High-Fidelity Simulation-Based Education: Description of an Original Crisis Resource Management and Sedation Learning for Dental Surgeons
Abstract
:1. Introduction
2. Materials and Methods
2.1. Simulation-Based Sedation Program
2.1.1. Need Assessment
2.1.2. Educational Objectives
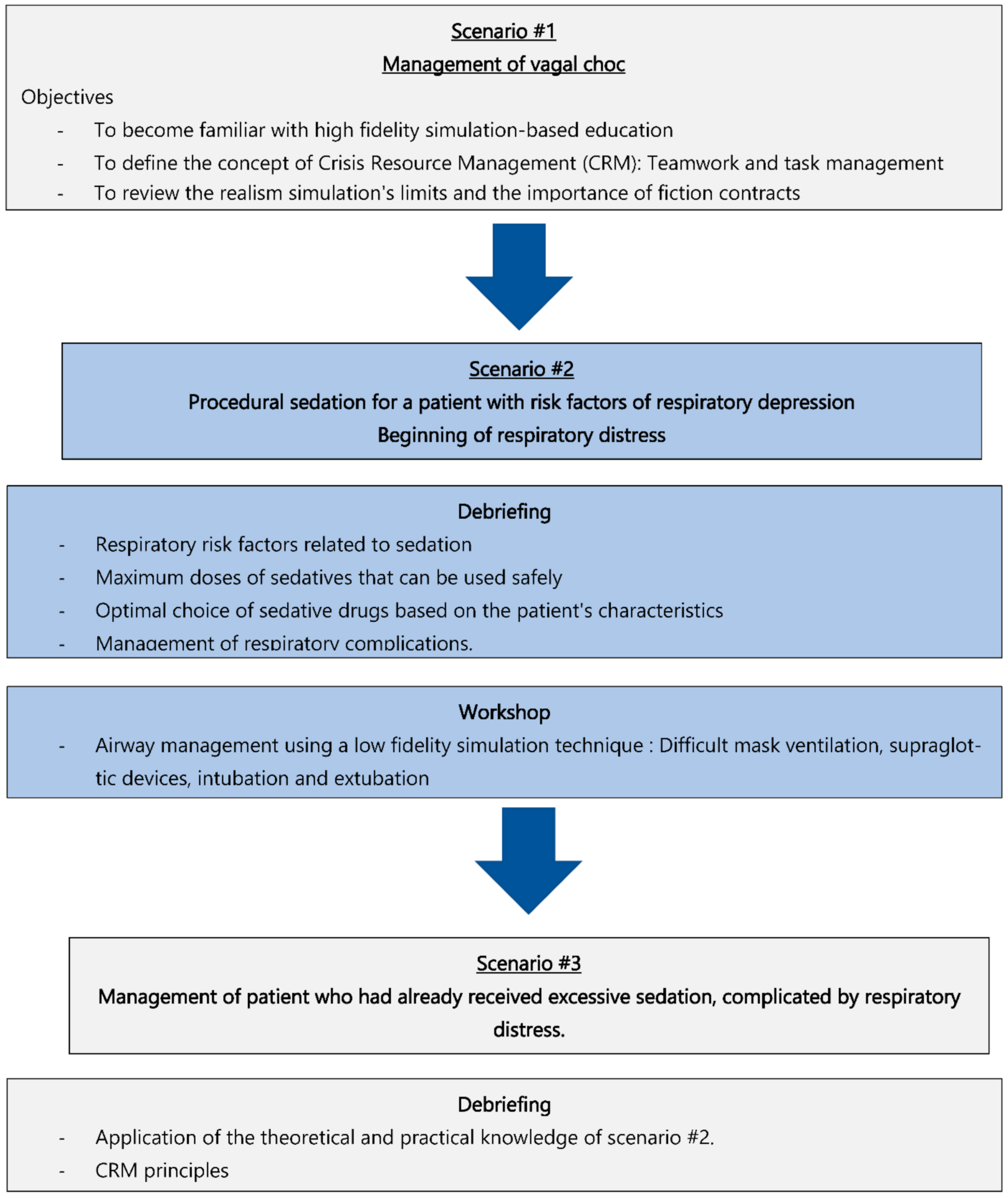
2.1.3. Learning Methods
2.1.4. High Fidelity Simulation and Oriented Debriefing
2.1.5. Data Collection
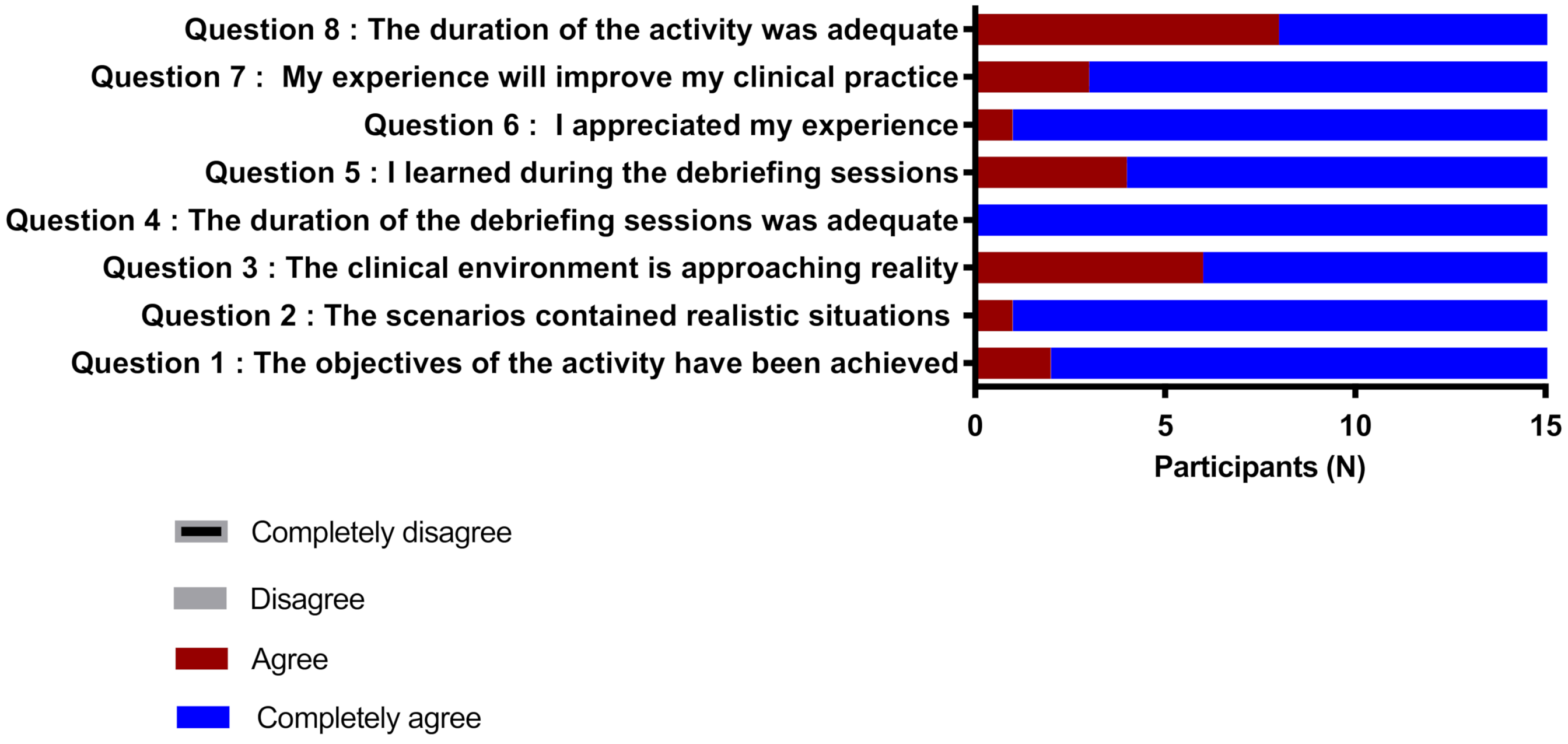
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jeffrey, B.; Gross, M.D.; Farmington, C.T.; Peter, L.; Bailey, M.D. American Society of Anesthesiologists Task Force. Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology 2002, 96, 1004–1017. [Google Scholar]
- McGaghie, W.C.; Issenberg, S.B.; Barsuk, J.H.; Wayne, D.B. A critical review of simulation-based mastery learning with translational outcomes. Med. Educ. 2014, 48, 375–385. [Google Scholar] [CrossRef]
- Fung, L.; Boet, S.; Bould, M.D.; Qosa, H.; Perrier, L.; Tricco, A.; Tavares, W.; Reeves, S. Impact of crisis resource management simulation-based training for interprofessional and interdisciplinary teams: A systematic review. J. Interprof. Care 2015, 29, 433–444. [Google Scholar] [CrossRef]
- Chirurgie Buccale et Maxillofaciale. Available online: http://www.fdsq.qc.ca/fr/maxillo.html (accessed on 17 January 2022).
- Critical Care Nurse Training Standards Task Group Final Report. Available online: https://www.caccn.ca/files/mohltc_report_ccn_stds.pdf (accessed on 17 January 2022).
- Hinkelbein, J.; Lamperti, M.; Akeson, J.; Santos, J.; Costa, J.; de Robertis, E.; Longrois, D.; Novak-Jankovic, V.; Petrini, F.; Struys, M.M.R.F.; et al. European Society of Anaesthesiology and European Board of Anaesthesiology guidelines for procedural sedation and analgesia in adults. Eur. J. Anaesthesiol. 2018, 35, 6–24. [Google Scholar] [CrossRef]
- Royal College of Physicians and Surgeons of Canada: Navigating Medical Emergencies. Available online: https://www.royalcollege.ca/rcsite/ppi/educational-resources-e (accessed on 17 January 2022).
- Dupont, S.; Durand, S.; Garner, M.; Gélinas, C.; Haig, M.J.; Hébert, F.; Morin, L.; Ouellet, J.; Parent, J.; Tétreault, M. Lignes Directrices de Pratique de la Sédation-Analgésie du Collège des Médecins du Québec (CMQ); Publication du Collège des Médecins du Québec: Quebec, QC, Canada, 2015. [Google Scholar]
- Komasawa, N.; Fujiwara, S.; Atagi, K.; Ueki, R.; Haba, M.; Ueshima, H.; Kaminoh, Y.; Minami, T. Effects of a simulation-based sedation training course on non-anesthesiologists’ attitudes toward sedation and analgesia. J. Anesth. 2014, 28, 785–789. [Google Scholar] [CrossRef]
- Krauss, B.; Green, S.M. Training and credentialing in procedural sedation and analgesia in children: Lessons from the United States model. Paediatr. Anaesth. 2008, 18, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Cabadas-Avion, R.; Baluja, A.; Ojea-Cendon, M.; Leal-Ruiloba, M.S.; Vazquez-Lopez, S.; Rey-Martinez, M. Effectiveness and safety of gastrointestinal endoscopy during a specific sedation training program for non-anesthesiologists. Rev. Esp. Enferm. Dig. 2019, 111, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Gordon, M.; Fell, C.W.; Box, H.; Farrell, M.; Stewart, A. Learning health ’safety’ within non-technical skills interprofessional simulation education: A qualitative study. Med. Educ. Online 2017, 22, 1272838. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pearson, E.; McLafferty, I. The use of simulation as a learning approach to non-technical skills awareness in final year student nurses. Nurse Educ. Pract. 2011, 11, 399–405. [Google Scholar] [CrossRef]
- Komasawa, N.; Sanuki, T.; Fujiwara, S.; Haba, M.; Ueki, R.; Kaminoh, Y.; Minami, T. Significance of debriefing methods in simulation-based sedation training courses for medical safety improvement in Japan. Springerplus 2014, 3, 637. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ueshima, H.; Komasawa, N.; Kitamura, A. Hospital Doctors Should Receive Lecture for Sedation According to Joint Commission International. Masui 2015, 64, 883–887. [Google Scholar] [PubMed]
- Fujiwara, S.; Komasawa, N.; Tatsumi, S.; Sawai, T.; Minami, T. Simulation-based sedation training in the operating room. Masui 2014, 63, 934–937. [Google Scholar] [PubMed]
- Villemure, C.; Georgescu, L.M.; Tanoubi, I.; Dubé, J.N.; Chiocchio, F.; Houle, J. Examining perceptions from in situ simulation-based training on interprofessional collaboration during crisis event management in post-anesthesia care. J. Interprof. Care 2019, 33, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Gellis, Z.D.; Kim, E.; Hadley, D.; Packel, L.; Poon, C.; Forciea, M.A.; Bradway, C.; Streim, J.; Seman, J.; Hayden, T.; et al. Evaluation of interprofessional health care team communication simulation in geriatric palliative care. Gerontol. Geriatr. Educ. 2019, 40, 30–42. [Google Scholar] [CrossRef] [PubMed]
- Papastavrou, E.; Dimitriadou, M.; Tsangari, H.; Andreou, C. Nursing students’ satisfaction of the clinical learning environment: A research study. BMC Nurs. 2016, 15, 44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McGaghie, W.C.; Issenberg, S.B.; Cohen ME, R.; Barsuk, J.H.; Wayne, D.B. Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Acad. Med. 2011, 86, 706–711. [Google Scholar] [CrossRef] [PubMed] [Green Version]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tanoubi, I.; Perron, R.; Bélanger, M.-È.; Georgescu, M.; Robitaille, A.; Drolet, P. High-Fidelity Simulation-Based Education: Description of an Original Crisis Resource Management and Sedation Learning for Dental Surgeons. Eur. J. Investig. Health Psychol. Educ. 2022, 12, 91-97. https://doi.org/10.3390/ejihpe12020008
Tanoubi I, Perron R, Bélanger M-È, Georgescu M, Robitaille A, Drolet P. High-Fidelity Simulation-Based Education: Description of an Original Crisis Resource Management and Sedation Learning for Dental Surgeons. European Journal of Investigation in Health, Psychology and Education. 2022; 12(2):91-97. https://doi.org/10.3390/ejihpe12020008
Chicago/Turabian StyleTanoubi, Issam, Roger Perron, Marie-Ève Bélanger, Mihai Georgescu, Arnaud Robitaille, and Pierre Drolet. 2022. "High-Fidelity Simulation-Based Education: Description of an Original Crisis Resource Management and Sedation Learning for Dental Surgeons" European Journal of Investigation in Health, Psychology and Education 12, no. 2: 91-97. https://doi.org/10.3390/ejihpe12020008
APA StyleTanoubi, I., Perron, R., Bélanger, M.-È., Georgescu, M., Robitaille, A., & Drolet, P. (2022). High-Fidelity Simulation-Based Education: Description of an Original Crisis Resource Management and Sedation Learning for Dental Surgeons. European Journal of Investigation in Health, Psychology and Education, 12(2), 91-97. https://doi.org/10.3390/ejihpe12020008






