Abstract
Background: Therapeutic exercise seems to minimize musculoskeletal risk factors related to swimmer’s shoulder. However, there is an absence of a qualitative evaluation of these programs and a great variability regarding the characteristics of exercises. The objective of this review was to identify, evaluate, and compare exercise programs used to minimize musculoskeletal risk factors related to swimmer’s shoulder. Methods: PubMed, CochraneLibrary, ScienceDirect, and Medscape were searched during January 2022. The research was limited to meta-analyses, systematic reviews, and RCTs written in English, Spanish, and Portuguese without publication time. The researched papers had swimmers as the population, compared an exercise program with another program or without intervention, and had as outcomes musculoskeletal risk factor variables. Results: Eleven articles were considered for analysis. There were three positive effects of strength programs on shoulder rotators’ strength and endurance, two positive effects of strength and stretching programs on shoulder posture, and one positive effect of a stretching program on shoulder ROM and a plyometric program on proprioception. Conclusions: There is high heterogeneity and little methodological quality evidence about the theme. However, strength programs with five or fewer OKC exercises performed out of the water seems to lead to better results in the swimmer’s shoulder prevention.
1. Introduction
Elite swimmers swim around 14,000 m daily, which results in about 2500 shoulder revolutions each workout and 16,000 each training week. This large amount of shoulder revolutions can easily overload soft tissue structures around the shoulder and create an overuse injury [1]. Swimmer’s shoulder is the most common injury in swimmers and is defined as a painful syndrome that occurs mostly in the anterior region of the shoulder and results from repetitive impingement of the rotator cuff under the coracoacromial arch during the technical gesture of swimming [1,2]. It is estimated that 91% of competitive swimmers experience this injury during their sports career [1,3], leading to the major cause of missed practice [2,3,4,5]. Described in the literature are several types of risk factors related to swimmer’s shoulder such as musculoskeletal, training, epidemiological, physiological, and lifestyle factors [1,2,3,5,6,7,8] (Table 1). Musculoskeletal risk factors have great importance in the clinical context because they are modifiable factors and some of them have good power to predict this injury [8].

Table 1.
Summary table of main risk factors related to swimmer’s shoulder.
In the last two decades, several studies have been carried out to test some prevention exercise programs to minimize swimmer’s shoulder musculoskeletal risk factors [9,10,11,12,13,14,15,16,17,18,19]. Most of them have had a positive effect favorable to therapeutic exercise when compared to no intervention, leading to the assertion that therapeutic exercise seems to be one of the principal tools available to prevent this injury [9,10,11,12,13,14]. Mostly, the impact of these therapeutic exercise programs has been studied on variables that characterize the strength and endurance of the shoulder musculature [9,11,12,13,15,16,17,18,19], which seems to be the musculoskeletal risk factor with the highest rate of injury prediction [8]. However, although in a minority, some studies have investigated the impact of therapeutic exercise in other important swimmer’s shoulder risk factors such as posture [10,11], proprioception [9], shoulder range of motion [14], and scapular dyskinesia [17]. The great variability regarding the characteristics of the prevention exercise programs tested, as well as the lack of a detailed qualitative evaluation of each study, makes it impossible to extract strong conclusions that guide and support the clinical practice. Currently, although therapeutic exercises are used in the swimming context, there are no criteria about the best type of exercise, what characteristics it should have, or what its purpose is in the context of prevention. This adds interest to the present study that attempted to fulfil the lack of information about the real effectiveness of therapeutic exercises for swimmers’ shoulder musculoskeletal risk factors.
The main objective of this systematic review was to identify, evaluate, and compare the effectiveness of different therapeutic exercise programs reported in the scientific literature in changing musculoskeletal risk factors related to swimmer’s shoulder: strength and endurance, shoulder posture, proprioception, glenohumeral instability, shoulder range of motion (ROM), and scapular dyskinesia.
2. Materials and Methods
The protocol followed in this review began with the search and selection of individual studies, quality assessment of the studies, data collection, analysis and interpretation of results, and extraction of conclusions. To structure the systematic review, the PRISMA recommendations were used [20] (Table S1). This systematic review was carried out with the participation of 5 researchers. Two researchers carried out the entire process of creating the systematic review and making the final decision on the selection of studies, and the others were responsible for supervising the process and the final evaluation of the review.
2.1. Eligibility Criteria
The research was limited to meta-analyses, systematic reviews, and randomized controlled trials (RCTs) written in English, Spanish, or Portuguese and published in scientific journals. There were no restrictions on the year of publication of the articles sought. The population considered for the searched articles included competitive swimmers of any age without shoulder pain. All articles with athletes from other water sports such as water polo, synchronized swimming, surf, or sports that combined swimming with other sports activities such as aquathlon or triathlon were excluded. Studies that performed a comparison between a therapeutic exercise program with another program or with no intervention were sought. The outcomes were variables that characterize musculoskeletal risk factors described in Table 1. All articles that did not meet the criteria presented above related to study design, language, population, intervention, comparison, and outcomes were excluded from this systematic review. All studies that investigated the acute effects of therapeutic exercise were excluded, and only articles that studied the effect of intervention applied for a minimum of 2 weeks were accepted.
2.2. Information Sources
To carry out the bibliographic research, PubMed, Cochrane Library, ScienceDirect, and Medscape databases were consulted in the period from January 1st to 31st in the year 2022.
2.3. Search Strategy
The criteria applied to each database, as well as the descriptors used in the research, are listed in Table 2.

Table 2.
Databases, criteria applied, and descriptors used in the bibliographic research.
2.4. Selection Process
After performing the bibliographic search, repeated articles were verified and excluded. Then, all titles were read and studies whose population were not swimmers or whose anatomical region under study was not the shoulder were removed. Subsequently, the abstracts were read and all articles that did not have the qualifying study design for this systematic review were excluded. Furthermore, all articles whose intervention was not a therapeutic exercise program and whose results were not variables that characterize musculoskeletal risk factors related to swimmer’s shoulder were also excluded. Finally, the articles were read in full, and the studies that only investigated the acute effect of the therapeutic exercise were removed.
2.5. Data Collection Process
The present data in this systematic review were collected by reading the selected articles, and it was used the information expressed in the published full text. Article identification, eligibility criteria, number of participants, sample characteristics, study design, type of intervention, the outcome of interest, number of dropouts, statistical significance and if available, study limitations were collected.
2.6. Data Items
The independent variables of this review were swimmers and therapeutic exercise programs. All variables characterizing musculoskeletal risk factors for swimmer’s shoulder were dependent variables:
- Strength and endurance: peak torque (PT) or peak force (PF), time to PT or PF, PT or PF to body weight ratio, torque decrement, amortization time, conventional and functional agonist–antagonist PT or PF ratios, and fatigue index.
- Shoulder posture: acromial distance, forward head angle, total scapular distance, and pectoralis minor length.
- Proprioception: joint position sense (JPS), kinesthesia, and force sense.
- Glenohumeral instability: inferior, anterior, and posterior displacement of the humeral head.
- Shoulder ROM: physiological shoulder ROM of internal rotation (IR), external rotation (ER), flexion (FLX), extension (EXT), adduction (ADD), abduction (ABD), horizontal adduction (HADD), and horizontal abduction (HABD); glenohumeral internal rotation deficit (GIRD), total rotational range of motion (TRROM), posterior shoulder tightness (PST), and humeral torsion (HT).
- Scapular dyskinesia: mean difference in the position of the scapula evaluated in: IR and ER, elevation and depression, protraction and retraction, anterior and posterior tipping, and upward and downward rotation.
2.7. Study Risk of Bias Assessment
The assessment of the risk of bias in the studies included in this review was performed by applying the PEDro scale criteria [21]. Whenever the article was already classified in the Physiotherapy Evidence Database (https://pedro.org.au accessed on 13 February 2022), this score was accepted. When this did not happen, the article was read in its entirety and subsequently evaluated by two authors (N.T. and M.A.C.), using the available criteria. The final score higher than 7 was attributed to a study with “high quality”, between 5 and 6 for “moderate quality” was considered, and scores lower than 4 were of “low quality” [22].
Additionally, the RoB2 tool (https://riskofbias.info/welcome/rob-2-0-tool accessed on 20 February 2022) from Cochrane was used. The “robvis (visualization tool)” (https://mcguinlu.shinyapps.io/robvis accessed on 20 February 2022) was used to access the risk of bias characterization charts of the individual studies. A generic evaluation grid was chosen and built two types of charts: a summary plot—where an assessment of certain biases was carried out in each study, and a traffic light plot—which revealed the global percentage of studies that contained the different biases.
2.8. Effect Measures
If possible, the measures collected from the individual studies were the effect size, mean difference between sample groups, the respective confidence interval, and its statistical significance (p-value).
2.9. Certainty Assessment
Certainty assessment of the positive effects was performed by two authors (N.T. and M.A.C.) based on four domains of GRADE assessment: risk of bias, inconsistency, indirectness, and imprecision [23].
3. Results
3.1. Study Selection
After consulting PubMed, Cochrane Library, ScienceDirect, and Medscape databases, a total of 918 articles were found, of which 157 were excluded because they were repeated in more than one database. Then, the title was read and all articles that did not have swimmers as a population and that did not investigate the shoulder were excluded, leaving 225 articles. Of these publications, the abstract was read, and all study designs that were not meta-analyses, systematic reviews, and RCTs were excluded. In the same way, articles that did not compare an exercise program with another program or with no intervention and that did not investigate the impact of exercise on the variables that characterize the musculoskeletal risk factors in swimmer’s shoulder were also excluded. Finally, the 13 remaining articles were fully read, and 2 studies were excluded from this systematic review as they investigated the immediate effects of a therapeutic exercise intervention (Figure 1).
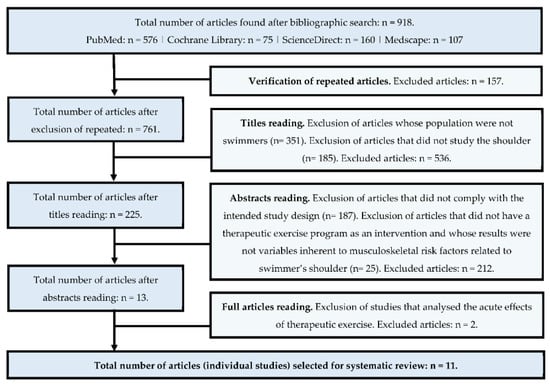
Figure 1.
Study selection process for the systematic review.
3.2. Study Characteristics
The characteristics of the individual studies are described in Table 3.

Table 3.
Individual study characteristics: population, intervention, and conclusion.
3.3. Risk of Bias in Studies

Table 4.
Risk of bias assessment of individual studies using the PEDro scale.
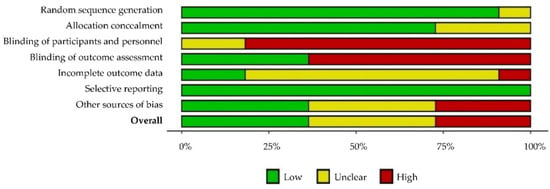
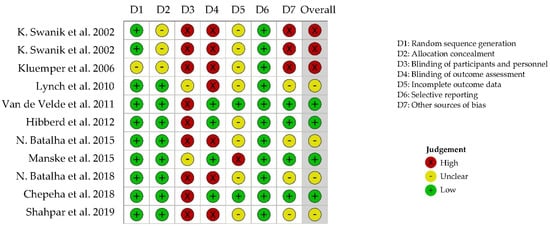
Figure 2.
Risk of bias assessment using RoB2: generic—summary plot and traffic light plot [9,10,11,12,13,14,15,16,17,18,19].
3.4. Results of Individual Studies
3.4.1. Strength Program vs. No Intervention
After performing a 6 week program of plyometric exercises, significant differences were visible in the experimental group in the time to PT of the shoulder IR evaluated at 60°/s (p = 0.020) and 240°/s (p = 0.001), in the time of amortization evaluated at 450°/s (p = 0.008), and in torque decrement rated at 240°/s (p = 0.002). There were no differences between groups in the PT to body weight ratio of IR and ER/IR ratio [9]. In turn, the application of a strength program over 16 weeks led to significant mean differences verified in the experimental group in the PT of the ER: 2.93 ± 2.83 N.m, p = 0.008 (dominant side at 60°/s); 3.23 ± 1.68 N.m, p = 0.015 (non-dominant side at 60°/s); and 2.81 ± 2.66, p = 0.015 (dominant side at 180°/s), and in the ER/IR ratio: 10.31 ± 9.98, p = 0.001 (dominant side at 60°/s); 10.31 ± 9.98, p = 0.036 (non-dominant side at 60°/s); and 12.18 ± 8.66, p = 0.020 (dominant side at 180°/s). No significant differences were visible between groups in the PT of IR [12]. Similarly, the realization of a strength program for 12 weeks also showed a significant difference (p ≤ 0.05) found in the experimental group in the isometric maximum strength of the ER. After the intervention, the experimental group increased 1.19 ± 0.55 kg, which is equivalent to a 23% difference compared to the initial evaluation, and the control group increased 0.46 ± 0.63 kg; that is, an 11% difference compared to the initial evaluation [13]. In the opposite direction, the performance of a 6 week program of functional training did not lead to any significant difference between the experimental and control groups regarding the PT to body weight ratio, tested at 180°/s and 300°/s in IR, ER, HADD, HABD, and Serratus punch [15].
3.4.2. Strength and Stretching Program vs. No Intervention
Although the application of the combined strength and stretching program over 6 weeks resulted in differences in maximal strength of the shoulder flexors (p = 0.020) and abductors (p = 0.014) in the intervention group, this was not considered statistically significant using the Bonferroni test. There were also significant gains in maximal strength in the shoulder extensors (p = 0.005) and muscles responsible for scapular retraction (p < 0.005), but this occurred similarly in both groups [17]. Similarly, another combined strength and stretching program did not cause significant differences between the control and experimental group in maximal strength of the middle trapezius, lower trapezius, and serratus anterior. When performing an analysis between the initial and final evaluation, there were visible improvements in the maximum strength of these muscles (p < 0.05); however, this increase occurred identically in both groups and may be related to the intensity of swimming training [11].
3.4.3. Strength Program vs. Strength Program
The 12 week strength program compared with a 12 week endurance program caused significant improvements in maximal strength and scapular protraction–retraction ratio in both sample groups. However, these programs also led to a significant increase in the fatigue index for protraction on both sides (p = 0.05) and retraction on the non-dominant side (p = 0.009). Therefore, there seems to be a tendency for both programs to have positive effects on strength outcomes, but not on endurance outcomes [16]. In another study, the effectiveness of a dry-land strength program was compared with another strength program performed in water for 10 weeks. The final evaluation showed significant differences (p < 0.05) in the group that performed aquatic exercises in the PT of the IR in both shoulders tested at 60°/s and in the non-dominant shoulder tested at 180°/s. However, this intervention induced a significant decrease in the ER/IR ratios in this experimental group, leading to an imbalance in the shoulder stabilizing muscles of the swimmers. Additionally, the authors described a significant decrease in the ER fatigue ratio of both shoulders (p < 0.05) in the group that performed a dry-land exercise program [18]. Another research compared the effectiveness of an 8 week combined stretching and strength program in an open kinetic chain with another stretching and strength program in a closed kinetic chain and with a control group. The study concluded that open and closed kinetic chain exercises improved (p < 0.05) the PT of ER and IR significantly at all speeds tested—60°/s, 120°/s, and 180°/s. The improvement in strength was more pronounced in the group that performed the open kinematic chain exercise program [19].
3.4.4. Shoulder Posture
After performing a 6 week strength and stretching program, a significant decrease of 9.6 ± 7.3 mm (p < 0.05) in the acromial distance measured in the standing relaxed position was observed in the experimental group [10]. Likewise, after applying an 8 week strength and stretching program, a significant reduction was observed in the anterior angle of the head (p = 0.005) and in the anterior translation of the shoulder (p = 0.001) in the experimental group. No differences were found between groups regarding scapular distance [11].
3.4.5. Proprioception
The application of a plyometric program for 6 weeks led to significant improvements in the experimental group in the two components of proprioception evaluated. Regarding JPS, there was a significant improvement in the 0° ER during the ER movement (p = 0.015); 75° ER during the ER (p = 0.013) and IR (p = 0.007) movements; and 90% of the maximum ER position during the ER (p = 0.032) and IR (p = 0.003) movements. In the kinesthesia, significant differences were visible in all measurements evaluated: 0° ER to IR (p = 0.016) and ER (p = 0.003), 75° ER to IR (p = 0.028) and ER (p = 0.001), and 90% of the maximum ER to IR (p = 0.001) and ER (p = 0.003) [9].
3.4.6. Shoulder ROM
Before and after 4 and 8 weeks of a sleeper stretch, IR and HADD ROM were evaluated in the shoulders. The results indicated a significant gain in the experimental group in dominant shoulder IR ROM (p < 0.001) and in GIRD (p < 0.001) after 4 and 8 weeks; and in non-dominant shoulder IR ROM (p = 0.03), dominant shoulder HADD ROM (p = 0.003), and non-dominant shoulder HADD ROM (p = 0.05) after 8 weeks [14].
3.4.7. Shoulder Dyskinesia
After an execution of the combined strength and stretching program for 6 weeks, it was observed that the differences between the scapular kinematics variables were insignificant. Although there seems to be a tendency for the experimental group to achieve a greater scapular IR at 0° and 30° of flexion and some differences in scapular elevation and depression, this was not considered a significant interaction [17].
3.5. Certainty of Evidence
The effectiveness of a strength program on shoulder rotators’ strength and endurance [9,12,13] and strength and stretching program on shoulder posture [10,11] were classified as moderate evidence because they present a high risk of bias—an average of 4/10 and 3/10 on the PEDro scale. The other two positive effects were classified as low evidence. The first problem is related to the fact that it is impossible to classify the consistency in both cases because there was only one study that reported a positive effect. Additionally, both samples have limitations in their constitution. The effect of a plyometric program [9] was observed only in female swimmers and the effect of a stretching program [14] was studied in a small and poorly characterized sample. Finally, in the first case, there was also a high risk of bias—3/10 on the PEDro scale (Table 5).

Table 5.
Certainty of evidence assessment.
4. Discussion
Summary of Evidence
The main objective of this review was to identify, evaluate, and compare the different therapeutic exercise programs used to minimize musculoskeletal risk factors related to swimmer’s shoulder.
Eleven articles were considered for analysis. There were three positive effects of strength programs on shoulder rotators’ strength and endurance [9,12,13], two positive effects of strength and stretching programs on shoulder posture [10,11], and one positive effect of a stretching program on shoulder ROM [14] and a plyometric program on proprioception [9]. In general, it was observed that there is high heterogeneity in the genesis of these investigations. This fact led to the creation of a systematic review without meta-analyses. One of the examples of this huge variability is in maximal strength. This variable appeared in six different studies [11,12,13,16,18,19], and the authors used two different outcomes for their characterization (PT and PF), two different assessment instruments (isokinetic dynamometer and manual dynamometer), and three different units (Nm, N, and Kg). Additionally, when evaluating the sample groups of these six studies, it was observed that some have compared a therapeutic exercise program with a control group [11,12,13], and others with another therapeutic exercise program under different conditions [16,18,19].
Regarding the qualitative evaluation of the articles, 7 of the 11 studies [9,10,11,12,15,18,19] had low quality, which necessarily leads to the conclusions of this systematic review having to be viewed with some caution (Table 4). The blinding of the participants and the blinding of the evaluators were the main biases found in the individual studies, with a prevalence of high risk of bias above 75% and 50%, respectively (Figure 2).
Strength and endurance were the most analyzed risk factors in individual studies [9,11,12,13,15,16,17,18,19]. All strength programs that caused significant differences in favor of the experimental group had five or fewer exercises [9,12,13], and the only study where this was not observed had seven exercises [15]. When strength programs were tested alone compared to a control group, there seemed to be a positive effect in favor of the experimental group, especially in maximal ER strength [12,13]. In contrast, some studies have applied a combined strength and stretching program that did not show significant changes in strength and endurance variables [11,17]. Lastly, strength programs performed out of the water [18] and with open kinematic chain exercises [19] seems to lead to more significant improvements in strength and endurance outcomes.
In contrast, there were a small number of studies investigating the influence of therapeutic exercise on other musculoskeletal risk factors [9,10,11,14,17]. In two of these studies, the effect of a combined strength and stretching program on shoulder posture was observed, with significant differences favorable to the experimental group in the acromial distance [10], anterior shoulder translation, and in the head forward angle [11]. Although it lacks more robustness, there seems to be a tendency for a strength program to improve some of the components of proprioception [9] and a stretching program to contribute to a better balance in rotation ROM between the dominant and non-dominant shoulder [14]. The analysis of the influence of exercise in the improvement of scapular dyskinesia in swimmers did not show a significant difference; however, this risk factor was only evaluated after a very extensive intervention that combined strength and stretching exercises [17]. No studies were found that explore the impact of therapeutic exercise on glenohumeral instability in swimmers.
About the characteristics of exercise programs, due to their enormous variability, it is difficult to extract strong conclusions. Strength exercises were usually performed with elastic bands [9,10,12,13,15,17,18], focusing mostly on the ER, IR, middle trapezius, lower trapezius, and serratus anterior. All therapeutic exercise programs found had a minimum duration of 6 weeks [9,10,11,12,13,14,15,16,17,18,19], and normally were carried out 2–3 times a week [9,10,11,12,13,15,16,17,18,19]. The most frequently reported volume for strength exercises was three sets of 10 or 15 repetitions [9,10,11,15,16,19]. In turn, muscle stretching exercises tended to be static, with the pectoralis minor being the most targeted muscle [10,11,17,19] (Table 3). Five of seven positive effects considered in this review had progressions over time [9,10,12,13].
The main limitation of this systematic review is the high heterogeneity of the analyzed evidence, making it impossible to carry out a meta-analysis of the results, combined with the low methodological quality of the individual studies, which decreases the reliability of the conclusions obtained.
5. Conclusions
Therapeutic exercise is a strong and safe tool that can be used in the clinical practice of swimming to reduce the risk of injury associated with some musculoskeletal factors. Strength programs, with five or fewer exercises, performed out of the water and with OKC exercises, seem to lead to more improvements in the strength and endurance of the shoulder rotators, and possibly reduce the impact of this musculoskeletal risk factor on swimmer’s shoulder. This program should last for 6 weeks, be carried out 2–3 times a week, and have progressions over time. Programs that combine strength and stretching exercises seem to improve some variables that characterize shoulder posture, but not strength and endurance.
However, there is evidence with high heterogeneity and low methodological quality regarding the effectiveness of therapeutic exercise programs on musculoskeletal risk factors related to swimmer’s shoulder. In the future, more studies are needed to give better consistency and robustness to the conclusions obtained in this review regarding shoulder strength, endurance, and posture. Further investigations are essential to verify the impact of therapeutic exercise on other musculoskeletal risk factors related to swimmer’s shoulder, such as proprioception, shoulder ROM, scapular dyskinesia, and glenohumeral instability.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ejihpe12060044/s1, Table S1: PRISMA 2020 Checklist.
Author Contributions
Conception and study design N.T. and M.A.C.; search and selection of studies, N.T. and M.A.C.; writing, N.T.; visualization, N.T., G.D., P.C., J.P.V.-B., and M.A.C.; manuscript revision, J.P.V.-B. and M.A.C. All authors have read and agreed to the published version of the manuscript.
Funding
Researcher MAC acknowledges the sponsor of FCT—Fundação para a Ciência e a Tecnologia—under the project UIDB/00285/2020 and LA/P/0112/2020.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data sharing not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Struyf, F.; Tate, A.; Kuppens, K.; Feijen, S.; Michener, L.A. Musculoskeletal dysfunctions associated with swimmers’ shoulder. Br. J. Sports Med. 2017, 51, 775–780. [Google Scholar] [CrossRef]
- Hill, L.; Collins, M.; Posthumus, M. Risk factors for shoulder pain and injury in swimmers: A critical systematic review. Phys. Sportsmed. 2015, 43, 412–420. [Google Scholar] [CrossRef] [PubMed]
- Feijen, S.; Tate, A.; Kuppens, K.; Claes, A.; Struyf, F. Swim-training volume and shoulder pain across the life span of the competitive swimmer: A systematic review. J. Athl. Train. 2020, 55, 32–41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walker, H.; Gabbe, B.; Wajswelner, H.; Blanch, P.; Bennell, K. Shoulder pain in swimmers: A 12-month prospective cohort study of incidence and risk factors. Phys. Ther. Sport 2012, 13, 243–249. [Google Scholar] [CrossRef]
- Schlueter, K.R.; Pintar, J.A.; Wayman, K.J.; Hartel, L.J.; Briggs, M.S. Clinical evaluation techniques for injury risk assessment in elite swimmers: A systematic review. Sports Health 2021, 13, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Gaunt, T.; Maffulli, N. Soothing suffering swimmers: A systematic review of the epidemiology, diagnosis, treatment and rehabilitation of musculoskeletal injuries in competitive swimmers. Br. Med. Bull. 2012, 103, 45–88. [Google Scholar] [CrossRef] [Green Version]
- Wanivenhaus, F.; Fox, A.J.; Chaudhury, S.; Rodeo, S.A. Epidemiology of injuries and prevention strategies in competitive swimmers. Sports Health 2012, 4, 246–251. [Google Scholar] [CrossRef] [Green Version]
- Feijen, S.; Struyf, T.; Kuppens, K.; Tate, A.; Struyf, F. Prediction of shoulder pain in youth competitive swimmers: The development and internal validation of a prognostic prediction model. Am. J. Sports Med. 2021, 49, 154–161. [Google Scholar] [CrossRef]
- Swanik, K.A.; Lephart, S.M.; Swanik, C.B.; Lephart, S.P.; Stone, D.A.; Fu, F.H. The effects of shoulder plyometric training on proprioception and selected muscle performance characteristics. J. Shoulder Elbow. Surg. 2002, 11, 579–586. [Google Scholar] [CrossRef] [Green Version]
- Kluemper, M.; Uhl, T.; Hazelrigg, H. Effect of stretching and strengthening shoulder muscles on forward shoulder posture in competitive swimmers. J. Sport Rehabil. 2006, 15, 58–70. [Google Scholar] [CrossRef]
- Lynch, S.S.; Thigpen, C.A.; Mihalik, J.P.; Prentice, W.E.; Padua, D. The effects of an exercise intervention on forward head and rounded shoulder postures in elite swimmers. Br. J. Sports Med. 2010, 44, 376–381. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Batalha, N.; Raimundo, A.; Tomas-Carus, P.; Paulo, J.; Simão, R.; Silva, A.J. Does a land-based compensatory strength-training programme influences the rotator cuff balance of young competitive swimmers? Eur. J. Sport Sci. 2015, 15, 764–772. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manske, R.C.; Lewis, S.; Wolff, S.; Smith, B. Effects of a dry-land strengthening program in competitive adolescent swimmers. Int. J. Sports Phys. Ther. 2015, 10, 858–867. [Google Scholar] [PubMed]
- Chepeha, J.C.; Magee, D.J.; Bouliane, M.; Sheps, D.; Beaupre, L. Effectiveness of a posterior shoulder stretching program on university-level overhead athletes: Randomized controlled trial. Clin. J. Sport Med. 2018, 28, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Swanik, K.A.; Swanik, C.B.; Lephart, S.M.; Huxel, K. The effect of functional training on the incidence of shoulder pain and strength in intercollegiate swimmers. J. Sport Rehabil. 2002, 11, 140–154. [Google Scholar] [CrossRef]
- Van de Velde, A.; De Mey, K.; Maenhout, A.; Calders, P.; Cools, A.M. Scapular-muscle performance: Two training programs in adolescent swimmers. J. Athl. Train. 2011, 46, 160–167. [Google Scholar] [CrossRef] [Green Version]
- Hibberd, E.E.; Oyama, S.; Spang, J.T.; Prentice, W.; Myers, J.B. Effect of a 6-week strengthening program on shoulder and scapular-stabilizer strength and scapular kinematics in division I collegiate swimmers. J. Sport Rehabil. 2012, 21, 253–265. [Google Scholar] [CrossRef]
- Batalha, N.; Dias, S.; Marinho, D.A.; Parraca, J.A. The effectiveness of land and water based resistance training on shoulder rotator cuff strength and balance of youth swimmers. J. Hum. Kinet. 2018, 62, 91–102. [Google Scholar] [CrossRef] [Green Version]
- Shahpar, F.M.; Rahnama, N.; Salehi, S. The effect of 8 weeks open and closed kinetic chain strength training on the torque of the external and internal shoulder rotator muscles in elite swimmers. Asian J. Sports Med. 2019, 10, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef]
- De Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef] [Green Version]
- Pereira, M.J.; Mendes, R.; Mendes, R.S.; Martins, F.; Gomes, R.; Gama, J.; Dias, G.; Castro, M.A. Benefits of pilates in the elderly population: A systematic review and meta-analysis. Eur. J. Investig. Health Psychol. Educ. 2022, 12, 236–268. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions; Version 6.3 (Updated February 2022); Cochrane, 2022; Available online: www.training.cochrane.org/handbook (accessed on 3 April 2022).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).