −0.35 | −0.54 | v36 | 3.51 | 0.93 | −0.24 | −0.28 |
| v45 | 3.76 | 0.89 | −0.12 | −0.65 | v53 | 3.48 | 0.95 | −0.03 | −0.40 |
| v6 | 3.74 | 0.80 | 0.10 | −0.61 | v59 | 3.48 | 0.83 | 0.05 | −0.47 |
| v54 | 3.74 | 0.85 | −0.26 | −0.26 | v58 | 3.47 | 0.80 | 0.34 | −0.30 |
| v49 | 3.74 | 0.88 | −0.18 | −0.53 | v30 | 3.44 | 0.96 | −0.21 | −0.45 |
| v26 | 3.73 | 0.88 | −0.19 | −0.43 | v63 | 3.44 | 0.88 | 0.13 | −0.49 |
| v50 | 3.73 | 0.86 | −0.15 | −0.55 | v9 | 3.44 | 0.92 | −0.05 | −0.46 |
| v12 | 3.73 | 0.90 | −0.17 | −0.63 | v5 | 3.43 | 0.93 | −0.02 | −0.60 |
| v13 | 3.73 | 0.89 | −0.13 | −0.79 | v32 | 3.40 | 0.95 | −0.14 | −0.30 |
| v44 | 3.73 | 0.90 | −0.13 | −0.58 | v37 | 3.38 | 0.93 | −0.09 | −0.26 |
| v28 | 3.72 | 1.08 | −0.33 | −0.88 | v33 | 3.38 | 0.91 | 0.02 | −0.22 |
| v60 | 3.71 | 0.80 | 0.09 | −0.71 | v35 | 3.31 | 0.95 | −0.06 | −0.43 |
| v41 | 3.70 | 0.93 | −0.38 | −0.24 | v62 | 3.21 | 0.98 | −0.04 | −0.32 |
| v3 | 3.70 | 0.86 | −0.13 | −0.39 | v19 | 3.07 | 0.93 | 0.18 | −0.28 |
| v8 | 3.67 | 0.86 | −0.13 | −0.36 | v21 | 2.88 | 0.94 | 0.14 | −0.19 |
| v46 | 3.67 | 0.91 | −0.16 | −0.52 | v20 | 2.83 | 1.04 | 0.14 | −0.40 |
| v42 | 3.65 | 0.90 | −0.18 | −0.25 | v64 | 2.78 | 1.08 | 0.20 | −0.43 |
| v11 | 3.65 | 0.97 | −0.25 | −0.48 |
| Item | Factor Loading | Item-Total Correlation | α if Deleted |
|---|---|---|---|
| Factor 1. ME-CO—Providing clear information (α = 0.90) | |||
| v24 | 0.95 | 0.82 | 0.86 |
| v23 | 0.89 | 0.81 | 0.86 |
| v22 | 0.74 | 0.72 | 0.89 |
| v25 | 0.73 | 0.72 | 0.88 |
| v27 | 0.63 | 0.70 | 0.89 |
| Factor 2. ME-CO—Active listening (α = 0.86) | |||
| v14 | 0.97 | 0.76 | 0.81 |
| v15 | 0.80 | 0.72 | 0.82 |
| v11 | 0.67 | 0.64 | 0.84 |
| v16 | 0.64 | 0.65 | 0.84 |
| v13 | 0.58 | 0.64 | 0.84 |
| Factor 3. ME-CO—Communicating a diagnosis (α = 0.88) | |||
| v20 | 0.92 | 0.81 | 0.79 |
| v19 | 0.87 | 0.80 | 0.80 |
| v21 | 0.69 | 0.69 | 0.88 |
| Factor 4. ME-CO—Recognition of patients’ clues and suggestions (α = 0.77) | |||
| v8 | 0.89 | 0.61 | 0.71 |
| v7 | 0.66 | 0.60 | 0.71 |
| v6 | 0.50 | 0.52 | 0.74 |
| v5 | 0.47 | 0.50 | 0.75 |
| v9 | 0.42 | 0.61 | 0.71 |
| Factor 5. ME-CO—Non-verbal communication (α = 0.86) | |||
| v45 | 0.85 | 0.78 | 0.77 |
| v46 | 0.82 | 0.73 | 0.81 |
| v44 | 0.80 | 0.70 | 0.84 |
| Factor 6. ME-CO—Asking questions (α = 0.82) | |||
| v3 | 0.89 | 0.68 | 0.75 |
| v2 | 0.67 | 0.68 | 0.75 |
| v4 | 0.65 | 0.60 | 0.78 |
| v1 | 0.54 | 0.58 | 0.79 |
| Factor 7. ME-CO—Being empathetic (α = 0.77) | |||
| v64 | 0.90 | 0.65 | 0.64 |
| v62 | 0.69 | 0.60 | 0.70 |
| v63 | 0.59 | 0.58 | 0.73 |
| Factor 8. ME-CO—Information checking (α = 0.78) | |||
| v36 | 0.87 | 0.67 | 0.64 |
| v35 | 0.71 | 0.62 | 0.70 |
| v37 | 0.55 | 0.56 | 0.76 |
| Mean a/b | Factor Loading a/b | SD a/b | Ske a/b | Kur a/b | Item-Total Corr. a/b | α if Deleted a/b | |
|---|---|---|---|---|---|---|---|
| 1. ME-CO—Providing clear information (α a = 0. 90, α b = 0.90) | |||||||
| v24 | 4.102/4.081 | 0.93 | 0.85/0.89 | −0.54/−0.65 | −0.46/−0.05 | 0.81/0.83 | 0.86/0.86 |
| v23 | 3.997/3.966 | 0.85 | 0.87/0.92 | −0.38/−0.42 | −0.77/−0.80 | 0.79/0.83 | 0.87/0.86 |
| v25 | 4.124/4.078 | 0.77 | 0.81/0.86 | −0.48/−0.62 | −0.66/−0.06 | 0.72/0.72 | 0.88/0.89 |
| v22 | 3.869/3.773 | 0.75 | 0.90/0.97 | −0.29/−0.38 | −0.70/−0.46 | 0.71/0.72 | 0.89/0.89 |
| v27 | 3.914/3.972 | 0.67 | 0.85/0.86 | −0.31/−0.44 | −0.34/−0.42 | 0.72/0.68 | 0.88/0.89 |
| 2. ME-CO—Active listening (α a = 0.86, α b = 0.86) | |||||||
| v11 | 3.706/3.586 | 0.88 | 1.00/0.95 | −0.40/−0.10 | −0.30/−0.61 | 0.63/0.65 | 0.85/0.84 |
| v14 | 3.455/3.578 | 0.71 | 0.99/0.96 | −0.01/−0.20 | −0.73/−0.35 | 0.77/0.76 | 0.81/0.81 |
| v13 | 3.729/3.726 | 0.70 | 0.87/0.91 | −0.15/−0.11 | −0.69/−0.86 | 0.66/0.62 | 0.84/0.85 |
| v15 | 3.659/3.630 | 0.52 | 0.91/0.89 | −0.03/0.02 | −0.62/−0.67 | 0.73/0.71 | 0.83/0.82 |
| v16 | 3.548/3.481 | 0.44 | 0.96/0.96 | −0.17/−0.08 | −0.45/−0.70 | 0.64/0.66 | 0.85/0.84 |
| 3. ME-CO—Communicating a diagnosis (α a = 0.88, α b = 0.88) | |||||||
| v20 | 2.783/2.870 | 0.91 | 1.03/1.05 | 0.18/0.10 | −0.35/−0.43 | 0.82/0.80 | 0.77/0.79 |
| v19 | 3.003/3.134 | 0.84 | 0.90/0.96 | 0.26/0.09 | −0.10/−0.40 | 0.79/0.80 | 0.80/0.79 |
| v21 | 2.788/2.969 | 0.66 | 0.94/0.94 | 0.24/0.04 | −0.05/−0.24 | 0.69/0.69 | 0.88/0.88 |
| 4. ME-CO—Recognition of patients’ clues and suggestions (α a = 0.78, α b = 0.78) | |||||||
| v8 | 3.636/3.713 | 0.79 | 0.86/0.86 | −0.15/−0.12 | −0.30/−0.42 | 0.59/0.63 | 0.72/0.70 |
| v7 | 3.552/3.603 | 0.75 | 0.83/0.85 | −0.037/−0.09 | −0.21/−0.16 | 0.63/0.57 | 0.71/0.72 |
| v9 | 3.383/3.489 | 0.48 | 0.93/0.91 | −0.09/−0.01 | −0.29/−0.66 | 0.53/0.50 | 0.74/0.74 |
| v6 | 3.748/3.742 | 0.47 | 0.77/0.83 | 0.30/−0.05 | −0.97/−0.36 | 0.53/0.50 | 0.74/0.74 |
| v5 | 3.390/3.469 | 0.41 | 0.93/0.92 | 0.04/−0.07 | −0.67/−0.51 | 0.48/0.51 | 0.76/0.74 |
| 5. ME-CO—Non-verbal communication (α a = 0.86, α b = 0.87) | |||||||
| v46 | 3.662/3.676 | 0.84 | 0.88/0.95 | 0.00/−0.28 | −0.78/−0.34 | 0.75/0.72 | 0.80/0.82 |
| v44 | 3.717/3.735 | 0.77 | 0.88/0.91 | −0.03/−0.22 | −0.72/−0.44 | 0.70/0.70 | 0.84/0.83 |
| v45 | 3.707/3.820 | 0.77 | 0.90/0.87 | −0.03/−0.20 | −0.87/−0.38 | 0.77/0.78 | 0.78/0.76 |
| 6. ME-CO—Asking questions (α a = 0.82, α b = 0.82) | |||||||
| v3 | 3.696/3.707 | 0.84 | 0.84/0.88 | 0.00/−0.25 | −0.56/−0.25 | 0.66/0.70 | 0.77/0.73 |
| v4 | 3.550/3.590 | 0.69 | 0.87/0.88 | 0.14/−0.22 | −0.70/−0.27 | 0.63/0.58 | 0.78/0.78 |
| v2 | 3.599/3.640 | 0.65 | 0.86/0.82 | 0.07/0.04 | −0.57/−0.44 | 0.71/0.65 | 0.75/0.75 |
| v1 | 3.825/3.851 | 0.61 | 0.96/0.88 | −0.27/−0.15 | −0.69/−0.81 | 0.58/0.58 | 0.81/0.78 |
| 7. ME-CO—Being empathetic (α a = 0.80, α b = 0.81) | |||||||
| v64 | 2.764/2.786 | 0.83 | 1.10/1.06 | 0.22/0.18 | −0.45/−0.41 | 0.50/0.66 | 0.59/0.61 |
| v63 | 3.473/3.413 | 0.73 | 0.85/0.91 | 0.17/0.11 | −0.42/−0.56 | 0.39/0.55 | 0.72/0.74 |
| v62 | 3.235/3.189 | 0.70 | 1.00/0.97 | −0.05/−0.03 | −0.40/−0.22 | 0.63/0.59 | 0.43/0.70 |
| 8. ME-CO—Checking information (α a = 0.80, α b = 0.81) | |||||||
| v37 | 3.408/3.358 | 0.74 | 0.98/0.89 | −0.05/−0.15 | −0.45/−0.05 | 0.56/0.56 | 0.74/0.78 |
| v36 | 3.525/3.488 | 0.58 | 0.94/0.92 | −0.20/−0.29 | −0.46/−0.08 | 0.68/0.66 | 0.61/0.67 |
| v35 | 3.332/3.289 | 0.35 | 0.95/0.95 | −0.03/−0.10 | −0.55/−0.31 | 0.58/0.66 | 0.72/0.68 |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. ME-CO | 1 | ||||||||
| 2. Providing clear information | 0.75 ** | 1 | |||||||
| 3. Active listening | 0.78 ** | 0.49 ** | 1 | ||||||
| 4. Communicating a diagnosis | 0.60 ** | 0.35 ** | 0.36 ** | 1 | |||||
| 5. Recognition of patients’ clues and suggestions. | 0.80 ** | 0.56 ** | 0.57 ** | 0.42 ** | 1 | ||||
| 6. Non-verbal communication | 0.70 ** | 0.55 ** | 0.47 ** | 0.34 ** | 0.49 ** | 1 | |||
| 7. Asking questions | 0.77 ** | 0.49 ** | 0.53 ** | 0.40 ** | 0.63 ** | 0.49 ** | 1 | ||
| 8. Being empathetic | 0.64 ** | 0.29 ** | 0.50 ** | 0.34 ** | 0.42 ** | 0.34 ** | 0.41 ** | 1 | |
| 9. Information checking | 0.70 ** | 0.46 ** | 0.49 ** | 0.34 ** | 0.45 ** | 0.40 ** | 0.48 ** | 0.50 ** | 1 |
| 10. Social self-efficacy | 0.53 ** | 0.31 ** | 0.39 ** | 0.38 ** | 0.43 ** | 0.33 ** | 0.39 ** | 0.47 ** | 0.40 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Capone, V. Medical Communication Perceived Self-Efficacy (ME-CO) Scale: Construction and Validation of a New Measuring Instrument from a Socio-Cognitive Perspective. Eur. J. Investig. Health Psychol. Educ. 2022, 12, 765-780. https://doi.org/10.3390/ejihpe12070056
Capone V. Medical Communication Perceived Self-Efficacy (ME-CO) Scale: Construction and Validation of a New Measuring Instrument from a Socio-Cognitive Perspective. European Journal of Investigation in Health, Psychology and Education. 2022; 12(7):765-780. https://doi.org/10.3390/ejihpe12070056
Chicago/Turabian StyleCapone, Vincenza. 2022. "Medical Communication Perceived Self-Efficacy (ME-CO) Scale: Construction and Validation of a New Measuring Instrument from a Socio-Cognitive Perspective" European Journal of Investigation in Health, Psychology and Education 12, no. 7: 765-780. https://doi.org/10.3390/ejihpe12070056
APA StyleCapone, V. (2022). Medical Communication Perceived Self-Efficacy (ME-CO) Scale: Construction and Validation of a New Measuring Instrument from a Socio-Cognitive Perspective. European Journal of Investigation in Health, Psychology and Education, 12(7), 765-780. https://doi.org/10.3390/ejihpe12070056






