Psychophysiological Regulation and Classroom Climate Influence First and Second Graders’ Well-Being: The Role of Body Mass Index
Abstract
1. Introduction
1.1. Cardiac Vagal Response to Academic Test
1.2. Classroom Climate
1.3. Body Mass Index
1.4. Cardiac Vagal Tone and BMI
1.5. Classroom Climate, BMI and Well-Being
1.6. The Present Study
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Measures
2.3.1. Child’s Perception of His/Her Health and Well-Being
2.3.2. Child’s Perception of Classroom Climate
2.3.3. Simulation of a School Oral Test
2.3.4. Psychophysiological Measure
2.3.5. Body Mass Index
2.4. Statistical Methods
3. Results
3.1. Preliminary Analyses
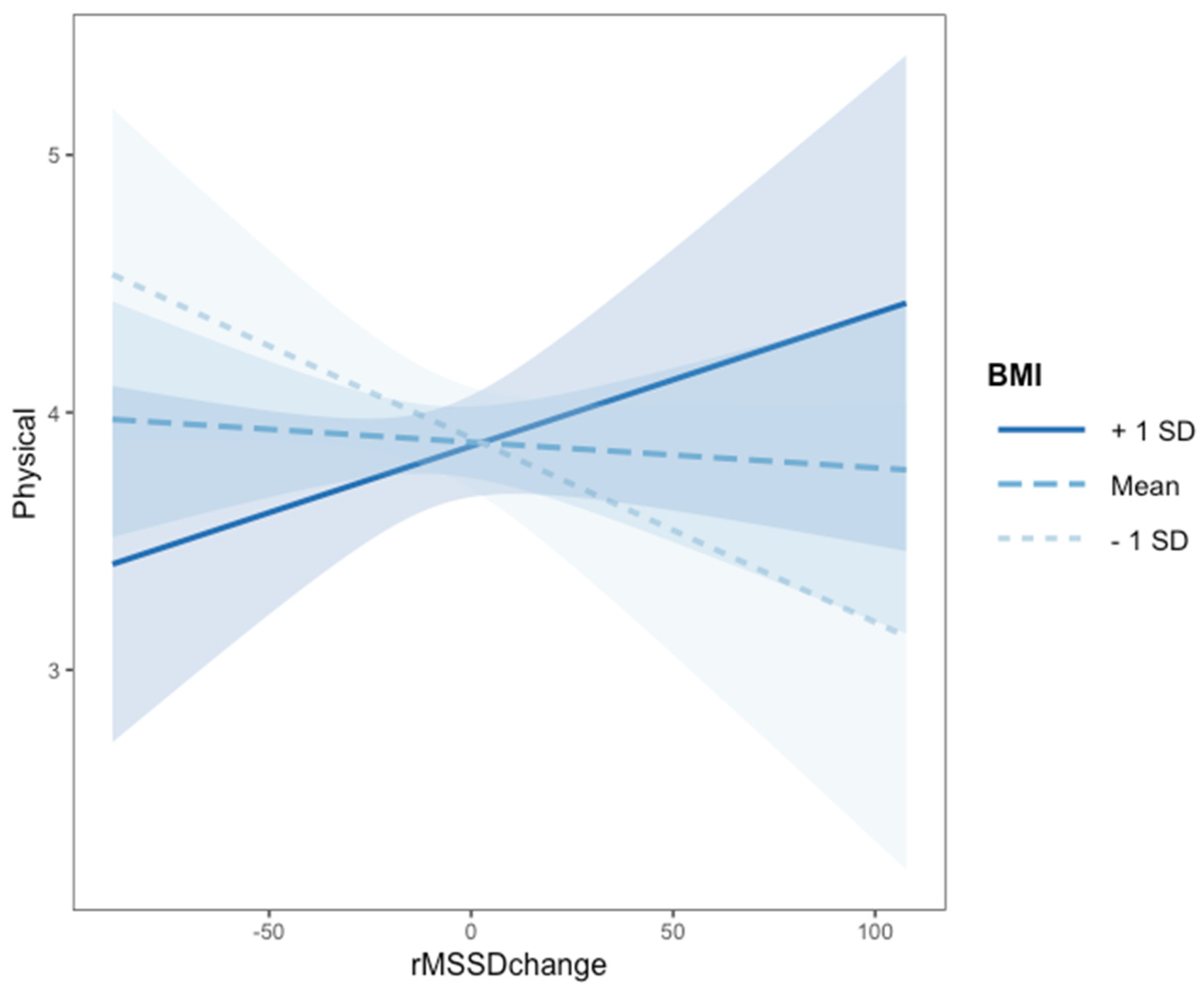
3.2. Association between Classroom Climate, Body Weight, Psychophysiological Regulation and Physical Comfort (RQ1)
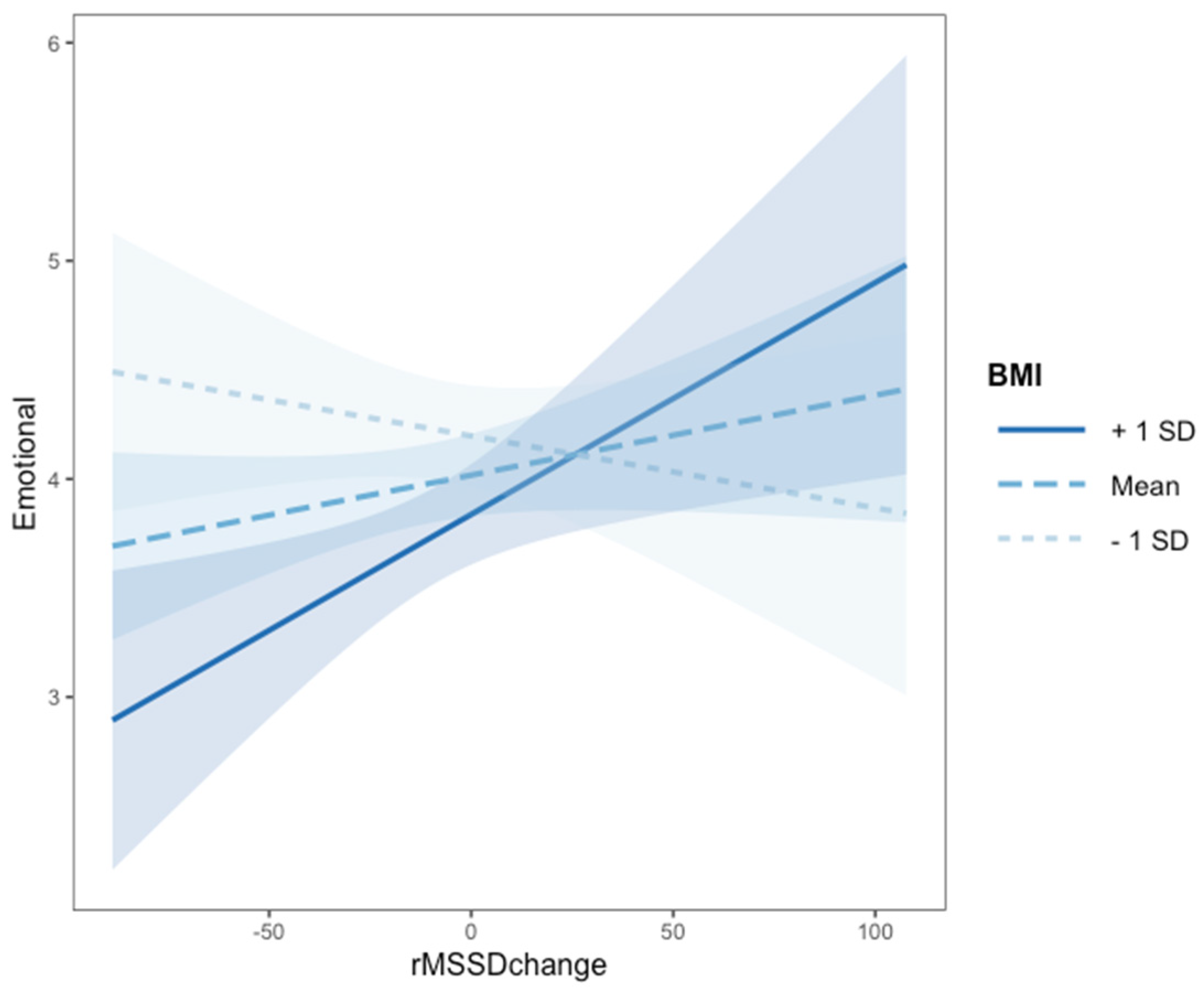
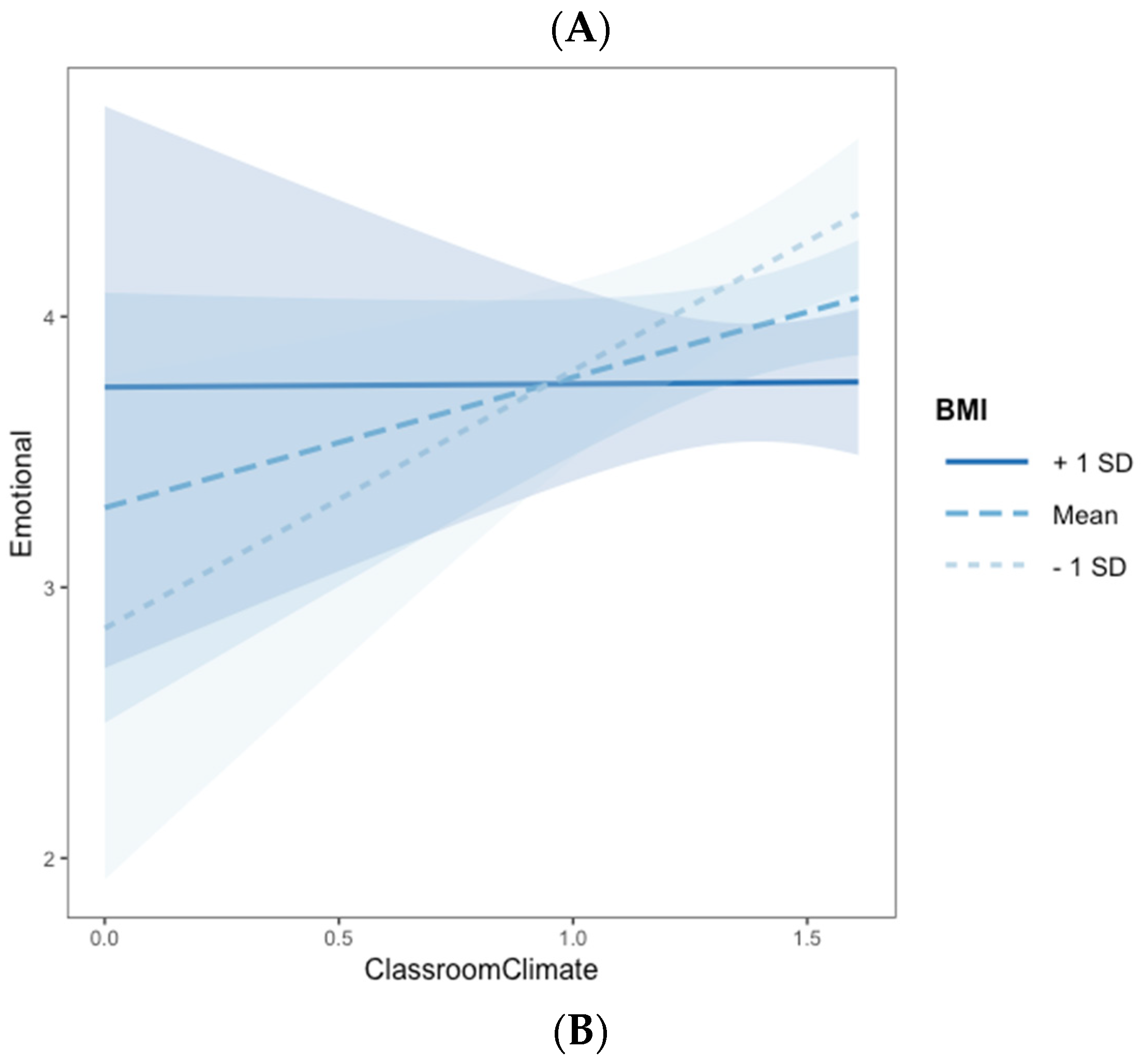
3.3. Association between Classroom Satisfaction, Psychophysiological Regulation, Body Weight and Emotional Comfort (RQ2)
4. Discussion
4.1. Study Limitations
4.2. General Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sirsch, U. The impending transition from primary to secondary school: Challenge or threat? Int. J. Behav. Dev. 2003, 27, 385–395. [Google Scholar] [CrossRef]
- Scrimin, S.; Altoè, G.; Moscardino, U.; Pastore, M.; Mason, L. Individual Differences in Emotional Reactivity and Academic Achievement: A Psychophysiological Study. Mind Brain Educ. 2016, 10, 34–46. [Google Scholar] [CrossRef]
- Scrimin, S.; Moscardino, U.; Altoè, G.; Mason, L. Attentional Bias for Academic Stressors and Classroom Climate Predict Adolescents’ Grades and Socioemotional Functioning. J. Res. Adolesc. 2017, 28, 245–258. [Google Scholar] [CrossRef] [PubMed]
- Masten, A.S. Resilience comes of age: Reflections on the past and outlook for the next generation of research. In Resilience and Development: Positive Life Adaptations; Glantz, M.D., Johnson, J., Huffman, L., Eds.; Plenum: New York, NY, USA, 1999; pp. 289–296. [Google Scholar]
- Moore, K.A.; Lippman, L.; Brown, B. Indicators of Child Well-Being: The Promise for Positive Youth Development. Ann. Am. Acad. Politi. Soc. Sci. 2004, 591, 125–145. [Google Scholar] [CrossRef]
- Ferrans, C.E.; Zerwic, J.J.; Wilbur, J.E.; Larson, J.L. Conceptual Model of Health-Related Quality of Life. J. Nurs. Sch. 2005, 37, 336–342. [Google Scholar] [CrossRef] [PubMed]
- Helliwell, J.F. How’s life? Combining individual and national variables to explain subjective well-being. Econ. Model. 2003, 20, 331–360. [Google Scholar] [CrossRef]
- Wilson, I.B. Linking Clinical Variables with Health-Related Quality of Life. Jama 1995, 273, 59–65. [Google Scholar] [CrossRef]
- Kaplan, D.S.; Liu, R.X.; Kaplan, H.B. School related stress in early adolescence and academic performance three years later: The conditional influence of self expectations. Soc. Psychol. Educ. 2005, 8, 3–17. [Google Scholar] [CrossRef]
- Scrimin, S.; Moscardino, U.; Finos, L.; Mason, L. Effects of Psychophysiological Reactivity to a School-Related Stressor and Temperament on Early Adolescents’ Academic Performance. J. Early Adolesc. 2019, 39, 904–931. [Google Scholar] [CrossRef]
- Scrimin, S.; Moscardino, U.; Mason, L. First-graders’ allocation of attentional resources in an emotional Stroop task: The role of heart period variability and classroom climate. Br. J. Educ. Psychol. 2019, 89, 146–164. [Google Scholar] [CrossRef]
- Nyaradi, A.; Li, J.; Hickling, S.; Whitehouse, A.; Foster, J.K.; Oddy, W.H. Diet in the early years of life influences cognitive outcomes at 10 years: A prospective cohort study. Acta Paediatr. 2013, 102, 1165–1173. [Google Scholar] [CrossRef] [PubMed]
- Redka, I.V.; Danylenko, H.M.; Sotnikova-Meleshkina, Z.V.; Mikhalchuk, O.Y. Prenosological screening of Autonomic Regulatory Systems Tension in secondary school students. Biomed. Biosoc. Anthropol. 2020, 47–53. [Google Scholar] [CrossRef]
- Kreibig, S.D.; Gendolla, G.H.; Scherer, K.R. Goal relevance and goal conduciveness appraisals lead to differential autonomic reactivity in emotional responding to performance feedback. Biol. Psychol. 2012, 91, 365–375. [Google Scholar] [CrossRef]
- Porges, S.W. The polyvagal perspective. Biol. Psychol. 2007, 74, 116–143. [Google Scholar] [CrossRef] [PubMed]
- Calkins, S.D.; Graziano, P.A.; Keane, S.P. Cardiac vagal regulation differentiates among children at risk for behavior problems. Biol. Psychol. 2007, 74, 144–153. [Google Scholar] [CrossRef] [PubMed]
- Porges, S.W.; Doussard-Roosevelt, J.A.; Portales, A.L.; Greenspan, S.I. Infant regulation of the vagal? brake? predicts child behavior problems: A psychobiological model of social behavior. Dev. Psychobiol. 1996, 29, 697–712. [Google Scholar] [CrossRef]
- Scrimin, S.; Patron, E.; Lanfranchi, S.; Moscardino, U.; Palomba, D.; Mason, L. Profiles of vagal withdrawal to challenging interactions: Links with preschoolers’ conceptual shifting ability. Dev. Psychobiol. 2019, 61, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Marcovitch, S.; Leigh, J.; Calkins, S.D.; Leerks, E.M.; O’Brien, M.; Blankson, A.N. Moderate vagal withdrawal in 3.5-year-old children is associated with optimal performance on executive function tasks. Dev. Psychobiol. 2010, 52, 603–608. [Google Scholar] [CrossRef]
- Graziano, P.; Derefinko, K. Cardiac vagal control and children’s adaptive functioning: A meta-analysis. Biol. Psychol. 2013, 94, 22–37. [Google Scholar] [CrossRef]
- Donzella, B.; Gunnar, M.R.; Krueger, W.K.; Alwin, J. Cortisol and vagal tone responses to competitive challenge in preschoolers: Associations with temperament. Dev. Psychobiol. 2000, 37, 209–220. [Google Scholar] [CrossRef]
- Mastromatteo, L.Y.; Zaccoletti, S.; Mason, L.; Scrimin, S. Physiological responses to a school task: The role of student–teacher relationships and students’ emotional appraisal. Br. J. Educ. Psychol. 2021, 91, 1146–1165. [Google Scholar] [CrossRef]
- Oberle, E.; Schonert-Reichl, K.A. Stress contagion in the classroom? The link between classroom teacher burnout and morning cortisol in elementary school students. Soc. Sci. Med. 2016, 159, 30–37. [Google Scholar] [CrossRef]
- Homberg, J.R. The stress-coping (mis)match hypothesis for nature×nurture interactions. Brain Res. 2012, 1432, 114–121. [Google Scholar] [CrossRef] [PubMed]
- Wilson, H.K.; Pianta, R.; Stuhlman, M. Typical Classroom Experiences in First Grade: The Role of Classroom Climate and Functional Risk in the Development of Social Competencies. Elementary Sch. J. 2007, 108, 81–96. [Google Scholar] [CrossRef]
- Haynes, N.M.; Emmons, C.; Ben-Avie, M. School Climate as a Factor in Student Adjustment and Achievement. J. Educ. Psychol. Consult. 1997, 8, 321–329. [Google Scholar] [CrossRef]
- Kutsyuruba, B.; Klinger, D.A.; Hussain, A. Relationships among school climate, school safety, and student achievement and well-being: A review of the literature. Rev. Educ. 2015, 3, 103–135. [Google Scholar] [CrossRef]
- Solomon, D.; Battistich, V.; Watson, M.; Schaps, E.; Lewis, C. A six-district study of educational change: Direct and mediated effects of the child development project. Soc. Psychol. Educ. 2000, 4, 3–51. [Google Scholar] [CrossRef]
- Caprara, G.V.; Barbaranelli, C.; Pastorelli, C.; Bandura, A.; Zimbardo, P.G. Prosocial Foundations of Children’s Academic Achievement. Psychol. Sci. 2000, 11, 302–306. [Google Scholar] [CrossRef] [PubMed]
- Wentzel, K.R. Student motivation in middle school: The role of perceived pedagogical caring. J. Educ. Psychol. 1997, 89, 411–419. [Google Scholar] [CrossRef]
- La Paro, K.M.; Pianta, R.; Stuhlman, M. The Classroom Assessment Scoring System: Findings from the Prekindergarten Year. Elementary Sch. J. 2004, 104, 409–426. [Google Scholar] [CrossRef]
- Fraser, S.W.; Greenhalgh, T. Complexity science: Coping with complexity: Educating for capability. BMJ 2001, 323, 799–803. [Google Scholar] [CrossRef] [PubMed]
- Cimino, S.; Cerniglia, L.; Almenara, C.A.; Ježek, S.; Erriu, M.; Tambelli, R. Developmental trajectories of body mass index and emotional-behavioral functioning of underweight children: A longitudinal study. Sci. Rep. 2016, 6, 20211. [Google Scholar] [CrossRef] [PubMed]
- Pietrobelli, A.; Faith, M.S.; Allison, D.; Gallagher, D.; Chiumello, G.; Heymsfield, S.B. Body mass index as a measure of adiposity among children and adolescents: A validation study. J. Pediatr. 1998, 132, 204–210. [Google Scholar] [CrossRef]
- Tauman, R.; Gozal, D. Obesity and obstructive sleep apnea in children. Paediatr. Respir. Rev. 2006, 7, 247–259. [Google Scholar] [CrossRef]
- Sabia, J.J.; Rees, D.I. Body weight, mental health capital, and academic achievement. Rev. Econ. Househ. 2015, 13, 653–684. [Google Scholar] [CrossRef]
- Luppino, F.S.; de Wit, L.; Bouvy, P.F.; Stijnen, T.; Cuijpers, P.; Penninx, B.W.J.H.; Zitman, F.G. Overweight, Obesity, and Depression. Arch. Gen. Psychiatry 2010, 67, 220–229. [Google Scholar] [CrossRef]
- Hunsberger, M.; on behalf of the IDEFICS Consortium; Lehtinen-Jacks, S.; Mehlig, K.; Gwozdz, W.; Russo, P.; Michels, N.; Bammann, K.; Pigeot, I.; Fernández-Alvira, J.M.; et al. Bidirectional associations between psychosocial well-being and body mass index in European children: Longitudinal findings from the IDEFICS study. BMC Public Health 2016, 16, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Rippe, R.C.; Noppe, G.; Windhorst, D.A.; Tiemeier, H.; van Rossum, E.F.; Jaddoe, V.W.; Verhulst, F.C.; Bakermans-Kranenburg, M.J.; van Ijzendoorn, M.H.; Akker, E.L.V.D. Splitting hair for cortisol? Associations of socio-economic status, ethnicity, hair color, gender and other child characteristics with hair cortisol and cortisone. Psychoneuroendocrinology 2016, 66, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Veldhorst, M.A.B.; Noppe, G.; Jongejan, M.; Kok, C.; Mekic, S.; Koper, J.W.; Van Rossum, E.F.C.; van der Akker, E.L.T. Increased Scalp Hair Cortisol Concentrations in Obese Children. J. Clin. Endocrinol. Metab. 2014, 99, 285–290. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gerber, M.; Endes, K.; Brand, S.; Herrmann, C.; Colledge, F.; Donath, L.; Faude, O.; Pühse, U.; Hanssen, H.; Zahner, L. In 6- to 8-year-old children, hair cortisol is associated with body mass index and somatic complaints, but not with stress, health-related quality of life, blood pressure, retinal vessel diameters, and cardiorespiratory fitness. Psychoneuroendocrinology 2017, 76, 1–10. [Google Scholar] [CrossRef]
- Olstad, D.L.; Ball, K.; Wright, C.; Abbott, G.; Brown, E.; Turner, A.I. Hair cortisol levels, perceived stress and body mass index in women and children living in socioeconomically disadvantaged neighborhoods: The READI study. Stress 2016, 19, 158–167. [Google Scholar] [CrossRef] [PubMed]
- Dallman, M.F.; Pecoraro, N.C.; La Fleur, S.E. Chronic stress and comfort foods: Self-medication and abdominal obesity. Brain Behav. Immun. 2005, 19, 275–280. [Google Scholar] [CrossRef]
- Bergmeier, H.; Skouteris, H.; Horwood, S.; Hooley, M.; Richardson, B. Child temperament and maternal predictors of preschool children’s eating and body mass index. A prospective study. Appetite 2014, 74, 125–132. [Google Scholar] [CrossRef]
- Faith, M.S.; Hittner, J.B. Infant temperament and eating style predict change in standardized weight status and obesity risk at 6 years of age. Int. J. Obes. 2010, 34, 1515–1523. [Google Scholar] [CrossRef]
- Francis, L.A.; Susman, E.J. Self-regulation and Rapid Weight Gain in Children from Age 3 to 12 Years. Arch. Pediatr. Adolesc. Med. 2009, 163, 297–302. [Google Scholar] [CrossRef] [PubMed]
- Leung, C.Y.Y.; Miller, A.; Kaciroti, N.; Chen, S.Y.-P.; Rosenblum, K.; Lumeng, J.C. Low-income pre-schoolers with higher temperamental surgency enjoy and respond more to food, mediating the path to higher body mass index. Pediatr. Obes. 2015, 11, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Epel, E.; Jimenez, S.; Brownell, K.; Stroud, L.; Stoney, C.; Niaura, R. Are Stress Eaters at Risk for the Metabolic Syndrome? Ann. N. Y. Acad. Sci. 2004, 1032, 208–210. [Google Scholar] [CrossRef] [PubMed]
- Cohen, D.A.; Finch, B.K.; Bower, A.; Sastry, N. Collective efficacy and obesity: The potential influence of social factors on health. Soc. Sci. Med. 2006, 62, 769–778. [Google Scholar] [CrossRef] [PubMed]
- Hill, D.; Moss, R.H.; Sykes-Muskett, B.; Conner, M.; O’Connor, D.B. Stress and eating behaviors in children and adolescents: Systematic review and meta-analysis. Appetite 2018, 123, 14–22. [Google Scholar] [CrossRef]
- O’Connor, D.B.; Conner, M. Effects of stress on eating behaviour. In The Handbook of Stress Science: Biology, Psychology and Health; Richard, J., Contrada, B., Andrew, B., Eds.; Springer Publishing Company: New York, NY, USA, 2011; pp. 275–286. [Google Scholar]
- Oliver, G.; Wardle, J. Perceived Effects of Stress on Food Choice. Physiol. Behav. 1999, 66, 511–515. [Google Scholar] [CrossRef]
- Tamashiro, K.L.; Sakai, R.R.; Shively, C.A.; Karatsoreos, I.N.; Reagan, L.P. Chronic stress, metabolism, and metabolic syndrome. Stress 2011, 14, 468–474. [Google Scholar] [CrossRef]
- Petrovich, G.D. Forebrain networks and the control of feeding by environmental learned cues. Physiol. Behav. 2013, 121, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Riley, A.W.; Forrest, C.B.; Rebok, G.W.; Starfield, B.; Green, B.F.; Robertson, J.A.; Friello, P. The Child Report Form of the CHIP–Child Edition. Med. Care 2004, 42, 221–231. [Google Scholar] [CrossRef]
- Berntson, G.G.; Bigger, J.T.; Eckberg, D.L.; Grossman, P.; Kaufmann, P.G.; Malik, M.; Nagaraja, H.N.; Porges, S.W.; Saul, J.P.; Stone, P.H.; et al. Heart rate variability: Origins, methods, and interpretive caveats. Psychophysiology 1997, 34, 623–648. [Google Scholar] [CrossRef] [PubMed]
- Cole, T.J.; Flegal, K.; Nicholls, D.; Jackson, A.A. Body mass index cut offs to define thinness in children and adolescents: International survey. BMJ 2007, 335, 194. [Google Scholar] [CrossRef] [PubMed]
- Krebs, N.F. American Academy of Pediatrics Committee on Nutrition Prevention of Pediatric Overweight and Obesity. Pediatrics 2003, 112, 424–430. [Google Scholar] [CrossRef] [PubMed]
- De Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef]
- Mardia, K.V. Applications of some measures of multivariate skewness and kurtosis in testing normality and robustness stud-ies. Sankhyā. Indian J. Stat. Ser. B 1974, 115–128. Available online: http://www.jstor.org/stable/25051892 (accessed on 29 November 2021).
- Akaike, H. Factor analysis and AIC. Psychometrika 1987, 52, 317–332. [Google Scholar] [CrossRef]
- Wagenmakers, E.-J.; Farrell, S. AIC model selection using Akaike weights. Psychon. Bull. Rev. 2004, 11, 192–196. [Google Scholar] [CrossRef]
- Bauer, D.J.; Curran, P.J. Probing Interactions in Fixed and Multilevel Regression: Inferential and Graphical Techniques. Multivar. Behav. Res. 2005, 40, 373–400. [Google Scholar] [CrossRef]
- Wickham, H.; Chang, W. Ggplot2: An Implementation of the Grammar of Graphics. R Package Version. 2018, 1.0. Available online: https://cran.r-project.org/web/packages/ggplot2/index.html (accessed on 10 September 2021).
- Micceri, T. The unicorn, the normal curve, and other improbable creatures. Psychol. Bull. 1989, 105, 156–166. [Google Scholar] [CrossRef]
- Berkowitz, R.; Moore, H.; Astor, R.A.; Benbenishty, R. A Research Synthesis of the Associations between Socioeconomic Background, Inequality, School Climate, and Academic Achievement. Rev. Educ. Res. 2017, 87, 425–469. [Google Scholar] [CrossRef]
- Upadyaya, K.; Salmela-Aro, K. Development of School Engagement in Association with Academic Success and Well-Being in Varying Social Contexts: A review of empirical research. Eur. Psychol. 2013, 18, 136–147. [Google Scholar] [CrossRef]
- Beauchaine, T.P.; Thayer, J.F. Heart rate variability as a transdiagnostic biomarker of psychopathology. Int. J. Psychophysiol. 2015, 98, 338–350. [Google Scholar] [CrossRef] [PubMed]
- Pauli-Pott, U.; Albayrak, Ö.; Hebebrand, J.; Pott, W. Association between Inhibitory Control Capacity and Body Weight in Overweight and Obese Children and Adolescents: Dependence on Age and Inhibitory Control Component. Child Neuropsychol. 2010, 16, 592–603. [Google Scholar] [CrossRef]
- World Health Organization. Guiding Principles for Feeding Non-Breastfed Children 6-24 Months of Age; World Health Organization: Geneva, Switzerland, 2005; Available online: http://www.who.int/childgrowth/en/ (accessed on 24 October 2021).
- Breslin, G.; Gossrau-Breen, D.; McCay, N.; Gilmore, G.; Macdonald, L.; Hanna, D. Physical Activity, Gender, Weight Status, and Wellbeing in 9- to 11-Year-Old Children: A Cross-Sectional Survey. J. Phys. Act. Health 2012, 9, 394–401. [Google Scholar] [CrossRef]
- Silveira, D.; De Aguiar Carrazedo Taddei, J.A.; Escrivão, M.A.; Oliveira, F.L.; Ancona-Lopez, F. Risk factors for overweight among Brazilian adolescents of low-income families: A case-control study. Public Health Nutr. 2006, 9, 421–428. [Google Scholar] [CrossRef]
- Belsky, J. The differential susceptibility hypothesis: Sensitivity to the environment for better and for worse. JAMA Pediatr. 2016, 170, 321–322. [Google Scholar] [CrossRef]
- Belsky, J.; Pluess, M. Beyond diathesis stress: Differential susceptibility to environmental influences. Psychol. Bull. 2009, 135, 885–908. [Google Scholar] [CrossRef]
- De Sousa, A.F.M.; Medeiros, A.R.; Benitez-Flores, S.; Del Rosso, S.; Stults-Kolehmainen, M.; Boullosa, D.A. Improvements in Attention and Cardiac Autonomic Modulation After a 2-Weeks Sprint Interval Training Program: A Fidelity Approach. Front. Physiol. 2018, 9, 1–9. [Google Scholar] [CrossRef]
- Kim, S.; Kim, Y.; Park, S.M. Body Mass Index and Decline of Cognitive Function. PLoS ONE 2016, 11, e0148908. [Google Scholar] [CrossRef]
- Gao, Z.; Lee, J.E.; Zeng, N.; Pope, Z.C.; Zhang, Y.; Li, X. Home-Based Exergaming on Preschoolers’ Energy Expenditure, Cardiovascular Fitness, Body Mass Index and Cognitive Flexibility: A Randomized Controlled Trial. J. Clin. Med. 2019, 8, 1745. [Google Scholar] [CrossRef] [PubMed]
- Thayer, J.F.; Lane, R.D. A model of neurovisceral integration in emotion regulation and dysregulation. J. Affect. Disord. 2000, 61, 201–216. [Google Scholar] [CrossRef]
| 2 | 3 | 4 | 5 | 6 | 7 | M (SD) | Range | |
|---|---|---|---|---|---|---|---|---|
| 1. Physical Comfort | 0.283 ** | 0.186 * | −0.066 | −0.077 | 0.090 | −0.031 | 3.91 (0.77) | 1.2–5 |
| 2. Emotional Comfort | 0.146 | 0.078 | −0.219 ** | −0.021 | −0.065 | 3.86 (0.74) | 2–5 | |
| 3. Classroom Climate a | 0.084 | −0.059 | −0.214 * | 0.169 * | 1.44 (0.22) | 0–1.61 | ||
| 4. rMSSD change | −0.043 | −0.212 * | 0.076 | −7.93 (24.61) | −88.80–107.70 | |||
| 5. zBMI | 0.151 | −0.019 | 0.08 (0.92) | −2.10–3.81 d | ||||
| 6. Age b | −0.031 | 6.82 (0.71) | 6–8 | |||||
| 7. Gender c | 63 (44%) boys |
| Panel A: Summary of Regression Analysis for Variables Predicting Physical Comfort | |||
|---|---|---|---|
| Predictor | B (SE) a | p | η2p |
| rMSSD change | −0.036 (0.017) * | 0.033 | 0.002 |
| Classroom Climate | 0.694 (0.300) * | 0.023 | 0.040 |
| zBMI | −0.005 (0.023) | 0.825 | 0.007 |
| rMSSD change x zBMI | 0.002 (0.009) * | 0.038 | 0.033 |
| Total R2 a | 0.15 | ||
| N | 138 | ||
| Panel B: Summary of Regression Analysis for Variables Predicting Emotional Comfort | |||
| Predictor | B(SE)a | p | η2p |
| Gender b | −0.237 (0.128) | 0.066 | 0.026 |
| rMSSD change | −0.036 (0.017) * | 0.031 | 0.011 |
| Classroom Climate | 3.138 (1.230) * | 0.012 | 0.029 |
| zBMI | 0.164 (0.100) | 0.102 | 0.064 |
| rMSSD change x zBMI | 0.002 (0.009) * | 0.018 | 0.043 |
| Classroom Climate x zBMI | −0.155(0.071) * | 0.032 | 0.036 |
| Total R2 a | 0.15 | ||
| N | 139 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scrimin, S.; Peruzza, M.; Mastromatteo, L.Y.; Patron, E. Psychophysiological Regulation and Classroom Climate Influence First and Second Graders’ Well-Being: The Role of Body Mass Index. Eur. J. Investig. Health Psychol. Educ. 2021, 11, 1581-1598. https://doi.org/10.3390/ejihpe11040112
Scrimin S, Peruzza M, Mastromatteo LY, Patron E. Psychophysiological Regulation and Classroom Climate Influence First and Second Graders’ Well-Being: The Role of Body Mass Index. European Journal of Investigation in Health, Psychology and Education. 2021; 11(4):1581-1598. https://doi.org/10.3390/ejihpe11040112
Chicago/Turabian StyleScrimin, Sara, Marta Peruzza, Libera Ylenia Mastromatteo, and Elisabetta Patron. 2021. "Psychophysiological Regulation and Classroom Climate Influence First and Second Graders’ Well-Being: The Role of Body Mass Index" European Journal of Investigation in Health, Psychology and Education 11, no. 4: 1581-1598. https://doi.org/10.3390/ejihpe11040112
APA StyleScrimin, S., Peruzza, M., Mastromatteo, L. Y., & Patron, E. (2021). Psychophysiological Regulation and Classroom Climate Influence First and Second Graders’ Well-Being: The Role of Body Mass Index. European Journal of Investigation in Health, Psychology and Education, 11(4), 1581-1598. https://doi.org/10.3390/ejihpe11040112






