Accuracy of Body Mass Index and Obesity Status in Police Trainees
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Procedures
2.3. Statistical Analysis
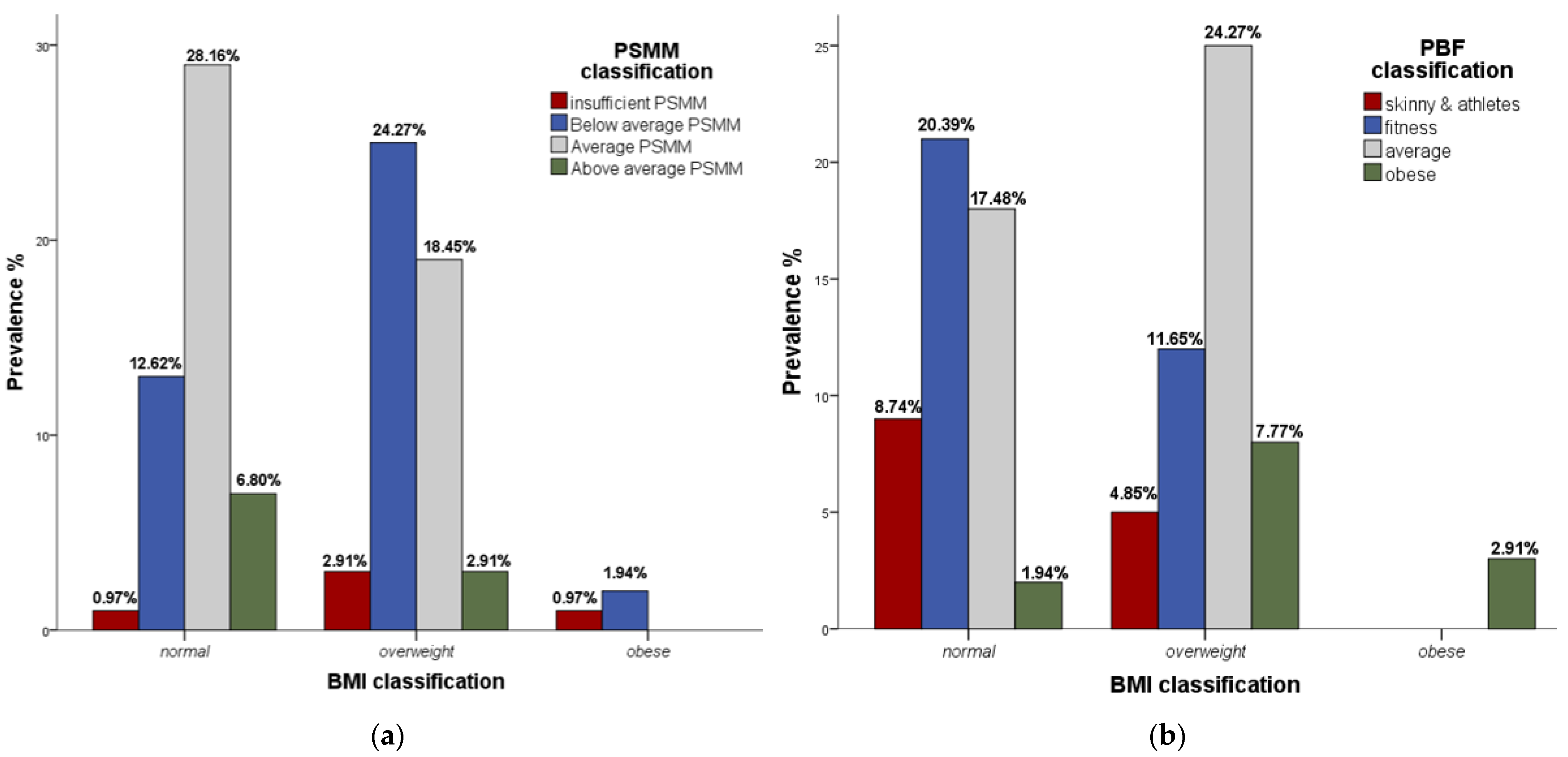
3. Results
4. Discussion
4.1. Study Limitations
4.2. Practical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dawes, J.J.; Orr, R.M.; Siekaniec, C.L.; Vanderwoude, A.A.; Pope, R. Associations between Anthropometric Characteristics and Physical Performance in Male Law Enforcement Officers: A Retrospective Cohort Study. Ann. Occup. Environ. Med. 2016, 28, 26. [Google Scholar] [CrossRef] [PubMed]
- Heinrich, K.M.; Gurevich, K.G.; Arkhangelskaia, A.N.; Karazhelyaskov, O.P.; Poston, W.S.C. Despite Low Obesity Rates, Body Mass Index Under-Estimated Obesity among Russian Police Officers When Compared to Body Fat Percentage. Int. J. Environ. Res. Public Health 2020, 17, 1937. [Google Scholar] [CrossRef]
- Kukić, F.; Koropanovski, N.; Čvorović, A. Body Composition of Police Officers: Occupational Health Perspectives, Issues, and Solutions. In Advances in Health and Disease; Nova Science: New York, NY, USA, 2020; Volume 24, pp. 161–213. ISBN 978-1-5361-8302-3. [Google Scholar]
- Čvorović, A.; Kukić, F.; Orr, R.M.; Dawes, J.J.; Jeknić, V.; Stojković, M. Impact of a 12-Week Postgraduate Training Course on the Body Composition and Physical Abilities of Police Trainees. J. Strength Cond. Res. 2021, 35, 826–832. [Google Scholar] [CrossRef]
- Dopsaj, M.; Kukić, F.; Đorđević-Nikić, M.; Koropanovski, N.; Radovanović, D.; Miljuš, D.; Subošić, D.; Tomanić, M.; Dopsaj, V. Indicators of Absolute and Relative Changes in Skeletal Muscle Mass during Adulthood and Ageing. Int. J. Environ. Res. Public Health 2020, 17, 5977. [Google Scholar] [CrossRef] [PubMed]
- Stojković, M.; Čvorović, A.; Jeknić, V.; Kukić, F. Influence of Two-Month Training Program on Anthropometry and VO2max in Recreational Athletes. Int. J. Phys. Educ. Fit. Sports 2017, 6, 19–24. [Google Scholar] [CrossRef][Green Version]
- Vuković, M.; Kukić, F.; Čvorović, A.; Janković, D.; Prćić, I.; Dopsaj, M. Relations between Frequency and Volume of Leisure-Time Physical Activity and Body Composition in Police Officers. Res. Q. Exerc. Sport 2020, 91, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; Ma, F.; Lou, H.; Liu, Y. The Utility of Fat Mass Index vs. Body Mass Index and Percentage of Body Fat in the Screening of Metabolic Syndrome. BMC Public Health 2013, 13, 629. [Google Scholar] [CrossRef]
- Randhawa, A.K.; Jamnik, V.; Fung, M.D.T.; Fogel, A.S.; Kuk, J.L. No Differences in the Body Fat after Violating Core Bioelectrical Impedance Measurement Assumptions. BMC Public Health 2021, 21, 495. [Google Scholar] [CrossRef] [PubMed]
- Jeknić, V.; Stojković, M.; Bacetić, N. Fitness Level Comparison between Police College Freshman and Senior Students. Int. J. Phys. Educ. Sports Health 2018, 5, 99–104. [Google Scholar]
- Kukić, F.; Dawes, J.; Joyce, J.; Čvorović, A.; Dopsaj, M. Accuracy and predictive capability of body mass index in evaluation of obesity and body fatness level in police officers. NBP—J. Crim. Law 2020, 25, 3–16. [Google Scholar] [CrossRef]
- Dawes, J.J.; Lockie, R.G.; Kukic, F.; Cvorovic, A.; Kornhauser, C.; Holmes, R.; Orr, R.M. Accuracy of Self-Report Height, Body Mass and Derived Body Mass Index in a Group of Law Enforcement Officers. NBP—J. Crim. Law 2019, 24, 7–15. [Google Scholar]
- Kukić, F.; Jeknić, V.; Dawes, J.; Orr, R.; Stojković, M.; Čvorović, A. Effects of Training and a Semester Break on Physical Fitness of Police Trainees. Kinesiology 2019, 51, 161–169. [Google Scholar] [CrossRef]
- Mullie, P.; Vansant, G.; Hulens, M.; Clarys, P.; Degrave, E. Evaluation of Body Fat Estimated from Body Mass Index and Impedance in Belgian Male Military Candidates: Comparing Two Methods for Estimating Body Composition. Mil. Med. 2008, 173, 266–270. [Google Scholar] [CrossRef]
- Violanti, J.M.; Ma, C.C.; Fekedulegn, D.; Andrew, M.E.; Gu, J.K.; Hartley, T.A.; Charles, L.E.; Burchfiel, C.M. Associations Between Body Fat Percentage and Fitness among Police Officers: A Statewide Study. Saf. Health Work. 2017, 8, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Alasagheirin, M.H.; Clark, M.K.; Ramey, S.L.; Grueskin, E.F. Body Mass Index Misclassification of Obesity among Community Police Officers. AAOHN J. 2011, 59, 469–475. [Google Scholar] [CrossRef] [PubMed]
- Boyce, R.; Jones, G.; Lloyd, C. A Longitudinal Observation of Police: Body Composition Changes over 12 Years with Gender and Race Comparisons. J. Exerc. Physiol. Online 2008, 11, 1–13. [Google Scholar]
- Janssen, I.; Heymsfield, B.S.; Wang, Z.; Ross, R. Skeletal Muscle Mass and Distribution in 468 Men and Women Aged 18–88 Yr. J. Appl. Physiol. 2000, 89, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Lagestad, P.; Jenssen, O.R.; Dillern, T. Changes in Police Officers’ Physical Performance after 16 Years of Work. Int. J. Police Sci. Manag. 2014, 16, 308–317. [Google Scholar] [CrossRef]
- Čvorović, A.; Orr, R.M.; Bacetić, N. Effects of a 12-Week Physical Training Program and Nutrition Plan on the Body Composition of Overweight Police Trainers. In International Scientific Conference “Archibald Reiss Days”; Thematic Conference Proceedings of International Significance; Academy of Criminalistic and Police Studies: Belgrade, Serbia, 2018; Volume 2, pp. 49–59. [Google Scholar]
- Kukic, F.; Dopsaj, M.; Dawes, J.; Orr, R.; Cvorovic, A. Use of Human Body Morphology as an Indication of Physical Fitness: Implications for Police Officers. Int. J. Morphol. 2018, 36, 1407–1412. [Google Scholar] [CrossRef]
- Kukić, F.; Dopsaj, M.; Čvorović, A.; Stojković, M.; Jeknić, V. A Brief Review of Body Composition in Police Workforce. Int. J. Phys. Educ. Fit. Sports 2018, 7, 10–19. [Google Scholar] [CrossRef][Green Version]
- Greco, G.; Fischetti, F. Physical, technical, and tactical training and stress management in law enforcement. J. Phys. Educ. Sport. 2018, 18, 555–560. [Google Scholar] [CrossRef]
- World Medical Association (WMA). Declaration of Helsinki. Ethical Principles for Medical Research Involving Human Subjects. Jahrbuch Für Wissenschaft Und Ethik 2009, 14. [Google Scholar] [CrossRef]
- Kukić, F.; Heinrich, K.M.; Koropanovski, N.; Poston, W.S.C.; Čvorović, A.; Dawes, J.J.; Orr, R.; Dopsaj, M. Differences in Body Composition across Police Occupations and Moderation Effects of Leisure Time Physical Activity. Int. J. Environ. Res. Public Health 2020, 17, 6825. [Google Scholar] [CrossRef]
- InBody Co., Ltd. InBody370 USER’S MANUAL 1996. Available online: https://www.inbody.com/en/download_center (accessed on 26 December 2021).
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation; WHO Technical Report Series; World Health Organization: Geneva, Switzerland, 2000; ISBN 978-92-4-120894-9. [Google Scholar]
- Riebe, D.; Ehrman, J.K.; Liguori, G.; Megal, M. ACSM’s Guidelines for Exercise Testing and Prescription, 10th ed.; Wolters Kluwer: Philadelphia, PA, USA, 2018. [Google Scholar]
- Dopsaj, M.; Vuković, M. Prevalenca Indeksa Telesne Mase (BMI) Kod Pripadnika MUP-a Republike Srbije: Pilot Istraživanje. Bezbednost 2015, 3, 28–48. [Google Scholar] [CrossRef]
- Sullivan, G.M.; Feinn, R. Using Effect Size—Or Why the P Value Is Not Enough. J. Grad. Med. Educ. 2012, 4, 279–282. [Google Scholar] [CrossRef]
- Campa, F.; Piras, A.; Raffi, M.; Toselli, S. Functional movement patterns and body composition of high-level volleyball, soccer, and rugby players. J. Sport Rehabil. 2019, 28, 740–745. [Google Scholar] [CrossRef] [PubMed]
- Rothman, K.J. BMI-Related Errors in the Measurement of Obesity. Int. J. Obes. 2008, 32, S56–S59. [Google Scholar] [CrossRef] [PubMed]
- Ho-Pham, L.T.; Lai, T.Q.; Nguyen, M.T.T.; Nguyen, T.V. Relationship between Body Mass Index and Percent Body Fat in Vietnamese: Implications for the Diagnosis of Obesity. PLoS ONE 2015, 10, e0127198. [Google Scholar] [CrossRef]
- Foulis, S.A.; Hughes, J.M.; Friedl, K.E. New Concerns About Military Recruits with Metabolic Obesity but Normal Weight (“Skinny Fat”). Obesity 2020, 28, 223. [Google Scholar] [CrossRef] [PubMed]
| Variables | Calculations | Mean | SD | Min | Max | cV% | K-S Test |
|---|---|---|---|---|---|---|---|
| Age (years) | 21.5 | 0.6 | 21.0 | 23.0 | |||
| BH (cm) | 174.1 | 6.3 | 147.0 | 190.0 | 3.63 | 0.200 | |
| BM (kg) | 76.0 | 8.1 | 58.7 | 99.2 | 10.66 | 0.151 | |
| BMI (kg/m2) | BM/BH2 | 25.1 | 2.1 | 20.9 | 34.3 | 8.47 | 0.002 |
| SMM (kg) | 34.9 | 4.1 | 24.3 | 46.3 | 11.72 | 0.052 | |
| PSMM (%) | (SMM/BM) × 100 | 46.0 | 3.2 | 32.8 | 52.0 | 6.85 | 0.200 |
| BF (kg) | 14.7 | 4.6 | 6.7 | 30.4 | 31.16 | 0.106 | |
| PBF (%) | (BFM/BM) × 100 | 19.2 | 5.2 | 9.5 | 41.1 | 26.81 | 0.200 |
| BMI | N (%) | PSMM | N (%) | PBF | N (%) |
|---|---|---|---|---|---|
| Normal | 50 (48.5) | Insufficient | 5 (4.9) | Skinny and athletes | 14 (13.6) |
| Overweight | 50 (48.5) | Below average | 40 (38.8) | Fitness | 33 (32.0) |
| Obese | 3 (2.9) | Average | 48 (46.6) | Average | 43 (41.7) |
| Above average | 10 (9.7) | Obese | 13 (12.6) |
| Variable | BMI | |
|---|---|---|
| r | p | |
| PBF | 0.361 | <0.001 ** |
| PSMM | −0.344 | <0.001 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stojković, M.; Heinrich, K.M.; Čvorović, A.; Jeknić, V.; Greco, G.; Kukić, F. Accuracy of Body Mass Index and Obesity Status in Police Trainees. Eur. J. Investig. Health Psychol. Educ. 2022, 12, 42-49. https://doi.org/10.3390/ejihpe12010004
Stojković M, Heinrich KM, Čvorović A, Jeknić V, Greco G, Kukić F. Accuracy of Body Mass Index and Obesity Status in Police Trainees. European Journal of Investigation in Health, Psychology and Education. 2022; 12(1):42-49. https://doi.org/10.3390/ejihpe12010004
Chicago/Turabian StyleStojković, Miloš, Katie M. Heinrich, Aleksandar Čvorović, Velimir Jeknić, Gianpiero Greco, and Filip Kukić. 2022. "Accuracy of Body Mass Index and Obesity Status in Police Trainees" European Journal of Investigation in Health, Psychology and Education 12, no. 1: 42-49. https://doi.org/10.3390/ejihpe12010004
APA StyleStojković, M., Heinrich, K. M., Čvorović, A., Jeknić, V., Greco, G., & Kukić, F. (2022). Accuracy of Body Mass Index and Obesity Status in Police Trainees. European Journal of Investigation in Health, Psychology and Education, 12(1), 42-49. https://doi.org/10.3390/ejihpe12010004









